Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Before the advent of cardiopulmonary bypass in the mid-1950s, little attention was given to the diagnosis of congenital heart disease (CHD) because no effective treatment was available. Physical examination, auscultation, electrocardiography, and radiography were the main diagnostic tools. Progress in open-heart techniques for repair of CHD required accurate and comprehensive delineation of cardiovascular anatomy and function. During the 1960s and 1970s, cardiac catheterization and angiography were the principal tools used to diagnose CHD. Echocardiography entered the arena in the late 1970s. The diagnostic capability of M-mode echocardiography proved insufficient in patients with CHD, but the rapid evolution of two-dimensional echocardiography during the following decade transformed the field. The technologic advances in transducer design, image processing, and image display—together with development and refinement of new imaging planes and examination techniques—allowed high-quality tomographic visualization of most cardiac defects. The application of Doppler ultrasound to investigate blood flow allowed comprehensive hemodynamic assessment. By the mid-1980s, much of the necessary anatomic and hemodynamic information required for patient management could be obtained noninvasively, obviating the need for a diagnostic catheterization in many patients. During the late 1990s and into the 2000s, the field of pediatric cardiac imaging experienced accelerated progress in areas such as three-dimensional echocardiography, sophisticated techniques for assessment of myocardial function, and the application of magnetic resonance imaging (MRI) to CHD. At the same time, the proportion of cardiac catheterization procedures performed solely for diagnostic purposes has drastically declined. More recently, the role of multimodality cardiac imaging for preintervention planning and for guidance of cardiovascular procedures has expanded dramatically.
This chapter discusses the clinical application of the two main noninvasive diagnostic imaging modalities used for anatomic and physiologic evaluation of preoperative and postoperative CHD: echocardiography and cardiovascular MRI.
Echocardiography is an ideal diagnostic tool in pediatric cardiology because of its noninvasive nature, relatively low cost, superb spatial and temporal resolutions, and ability to image cardiovascular anatomy and to evaluate physiology in real time. In addition, modern cardiac ultrasound equipment is portable and adaptable to different environments, such as the operating room, intensive care unit, at the bedside, and in an outpatient office setting. In today's pediatric cardiology practice, echocardiography is the primary diagnostic modality used to evaluate anatomy and physiology preoperatively, intraoperatively, postoperatively, during follow-up of CHD, and prenatally.
To obtain an echocardiographic image, a burst of ultrasound energy is generated by a piezoelectric crystal and travels through the soft tissue at an average speed of approximately 1540 m/sec. When the propagating ultrasound wave encounters an interface between tissues with different acoustic properties, some of the energy is reflected back toward the transducer and some of the energy is refracted and continues to travel in the medium until it encounters the next interface. The returning ultrasound energy is captured by the piezoelectric crystal and converted into an electrical energy that goes through a series of electronic processes, including amplification, filtering, postprocessing, and display.
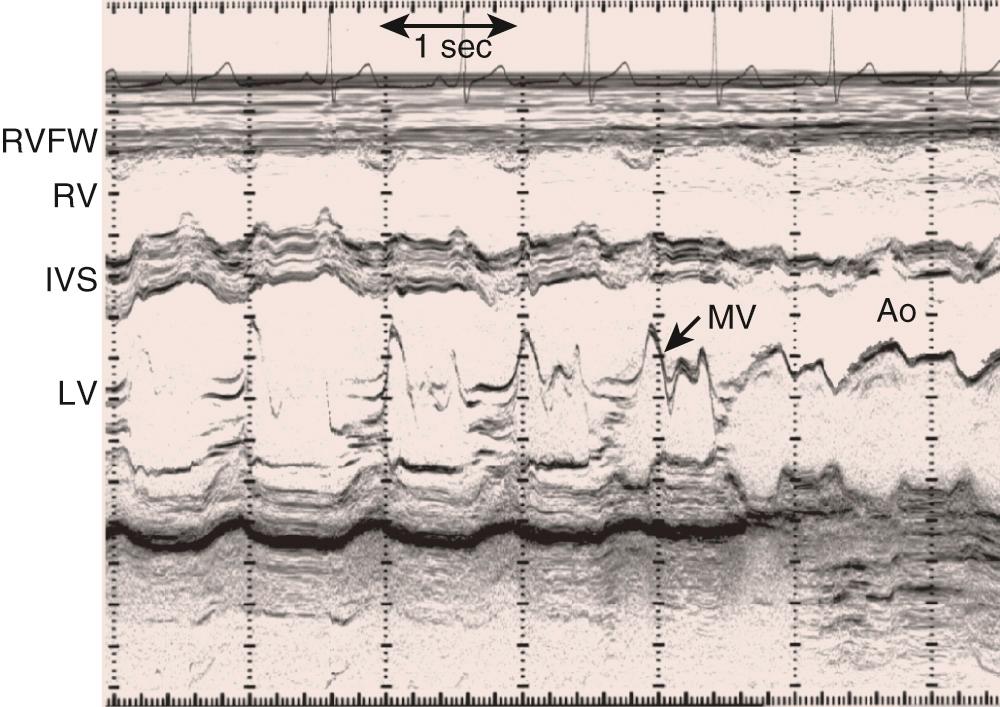
A narrow beam of ultrasound energy is emitted toward the heart, and structures along the beam path reflect echoes back toward the transducer. A dot is displayed on the screen in a position corresponding to its distance from the transducer. This process is repeated rapidly to create an image. The distance from the transducer is displayed on the y -axis and time is displayed on the x -axis ( Fig. 106-1 ). This provides an anatomically one-dimensional image of the heart that is characterized by excellent temporal and axial resolutions. In today's clinical pediatric echocardiography, two-dimensional imaging has replaced M-mode for anatomic imaging of the heart and for assessment of ventricular size and function. In selected circumstances, when superior temporal resolution is required, two-dimensional directed M-mode is used to assess motion of specific structures such as native and prosthetic valve leaflets.
By rapidly sweeping an ultrasound beam through an arc, multiple “M-mode lines” are placed next to each other to construct a cross-sectional two-dimensional image of the heart ( Fig. 106-2 ). This can be accomplished by electronically sweeping the sound beam through multiple piezoelectric crystals (transducer elements), as in phased array transducers. Recent advances in transducer technology and image processing permit very high frame rates (>200 Hz), a feature that greatly enhances temporal resolution.
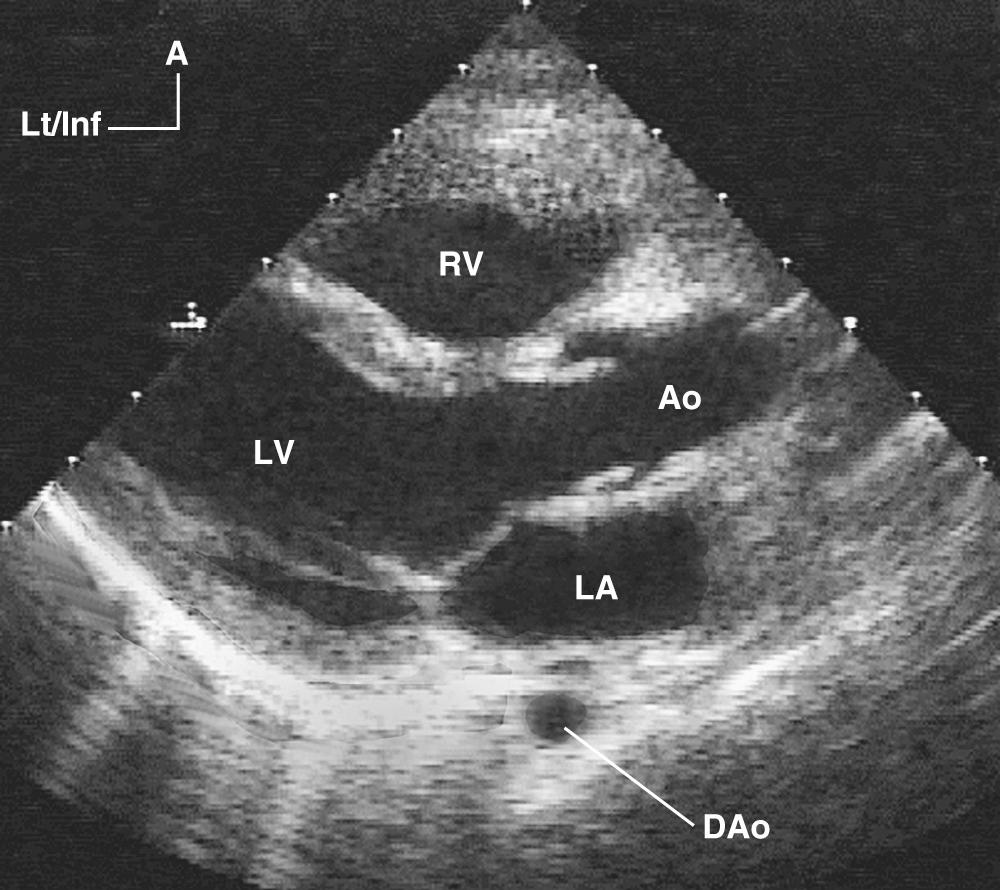
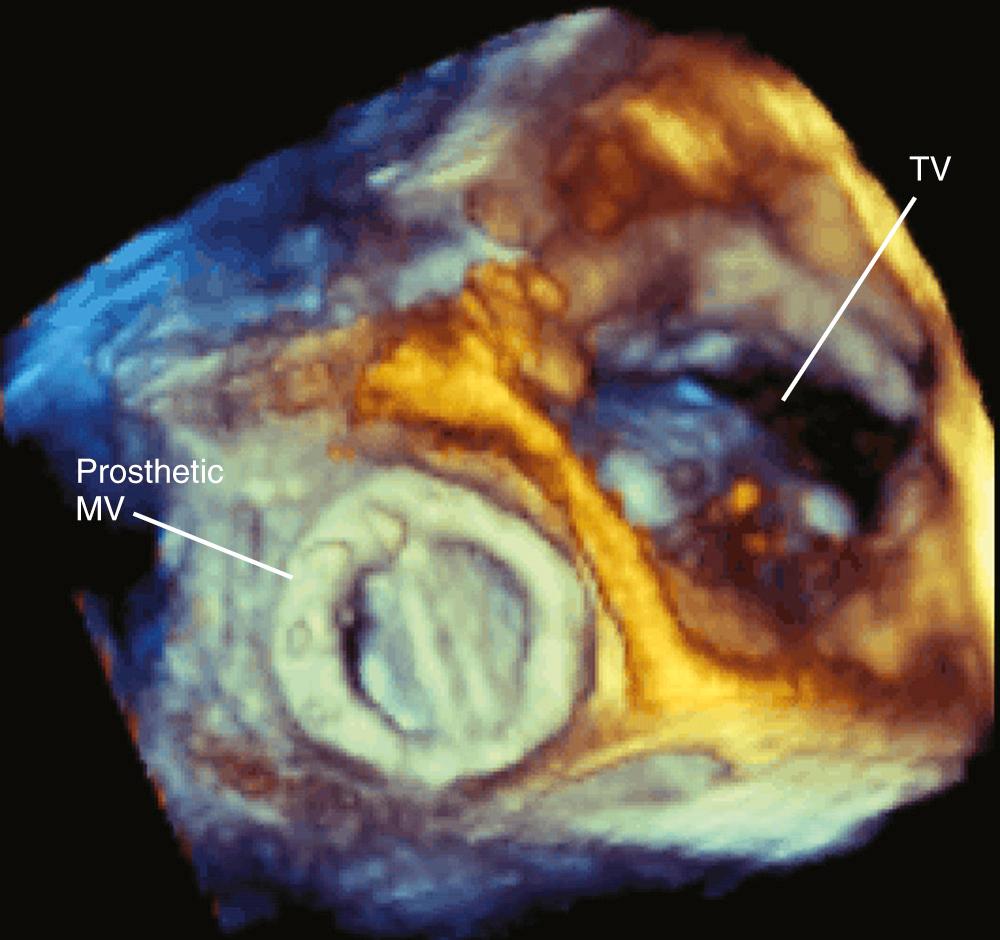
Accurate spatial perception of an object depends on recognition of its three dimensions: length, width, and depth. Although an experienced examiner can mentally construct a three-dimensional image of the heart from serial two-dimensional tomographic images obtained by sweeping the transducer across the heart, three-dimensional echocardiography offers enhanced perspective of cardiovascular structures and their interrelations. Previous approaches to obtaining three-dimensional echocardiographic images of the heart were based on computer reconstruction of contiguous two-dimensional cross-sectional images. These efforts were hampered by difficulties in accurately registering the ultrasound image data in time and space and by long processing times. Currently, three-dimensional images are generated by real-time three-dimensional echocardiography. This technology, which is based on a new generation of matrix array transducers with several thousands of simultaneously transmitting and receiving piezoelectric elements and sophisticated parallel data processing, provides real-time three-dimensional images with sufficient temporal resolution to display in cine-loop format ( Fig. 106-3 ). More recently, miniaturization of matrix array transducer technology has allowed development of a real-time three-dimensional transesophageal echocardiographic probe. Further refinements of this technology will result in continued improvement of spatial and temporal resolutions as well as better, more intuitive, user interface. Such advances will likely contribute to the ongoing acceptance of this technology in routine practice.
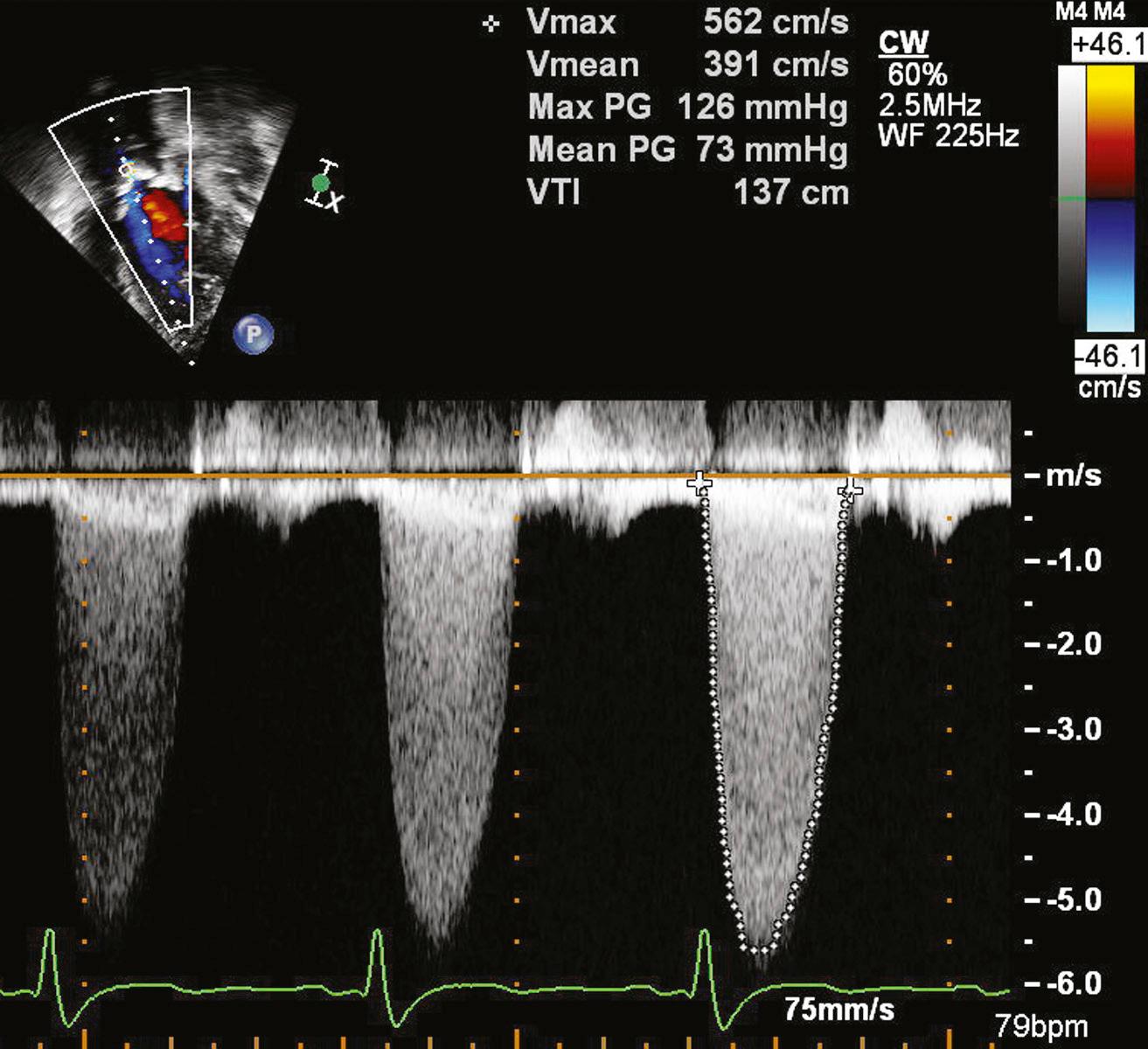
The use of Doppler ultrasound to assess normal and abnormal hemodynamics has become an integral part of the echocardiographic examination. The advent of two-dimensional directed Doppler interrogation has greatly enhanced the clinical application of this technique by allowing evaluation of flow characteristics in specific regions within the heart and great vessels. In today's echocardiography, spectral and color-coded Doppler flow mapping are used extensively to measure velocity and direction of blood flow ( Fig. 106-4 ). Calculations based on Doppler-derived measurements allow quantitative estimation of flow volume (such as cardiac output), pressure gradient across a stenotic region, cross-sectional flow area, and prediction of intracardiac pressures. Doppler echocardiography also provides qualitative and semiquantitative assessment of valve regurgitation, intra- and extracardiac shunts, as well as myocardial motion (tissue Doppler imaging). Detailed discussion of Doppler physics is beyond the scope of this text and can be found elsewhere.
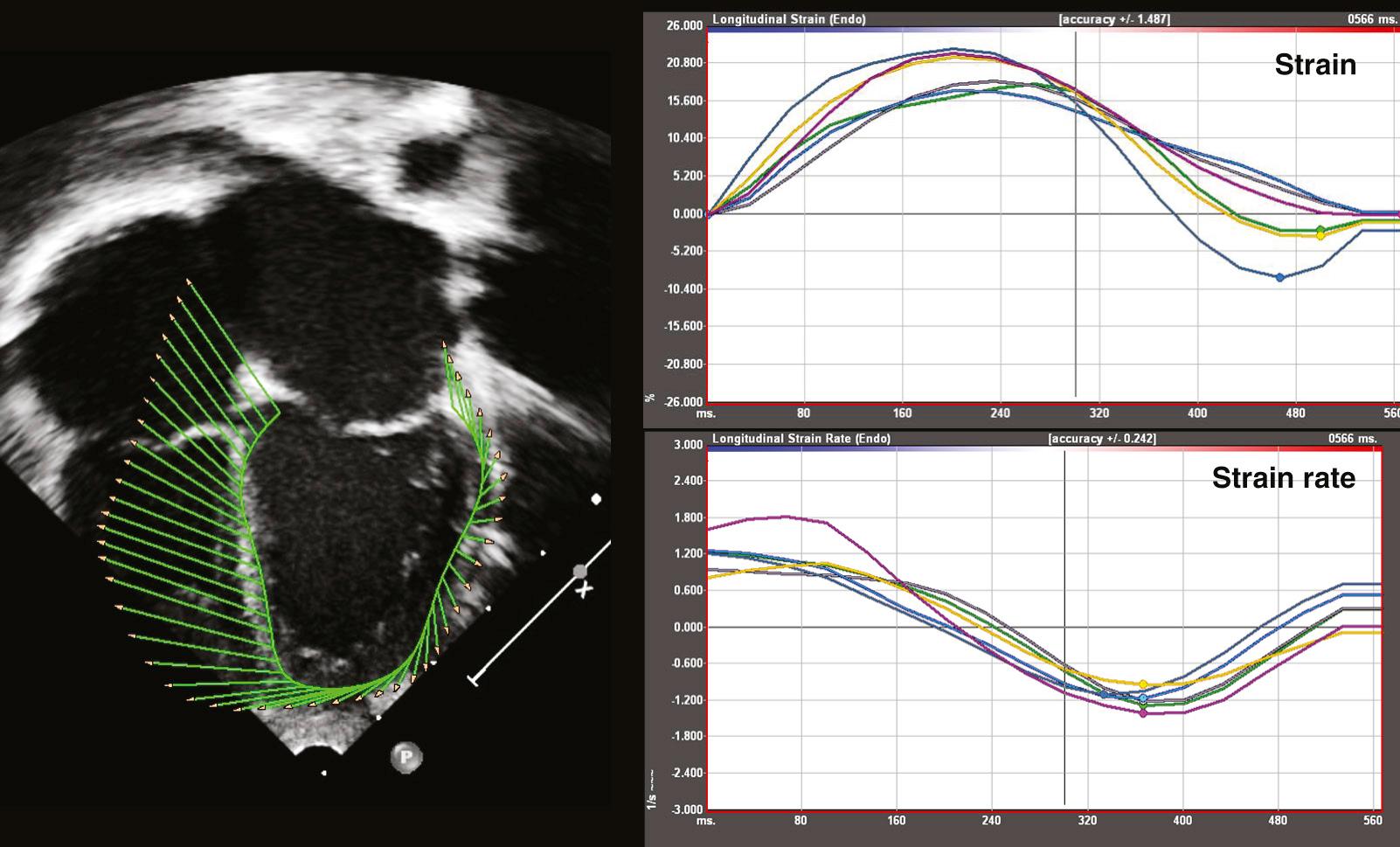
Speckle-tracking echocardiography (STE) is an echocardiographic technique that allows depiction and measurements of myocardial motion and function. The technique is based on frame-to-frame analysis of changes in the unique ultrasonic backscatter features (speckles) of sequential two-dimensional images while filtering out noise. STE displays local displacement of the myocardium that can be then analyzed for indices of myocardial deformation such as strain and strain rate, in any direction within the two-dimensional image ( Fig. 106-5 ). The technique, which was introduced in 2004, has been validated in an animal model against sonomicrometry and in vivo against cardiac MRI tagging. Advantages of STE over Doppler-based techniques for assessment of tissue motion include independence of angle of interrogation and insensitivity to tethering of the myocardium. More recently, three-dimensional STE has been developed and validated. A review of the use of STE in CHD can be found elsewhere.
As early as the late 1960s, Gramiak and colleagues noted that intravascular injection of almost any solution resulted in a contrast effect detectable by echocardiography. Initially, this technique was used to identify structures seen by M-mode echocardiography. Contrast echocardiography has been used to detect systemic and pulmonary venous anomalies, and for the detection of intracardiac and great artery level shunts. In today's pediatric echocardiography, contrast studies are infrequently performed and are usually limited to detection of intracardiac shunts in patients with limited echocardiographic windows, patch or baffle leak after cardiac surgery, and in pulmonary arteriovenous malformations.
The objectives of the echocardiographic examination must be tailored to the individual patient. The initial evaluation should include a comprehensive survey of all anatomic elements of the central cardiovascular system. Subsequent examinations are often targeted to answer specific clinical questions. It is important, however, to repeat complete echocardiograms during follow-up, even in patients who underwent a comprehensive initial examination, because of the dynamic nature of CHD. Examples include the late onset of discrete subaortic stenosis in patients with ventricular septal defect and/or coarctation of the aorta, double-chambered right ventricle, and supramitral stenosing ring.
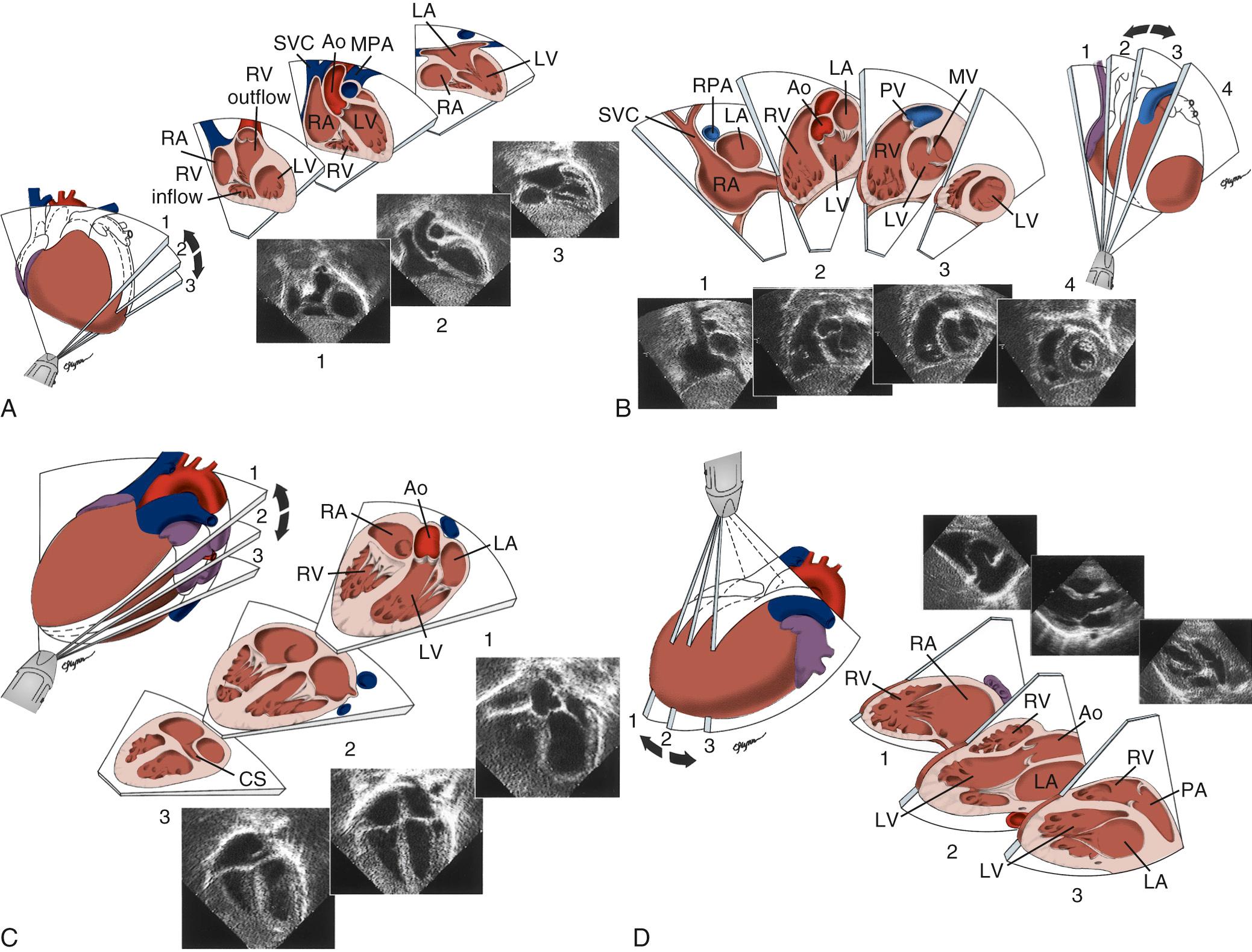
Proper planning of the echocardiographic examination is important to ensure that all diagnostic information is obtained most efficiently. This is particularly relevant in sedated patients in whom the time available for data acquisition is limited. Ideally, a complete segmental examination of cardiovascular anatomy and function should be performed in every new patient. This includes determination of visceral situs, heart position, atrial situs, systemic and pulmonary venous connections, ventricular situs, atrioventricular and ventriculoarterial alignments and connections, and coronary and great arterial anatomy. Assessment of ventricular function, intracardiac and vessel dimensions, and flow analysis across all valves, septa, chambers, and vessels are integral parts of the examination. Echocardiographic techniques include two-dimensional and three-dimensional imaging, blood flow imaging by color Doppler, measurements of flow velocities by pulsed and continuous wave Doppler, and assessment of myocardial function by tissue Doppler or STE. In young children with suspected heart disease, the examination begins from the subxiphoid approach by determining the abdominal situs and then proceeding by scanning the heart and great vessels, using a step-by-step segmental analysis ( Fig. 106-6 A and B ). This approach is advantageous because it provides a wide-angle view of heart position and cardiovascular anatomy and function at an early stage in the examination. Subsequent two-dimensional and Doppler analyses from the apical, parasternal, and suprasternal notch views supplement and confirm findings from the subxiphoid window (see Fig. 106-6 C -G ). The examination strategy should be tailored to the individual patient and modified according to the clinical situation as necessary. Although the standard views just described should be obtained in almost every patient and represent the minimum acceptable examination, flexibility and improvisation are important to optimally use the full potential of echocardiography.
When performing and reviewing an echocardiographic examination in a patient suspected of having CHD, a stepwise segmental approach to analysis of cardiac anatomy is taken. Each component of the heart is analyzed separately according to its unique morphologic features. The heart is composed of five segments—three main segments and two connecting segments. The three main segments are the atria, the ventricles, and the great arteries. The atrioventricular canal, which includes the mitral and tricuspid valves and the atrioventricular septum, connects the atria with the ventricles. The infundibulum (or conus) connects the ventricles with the great arteries. When analyzing cardiac anatomy, each cardiac chamber must be identified individually according to its unique anatomic-morphologic features and not according to its spatial position (right-sided or left-sided), valve of entry, or artery of exit. Throughout a systematic echocardiographic study, the examiner must go over a mental checklist of segments, their anatomic organization and position (situs), their connections and alignments with adjacent segments, and associated malformations. Using the aforementioned principles, any potential CHD can be accurately described in specific and precise terms. A detailed review of echocardiographic analysis of each cardiac segment can be found elsewhere.
Transesophageal echocardiography (TEE) was first introduced in 1976 and appeared in pediatric use in 1989. The miniaturization of probes and development of multiplanar imaging have greatly increased its role as an adjunct to transthoracic imaging, during surgical repair of CHD (intraoperative TEE), and to guide interventional catheterization procedures. Advances in transducer technology and image processing now allow real-time three-dimensional TEE.
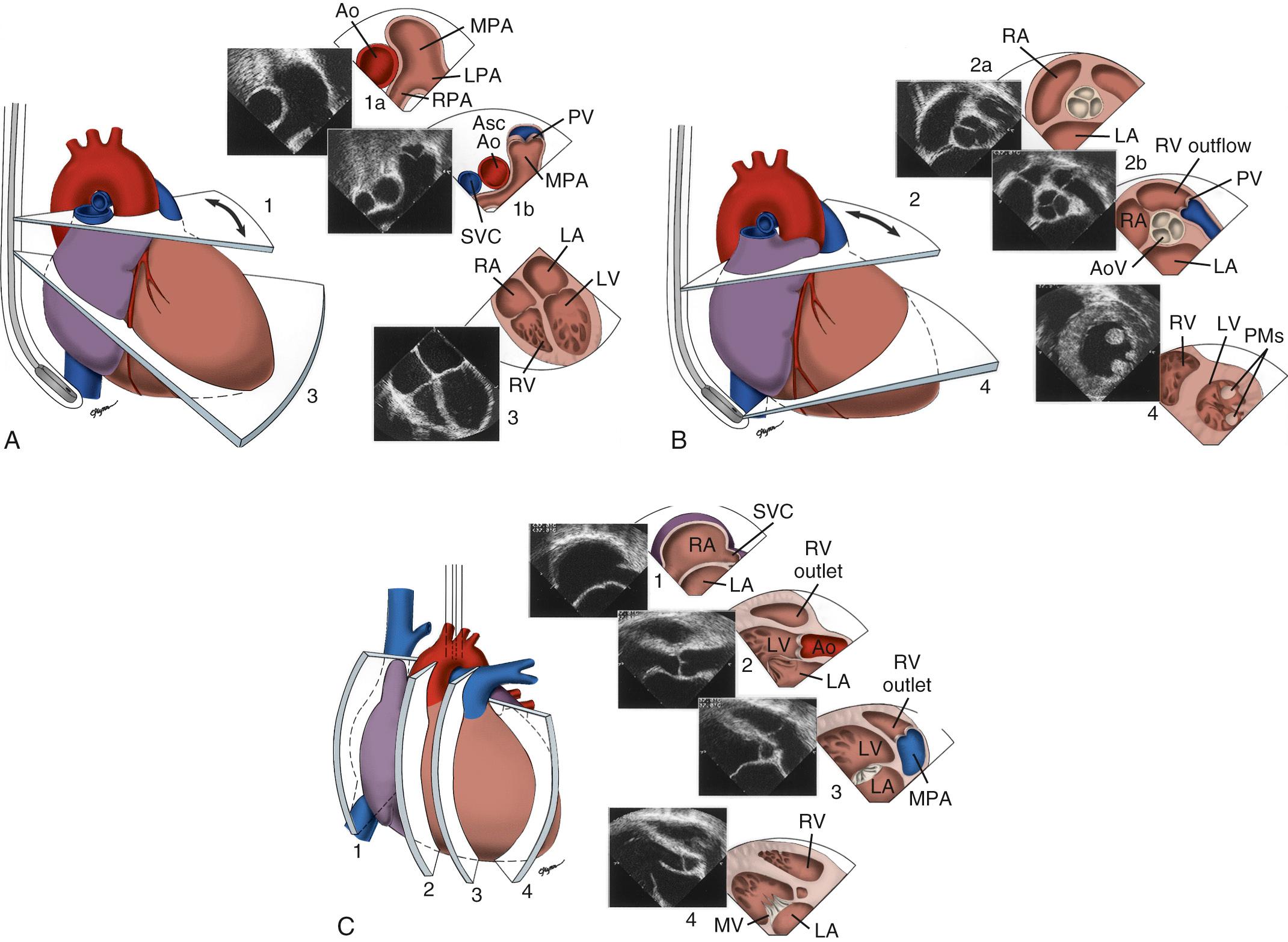
A TEE examination is usually performed to answer specific clinical questions. It is advisable, however, to perform a comprehensive examination of the heart and blood vessels for additional unsuspected anatomic and/or hemodynamic anomalies ( Fig. 106-7 ). Miniaturization of TEE probes designed for use in young infants weighing 3 to 3.5 kg or less has greatly enhanced the scope of TEE in the pediatric age group. Successful TEE examinations have been reported in patients weighing as little as 2.3 kg. The role of TEE in pediatric cardiology is continuously evolving. Although the transthoracic window is adequate in most situations, TEE provides distinct advantages during cardiovascular surgery, during video-assisted thoracoscopic procedures, for guidance of interventional catheter procedures, in the intensive care unit, for detection of intracardiac thrombi and vegetations, in the assessment of prosthetic valves, in selected patients on mechanical assist device and extracorporeal membrane oxygenator, and in selected patients with poor transthoracic windows, such as adults with CHD. The usefulness of selective versus routine use of intraoperative TEE in patients with CHD deserves further study.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here