Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pediatricians need to be able to distinguish normal development and individual differences from delayed or atypical patterns of development and behavior in both routine health supervision and in comprehensive management of children with other medical conditions. Once developmental or behavioral delays have been identified, the pediatrician conducts a diagnostic workup, initiates management, refers to appropriate services, counsels families, and coordinates care. The goal of this chapter is to review the developmental/behavioral issues faced in routine pediatric practice. In the first half, the fundamental principles of development are applied to each major domain of functioning. Within each domain, discussion centers on the major developmental milestones, methods of assessment, signs of developmental variation, and approaches to children who show developmental delays or deviant patterns. In the second half, several developmental disorders are described, including definitions, diagnostic criteria, and the role of physical examination in evaluation, physical findings, and prognosis.
Development is commonly discussed in terms of domains of function. Gross motor skills refer to the use of the large muscles of the body; fine motor skills refer to the use of small muscles of the hands; cognition means the use of higher mental processes including thinking, memory, and learning; language refers to the comprehension and production of meaningful symbolic communication; and social and emotional functioning refers to skills for interactions with others and emotional reactions to people and events. Within each domain, skills are typically acquired in a predictable sequence, although there is wide variation in the age of acquisition of specific milestones. Domains of development are interdependent. Cognitive abilities in infancy cannot readily be distinguished from sensorimotor functioning. Similarly, mature social functioning depends on competent language abilities. Early reflex patterns and congenital sensory and motor capabilities are the building blocks of higher-order skills.
In general, the development of a child is considered to occur in cephalocaudal and centrifugal directions, that is, from head to toe (the child holds his or her head up before being able to sit or stand up) and from proximal to distal (the child has rudimentary whole-hand grasp before developing a fine pincer grasp). In addition, the development of a child is considered to occur according to the general principle of dependence to independence (from no mobility to rolling, sitting, creeping, crawling, cruising, and walking) and in response to stimuli (from generalized reflexes to discrete voluntary actions).
A central component of health maintenance is the prompt identification of developmental problems and the promotion of developmental progress. Developmental surveillance refers to the longitudinal, continuous process by which physicians and other professionals use all available clinical tools to determine a child’s developmental status, to evaluate his or her developmental progress over time, and to identify children who may be at risk for disorders. Surveillance requires that physicians elicit and appropriately attend to parental concerns at each visit, review teacher and day care provider concerns, obtain a developmental history, make observations of current development and behavior, perform a physical examination, administer or review and interpret screening tests, and use other assessment techniques. Frequent routine assessments promote a longitudinal view of the child and allow parental concerns to be addressed in a timely manner. A formal developmental assessment can be arranged if there are severe or persistent concerns. Ideally, these formal developmental assessments take place in the natural environment where the child spends much of his/her time; for example: birth to 3 years old at home, 3 to 5 years old in a preschool or day care setting, and 5-year-old and older children in a school setting. Parental concerns must be addressed at each well childcare and sick visit; parents are generally accurate reporters of current developmental status, and therefore their concerns are sensitive indicators of delays or atypical patterns of development. Well childcare and sick visits can take place in person and through telemedicine two-way video technology.
The physician’s ability to identify children with developmental delays and disorders is improved by the appropriate use of validated screening tools ( Table 3.1 ). The tools have been designed to be used with unselected groups of children, ideally as part of routine developmental surveillance at a few selected health maintenance visits, such as the 9-, 18-, 24-, or 36-month visits. These visits can happen in person and/or through telemedicine two-way video technology. The sensitivity and specificity of these instruments used during these visits range from 0.70 to 0.90. The clinician’s judgment is required in interpretation of test results, particularly of measures that rely on parental report. Children who are developing normally may fail a screening test because of shyness, unfamiliarity with the examiner or the materials, or other factors unrelated to developmental competence. New telemedicine visits with two-way video technology might help to address this issue as children feel more comfortable at home or in their age-depended natural environment. In most cases, a positive screen should be followed by a comprehensive assessment of development and should not be ignored. These comprehensive assessments of development should ideally happen in person, although they can also be conducted through telehealth assessments with two-way video technology. They should happen, to the extent possible, in a natural environment where the child spends much of his or her time (e.g., birth to 3 years old at home, 3 to 5 years old in a preschool or day care setting, and 5-year-old and older children in a school setting). Screening tests can be used to confirm parental concerns but are not appropriate for diagnosing the nature of the problem. If parental concerns persist despite negative screening findings, a full evaluation is advisable because of the limited sensitivity of the tests and the importance of attending to parental concerns. To ensure that the performance is representative of the child’s ability, screening tests should be performed when the child is physically well, familiar with the setting and with the examiner, and under minimal stress. Examples of familiar settings include the child’s home for infants, toddlers, and younger children; the child’s preschool becomes another familiar setting for children 3 years old and older. Obtaining results from natural settings may require collaboration with community-based organizations that conduct home or school visiting, but it might be also conducted through telehealth assessments with two-way video technology.
| Name of Test | Parent Time | Provider Time | Age Range Covered |
|---|---|---|---|
| Ages and Stages Questionnaires (ASQ) | 10–20 min | 1–5 min | 4 months–5 years |
| Child Development Inventories | 30 min | 10 min | 15 months–6 years |
| Parents’ Evaluation of Developmental Status (PEDS) | 5 min | 2 min | 0–8 years |
| Denver II | 20 min | 2 weeks–6 years | |
| Guide for Monitoring Child Development (GMCD) | 7 min | 0–24 months | |
| Rapid Neurodevelopmental Assessment (RDNA) | 30 min | 2–5 years |
At birth, a neonate’s movements consist of alternating flexion and extension, which usually are symmetric and vary in strength with the infant’s state of alertness. In addition, involuntary “primitive” reflexes can be elicited; they indicate that the patterns of movement requiring the integrated activity of multiple muscle groups are present even at birth. The intact newborn sucks and grasps reflexively; these are motor patterns that are programmed into the organism to enhance survival. The presence of primitive reflexes in the newborn and the disappearance (integration) of these reflexes in a predictable sequence as the infant matures are indications of typical motor development reflecting many developmental and neural factors, such as underlying myelination of higher cortical pathways that allow for voluntary control of movement. Persistence of primitive reflexes beyond the typical age suggests abnormal myelination of the higher inhibitory pathways as seen in children with neurologic or developmental disorders, such as prenatal or perinatal hypoxic-ischemic brain injury.
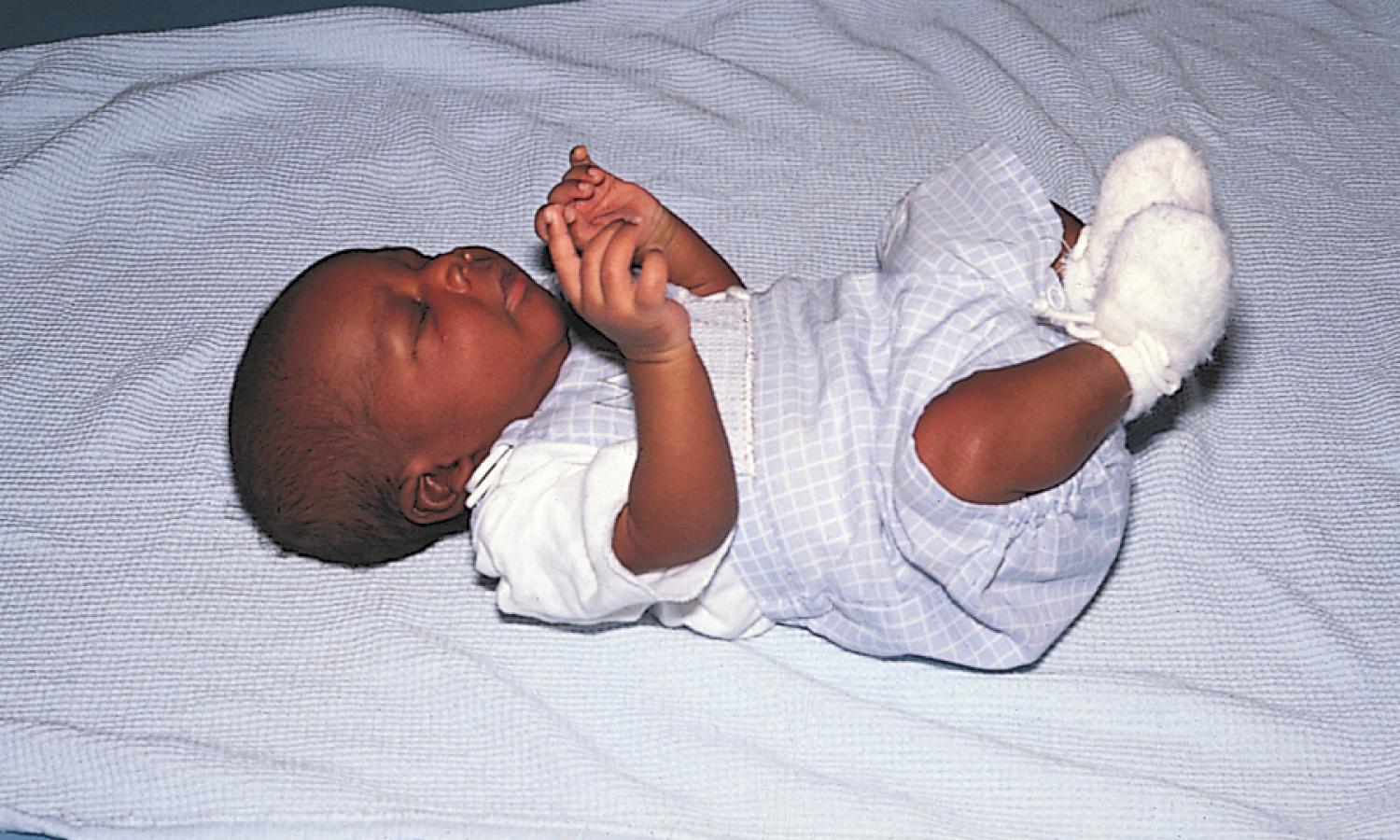
Perhaps the best known of these reflex patterns is the Moro response, or startle reflex. This reflex can occur spontaneously after a loud noise, but typically it is elicited during the physical examination by an abrupt extension of the infant’s neck. The response consists of symmetric abduction and extension of the arms with extension of the trunk ( Fig. 3.1 ) followed by adduction of the upper extremities, as in an embrace, and frequently is accompanied by crying ( Fig. 3.2 ). The Moro reflex gradually disappears by 4 months old, associated with the development of cortical functioning. In children up to 4 months old, the Moro response can be used to evaluate the integrity of the central nervous system and to detect peripheral nerve problems, such as congenital musculoskeletal abnormalities or neural plexus injuries; an asymmetric response may indicate unilateral weakness.

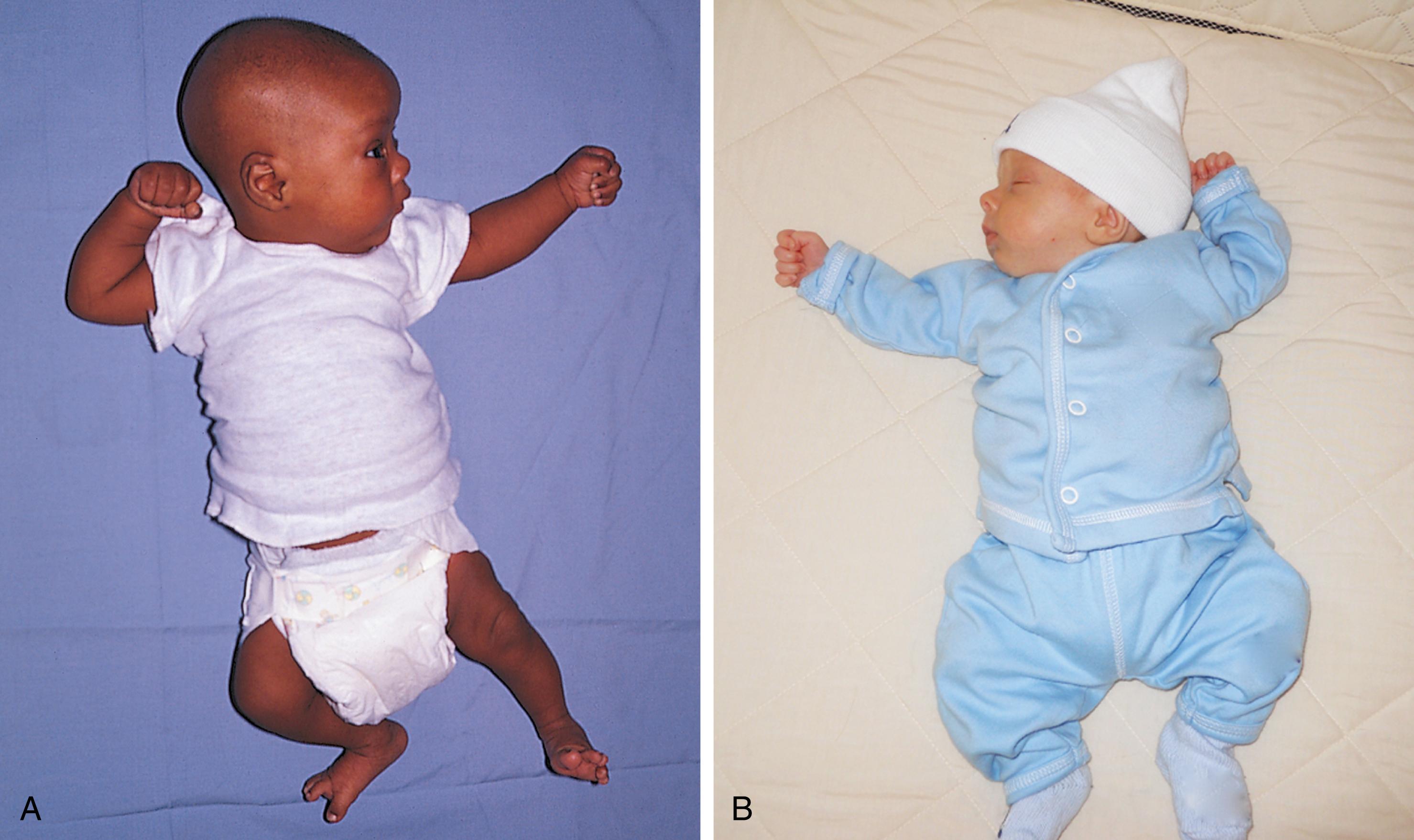
Another early reflex pattern is called the asymmetric tonic neck reflex (ATNR) ( Fig. 3.3 ). A newborn’s limb motions are strongly influenced by head position. If the head is directed to one side, either by passive turning or by inducing the baby to follow an object to that side, tone in the extensor muscles increases on that side and in the flexor muscles on the opposite side. This response may not be seen immediately after birth, when the newborn has high flexor tone throughout the body, but it usually appears by 2 to 4 weeks of age. The ATNR allows the baby to sight along the arm to the hand and is considered one of the first steps in the coordination of vision and reaching. This reflex disappears by 4 to 6 months old to allow for the development of voluntary reaching.
With the emergence of voluntary control from higher cortical centers, muscular flexion and extension become balanced. Primitive reflexes are replaced by reactions that allow children to maintain a stable posture, even if they are rapidly moved or jolted. A timetable listing the expected emergence and disappearance of primitive reflexes and the protective equilibrium responses is presented in Table 3.2 .
| Reflex | Appearance a | Disappearance a |
|---|---|---|
| Moro | Birth | 4 months old |
| Hand grasp | Birth | 3 months old |
| Crossed adductor | Birth | 7 months old |
| Toe grasp | Birth | 8–15 months old |
| ATNR | 2 weeks old | 6 months old |
| Head righting | 4–6 months old | Persists voluntarily |
| Protective equilibrium | 4–6 months old | Persists voluntarily |
| Parachute | 8–9 months old | Persists voluntarily |
a Different sources may vary on the precise timing of the appearance and disappearance of these primitive and equilibrium responses.
Muscle control develops in an organized fashion, from head to toe, or in a cephalocaudal progression—head control followed by reaching, followed by sitting, followed by standing—reflecting neuronal myelination in a typical sequence.
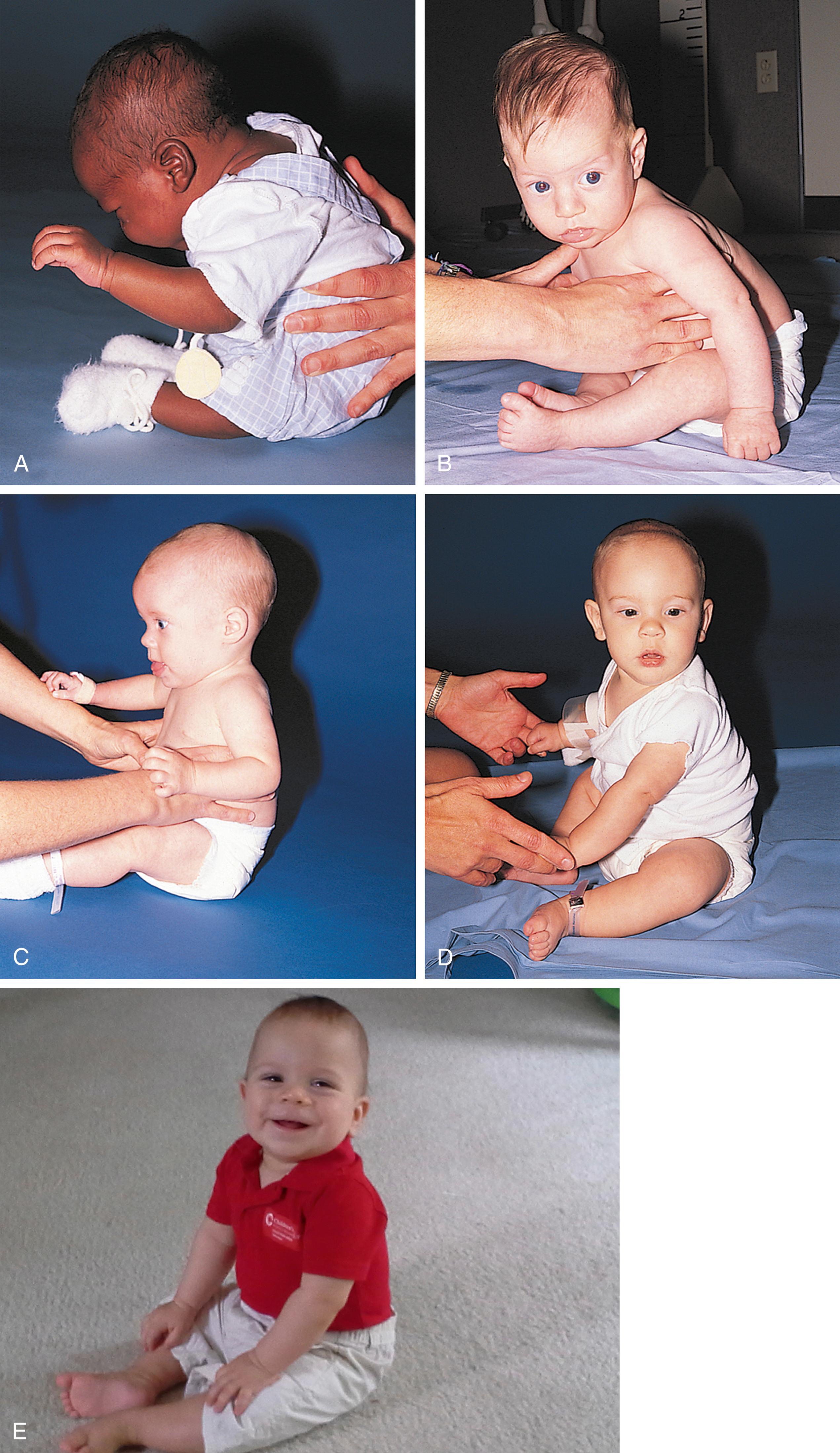
The infant’s earliest control task is to maintain a stable posture against the influence of gravity. Neck flexors allow head control against gravity when a child is pulled from the supine to the sitting position. Neonates show minimal control of the neck flexors, holding their heads upright only briefly when supported in a sitting position. When an infant is pulled to a sitting position, the head lags behind the arms and shoulders ( Fig. 3.4A ). By 4 months old, the child can support his head, and his head moves along with his shoulders when he is pulled to a sitting position (see Fig. 3.4B ). At 5 to 6 months old, the infant anticipates the direction of movement of the pull-to-sit maneuver and flexes the neck before the shoulders begin to lift (see Fig. 3.4C ).

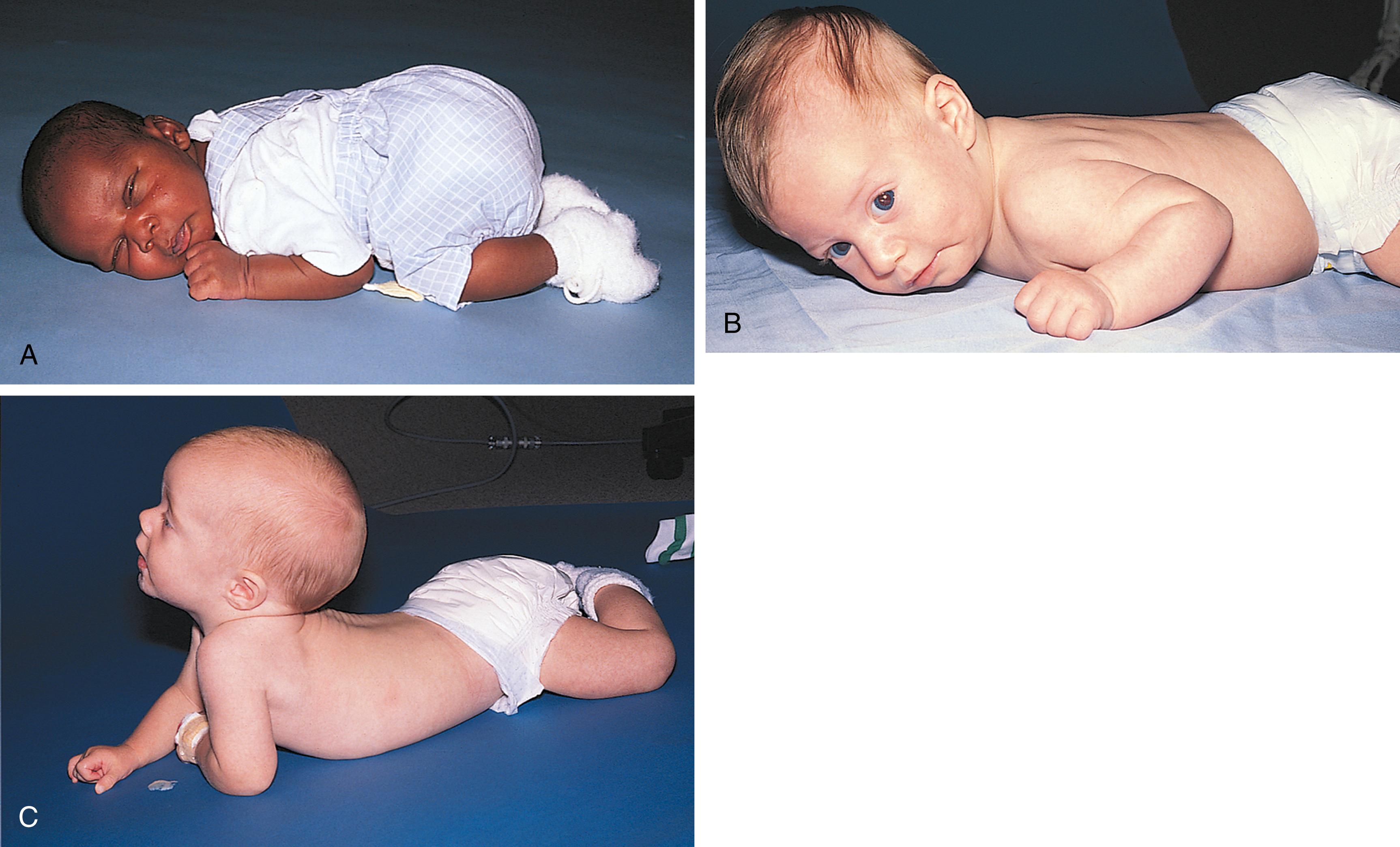
In the prone position, a newborn remains in a tightly flexed position and can simply turn the face from side to side along the bed sheets. Progressive control of the shoulders and upper trunk in the first few months of life, plus a decrease in flexor tone, enables the young infant to hold the chest off the bed with the weight supported on the forearms by approximately 4 months old ( Fig. 3.5 ). Evolution of trunk control down the thoracic spine can also be observed with the infant in a sitting position ( Fig. 3.6 ). As control reaches the lumbar area, the lumbar lordotic curve can be seen when the child is standing ( Fig. 3.7 ).

Equilibrium and protective reactions are automatic, reflexive patterns that also emerge in a cephalocaudal sequence. Head righting refers to the infant’s ability to keep the head vertical despite a tilt of the body. A 4-month-old infant typically demonstrates this ability in vertical suspension when gently swayed from side to side. As control moves downward, protective equilibrium responses can be elicited in a seated infant by abruptly but gently pushing the infant’s center of gravity past the midline in one of the horizontal planes. The lateral protective reaction involves increased trunk flexor tone toward the force and an outreached hand and limb away from the force; it usually emerges by 6 months old and is required for the development of stable, independent sitting ( Fig. 3.8 ). At 10 months old, the child develops the forward protective or parachute reaction, an outstretching of both arms and legs when the body is abruptly moved head first in a downward direction ( Fig. 3.9 ). The forward protective (parachute) reaction is a programmed reflex that protects the head if the child falls from standing or walking and is generally seen just before these motor skills develop.


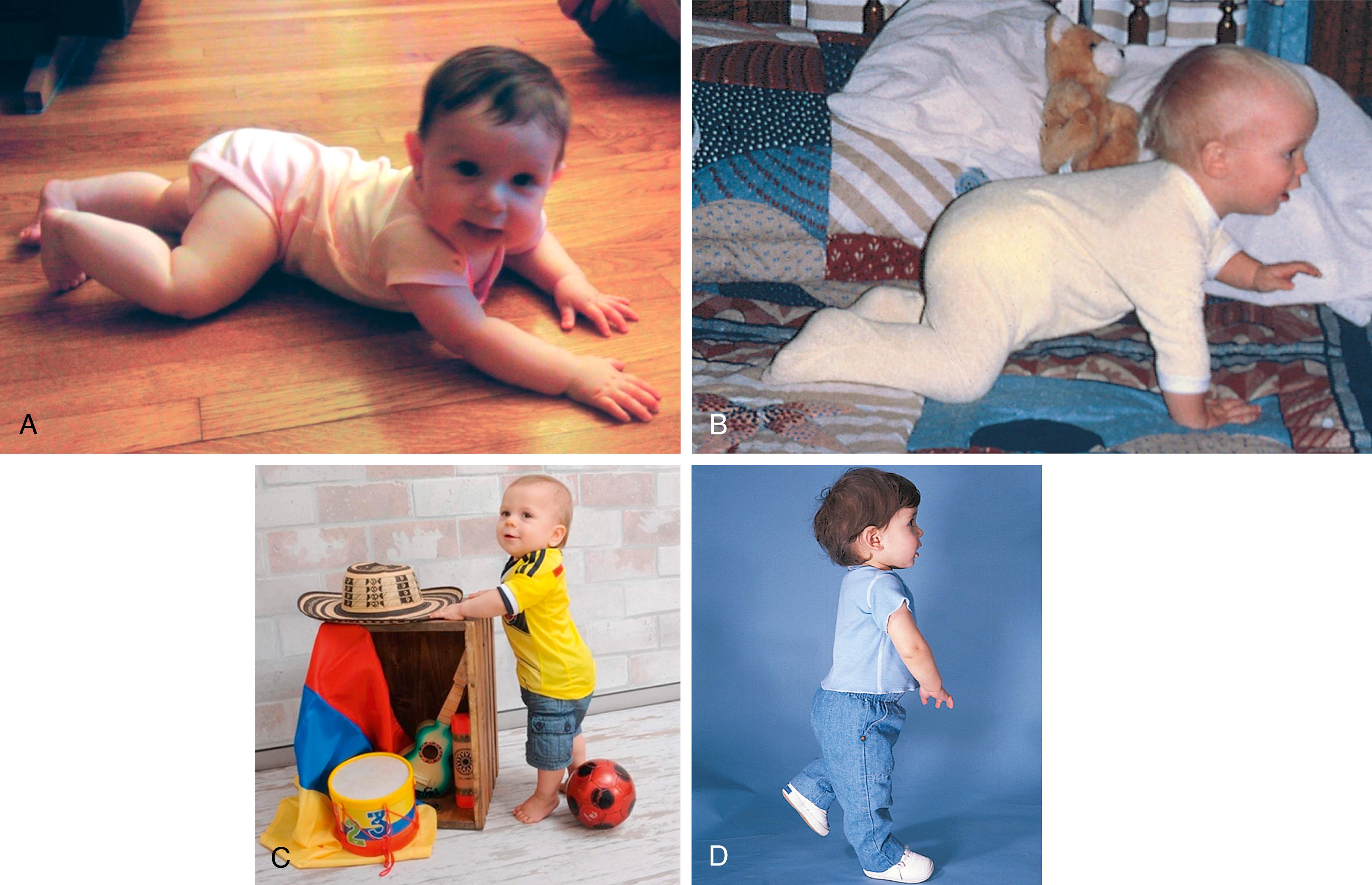
Gross motor milestones can also be described in terms of locomotion ( Table 3.3 ). Prone-to-supine (front to back) rolling may be accomplished by 3 to 4 months of age, after the child gains sufficient control of shoulder and upper trunk musculature to prop up on the arms. Supine-to-prone (back to front) rolling requires control of the lumbar spine and hip region, as well as the upper trunk; this is usually present by 5 to 6 months of age. Since the introduction of the Safe to Sleep campaign (formally known as the Back to Sleep campaign that included recommendations for supine sleeping to prevent sudden infant death syndrome), prone-to-supine rolling may appear later, at 5 to 6 months, because the child has had little experience in the prone position; it may actually occur later than supine-to-prone rolling, demonstrating the impact of experience on gross motor skill development. Creeping (also called commando or army crawling ), accomplished at 5 to 6 months of age ( Fig. 3.10A ), involves coordinated pulling with upper arms and passive dragging of the legs, akin to a soldier trying to keep the body low to the ground. By 6 to 9 months old, as voluntary control moves to the hips and legs, the child can get up on the hands and knees, assuming a quadruped position, and crawl (see Fig. 3.10B ). The next developmental milestone is supported standing. By 9 to 10 months old, many children like to demonstrate this new skill by holding on to a parent or by walking independently while holding on to furniture. This is called cruising (see Fig. 3.10C ). Increased control to the feet and disappearance of the plantar grasp reflex allow the child to walk independently. Walking three steps alone occurs at a median age of approximately 12 months old, with a range of 9 to 17 months old (see Fig. 3.10D ).
| Task | Age Range a |
|---|---|
| Sits alone momentarily | 4–8 months old |
| Rolls back to stomach | 4–10 months old |
| Sits steadily | 5–9 months old |
| Gets to sitting | 6–11 months old |
| Pulls to standing | 6–12 months old |
| Stands alone | 9–16 months old |
| Walks three steps alone | 9–17 months old |
a Wide ranges in the attainment of these gross motor milestones in healthy children are the rule rather than the exception.
Further progress in gross motor skills continues throughout childhood. The developmental sequence beyond walking incorporates improved balance and coordination and progressive narrowing of the base of support. The sequence of milestones is as follows: running, jumping on two feet, balancing on one foot, hopping, and skipping. The child simultaneously learns to use muscle groups in timed sequences. By 13 to 15 months old, the child walks well; by 36 months old, he or she can balance on one foot for 1 second. Most children can hop by age 4. They can throw a ball overhand by 22 to 24 months old, but catching develops later, at almost 5 years old.
Evaluation of gross motor skills can begin when the pediatrician enters the office for a well-child visit. The typical 2-month-old infant is cradled in the parent’s arms; the 4 month old has enough strength to support her back when held inside her arms by her parent’s hands but not enough strength to sit on her own ( Fig. 3.11 ); the 6-month-old child is sitting with minimal support on the parent’s lap or on the examination table next to the parent; and the 12 month old is cruising or toddling through the room. Although age of onset and duration of each stage vary, the 6-month-old infant who lacks head control on the pull-to-sit maneuver, who cannot clear the table surface with the chest by supporting weight on the arms when prone, who shows no head righting, or who has persistent primitive reflexes (e.g., a complete Moro response or ATNR) is at sufficient variance from peers to warrant evaluation for a possible neuromuscular disorder. In addition, when gross motor delays are found in association with verbal and social delays, asymmetric use of one limb or one side of the body, or loss of previously attained milestones, diagnostic evaluation is indicated.

Evaluation of the older infant or toddler who has mastered walking can occur during the physical and neurologic evaluation. Many children enjoy showing off their abilities to jump, balance on one foot, hop, and skip. Some pediatricians use gross motor testing to establish rapport at the outset of a physical examination. However, because an aroused preschooler may not cooperate with a sedentary evaluation of heart or ears, many pediatricians hold off on motor evaluation until the conclusion of the examination.
At the discovery of delayed or atypical development, the pediatrician’s first task is to develop a differential diagnosis and a plan to establish the specific diagnosis. Potential causes of delayed gross motor development are listed in Table 3.4 . Another equally important task is to recommend a treatment program. Early intervention programs and/or physical therapy should be actively considered for children with motor difficulties during infancy through preschool. Adaptive physical education programs are available for older children with mild problems that do not seriously impair function.
| Global Developmental Delay | Motor Dysfunction | Motor Intact But Otherwise Restricted |
|---|---|---|
|
|
|
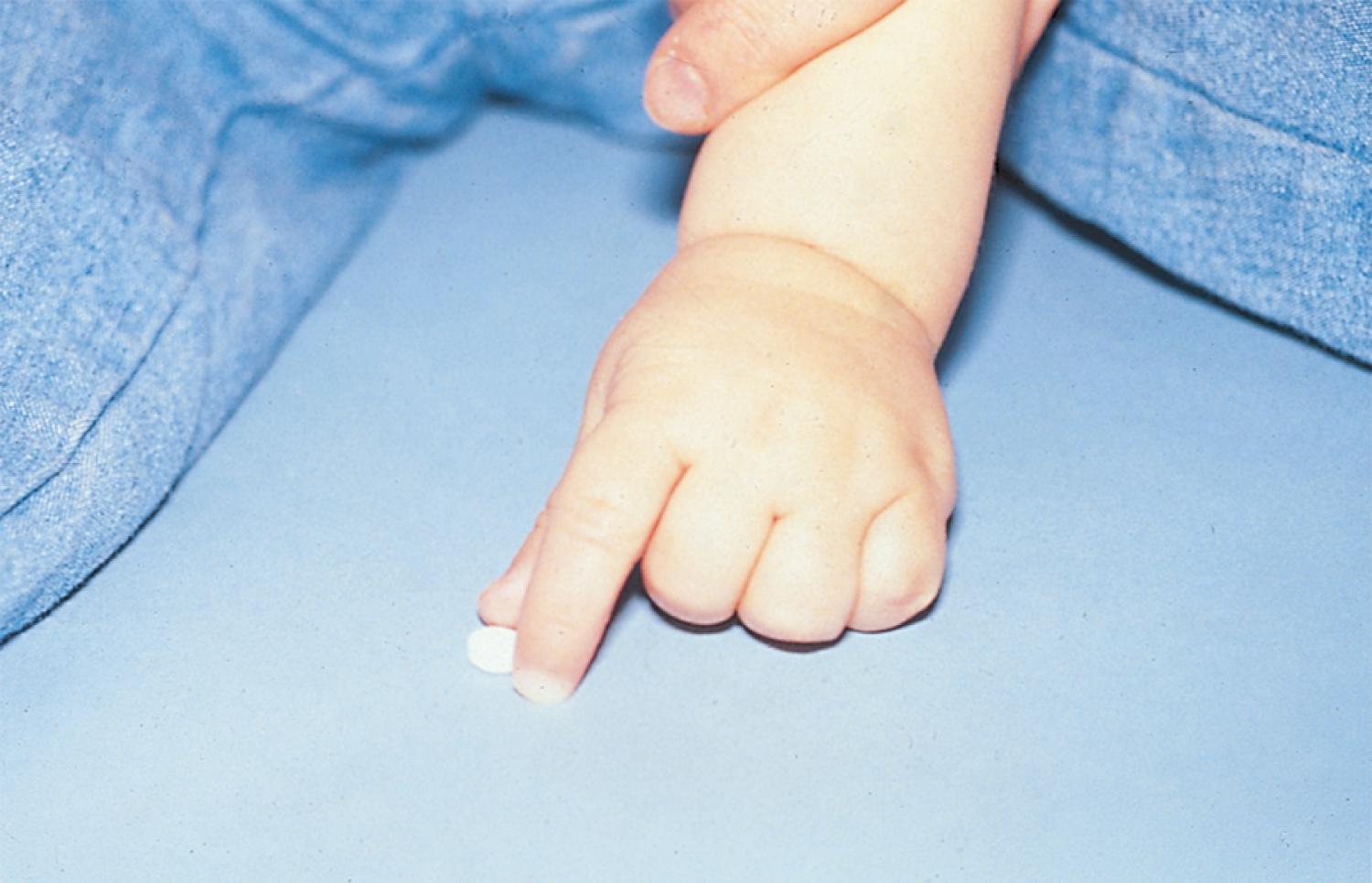
At birth, the neonate’s fingers and thumb are typically tightly fisted. A newborn baby grasps reliably and reflexively at any object placed in the palm ( Fig. 3.12 ) and cannot release the grasp. Because of this reflex, the newborn’s range of upper extremity motion is functionally limited. Normal development leads to acquisition of a voluntary grasp.

The reflexive palmar grasp gradually disappears at approximately 1 month old. From that point, the infant gains control of fine motor skills in an orderly progression. In the second or third month of life, the infant initially brings both hands together for midline hand play ( Fig. 3.13 ). Shortly after that, the baby begins to swipe at objects held in or near the midline ( Fig. 3.14 ). It is through swiping that the infant increases the exploratory range and fine-tunes the small muscles of the wrist, hand, and fingers.

Improvements in fine motor control increase sensory input from the hands and permit greater hand manipulation through space. By 2 to 3 months old, the hands are no longer tightly fisted, and the infant may begin sucking on a thumb or individual digit rather than the entire fist for self-comfort. A 3 month old is usually able to hold an object in either hand if it is placed there, although the ability to grasp voluntarily or to release that object is limited. At approximately 4 to 5 months old, infants begin to use their hands as entire units to draw objects toward them. Neither the hand nor the thumb functions independently at this point, and, consequently, the child uses the hand like a rake.
Next, the child develops the ability to bend the fingers against the palm (palmar grasp), squeeze objects, and obtain them independently for closer inspection ( Fig. 3.15 ). Differentiation of the parts of the hand develops in association with differentiation of the two hands. Between 5 and 7 months old, the infant can use hands independently to transfer objects across the midline. Further differentiation of the plane of movement of the thumb allows it to adduct as the fingers squeeze against the palm in a radial palmar or whole-hand grasp. With time, the thumb moves from adduction to opposition. The site of pressure of the thumb against the fingers moves away from the palm and toward the fingertips, in what is called an inferior pincer or radial digital grasp, seen around 9 months old ( Fig. 3.16 ). By 10 months old, differentiated use of the fingers allows the child to explore the details of an object.

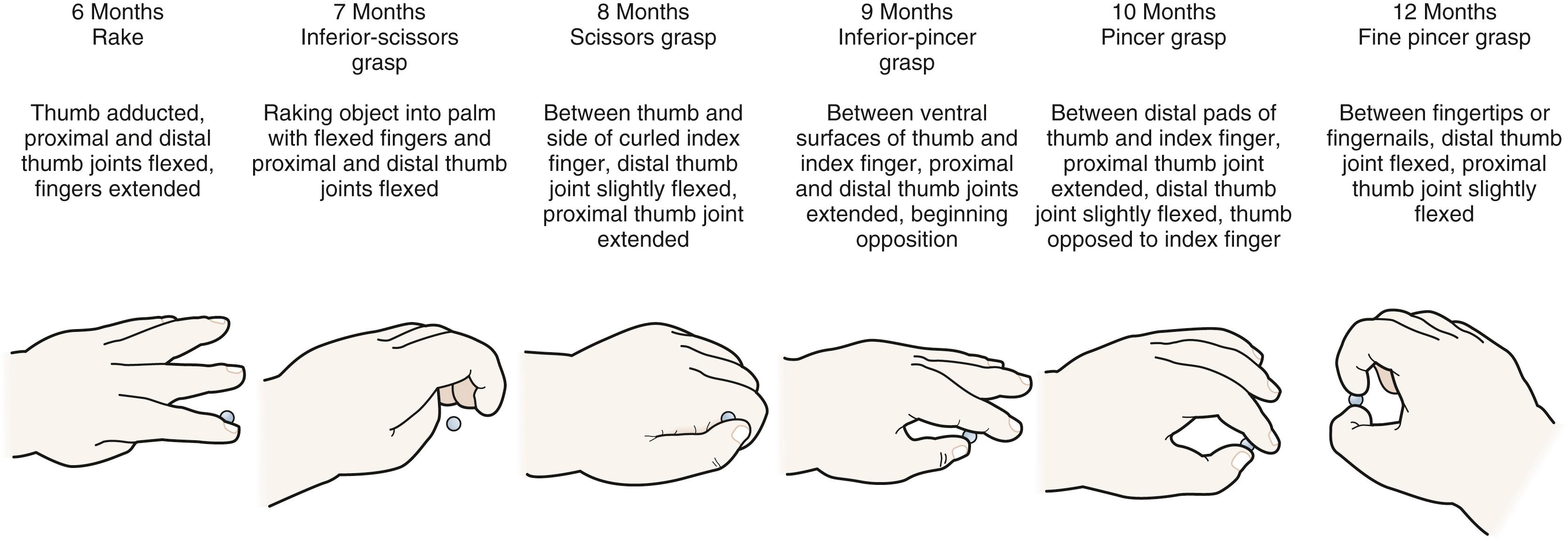
Between 9 and 12 months old, the fine pincer grasp develops, allowing opposition of the tip of the thumb and the index finger ( Fig. 3.17 ). This milestone enables the precise prehension of tiny objects (see Fig. 3.17 ). The infant uses this skill in tasks such as self-feeding and exploration of small objects. By 1 year old, the infant can position the hand in space to achieve vertical or horizontal orientation before grasping or releasing an object.
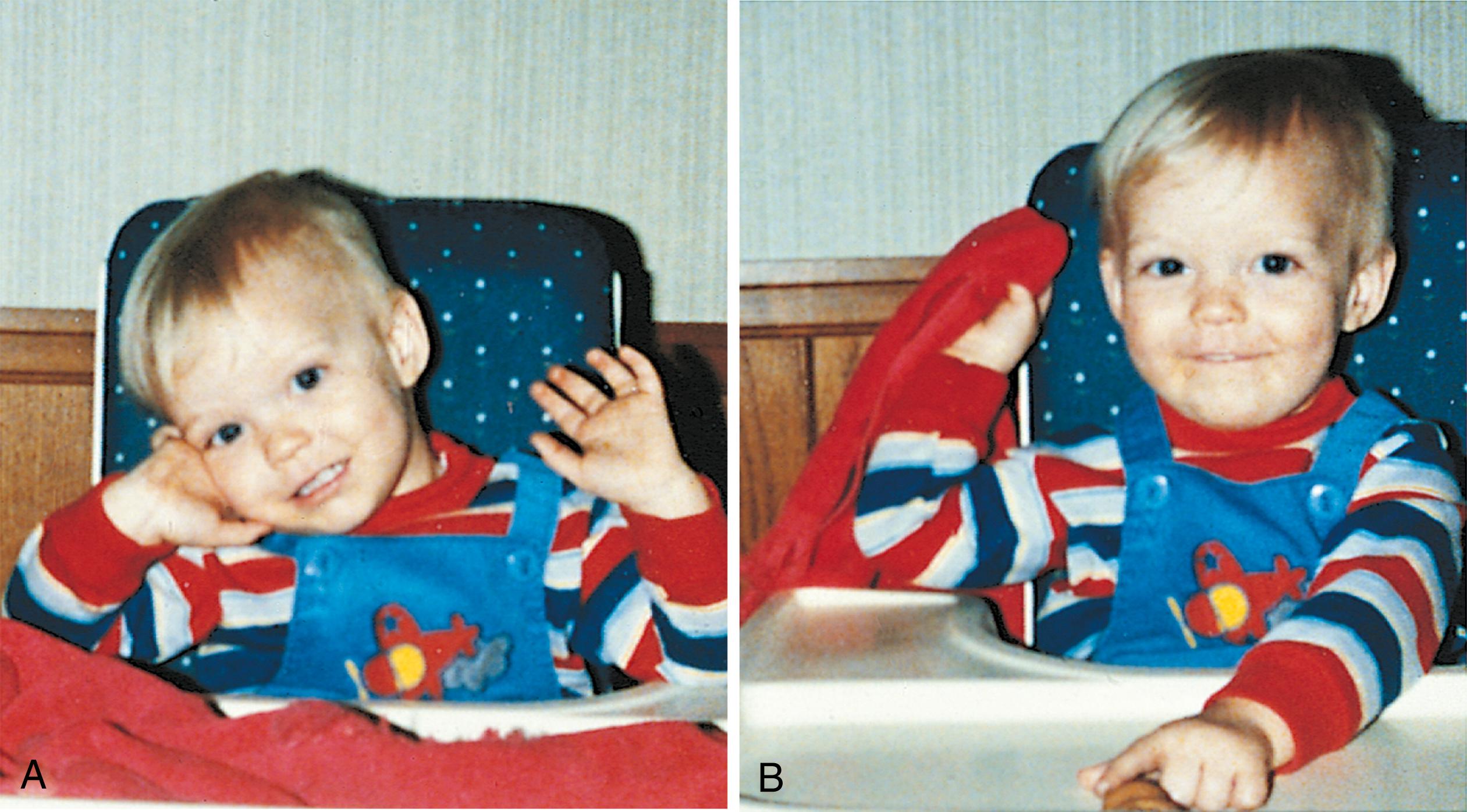
Early in the second year of life, the young child uses the grasp to master tools and to manipulate objects in new ways. Dropping and throwing, stacking, and putting objects in and out of receptacles become favorite pastimes. Mastery of the cup and spoon supplement or replace finger feeding as a more efficient and less messy means of eating ( Fig. 3.18 ).

Advancements in fine motor planning and control can be demonstrated through the child’s ability to stack small cubes. After children master stacking, they show consistent patterns of improvement in reproducing structures that they have watched the examiner assemble ( Fig. 3.19 ). The child’s ability to copy a variety of drawings also improves during this period.
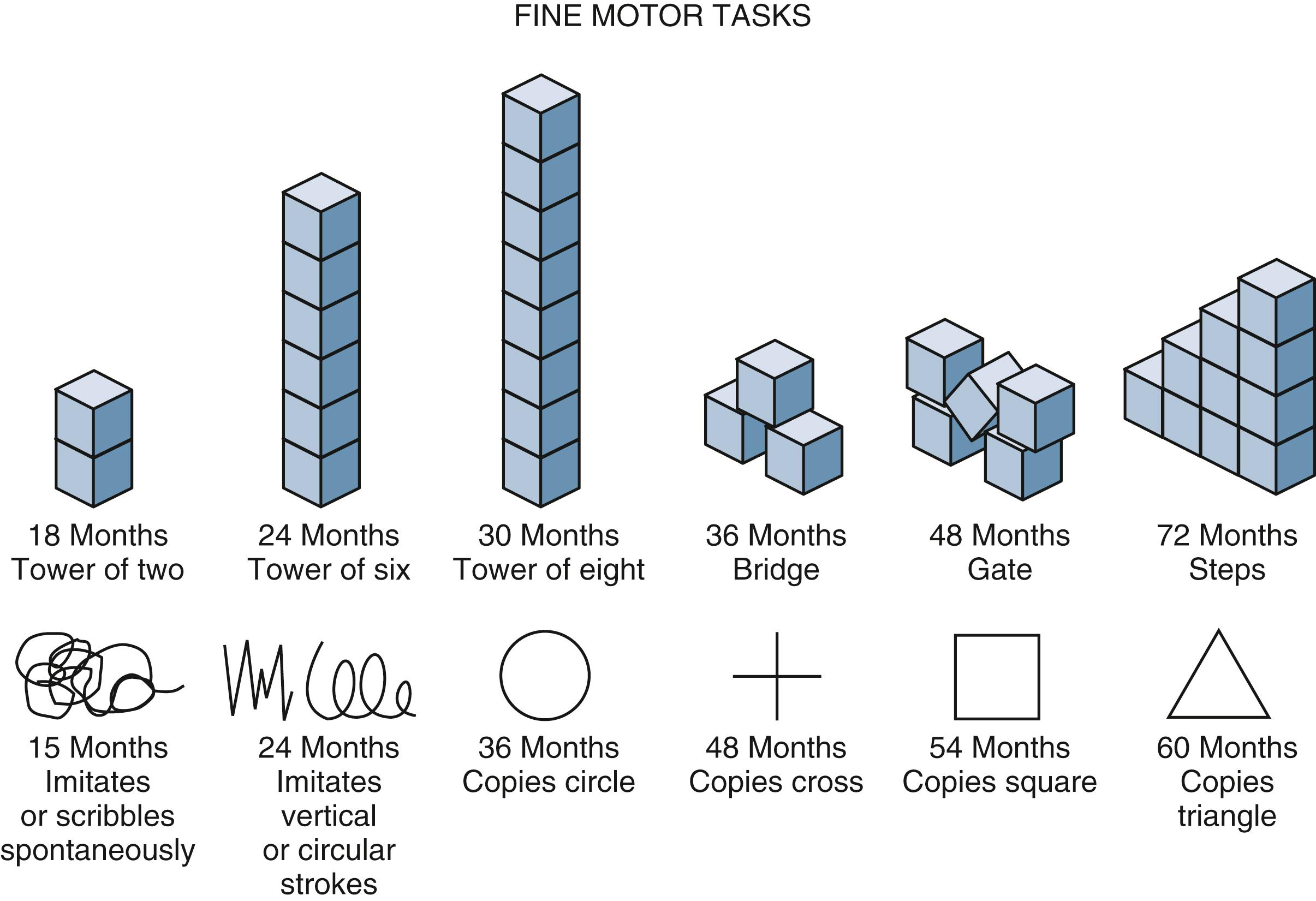
Fine motor testing can be incorporated readily into a physical examination and may uncover problems with vision, neuromuscular control, or perception, in addition to difficulties with attention or cooperation. The 4-month-old child usually can be encouraged to grasp a small toy or tongue depressor (see Fig. 3.15 ). By 6 to 9 months old, two tongue depressors should be offered, one for each hand, because the child can operate the hands independently. At 9 to 12 months old, the child spontaneously points with an isolated index finger or picks up small objects with a fine pincer grasp. Children younger than 18 months old generally use both hands equally well. Therefore the child who develops consistent handedness with neglect of the other limb before that time should have a neurodevelopmental assessment. The child who has not developed use of the thumb and pincer grasp by 18 months old deserves further evaluation, as does the child who is unable to copy vertical or horizontal lines by 3 years old or circles by 4 years old.
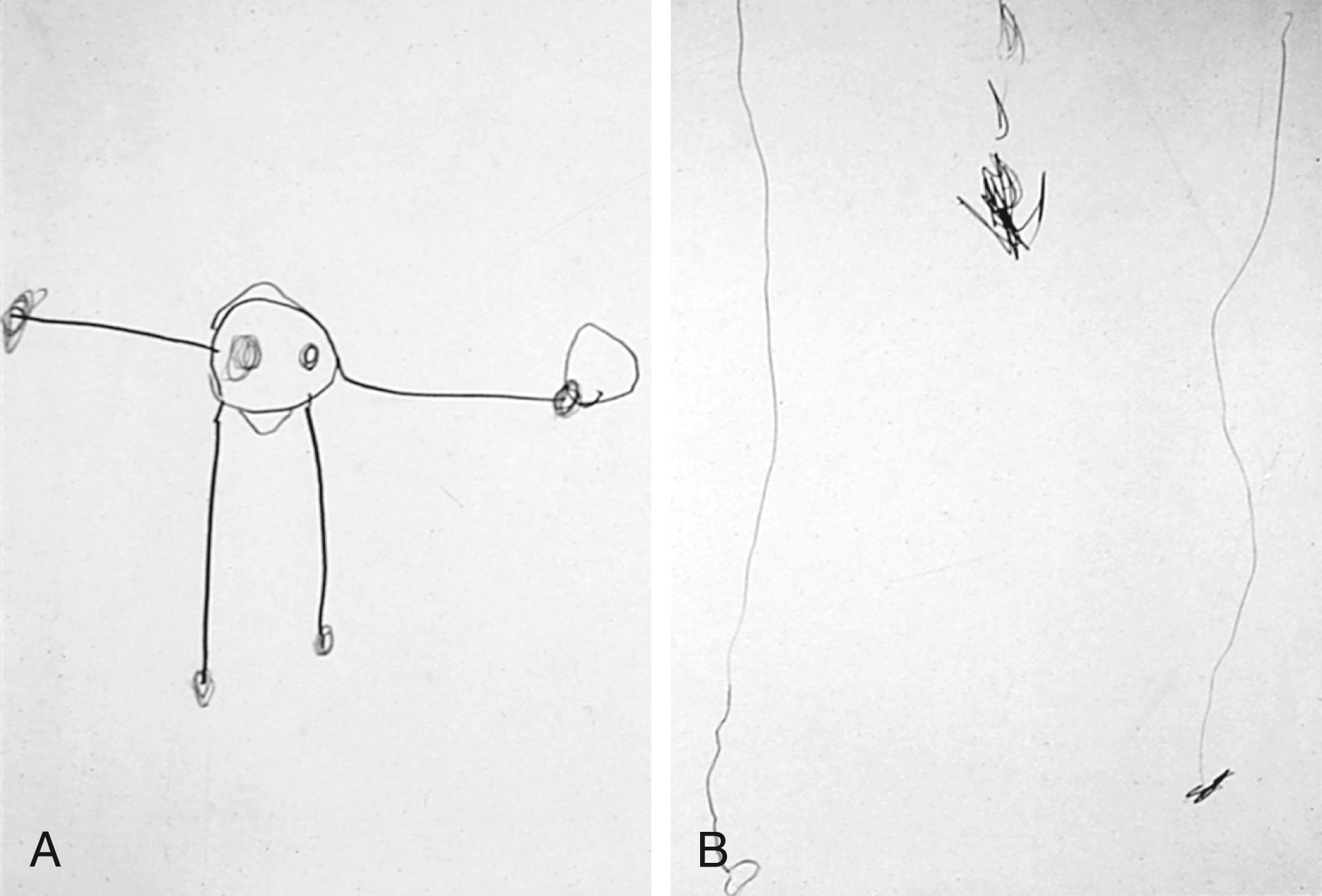
Fine motor activities can be engaging and nonthreatening to the preschool and school-age child; these activities allow the physician to make valuable observations and to establish rapport. The physician can routinely request that the child older than 3 years old use the waiting time or the period of history-taking to draw a self-portrait. These drawings provide a wealth of information not only on the child’s capacities for fine motor control but also on cognitive development and social and emotional functioning. A quick method for analyzing the age level of a drawing is to count the number of features in the drawing. The child receives one point for each of the following features: two eyes, two ears, a nose, a mouth, hair, two arms, two legs, two hands, two feet, a neck, and a trunk. Each point converts to the value of 3 months (or four points to a year) added to a base age of 3 years old ( Fig. 3.20 ). Screening tests and standardized measures, such as the Beery-Buktenica Developmental Test of Visual-Motor Integration, sixth edition, can also be used to assess fine motor skills.
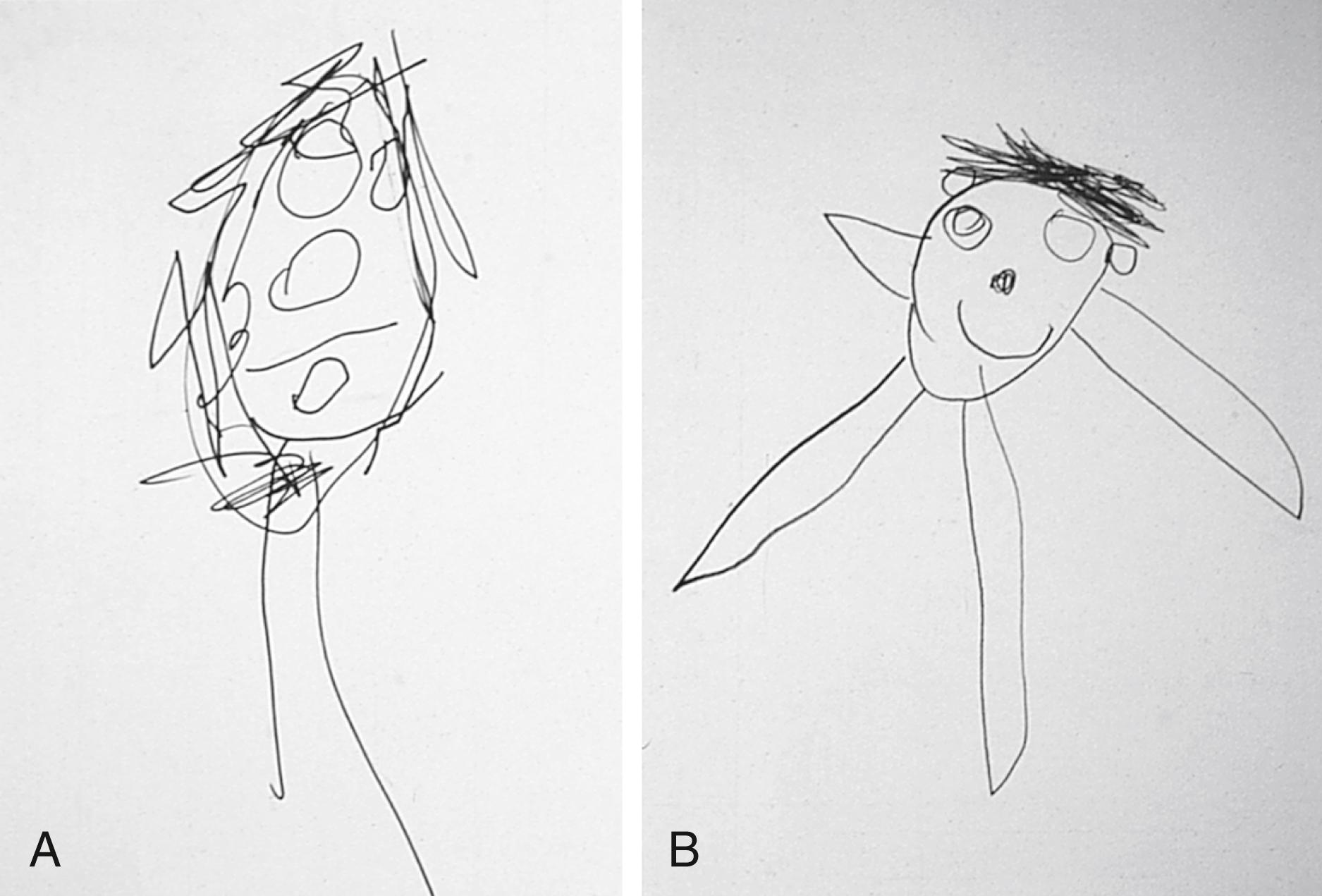
Children with brain damage are at increased risk for problems with perceptual/fine motor integration, even in the absence of visual problems and with minimal involvement of the upper extremities ( Fig. 3.21 ).
Fine motor skills figure prominently in self-care activities. The child who lacks the dexterity to complete simple daily activities (e.g., zipping, buttoning, or cutting with a knife) may lack the self-esteem that accompanies independent self-care. Furthermore, children who continually depend on parents or teachers may be viewed by peers; teachers; or, perhaps most damagingly, by themselves as less mature. In the school-age child, inefficient fine motor skills can have a significant impact on the ability to write legibly or to compete with peers in timed tasks, even if the child has sound academic and conceptual skills. Occupational therapy and special education may enhance fine motor skills and emotional development in these children.
Innate sensory capabilities serve as the building blocks of cognitive development. Even at birth, the healthy neonate responds to visual and auditory stimuli. These responses, like the primitive reflexes, take the form of integrated patterns of activity.
The visual acuity of the full-term infant is estimated to fall between 20/200 and 20/400 and improves rapidly over the first year of life. Even at birth, it is possible to get the full-term newborn to fix on faces 9 to 12 inches from the face and to track objects horizontally at least 30 degrees ( Fig. 3.22 ). Some neonates, if assessed when calm and fully alert, can track objects 180 degrees across the visual field. Newborns also respond to sound, typically quieting in response to a human voice, rattles, or music. In the first days of life, many infants turn to the source of sound and search for it with their eyes. These maneuvers, found on the Brazelton Neonatal Behavioral Assessment Scale, are useful in demonstrating neurobehavioral characteristics of newborns.

Examination must take place at optimal times when the infant is alert; if the infant is drowsy or agitated, the ability to track visually or to search for sounds is compromised. If, when assessed under optimal circumstances and when fully alert, infants do not demonstrate horizontal tracking of objects, do not look at the toys or people with whom they are involved, or hold their heads in unusual positions, the physician should recommend prompt evaluation for abnormal visual perception or central nervous system development. New technology offers the use of vision screener devices that allow for vision screenings as early as 6 months of age with minimal collaboration from the infant or the child. These vision screener devices use lights and sounds to help engage children from a three-foot distance.
During the first 2 years of life, the sensorimotor period of development, the young child’s cognitive abilities can be surmised only through use of the senses and through the physical manipulation of objects. The nature of an infant’s thinking is assessed through concrete interaction with the environment. During this period, the child develops an understanding of the concept of object permanence, the ability to recognize that an object exists even when it cannot be seen, heard, or felt. Simultaneously, the child develops an understanding of cause-and-effect relationships. Progress in the child’s development of these concepts is an important prerequisite to the development of pure mental activity, reflected in the ability to use symbols and language.
Early progress in the development of object permanence is indicated by the infant’s continued though brief gaze at the site where a familiar toy or face has disappeared. At this point, children also repeat actions that they have discovered will produce interesting results. Between 4 and 8 months of age, infants become interested in changes in the position and appearance of toys. They can track an object visually through a vertical fall ( Fig. 3.23 ) and search for a partially hidden toy. They also begin to vary the means of creating interesting effects. In these early months, the baby’s play consists of exploring toys to gain information about their physical characteristics. Activities such as mouthing, shaking, and banging can provide sensory input about an object beyond its visual features. However, when mouthing of toys persists as the predominant mode of exploration after 12 to 18 months of age, assessment of cognitive function is warranted.

At approximately 9 to 12 months of age, infants can locate objects that have been completely hidden ( Fig. 3.24 ). Not surprisingly, peek-a-boo becomes a favorite pastime at this point. Later, the infant can crawl away from the mother and recall where to return to find her.
As children near 1 year old, interest in toys extends beyond physical properties (e.g., color, texture). These children may begin to demonstrate their awareness that different objects have different purposes. For example, a child might touch a comb to the hair in a meaningful non-pretend action, which is typical of the 9- to 12-month age range. Beyond 1 year old, children begin to vary their behavior to create novel effects. They no longer need to be shown how to work dials or knobs, nor do they need to hit something by accident to discover the interesting effect that will result.
By 18 months old, children can deduce the location of an object even if they have not seen it hidden from view. They can maintain mental images of desired objects and develop plans for obtaining them. The child’s understanding of causality also advances; cause-and-effect relationships no longer need to be direct to be appreciated ( Fig. 3.25 ). These developments herald the beginning of a new stage in cognitive development, that of symbolic thinking. They also indicate that distraction may not succeed in drawing a child away from a desired object; a direct request is required.

In the second year of life, the child demonstrates mental activity independent of sensory processing or motor manipulation. For example, the child observes a television superhero performing a rescue mission and hours later reenacts the scene with careful precision. Clearly, the child has a mental image of the event and uses it to generate the delayed imitation.
As children develop the capacity for pure mental activity, they use objects to represent other objects or ideas. Genuine pretending begins; the child engages in playful representation of commonplace activities, using objects for their actual purpose but accompanied by exaggerated sounds or gestures. Pretend actions are combined into a series of events. For example, the child may hold a phone to the ear and then to a doll’s ear or may feed a teddy bear and then put the bear to bed.
The next stage in development allows the child to plan pretend activities in anticipation of the play theme to come, combining many steps into the play. Preparing for play indicates an advance in pretending beyond that of improvising with the objects at hand. For example, the child might be seen preparing the play area or searching for needed objects and announcing what the objects are meant to represent.
The preschool child has well-developed capabilities for mental representation and symbolic thinking. However, the dominance of sensory input, limited life experience, and a lack of formal education lead to a unique and charming logic during this period. Preschoolers often assume that all objects are alive like themselves. For example, a car and a tricycle may be seen as alive, perhaps because they are capable of movement. Similarly, children claim that the moon follows them on an evening walk.
The logic of the preschooler is in large part influenced by the appearance of objects. Because an airplane appears to become smaller as it takes off, the preschooler may assume that all the people on the plane become smaller as well. Piaget demonstrated that preschoolers seem to think that number and quantity vary with appearance ( Fig. 3.26 ). Under certain circumstances, a 4-year-old child may show understanding that a quantity remains invariant unless something is added or subtracted. However, that same child may insist that two rows of pennies are different in number simply because of a compelling visual difference between them.
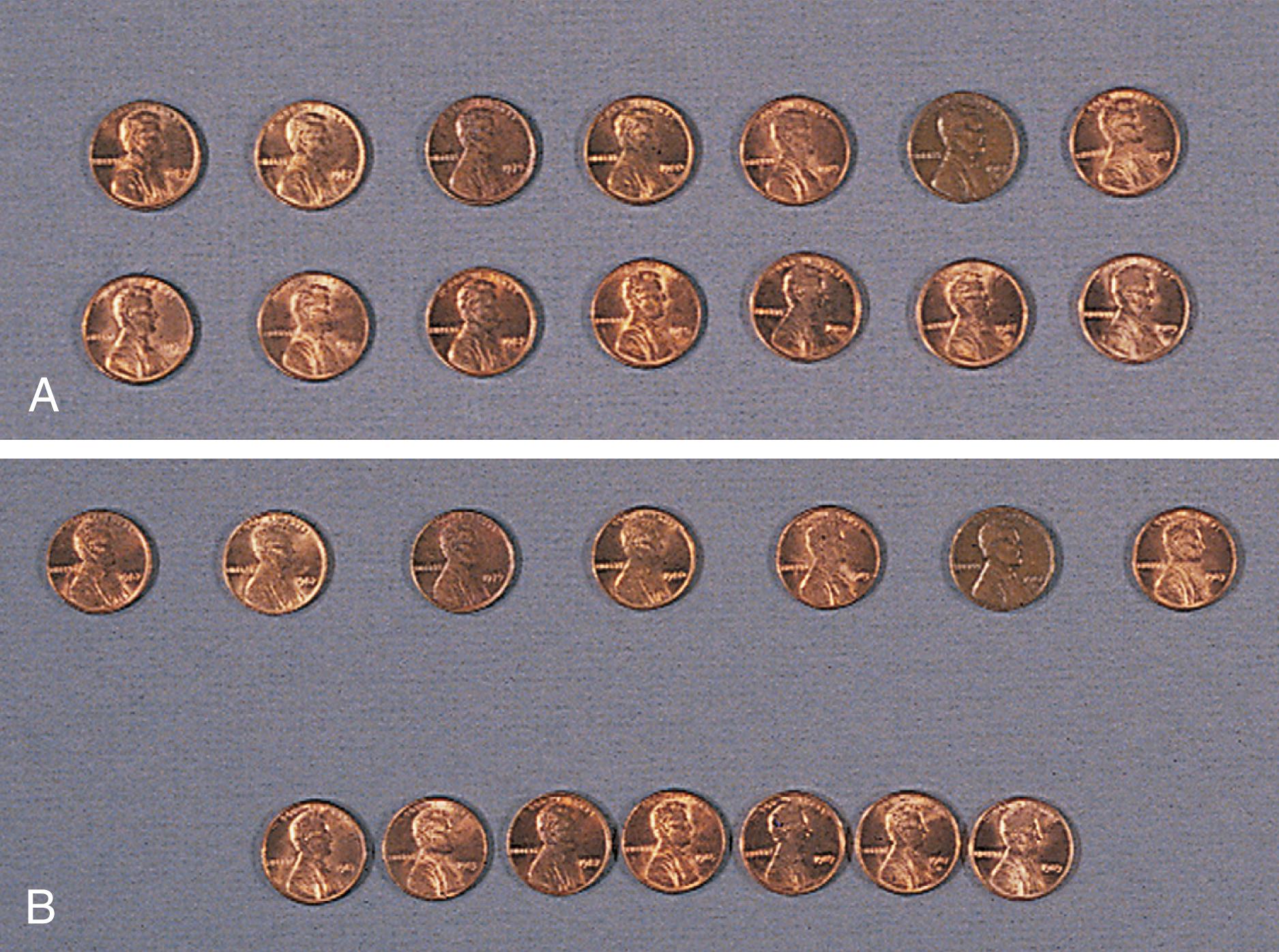
The immature logic of the preschooler is gradually replaced by conventional logic and wisdom. School-age children follow logic akin to adult reasoning, at least when the stimuli are concrete. Faced with the same question about the pennies, they readily acknowledge that the two rows have the same number regardless of their visual appearance (see Fig. 3.26 ). They also know that the airplane just looks smaller because it has moved farther from the viewer, and they giggle at the suggestion that the people on the plane have shrunk. Their logical limitations become obvious when they must reason about the hypothetical or the abstract.
Adolescents, particularly those with the benefits of formal education, tend to extend logical principles to increasingly diverse problems. They can generate multiple logical possibilities systematically when faced with scientific experiments, and they can also consider hypothetical problems. These principles of reasoning are applied not only to schoolwork but also to social situations.
The pediatric office assessment of cognitive ability in the preverbal child is best accomplished by observation of play. The pediatrician can induce the infant to look for a hidden toy or to play a game of peek-a-boo; the infant’s anticipation of reappearance indicates the development of the concept of object permanence. Similarly, the toddler’s ability to play with a toy telephone indicates the emergence of symbolic thought. Beyond the toddler stage, the physician typically relies on conversation and language ability to assess levels of cognitive skill. Screening tests are particularly useful for determining whether cognitive and language skills are within the normal range. Children with language delays may need a formal nonverbal assessment of cognitive abilities by a psychologist or developmental subspecialist.
For the parents, a delay in a child’s attainment of a well-known milestone may create tremendous fear about ultimate learning potential. In many cases, such parental concerns are put to rest at that time when the physician determines that the child’s learning to date is age appropriate. If a child does show delays in cognitive development, the physician should generate a differential diagnosis ( Table 3.5 ) from knowledge of the child’s level of functioning in multiple domains, history, and physical examination.
| Findings Sometimes Present on History or Examination | Possible Disorder |
|---|---|
| Decreased vision or hearing | Specific sensory deficits |
| Staring spells, motor automatism | Seizure disorders |
| Lethargy, ataxia | Overmedication with anticonvulsants |
| Myxedema, delayed return on DTRs, thick skin and tongue, sparse hair, constipation, increased sleep, coarse voice, short stature, goiter | Hypothyroidism |
| Irritability, cold sweats, tremor, loss of consciousness | Hypoglycemia |
| Unexplained bruises in various stages, failure to thrive | Child abuse and neglect |
| Short stature, weight below third percentile | Malnutrition or systemic illness producing failure to thrive |
| Poor purposeful attending in multiple settings | ADHD |
| No specific findings | Environmental deprivation |
| Anemia | Iron deficiency or lead exposure |
| Absent venous pulsations or papilledema on funduscopic examination, morning vomiting, headaches, brisk DTRs in lower extremities | Increased intracranial pressure |
| Vomiting, irritability and seizures, failure to thrive | Some inborn errors of metabolism (e.g., methylmalonic acidemia) |
| Hepatomegaly, jaundice, hypotonia, susceptibility to infection, cataracts | Galactosemia |
| Fair hair, blue eyes, “mousy” odor to urine | Phenylketonuria |
| Ongoing evidence of active or progressive disease | Chronic infection, inflammatory disease, malignancies |
Parents should be given information about their child’s delay as early as possible. Pediatricians serve a critical role in referring children to early intervention or special education programs and in monitoring their progress. Active communication between the providers of early intervention and the physician assists a comprehensive and cohesive approach.
Physicians frequently need the consultation of colleagues in psychology and education to assess the cognitive abilities of their older preschool and school-age patients. Several methods have been devised for formal assessment of mental achievement, and almost all parents are familiar with the term intelligence quotient, or IQ. Although not a means of comprehensively assessing all mental capabilities, normal IQ scores are (albeit imperfect) predictors of which children will have the cognitive and intellectual abilities to perform well in school. Low IQ scores may reflect a child’s poor ability to grasp new concepts, or they may indicate other issues, such as poor purposeful attending behaviors, as seen in depression or in attention-deficit/hyperactivity disorder (ADHD). Low scores may also reflect poor social adjustment or limitations in test-taking capabilities, such as sitting in a chair at a table and applying maximal effort to a task requested by an unfamiliar authority figure. Frequently, low scores result from a combination of difficulties in several areas.
If children with sensory or motor impairments are tested with instruments normalized on able-bodied children, they often obtain low scores. Different assessment techniques have been devised to circumvent specific disabilities while obtaining information about a child’s cognitive abilities; these are typically administered by psychologists, child development specialists, or special educators ( Table 3.6 ).
| Type of Scale | Test(s) Used | Age Range |
|---|---|---|
| Standard intelligence scales | Stanford-Binet Intelligence Scales-IV | 2 years old to adult |
| Wechsler Intelligence Scale for Children-IV | 5–16 years old | |
| Nonverbal intelligence scale | Leiter International Performance Scale-R | 2–18 years old |
| Infant development tests | Bayley Scales of Infant Development-III | 0–42 months old |
| Gesell Developmental Schedules | 0–5 years old | |
| Developmental scale for the visually impaired | Reynell-Zinkin Developmental Scales for Young Children with Visual Impairments | 0–5 years old |
| Adaptive behavior | Vineland Adaptive Behavior Scales-II | 0–18 years old |
| Adaptive Behavior Assessment System-II | 0–21 years old |
Assessment of a child’s abilities to learn must go beyond standardized IQ tests. For example, some children who can score in the normal range on IQ tests are unable to learn to read. A diversified and individualized assessment process should precede any educational recommendation. The pediatrician, in the role of advocate, should ensure that assessments include information about the child’s strengths and weaknesses, because educational planning should involve attention to all aspects of the child’s abilities. Moreover, the pediatrician can encourage families to maintain an active, decision-making role in their children’s education.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here