Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Transthoracic echocardiography (TTE) provides an accurate diagnosis of the cause of mitral regurgitation (MR) in most patients, although three-dimensional transesophageal imaging (TEE) often is needed for decisions about timing and type of intervention.
Primary MR is caused by disease of the leaflets or chords, most often mitral valve prolapse (MVP), rheumatic heart disease, or infective endocarditis. Secondary MR may be caused by ischemic or nonischemic conditions associated with regional or global left ventricular (LV) dilation and systolic dysfunction.
Guidelines use similar quantitative measures of MR severity for primary and secondary MR. Consideration is given to the patient’s symptoms, LV size and function, left atrial size, pulmonary pressures, and MR severity.
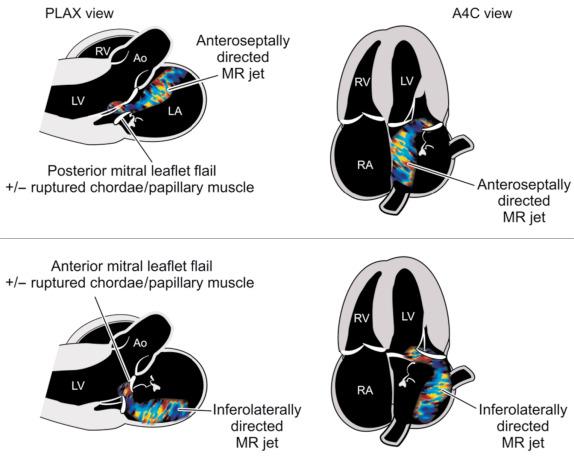
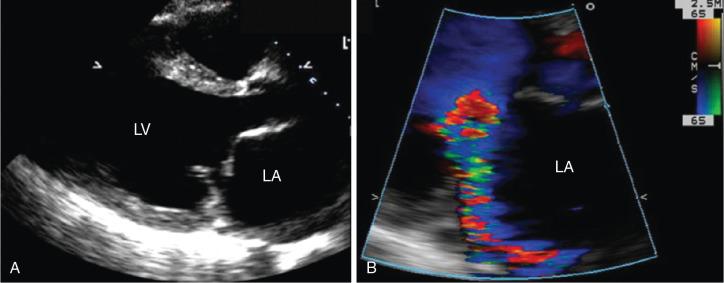
It is helpful to know the origin and direction of the MR jet when determining the exact mechanism of regurgitation and deciding on specific interventions to reduce MR severity.
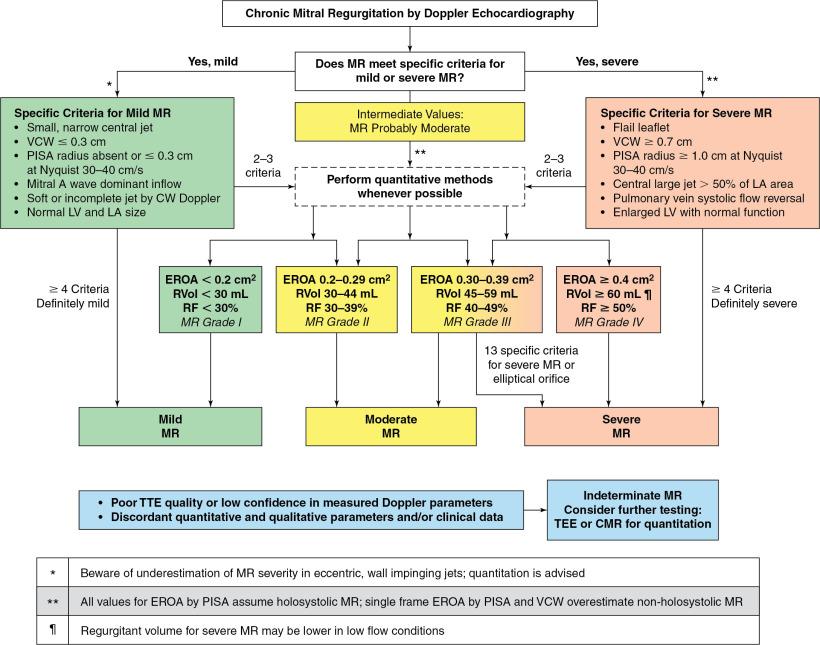
Evaluation of MR severity is based on integration of many qualitative and quantitative parameters (e.g., vena contracta width), and measurement of regurgitant volume and regurgitant orifice area is recommended when possible.
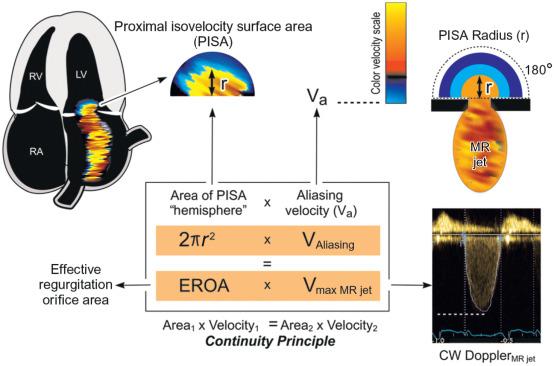
A simple, practical approach to quantitation of MR severity is measurement of the proximal isovelocity surface area (PISA) radius on color-flow Doppler imaging with the aliasing velocity set at 40 cm/s. The estimated effective regurgitation orifice area (EROA) is one half of the square of the PISA radius ( r 2 /2); a radius of approximately 1.0 cm indicates severe MR (EROA > 0.4 cm 2 ).
Evaluation of MR should take into account the dynamic changes in severity that can occur with changes in preload, afterload, and LV contractility.
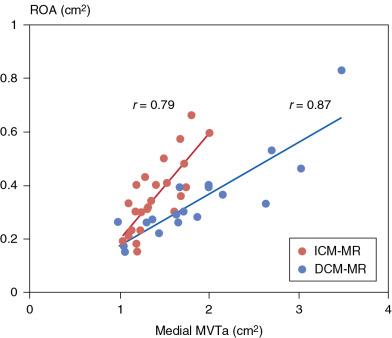
Imaging of LV size, geometry, and systolic function is a key element in the evaluation of patients with MR. Studies on transcatheter therapy for secondary MR offer insights into the complex interaction between LV size and function and MR severity.
In addition to TTE and TEE, cardiac magnetic resonance imaging, computed tomographic imaging, and invasive LV angiography may be helpful for selected patients.
The first step in imaging a patient with mitral valve (MV) disease is to diagnose the underlying disease process leading to valve dysfunction. Worldwide, mitral stenosis is most often caused by rheumatic valve disease. In developed countries, severe mitral annular calcification extending onto the valve leaflets is emerging as a cause of mitral stenosis in elderly patients. Mitral stenosis is discussed in Chapter 16 . This chapter focuses on imaging of patients with mitral regurgitation (MR).
The most common causes of MR include myxomatous MV disease (i.e., mitral valve prolapse [MVP] and ruptured or flail mitral chordae), rheumatic heart disease, infective endocarditis, hypertrophic cardiomyopathy, mitral annular calcification, dilated cardiomyopathy, and ischemic heart disease. Less common causes of MR include connective tissue disorders (e.g., Marfan syndrome, Loeys-Dietz syndrome), trauma, hypereosinophilic syndrome, metastatic carcinoid tumors, and exposure to certain drugs.
The causes of MR are categorized as primary (i.e., organic or degenerative) MR, which result from abnormalities of the MV apparatus itself, or secondary (i.e., functional) MR, which is associated with pathology of the left ventricle (LV), left atrium (LA), or mitral annulus but with relatively normal valve leaflets and chords. Ischemic MR is a subset of secondary MR that results from myocardial infarction with subsequent LV dysfunction and remodeling. Primary and secondary forms of MR are two distinct disease states with distinct pathologies, outcomes, and management considerations (see Chapters 17 and 18 ).
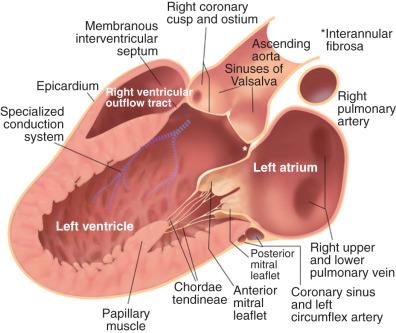
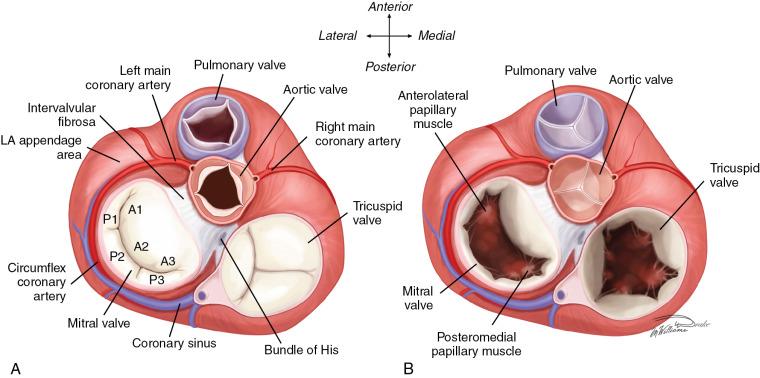
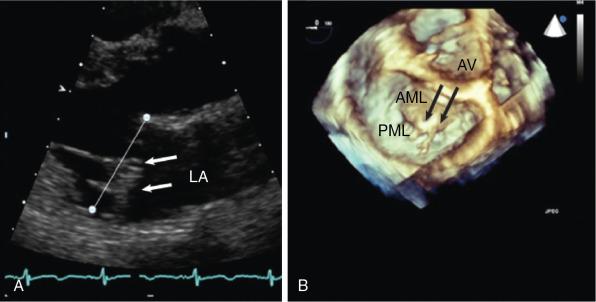
The next step in imaging the patient with MR is to determine the specific mechanism of MR. Abnormalities in the MV leaflets, chordae tendineae, papillary muscles, mitral annulus, LA, or LV can result in MR ( Figs. 15.1 and 15.2 ). One useful approach to categorizing the mechanism of MR is based on the pattern of leaflet motion: normal (type I), excessive (type II), or restricted (type IIIa, restricted opening; type IIIb, restricted closure) (see Fig. 19.3 in Chapter 19 ). This classification system is useful in considering potential surgical or transcatheter interventions for reducing MR severity. Types II and IIIa usually are caused by primary disorders of the valve leaflets, whereas in types I and IIIb, the leaflets are relatively normal but leaflet motion is distorted by LV, LA, and/or annular remodeling causing secondary MR.
Transthoracic echocardiography (TTE) is adequate for routine evaluation of the anatomy and motion of the valve leaflets, but transesophageal echocardiography (TEE) often is necessary for optimal visualization of valve anatomy and quantitation of regurgitant severity, particularly when surgical or transcatheter intervention is being considered.
Myxomatous disease occurs on a spectrum according to the relative degree of leaflet thickening and redundancy versus weakness in the mitral chords. On one end of the spectrum is Barlow syndrome ( Fig. 15.3 ), which is characterized by significant leaflet thickening and redundancy, prolapse of multiple scallops, and severe regurgitation arising from multiple points along the valve closure line. At the other end of the spectrum is fibroelastic deficiency, in which the leaflets are relatively thin; at presentation, there is isolated prolapse or flail of a single scallop with regurgitation originating from a single focus. Intermediate forms lie between these two extremes.

Infective endocarditis causes MR by destruction of valve leaflets, which results in inadequate coaptation, or by frank leaflet perforation. Vegetations on the MV can prevent complete leaflet closure. Even after effective treatment of endocarditis, valvular retraction and calcification can lead to persistent or worsening MR.
In the developing world, rheumatic heart disease remains a common cause of MR. In contrast to mitral stenosis, rheumatic MR is more frequent in men than in women. It is a consequence of shortening, rigidity, deformity, and retraction of one or both MV cusps and is associated with shortening and fusion of the chordae tendineae and papillary muscles.
MR can occur with exposure to drugs that cause fibrotic changes in the valve leaflets. Among drugs associated with MR are the ergot alkaloids methysergide and ergotamine, the anorexigens (dex)fenfluramine and benfluorex, the dopamine agonists pergolide and cabergoline, and MDMA (Ecstacy). The thickened, rigid leaflets are similar to those usually seen in patients with carcinoid and suggest a common pathophysiologic cause: overstimulation of the serotonin 2B receptor. In carcinoid limited to the gastrointestinal tract, the excess serotonin is metabolized in the lungs, and mitral involvement is not seen. However, with lung metastases or right-to-left shunting, mitral and aortic thickening and regurgitation may develop as a result of exposure to serotonin.
The normal mitral annulus in an adult has a circumference of approximately 10 cm. The annulus is soft and flexible, with systolic annular constriction caused by contraction of the surrounding LV muscle that contributes importantly to valve closure. Smooth muscle cells within the annulus and mitral leaflets may also exert a sphincter action on the valve. MR due to dilation of the mitral annulus can occur in any form of heart disease characterized by dilation of the LV or LA, especially in dilated cardiomyopathy and long-standing atrial fibrillation. ,
Aneurysm of the basal inferoposterior LV wall (i.e., submitral aneurysm) has been reported as a cause of annular MR in sub-Saharan Africa. It appears to result from a congenital defect in the posterior aspect of the annulus. Primary diseases of the leaflets, such as myxomatous disease, are associated with annular dilation and abnormal annular motion, which may worsen the severity of MR. ,
Idiopathic (degenerative) calcification of the mitral annulus or leaflets is commonly found at autopsy and is usually of little functional consequence. However, if severe annular or leaflet calcification develops ( Fig. 15.4 ), it can cause MR and even significant mitral stenosis. Mitral annular calcification shares common risk factors with atherosclerosis, including hypertension, dyslipidemia, and diabetes, and it is associated with coronary and carotid atherosclerosis and aortic valve calcification. Patients with significant annular or leaflet calcification are at higher risk for cardiovascular morbidity and mortality. Annular calcification may be accelerated by an intrinsic defect in the fibrous skeleton of the heart, as in patients with Marfan and Hurler syndromes, in which annular dilation further contributes to MR. The incidence of mitral annular calcification is increased in patients who have chronic renal failure with secondary hyperparathyroidism and in those with rheumatic involvement.
Abnormalities of the chordae tendineae are important causes of MR ( Fig. 15.5 ). Lengthening and rupture of the chordae tendineae are cardinal features of the MVP syndrome ( Fig. 15.6 ), particularly in cases of fibroelastic deficiency. The chordae may be congenitally abnormal; rupture may be spontaneous (primary), or it may occur as a consequence of infective endocarditis, trauma, rheumatic fever, or, rarely, osteogenesis imperfecta or relapsing polychondritis.
In most patients, no cause for chordal rupture is apparent other than increased mechanical strain on thin, myxomatous chords. Chords to the posterior leaflet rupture more frequently than those to the anterior leaflet. Depending on the number of chords involved in rupture and the rate at which rupture occurs, the resultant MR may be mild, moderate, or severe and acute, subacute, or chronic. Chordal rupture also has been reported as a result of trauma from percutaneous circulatory support devices.
The LV papillary muscles are perfused by the terminal portion of the coronary vascular bed, making them particularly vulnerable to ischemia, and any disturbance in coronary perfusion may result in papillary muscle dysfunction. Transient ischemia causes temporary papillary muscle dysfunction and transient episodes of MR that are sometimes associated with attacks of angina pectoris or pulmonary edema. If papillary muscle ischemia is severe and prolonged, papillary muscle dysfunction and scarring lead to chronic MR. MR occurs in approximately 20% of patients after acute myocardial infarction, and even when mild, it is associated with a higher risk of adverse outcomes.
The posterior papillary muscle, which is supplied by the posterior descending branch of the right coronary artery, becomes ischemic and infarcted more frequently than the anterolateral papillary muscle. The latter is often dually supplied by diagonal branches of the left anterior descending coronary artery and marginal branches from the left circumflex artery. Ischemia of the papillary muscles usually is caused by coronary atherosclerosis but also may occur in patients with severe anemia, shock, coronary arteritis of any cause, or an anomalous left coronary artery.
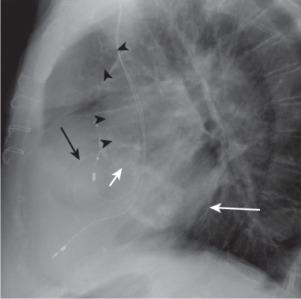
With remote myocardial infarction, MR may result from regional myocardial tissue at the base of a papillary muscle, most commonly due to right coronary or left circumflex coronary disease, which results in tethering of the mitral leaflets and incomplete leaflet coaptation. , Necrosis of a papillary muscle can complicate myocardial infarction, but frank rupture of the full papillary muscle is rarely diagnosed premortem because it usually causes severe or fatal acute MR. However, rupture of one or two of the apical heads of a papillary muscle can result in a flail leaflet ( Fig. 15.7 ) with a lesser degree of MR (although still usually severe). Survival is possible, usually with prompt surgical therapy, , although percutaneous repairs have also been reported.
Various other disorders of the papillary muscles may be responsible for the development of MR. They include congenital malposition of the papillary muscles, absence of one papillary muscle (leading to the parachute MV syndrome), and involvement or infiltration of the papillary muscles by a variety of processes such as abscesses, granulomas, neoplasms, amyloidosis, and sarcoidosis.
Ischemic LV dysfunction and dilated cardiomyopathy are contributors to the development of MR and represent the second leading cause of MR (after MVP) in the United States. LV dilation of any cause, including ischemia, can alter the spatial relationships between the papillary muscles and chordae tendineae and thereby result in secondary MR ( Fig. 15.8 ). For a given amount of LV dilation, MR is greater when there is asymmetric tethering of the MV caused by inferior and inferolateral ventricular scarring rather than symmetric dilation as in dilated cardiomyopathy ( Fig. 15.9 ).
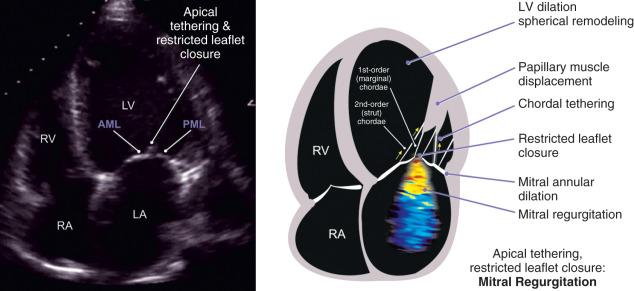
Some degree of MR is found in approximately 30% of patients with coronary artery disease who are referred for coronary artery bypass grafting (CABG). In most of these patients, MR develops from tethering of the posterior leaflet because of regional LV dysfunction. Other pathologic changes may include additional ischemic damage to the papillary muscles, dilation of the MV ring, and loss of systolic annular contraction contributing further to MR. The incidence and severity of regurgitation vary inversely with LV ejection fraction and directly with LV end-systolic volume (ESV).
Echocardiography plays a central role in quantifying MR severity. An integral part of evaluating MR severity is consideration of the degree of LA and LV enlargement and assessment of LV systolic function ( Tables 15.1 through 15.3 ). Doppler echocardiography characteristically reveals a high-velocity signal in the regurgitant orifice with flow from the LV to the LA during systole. Qualitative assessment of the color Doppler regurgitant jet size in the LA correlates reasonably well with quantitative methods in estimating MR severity. However, color-flow jet areas are significantly influenced by the driving pressure (i.e., LV-LA gradient), jet eccentricity, and a host of instrument factors such as transmission power and frequency, receiver gain, Nyquist limit, and wall filter, limiting the accuracy of this approach ( Table 15.4 ).
| SECONDARY MR | |||
|---|---|---|---|
| Parameter | Primary MR a | Regional LV Dysfunction | Global LV Dysfunction |
| Cause | Myxomatous or calcific leaflet degeneration | Inferior myocardial infarction | Nonischemic cardiomyopathy, large anterior or multiple myocardial infarctions |
| LV remodeling | Global if severe chronic MR | Primarily inferior wall | Global dilation with increased sphericity |
| LA remodeling | Moderate to severe if chronic MR | Varies | Usually severe |
| Annulus | Dilated, preserved dynamic function | Mild to no dilation, less dynamic | Dilated, flattened, nondynamic |
| Leaflet morphology | |||
| Thickening Prolapse or flail Calcification |
Yes/moderate, severe Usually present Varies |
No/mild No No/mild |
No/mild No No/mild |
| Tethering pattern | None | Asymmetric | Symmetric |
| Systolic tenting | None | Increased | Markedly increased |
| Papillary muscle distance | Normal | Increased posterior papillary-intervalvular fibrosa distance | Increased interpapillary muscle distance |
| MR jet direction | Eccentric or central | Posterior | Usually central |
| CWD | May be late systolic (if MVP) or uniform if flail or with calcific degeneration | Density usually uniform throughout systole | Biphasic pattern, with increased density in early- and late-systolic flow and midsystolic dropout |
| PISA | Often hemispheric | Often not hemispheric | Often not hemispheric; may be biphasic |
| Modality | Optimization | Example | Advantages | Pitfalls |
|---|---|---|---|---|
| Color-Flow Doppler | ||||
| Proximal flow convergence | Align direction of flow with insonation beam to avoid distortion of hemisphere from noncoaxial imaging Zoomed view Variance off Change baseline of Nyquist limit in the direction of the jet Adjust lower Nyquist limit to obtain the most hemispheric flow convergence (typically 30–40 cm/s) Measure the radius from the point of color aliasing to the VC |
 |
Rapid qualitative assessment Absence of proximal flow convergence usually a sign of mild MR |
Multiple jets Eccentric jets Constrained jet (LV wall) Nonhemispheric shape, particularly functional MR Overestimation when MR not holosystolic |
| VCW | Parasternal long-axis view Zoomed view Imaging plane for optimal VC Best measured when proximal flow convergence, VC, and MR jet aligned in same plane |
 |
Surrogate for regurgitant orifice size Independent of flow rate and driving pressure for a fixed orifice Can be applied to eccentric jets Depends less on technical factors Good at separating mild (<0.3 cm) from severe MR (≥0.7 cm) |
Problematic in the setting of multiple jets Convergence zone needs to be visualized for adequate measurement Overestimation when MR not holosystolic |
| Jet area or jet area/LA area ratio | Apical view Zoom view Measure largest jet alone or as ratio to LA area in same view |
  |
Easy to measure | Shown to be imprecise in multiple studies, particularly in eccentric, wall-impinging jets Depends on hemodynamic (especially LV systolic pressure) and technical variables Overestimation when MR not holosystolic |
| 3D VCA | Color-flow sector should be as narrow as possible to improve volume rates and line density Align orthogonal cropping planes along the axis of the jet Planimeter the high velocity aliased signal of VC, avoiding low velocity (dark color) signals |
 |
Multiple jets of different directions may be measured Can identify severe functional MR in some cases when PISA underestimates EROA (arrow) |
Subject to color Doppler blooming Limited temporal and spatial resolution Overestimation when MR not holosystolic Multiple jets may be in different planes, must be analyzed separately and then added Cumbersome; often requires offline analysis |
| Pulse-Wave Doppler | ||||
| Mitral inflow velocity | Align insonation beam with the flow across the MV at leaflet tips in apical four-chamber view |  |
E velocity ≥ 1.2 m/s is a supportive sign of severe MR (volume load) Dominant A-wave inflow pattern virtually excludes severe MR Can be obtained with TTE and TEE |
Depends on LV relaxation and filling pressures High E velocity not specific for severe MR in secondary MR, atrial fibrillation, and mitral inflow stenosis |
| Pulmonary vein flow pattern | Use small sample volume (3–5 mm) placed 1 cm into the pulmonary vein |  |
Systolic flow reversal in more than one pulmonary vein is specific for severe MR Normal pulmonary vein pattern suggests low LA pressure and nonsevere MR |
Eccentric MR of mild or moderate severity directed into a pulmonary vein alters flow pattern Systolic blunting is not specific for significant MR (common in secondary MR and present in elevated LA pressure, atrial fibrillation) |
| Continuous-Wave Doppler | ||||
| Density and contour of regurgitant jet | Align insonation beam with the flow |   |
Simple Density is proportional to the number of red blood cells reflecting the signal Faint or incomplete jet is compatible with mild MR A triangular contour (early MR peak velocity; arrow ) denotes a large regurgitant pressure wave and hemodynamic significance |
Qualitative Perfectly central jets may appear denser than eccentric jets of higher severity Density is gain dependent A contour with an early peak velocity is not sensitive for severe MR |
| Quantitative Doppler: EROA, RVol, and Fraction | ||||
Flow convergence method (PISA)  |
Align insonation beam with the flow, usually in apical views; zoomed view Lower the color Doppler baseline in the direction of the jet Look for the hemispheric shape to guide the best low Nyquist limit Look for need for angle correction if flow convergence zone is nonplanar Measure PISA radius at roughly the same time as CW jet peak velocity |
  |
Rapid quantitative assessment of lesion severity (EROA) and volume overload (RVol) Shown to predict outcomes in degenerative and functional MR |
May not be accurate in multiple jets Less accurate in eccentric jets or markedly crescent-shaped orifices Small errors in radius measurement can lead to substantial errors in EROA due to squaring of error; this is less likely to misclassify patients at very large (≥1.0 cm) or very small radii (≤0.4 cm) |
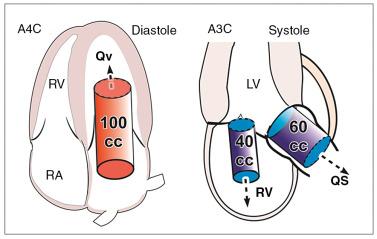
SV method  RVol = SV MV − SV LVO |
LVOT diameter measured at the annulus in systole and pulsed Doppler from apical views at same site Mitral annulus measured at mid-diastole; pulse-wave Doppler at the annulus level in diastole Total LVSV can be measured by pulsed Doppler technique at mitral annulus or by the difference between LV end-diastolic volume and end-systolic volume LV volumes are best measured by 3D; contrast may be needed to better trace endocardial borders; if 3D not feasible, use 2D method of disks |
Mitral annulus  LVOT  |
Quantitative, valid with multiple jets and eccentric jets Provides lesion severity (EROA, RF) and volume overload (RVol) Validated against CMR in isolated MR |
Not valid for combined MR and AR unless pulmonic site is used Cumbersome, needs training; small errors in each different measurement can combine to magnify error in final results Pulse-wave Doppler method (mitral SV) and LV volume method may give different results |
Quantitative methods to measure regurgitant fraction, regurgitant volume, and regurgitant orifice area have greater accuracy when done carefully ( Figs. 15.10 through 15.12 ). An integrative approach with consideration of multiple parameters of MR severity is strongly recommended ( Fig. 15.13 ).
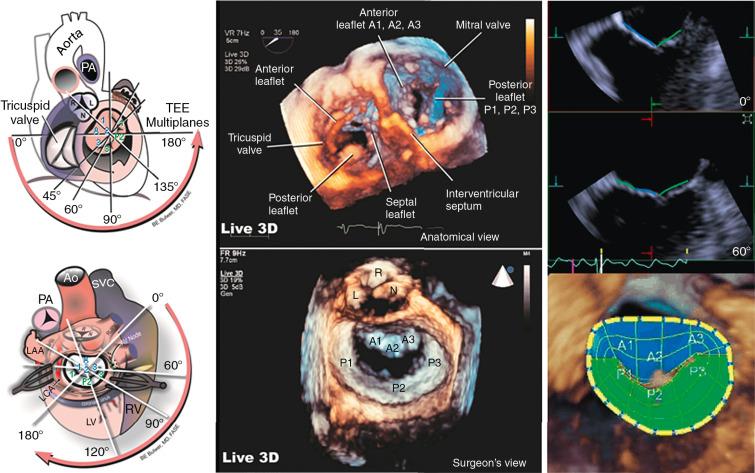
TEE imaging with three-dimensional (3D) visualization provides better assessment of mitral anatomy and leaflet motion, identification of the exact mechanism and origin of the regurgitant jet, and quantitation of regurgitant severity. MR assessment, with LV volumes routinely available, and surface rendering of the valve directly demonstrate the pathology. Multiplane imaging allows the valve to be interrogated in a structured fashion to optimally localize the pathology ( Fig. 15.14 ; see Fig. 15.7 ). 3D Doppler imaging , , helps elucidate the mechanism of MR ( Fig. 15.15 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here