Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An esophagogram, sometimes called a barium swallow, should be used to evaluate pharyngeal mucosa, whereas a modified barium swallow should be used to assess deglutition.
Positron emission tomography–computed tomography (PET-CT) has become an essential modality for the staging, monitoring, and surveillance of skull base, pharyngeal, and esophageal cancers.
The role of fluoroscopy in patients with dysphagia has undergone extensive changes in response to a better understanding of potential causes of this symptom.
Although endoscopy has replaced fluoroscopy for many pharyngoesophageal diagnoses, diseases of peristalsis, fistulae, and diverticula are still best evaluated radiographically.
Nasopharyngeal carcinoma is best staged with a combination of magnetic resonance imaging and PET-CT.
Advanced oropharyngeal and hypopharyngeal carcinomas are best staged with endoscopy and PET-CT.
It is important for referring otolaryngologists to understand the arsenal of tests offered by radiologists. The improved quality and availability of cross-sectional imaging, along with advances in endoscopic techniques, have resulted in major changes to the indications and techniques for fluoroscopic examinations. Nevertheless, many disorders of the pharynx and esophagus are still best evaluated with fluoroscopy. In particular, patients who have pain, trismus, a hyperactive gag reflex, or bulky disease are often not optimally evaluated with direct inspection or endoscopy, and mucosal lesions may not be evident on cross-sectional modalities. Furthermore, new fluoroscopic techniques and modalities can identify more subtle pathology than historical techniques could identify. This chapter discusses the basics of radiologic technique and anatomy with a focus on the appropriate choice of imaging modality for evaluation of the pharynx and esophagus. The radiologic appearance of specific disorders is also discussed.
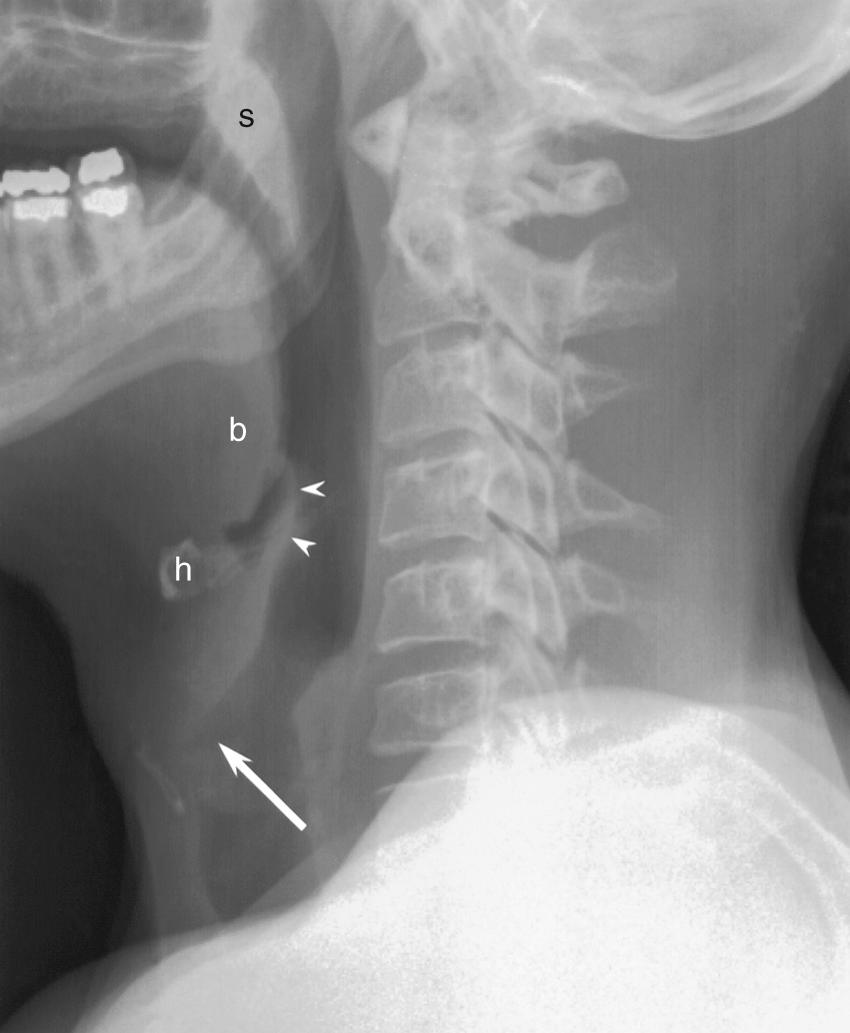
Conventional radiographs (plain films) of the neck are economical and readily available. They are particularly useful in pediatric patients with airway distress. The lateral projection provides the most information, and it will often be obtained without the frontal projection ( Fig. 100.1 ). If the examination is performed to evaluate a radiopaque foreign body, the frontal projection should be included. Patients are instructed to say the letter “e” during exposure to bring the tongue forward and better demonstrate the oropharynx. If a hypopharyngeal lesion is being evaluated, the patient should blow through compressed lips to distend the hypopharynx. In children, the lateral radiograph should be obtained during peak inspiration to prevent redundancy of the prevertebral soft tissues that may simulate pathology.
Chest radiographs occasionally reveal advanced esophageal abnormalities or pneumomediastinum, but fluoroscopy and cross-sectional imaging are preferred for evaluation of the thoracic esophagus.
Computed radiography and digital radiography have replaced traditional screen-film techniques. The newer modalities are advantageous because of the rapid processing and the ability to emphasize subtle soft tissue differences, even in suboptimally exposed images.
Xeroradiography and linear tomography are historical techniques that have been universally replaced by more advanced modalities.
Motion-capture techniques with intraluminal contrast are invaluable in studying the functional dynamics of the pharynx and esophagus. Although endoscopy provides direct visualization of the mucosa, radiographic techniques provide a more physiologic examination. Traditionally, fluoroscopic images were categorized as either cineradiography (high-resolution images obtained at a low frame rate) or video capture (low-resolution images obtained at a high frame rate). Cineradiography provides better spatial resolution for mucosal detail, whereas video capture allows more dynamic evaluation with less radiation. Modern picture archiving and communication systems allow review of cineradiography, but review of video capture is rarely available outside of the radiology department. Newer video capture technology, known as high temporal resolution fluoroscopy, allows for excellent spatial and temporal resolution, with frame rates up to 30 Hz. This requires a picture archiving and communication system (PACS) with extensive storage, and may not be available at some institutions. However, these techniques may allow for greater sensitivity for subtle pathology.
On traditional film, radiodense elements appear whiter than radiolucent elements. This convention has not persisted in the age of digital imaging, as some aspects of anatomy and pathology are visualized better when the image is inverted. The images in this chapter follow the traditional convention.
The term esophagogram is slowly replacing the ambiguous term barium swallow . Note that an esophagogram, which is designed to evaluate the pharyngeal and esophageal mucosa, is distinct from a modified barium swallow, which evaluates laryngotracheal aspiration and is usually performed in conjunction with a speech pathologist. At some institutions, an esophagogram includes a complete evaluation of the pharynx, but at other institutions, a cervical esophagogram, pharyngoesophagogram, or pharyngography must be specifically requested. Note that the nasopharynx is not evaluated with fluoroscopic techniques; cross-sectional imaging is required.
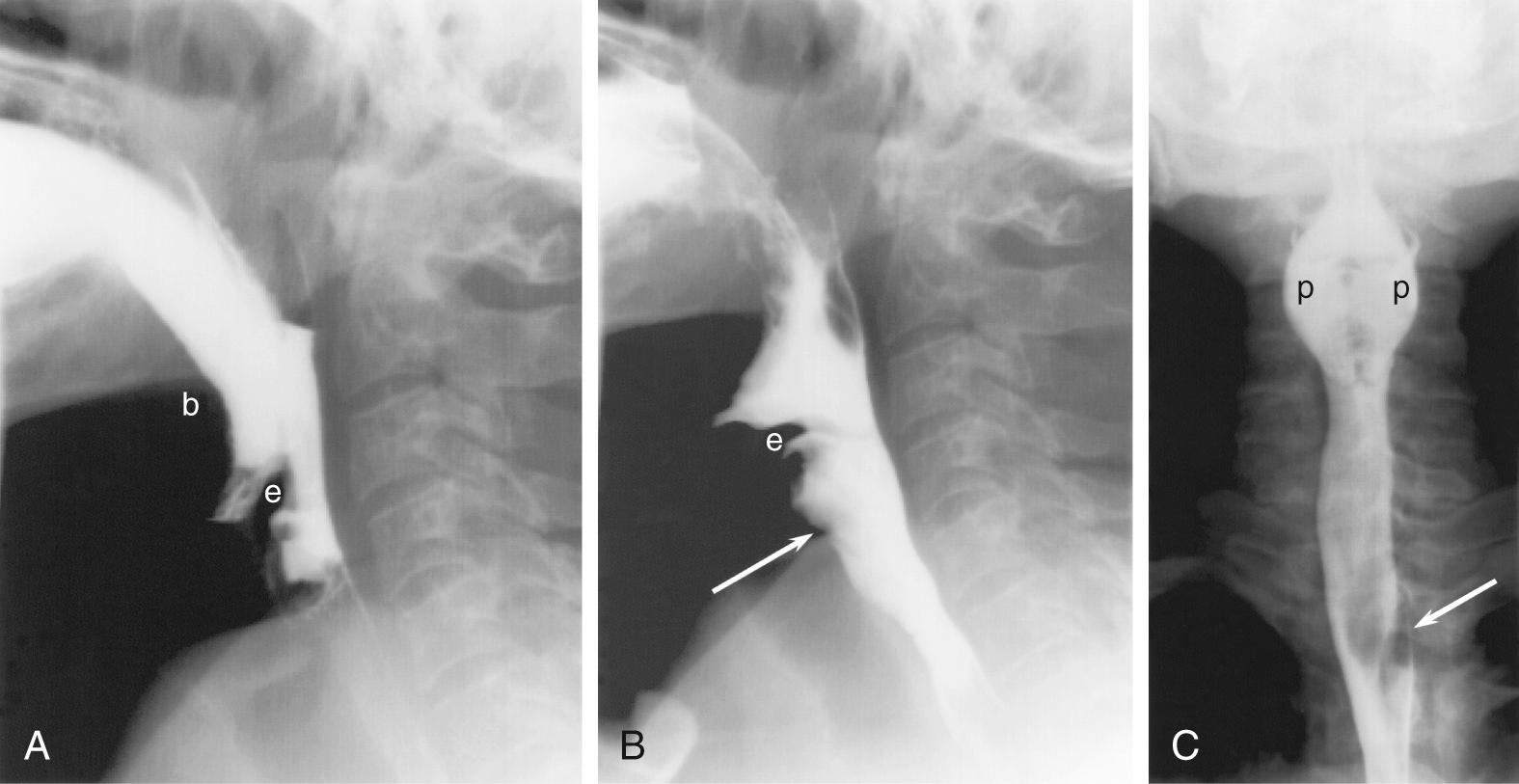
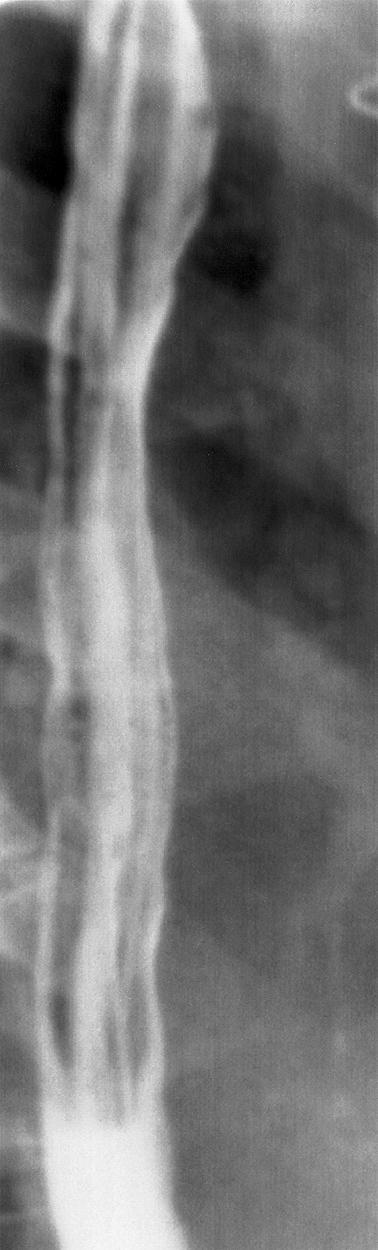
A traditional esophagogram has three phases: full-column (single contrast), air-contrast (double contrast), and mucosal relief. To obtain full-column images, the patient is given a thin suspension of barium by mouth. The pharynx is best imaged in the standing position, with rapid cineradiography (four to six images per second) in several projections ( Fig. 100.2 ). In the frontal projection, the patient's neck is extended to prevent the jaw from obscuring the pharynx. When digitally displayed, cine images reveal much of the swallowing dynamics. Video capture and high temporal resolution imaging are still useful, however, to evaluate equivocal filling defects. Full-column images of the esophagus ( Fig. 100.3 ) are obtained in a prone oblique position, with the patient drinking barium suspension from a straw. The two objectives of this portion of the examination are to evaluate esophageal peristalsis and maximally dilate the esophagus to identify contour abnormalities. Peristalsis is evaluated with videotaped single swallows, and maximum dilation is achieved with rapid swallows followed by a Valsalva maneuver. The prone position eliminates gravity as a factor in peristalsis.
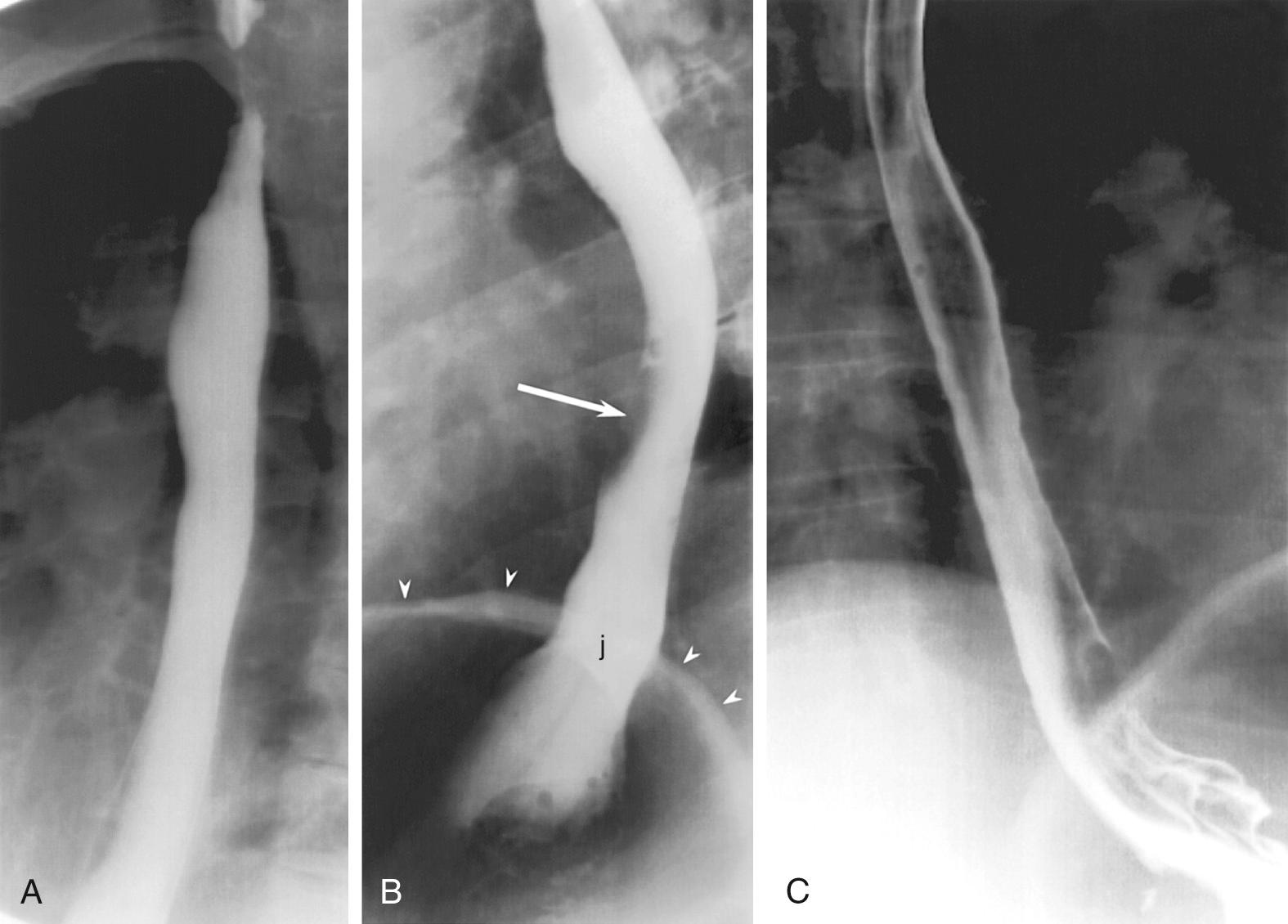
Air-contrast images of the esophagus (see Fig. 100.3 ) are obtained with the patient upright and in slightly left anterior obliquity. An effervescent agent is first administered, followed by a thick barium suspension. The barium coats the mucosal surface, whereas the gas from the effervescent agent distends the lumen. This provides exquisite mucosal detail and is most useful for the evaluation of small, plaque-like mucosal tumors and the mucosal irregularities of esophagitis. If the patient is unable to undergo the air-contrast portion of the thoracic esophagogram, prone full-column imaging should be obtained in two orthogonal planes as an alternative.
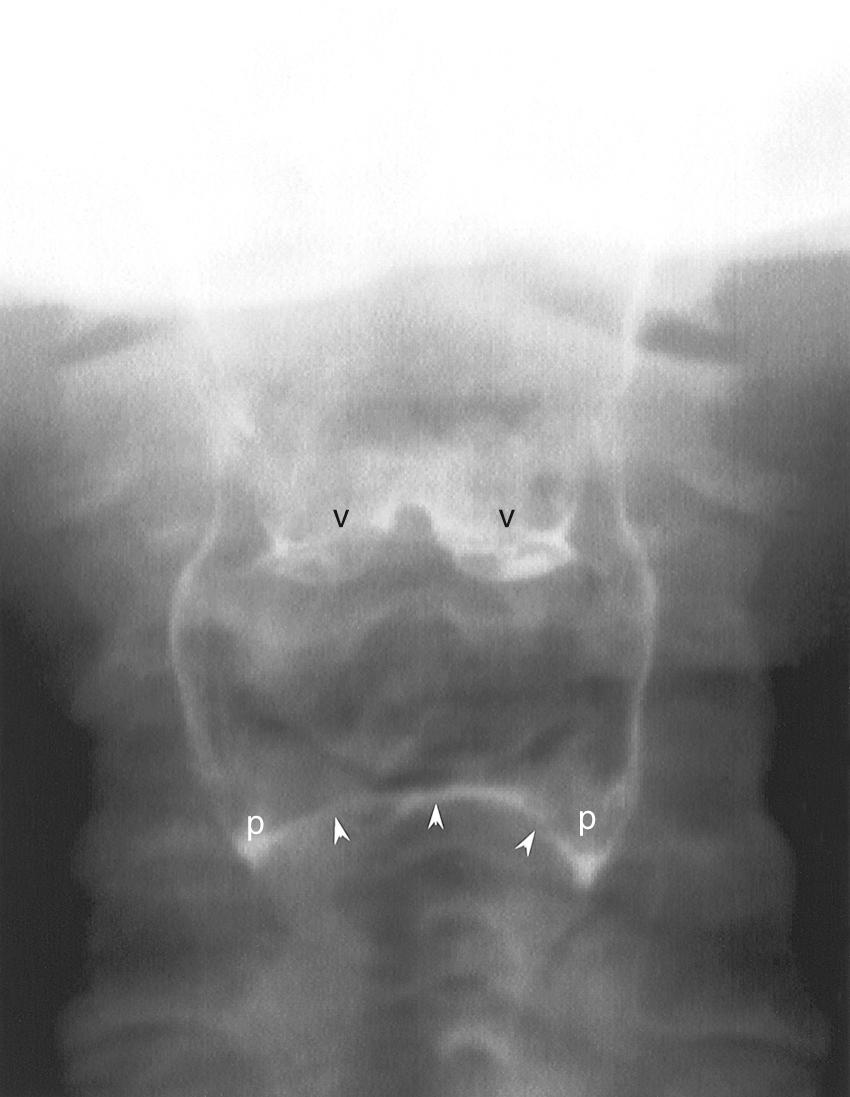
Air-contrast images of the pharynx are not always necessary because this region is amenable to endoscopic inspection. However, in some cases, such as with tumors that arise in the hypopharynx, air-contrast images are useful. After the administration of a thick barium suspension, phonation and a modified Valsalva maneuver are used to distend the pharynx ( Fig. 100.4 ).
Mucosal-relief images of the esophagus ( Fig. 100.5 ) are obtained after the administration of a thick barium suspension but without air distension. Esophageal varices and some mucosal lesions are best seen with mucosal relief. Only the distal esophagus and gastroesophageal junction need to be imaged in this phase of the examination.
At the conclusion of an esophagogram, after the esophagus has completely cleared all contrast, Valsalva and modified Valsalva maneuvers should be performed to document gastroesophageal reflux. It is important to realize, however, that these maneuvers are insensitive for the diagnosis of intermittent gastroesophageal reflux.
A modified barium swallow evaluates the coordination of the swallow reflex. It is most often used to determine a cause for, and evaluate the severity of, tracheal aspiration. A speech pathologist, using appropriate radiation safety precautions, administers oral barium suspensions while the radiologist observes fluoroscopically in the lateral projection. The entire examination is videotaped.
The patient is given barium suspension of several consistencies (e.g., thin liquid, thick liquid, paste, solid). The various barium suspensions are intended to mimic different food consistencies and provide a more complete assessment of aspiration risk. If tracheal aspiration or laryngeal penetration is identified with the head in a neutral position, the speech pathologist may direct the patient to perform protective maneuvers during deglutition. Such maneuvers include varying the head position (chin tuck, neck turn) and postprandial forced cough. The examination can be supplemented with images in the frontal projection to evaluate symmetry of the piriform sinuses.
Aspiration of barium suspension is dangerous because the barium may concrete within the lungs. Thus, the radiologist may need to terminate a modified barium swallow (MBS) before all of the desired consistencies are tested. If a patient aspirates more than 10% of a bolus, they are considered high risk. The patient may be subjected to an additional swallow to test protective maneuvers or a different consistency, but the test should be concluded prematurely for the patient's protection.
Many of the pathologies that were historically evaluated with fluoroscopy are now evaluated with endoscopic techniques. The role of the esophagogram has thus changed, with a greater emphasis on physiologic evaluation, and less emphasis on anatomic findings. Air-contrast and mucosal-relief images, which are used exclusively to evaluate mucosal lesions, are not a routine part of a modern esophagogram, although they may still be used in particular patients. This allows more time to be spent on dysphagia assessment.
Patients with dysphagia may have critical findings on either esophagography or MBS. Unfortunately, many insurers will not pay for both of these procedures. This has given rise to combined examinations that use elements of esophagograms and MBS and are tailored to individual patients. By incorporating a brief assessment of aspiration and a more complete assessment of swallowing physiology, the most important results from both esophagograms and MBS can be achieved in a single examination.
Critical to the success of these combined studies is a multidisciplinary approach with input from otolaryngologists, radiologists, and speech pathologists, consulting together to modify the procedure to the needs of the individual patient.
Barium suspension is the best-known fluoroscopic contrast agent, but some patients are not appropriate candidates for oral barium administration. Patients who may have a perforated pharynx or esophagus are at risk for barium extravasation into the soft tissues of the neck or chest. Extravasated barium may incite an inflammatory reaction or may become inspissated and fail to resorb. Water-soluble contrast agents, such as those used for intravenous (IV) contrast computed tomography (CT), may be used as an alternative. Unfortunately, water-soluble agents are not as dense as the barium suspension, so they are less sensitive to small leaks. If no leak is detected after the administration of a water-soluble agent, the examination should be repeated with barium.
Ionic contrast agents have another disadvantage: if they are aspirated into the lungs, they may cause a chemical pneumonitis and pulmonary edema. Nonionic water-soluble agents are presumed to be safer and thus should be used if risk of aspiration or tracheoesophageal fistula is present.
Oil-based contrast agents for the evaluation of the larynx and pharynx are of historic interest only.
At most institutions, CT is the modality of choice for evaluating masses in the neck and chest. All modern CT scanners use helical scanning modes, have multiple detector channels (multiple detector CT [MDCT]), and scanners with 64 or 128 detector channels are commonplace. The high resolution of MDCT allows multiplanar and three-dimensional re-formations that are useful for envisioning pathology in any anatomic orientation. Rapid scan times permit dynamic CT imaging, which can assess vascularity and other physiologic properties.
CT is readily available and provides critical information about the extent and character of mass lesions. In known tumors, CT is used to determine the degree of invasion into surrounding deep tissues, the relationship of the neoplasm to critical structures such as the vocal cords and arteries, and the involvement of regional lymph nodes. CT is comparable to magnetic resonance imaging (MRI) for the evaluation of bone invasion, but MRI is preferred for the evaluation of soft tissue extent, particularly at the skull base. Disadvantages of CT include artifacts from dental amalgam and from patient body habitus, particularly at the shoulders.
IV contrast is of particular importance in the neck because enlarged lymph nodes may be difficult to distinguish from surrounding structures. Renal dysfunction and allergies to contrast material are relative contraindications to IV contrast. Some practitioners avoid IV contrast in patients who may require radioablation of thyroid neoplasms because the contrast can impede iodine uptake for an indeterminate amount of time after the examination.
Ionic contrast media are more prone to allergic reactions than the more expensive nonionic media. For this reason, some institutions have abandoned ionic contrast media. Ionic contrast should be avoided in patients with airway pathology because a mild allergic reaction could precipitate severe airway compromise.
Helical neck CT should be performed with a maximum slice thickness of 3 mm. Thinner slices may be required to delineate the extent of pathology, particularly in tumors near the larynx. A contrast bolus of 75 to 125 mL is used, with a delay of 45 to 90 seconds. Faster scanners require longer contrast delays, so revised protocols are required when equipment is upgraded. Failure to do so will result in CT examinations with angiographic timing, such that the ability to distinguish tumor from underlying soft tissues will be lost.
CT of the chest is performed with a thickness of 5 to 7 mm; additional IV contrast is usually not required. CT of the neck and chest should not be performed as a continuous acquisition because the arms are positioned differently for the two scans.
Unlike CT, which relies on ionizing radiation to create images, MRI uses a strong magnetic field and radiofrequency pulses to interrogate the patient's tissues. It is particularly useful for evaluating tumors of the skull base, oral cavity, and larynx, but it is less useful in the thorax, where motion artifact and field distortions prevent a thorough evaluation of the mediastinum.
MRI has the substantial advantage of multiple pulse sequences, which allows more precise characterization of pathologic tissue. The most frequently used sequences are T1-weighted and T2-weighted sequences. Postcontrast images are usually T1-weighted sequences, which demonstrate anatomic relationships, whereas T2-weighted images are sensitive for pathology. Many additional sequences and modifications—such as inversion recovery, fat suppression, magnetization transfer, and diffusion weighting—can more precisely determine tissue characteristics and extent of pathology.
Advantages of MRI include reduced artifacts from dental amalgam and body habitus and the ability to directly image in any plane, including oblique planes. The gadolinium-based IV contrast agents used in MRI have a substantially lower risk of allergic reaction than CT agents do. However, gadolinium contrast agents have been implicated in nephrogenic systemic fibrosis, a severe illness seen in patients with renal disease who receive contrast for MRI. Thus gadolinium-based contrast agents are used conservatively in patients with renal dysfunction.
Disadvantages of MRI include the long duration of MRI studies, which sometimes results in motion artifact, especially in debilitated patients or in patients with respiratory compromise. The small bore of the MRI magnet often induces claustrophobia. Many patients cannot go near the MRI magnet because of metallic or electronic implants that might be displaced or triggered by the rapid changes in the magnetic field. In particular, cardiac pacemakers/defibrillators, cochlear implants, and ferromagnetic aneurysm clips are relative contraindications to MRI, although newer devices are often MR-compatible. Metallic foreign bodies may also be of concern, depending on their location. Each institution should have protocols in place for metal screening prior to MRI.
Different receiving coils are available for MRI, with characteristics tailored to different body parts. It is critical for head and neck patients to be imaged with a surface coil, which allows for improved spatial resolution and higher signal-to-noise ratios. Low-field-strength “open” MRI magnets do not have the spatial resolution or signal-to-noise characteristics to evaluate the intricate anatomy of the skull base or larynx and are not recommended for imaging of the head and neck.
Transcutaneous sonographic evaluation of the neck has undergone a resurgence in popularity in patients with thyroid cancer and for guidance in interventional procedures. Although ultrasound can be used to evaluate superficial lymph nodes in the neck, it may overlook deep nodes and cannot be relied on for a complete evaluation of cervical tissues. Transesophageal echosonography provides information that is complementary to CT and invaluable for the evaluation of the extent of esophageal lesions across tissue planes. All sonographic techniques are highly operator dependent, so experienced technologists and appropriately trained physicians are necessary to produce diagnostic-quality examinations.
Combined 18 F-fluorodeoxyglucose (FDG) positron emission tomography and CT scanning (PET-CT) has revolutionized the care of head and neck cancer patients. PET is a functional imaging technique that relies on the increased metabolic uptake of glucose in tumors to identify unknown primary tumors, stage malignancies, search for metastatic disease, and evaluate recurrences. The major limitation of PET imaging is its poor spatial resolution, which is particularly significant in the head and neck. Combined PET-CT scanners use the high spatial resolution of CT with the functional information of PET to produce fused images that overcome this difficulty ( Fig. 100.6 ). For the evaluation of head and neck cancers, PET-CT is superior to either PET or CT alone. However, this advantage relies on performing contrast-enhanced CT as part of the PET-CT examination, rather than attenuation-only CT, which is not of diagnostic quality.
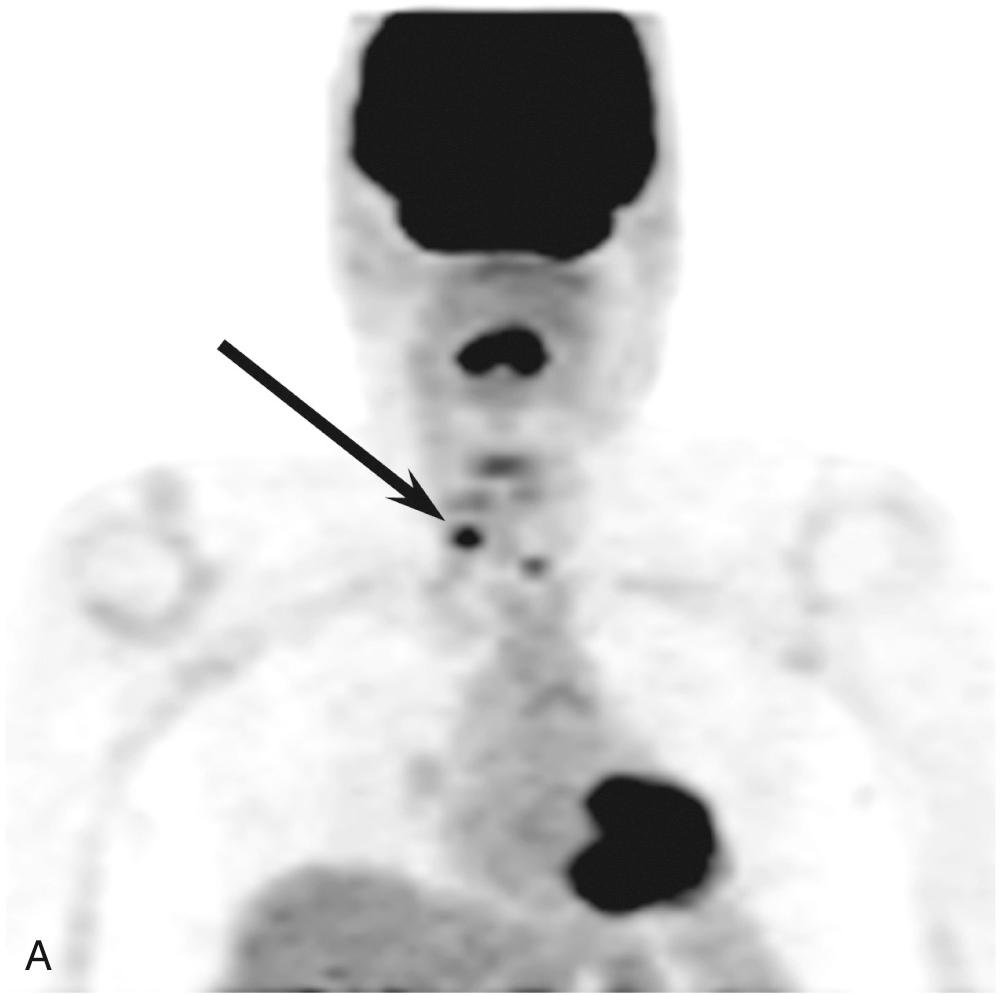
PET-CT is used in the staging of cancer, the monitoring of treatment response, and the surveillance of treated patients. Optimal monitoring and surveillance schemata have not yet been established, but it is known that PET-CT should not be performed until at least 8 weeks after the conclusion of therapy to avoid both false-positive and false-negative results. Surveillance with PET-CT is particularly useful because of the low rate of false-negative studies.
The analysis of PET-CT scans is complicated and requires a radiologist with experience in both PET-CT and head and neck imaging. Physiologic uptake of FDG is prevalent in the head and neck, especially during contraction of muscles (e.g., neck and thyroarytenoid muscles), and it may therefore be confused with tumor uptake. Inflammation—either postoperative or from infectious sources such as the teeth, salivary glands, or tonsils—may also obscure interpretation and can result in false-positive reads and unnecessary additional evaluations and biopsies.
Radioligands other than FDG are useful for some histologies other than squamous cell carcinoma. For example, gallium 68 dotatate is used to evaluate neuroendocrine tumors.
Future trends in PET-CT include combined positron emission tomography–magnetic resonance (PET-MR) scanners, the development of novel ligands to supplement or replace FDG, and guidelines for optimizing the use of this modality.
Although PET-CT is the most commonly used nuclear medicine examination in the head and neck, other nuclear medicine tests are sometimes useful. Esophageal transit, gastroesophageal reflux, and gastric emptying can be studied with conventional nuclear medicine techniques. These studies are more sensitive than fluoroscopy for the presence of reflux, but the quantitative degree of reflux does not correlate well with symptoms. Radionuclide swallowing studies are used predominantly in the pediatric population.
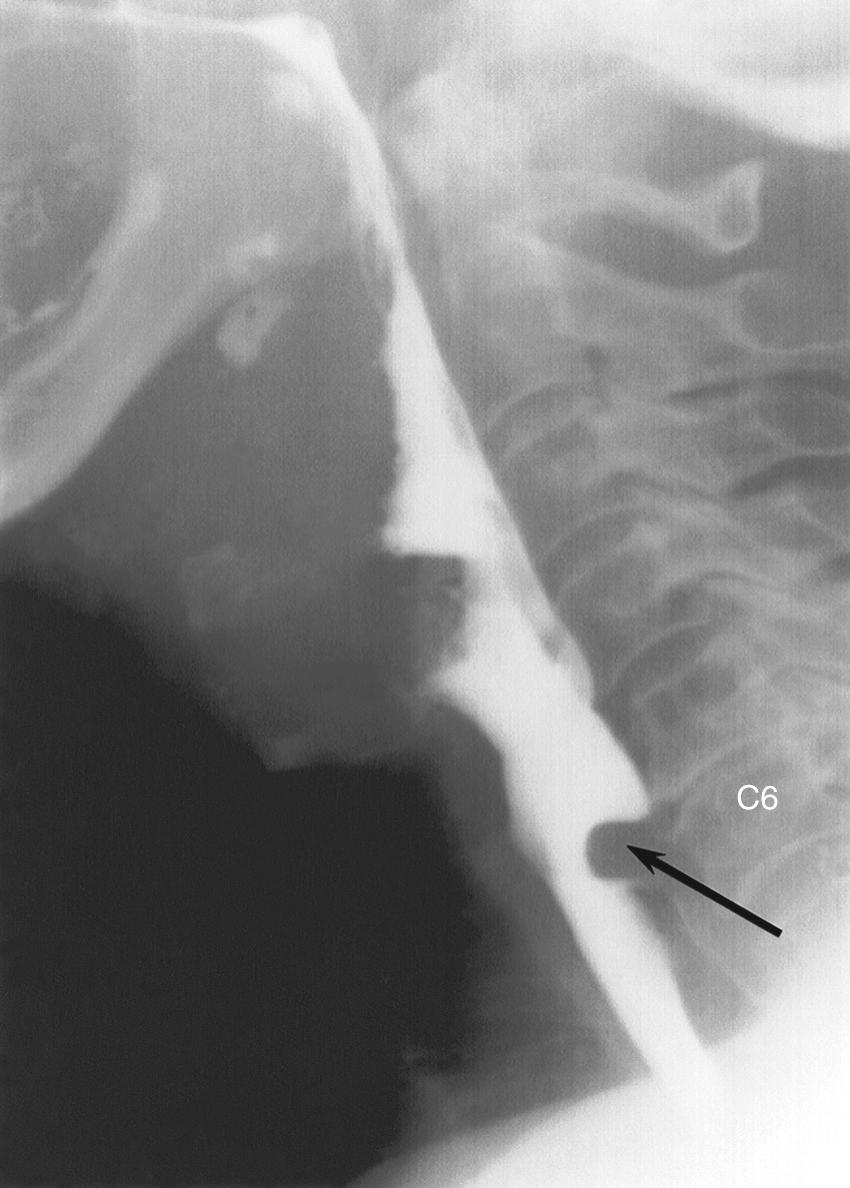
The radiographic anatomy of the pharyngeal lumen is best visualized with air-contrast fluoroscopic images (see Fig. 100.4 ). The mucosal surfaces of the epiglottis, valleculae, and piriform sinuses are easily identified. Normal asymmetry of the lingual tonsils should not be confused with a vallecular mass. The epiglottis is best evaluated in the lateral projection, which allows direct assessment of its thickness. The piriform sinuses may be asymmetric, but a complete lack of filling is suspicious for tumor. Barium pooled between the posterior margin of the larynx and the posterior wall of the hypopharynx forms the postcricoid line (see Fig. 102.4); disruption or irregularity of this line is a sign of tumor invasion. The cricopharyngeus muscle lies anterior to the sixth cervical vertebra. It may be seen as a slight indentation on the posterior wall of the hypopharynx, but it is often not visualized in normal individuals. The normal cross-sectional anatomy of the upper aerodigestive tract is demonstrated in Figs. 100.7 and 100.8 .
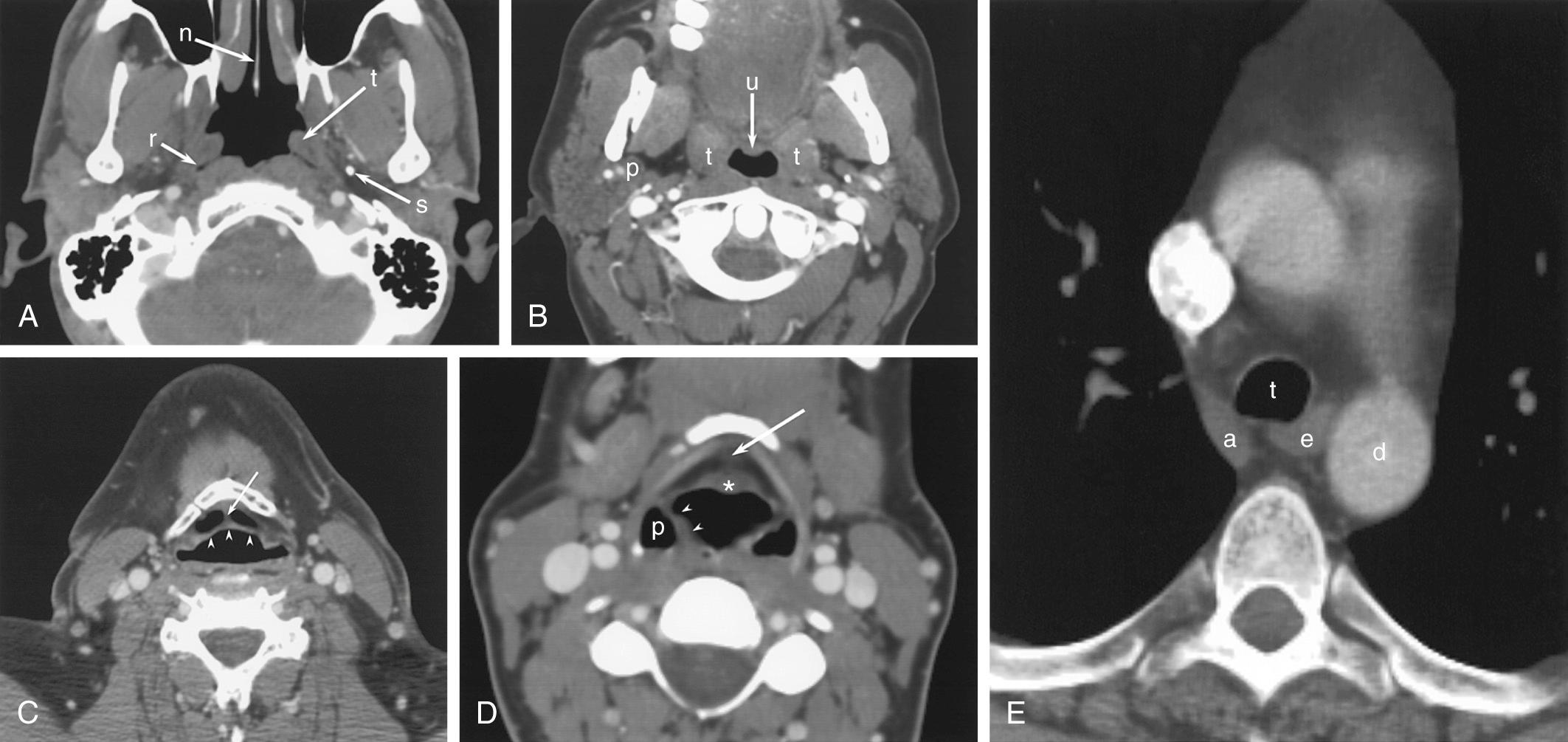
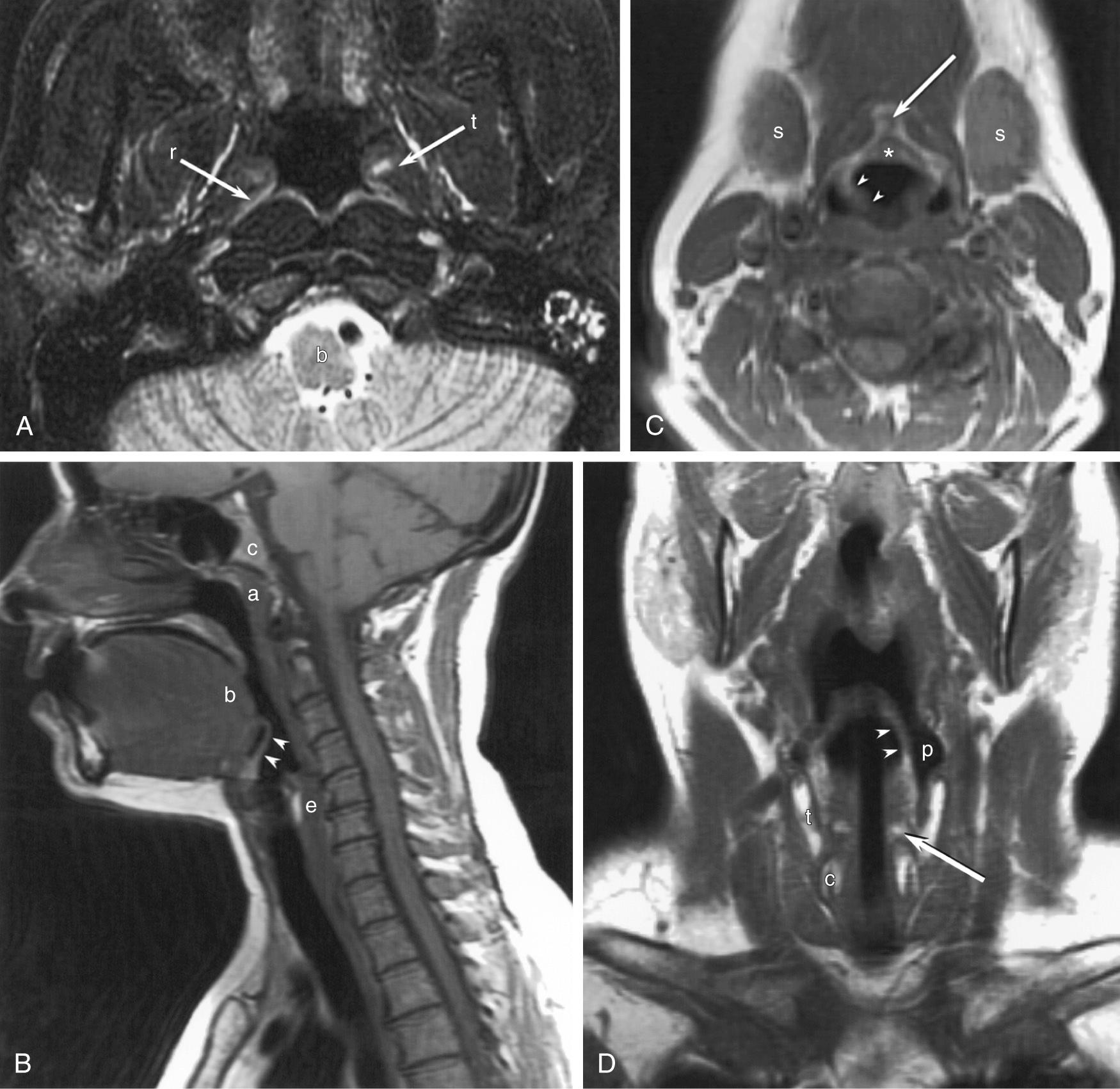
The esophagus begins at the level of the sixth cervical vertebra. The cervical esophagus lies posterior to and slightly to the left of, the trachea (see Fig. 100.7 ). Surrounding structures that may affect the cervical esophagus include the trachea, cervical spine, thyroid and parathyroid glands, and cervical lymph nodes. On CT, the anteroposterior diameter of the collapsed cervical esophagus should not exceed 16 mm, and its lateral dimension should not exceed 24 mm, except at the esophageal verge, where it may be slightly larger. On full-column lateral projections, a normal mucosal irregularity of the anterior esophagus is apparent just below the cricoid cartilage (see Fig. 100.2 ); this is caused by lax mucosal folds that overlie the ventral submucosal venous plexus, and it should not be mistaken for tumor invasion or a web. The venous plexus may change shape during swallowing.
The thoracic esophagus lies anterior to the spine, anteromedial to the descending aorta (see Fig. 100.7 ). The phrenic ampulla, which is a normal widening of the esophageal lumen, is seen just above the gastroesophageal junction ( Fig. 100.9 ). Three normal indentations found on the anterolateral esophagus are the (1) aortic arch, (2) left mainstem bronchus, and (3) left atrium (see Fig. 100.3 ). Other nearby structures include the descending aorta, aortic arch and great vessels, carina, mediastinal lymph nodes, and spine.

When the esophagus is filled with contrast, it is a featureless tube. When the esophagus is collapsed, longitudinal mucosal folds appear along the entire length of the organ; occasional transverse folds are normal.
The modified barium swallow is the most appropriate radiologic test to evaluate swallowing dysfunction. Although an esophagogram provides some information about deglutition, the modified swallow uses barium of several different consistencies, which provides a more detailed evaluation. Functional endoscopic evaluation of swallowing, with or without sensory testing, has been proposed as an alternative to the modified swallow. However, the modified swallow provides a more physiologic environment because no endoscope is present to interfere with motility. During a modified swallow, patients can use protective maneuvers such as a chin tuck and forced cough, which are not available during endoscopy. Furthermore, the modified swallow evaluates the upper phases of swallowing in more detail. Endoscopy and modified swallow are considered complementary examinations at most institutions.
The modified barium swallow can evaluate all phases of the swallow reflex. The tongue forms the oral bolus and then transports it from the oral cavity to the oropharynx. The soft palate elevates and approximates the posterior pharynx to prevent velopharyngeal reflux. The entire larynx elevates, followed by a peristaltic wave through the pharynx. The epiglottis inverts to deflect the bolus into the piriform sinuses and protect the laryngeal vestibule. At the bottom of the hypopharynx, the cricopharyngeus muscle relaxes to permit the passage of the food bolus.
Velopharyngeal occlusion can be observed directly. Elevation of the larynx is best visualized by observing the hyoid bone. Epiglottic inversion is fast, and confirmation of this event may require review of the video images. Brief episodes of contrast penetration may be seen in the laryngeal vestibule. If the contrast clears rapidly and without cough, this finding of “flash penetration” does not indicate a risk of tracheal aspiration. A small amount of barium may pool in the valleculae or the piriform sinuses in normal patients, but the peristaltic wave should strip the contrast from the remainder of the pharynx. At rest, the cricopharyngeus muscle lies at the level of the C6 vertebral body, but the muscle elevates along with the rest of the pharynx during deglutition. Because the muscle relaxes to allow passage of the contrast bolus, it is not normally visualized.
Aspiration can occur in any phase of deglutition and is classified as preprandial, prandial, or postprandial based on its relationship to the swallow reflex. During the oral phase (preprandial) , incomplete control of the oral bolus allows contrast to spill over the base of the tongue into the vallecula. In severe cases, the vallecula will fill completely, and contrast will spill over the epiglottis into the larynx. During peristalsis (prandial) , failure of epiglottic inversion allows contrast to enter the larynx. After the swallow (postprandial) , incomplete clearance of contrast leads to aspiration when the patient resumes breathing.
Abnormal pharyngeal motility is caused by disorders of (1) the brainstem, (2) cranial nerves IX and X, (3) the myoneural junction, or (4) the pharyngeal musculature. Myasthenia gravis is a disorder of the myoneural junction that produces hesitancy in swallow initiation, nasopharyngeal reflux, enlargement of the pharynx, tracheal aspiration, and incomplete clearance. The findings worsen over consecutive swallows and improve after neostigmine administration. Diseases that affect the pharyngeal muscles—such as dermatomyositis, systemic lupus erythematosus, myotonic dystrophy, systemic sclerosis, and oculopharyngeal myopathy—produce weakened pharyngeal contractility with incomplete clearance.
Unilateral pharyngeal palsy causes an asymmetry in the piriform sinuses because the contrast is thrown to the palsied side by the functioning pharyngeal constrictors. This asymmetry should not be misinterpreted as a filling defect from carcinoma in the unaffected side. A careful dynamic examination of several swallows may be necessary to prevent this diagnostic error.
Unlike the other muscles of pharyngeal constriction, the cricopharyngeus remains contracted between swallows and acts as an upper esophageal sphincter. It normally relaxes during deglutition to allow the passage of the food bolus. When the muscle fails to completely relax (cricopharyngeal achalasia), a smooth posterior impression is seen on the hypopharynx at the level of the C6 vertebra ( Fig. 100.10 ). Unlike most retropharyngeal masses, the cricopharyngeus does not exceed 1 cm in vertical dimension. The most frequent cause of cricopharyngeal achalasia is cerebrovascular disease. Other causes include pseudobulbar palsy, nasopharyngeal carcinoma, poliomyelitis, thyroid myopathy, cervical vagotomy, polymyositis, dermatomyositis, oculopharyngeal syndrome, amyotrophic lateral sclerosis, and hiatus hernia, but many cases are idiopathic. Cricopharyngeal achalasia has been implicated in the development of Zenker diverticula. Although cricopharyngeal dysphagia is generally considered to be a bilateral disease, unilateral forms are rarely seen and are best evaluated fluoroscopically.
Incompetence of the upper esophageal sphincter is called cricopharyngeal chalasia . It manifests radiographically as a lack of cricopharyngeal impression between swallows. Cricopharyngeal chalasia is specific for myotonic dystrophy, although most patients with myotonic dystrophy have cricopharyngeal achalasia instead.
Delayed opening of the cricopharyngeus, seen in familial dysautonomia, results in aspiration and recurrent pulmonary infections. This disorder is distinct from cricopharyngeal achalasia in that the muscle relaxes completely after a delay.
Manometry is considered the reference standard for evaluation of esophageal dysmotility. The relative sensitivity of fluoroscopy, radionuclide scans, and manometry is controversial. However, radiologic techniques are less invasive and elicit less patient discomfort. Fluoroscopy has the additional advantage of identifying structural abnormalities.
A normal (primary) peristaltic wave is initiated by a swallow, and the wave passes uninterrupted to the lower esophageal sphincter (LES). The contrast bolus should remain intact during a primary wave; contrast that escapes proximally is the earliest sign of weakened peristalsis. Secondary peristaltic waves are initiated in the mid esophagus by local irritation such as from gastroesophageal reflux (GER) or retained food. Tertiary contractions are nonperistaltic local contractions, a contributing factor in dysmotility.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here