Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Demyelinating and inflammatory disorders are neuroimmunologic disorders in which there is an exaggerated immune response to the central nervous system (CNS, Fig. 6.1 ). Neuroimmune disorders have become increasingly recognized as more prevalent than was previously understood, and the understanding of these disorders is rapidly changing and continually evolving. Advances in autoantibodies detection, combined with imaging, clinical signs and symptoms, and cerebrospinal fluid (CSF) findings have led to better understanding and characterization of several of these disorders. Neuroimmune disorders may be triggered by a recent infection or presence of a tumor or may be unknown. Genetic contributions remain to be investigated, but some associations have been found, such as the association between herpes simplex virus (HSV) encephalitis with inborn errors of antiviral interferon immunity, and influenza-mediated acute necrotizing encephalopathy with mutations in heat-shock protein. Most neuroimmune disorders occur in children who are otherwise previously healthy and had normal development. Clinical features include abrupt onset of neurologic signs and symptoms and often a recent history of illness. CSF testing is important for detecting autoantibodies as well as excluding an acute infection. The initial treatment of most neuroimmunologic disorders includes corticosteroids, intravenous immunoglobulin, or plasma exchange, depending on the diagnosis and severity, and has the primary goal of immunosuppression and immunomodulation.
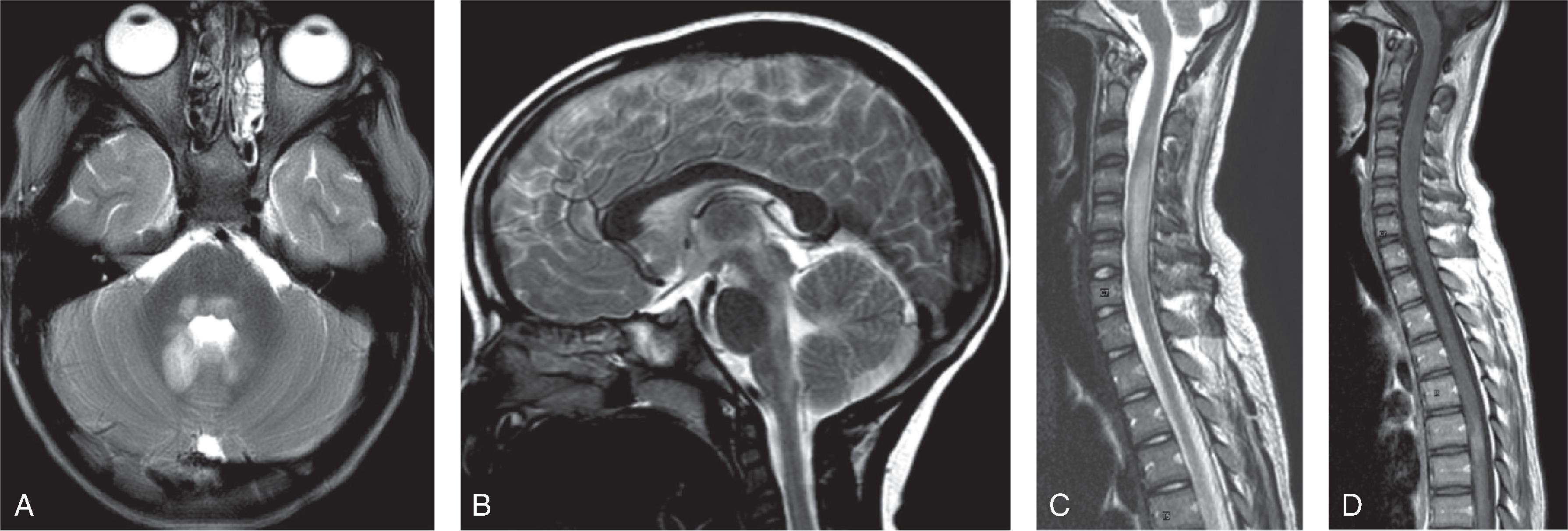
The primary imaging modality for detection of demyelinating and inflammatory disorders is MRI, typically of the brain and spine performed without and with contrast. This allows for detection of the full extent of disease, detection of all imaging features, differentiation from disorders that may mimic a demyelination or inflammatory process, and establishment of baseline imaging against which to compare to future imaging. Understanding that there is a wide range of imaging patterns possible with many of these disorders is the first step in the consideration of these neuroimmune disorders in children. Several of these disorders have imaging patterns that can mimic infections or even tumor. Although these disorders involve a wide range of brain, optic nerve, and spine involvement, recognition of patterns of involvement provides clues to the diagnosis. For example, lesions in multiple sclerosis predominate in the white matter and more typically have short-segment spinal cord lesions, whereas neuromyelitis optica (NMO) more often involves the thalamus, hypothalamus, and brainstem and has long segment spinal cord lesions. This chapter discusses the common demyelinating and inflammatory disorders in the brain in children and emphasizes several of the clinical and imaging predilections.
Immune-mediated, monophasic inflammatory and demyelinating disorder involving gray and white matter
Typically (∼75%) occurs within 2 to 4 weeks of viral infection or immunization
Most commonly seen in pediatric patients; may occur in adults
Less common multiphasic pattern defined as two episodes separated by 3 months, not followed by additional events (<10%). Repeat episodes should raise concern for demyelinating disorders, such as multiple sclerosis (MS), anti–myelin oligodendrocyte glycoprotein (MOG), or NMO.
Symptoms include encephalopathy that cannot be explained by fever, headache, meningismus, nausea, vomiting, pyramidal signs, cranial nerve palsies, vision loss due to optic neuritis, speech impairment, or hemiparesis
Anti-MOG antibodies may be transiently positive
Early use of corticosteroid therapy improves symptoms and prognosis; 10% to 20% have persistent or chronic symptoms
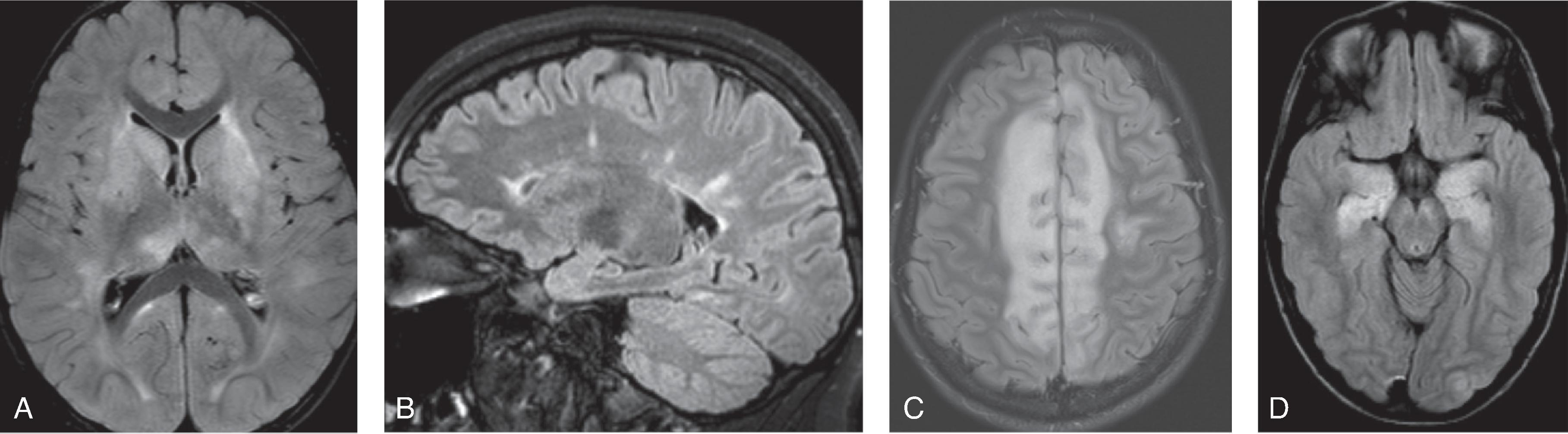
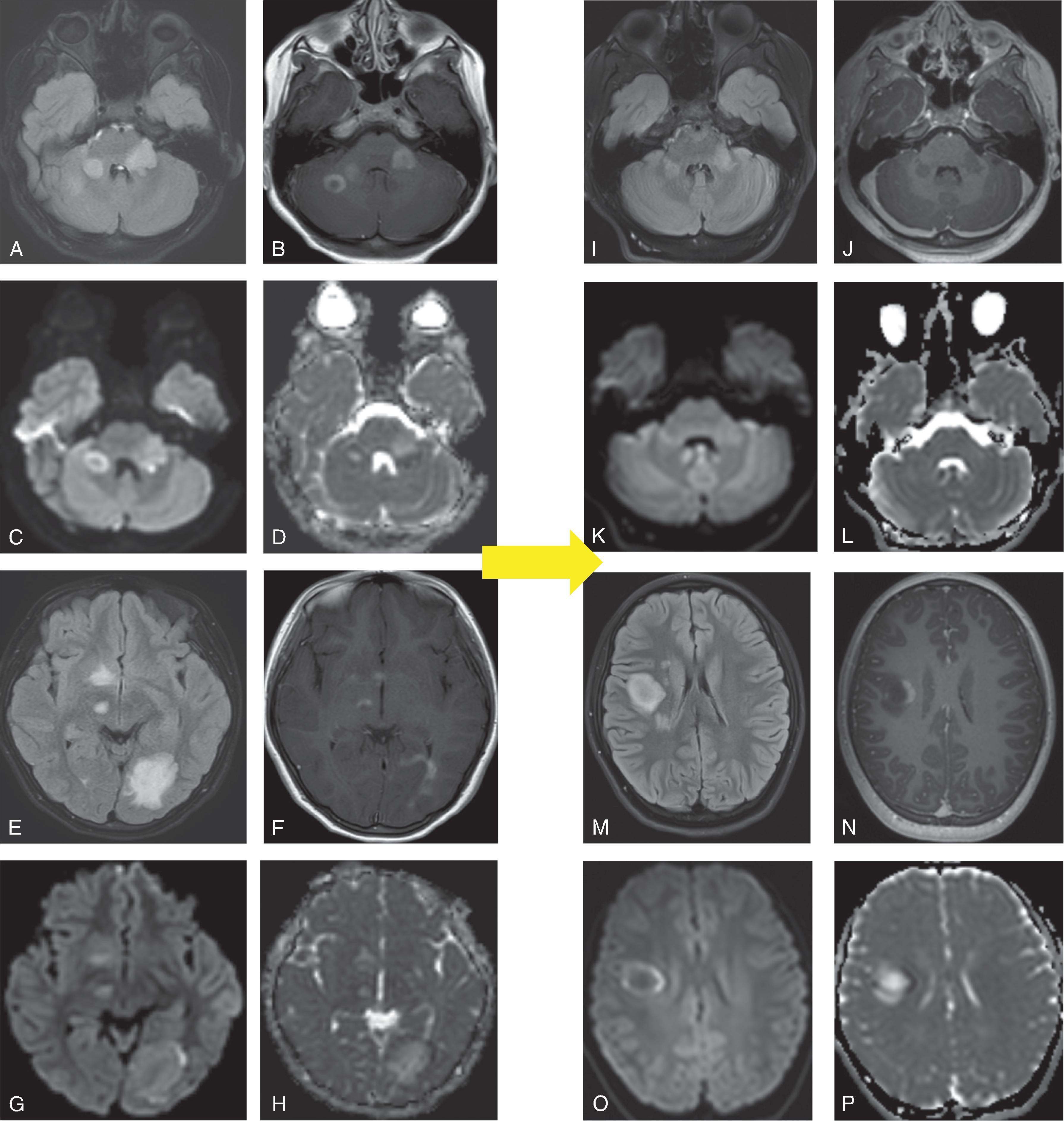
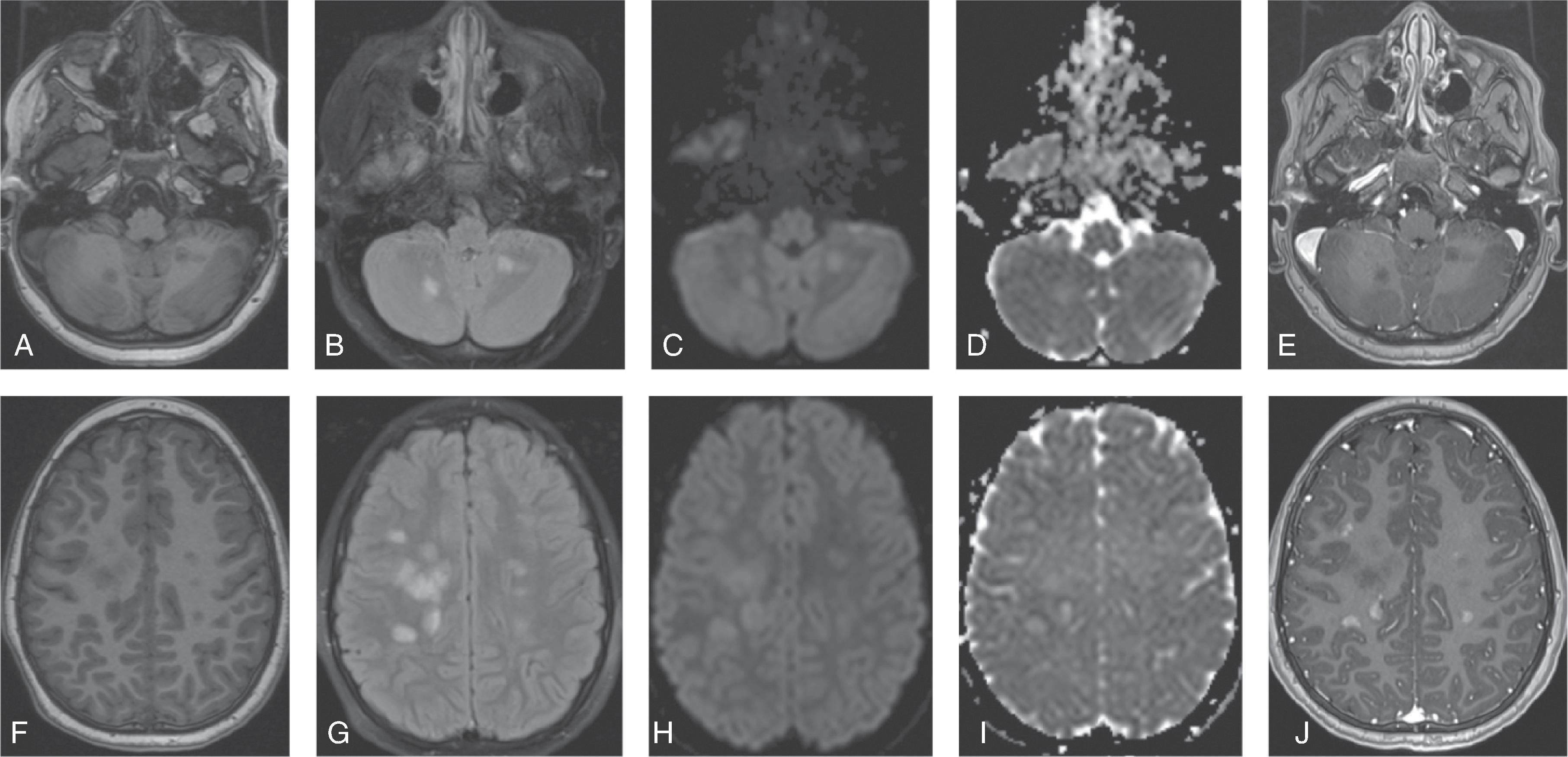
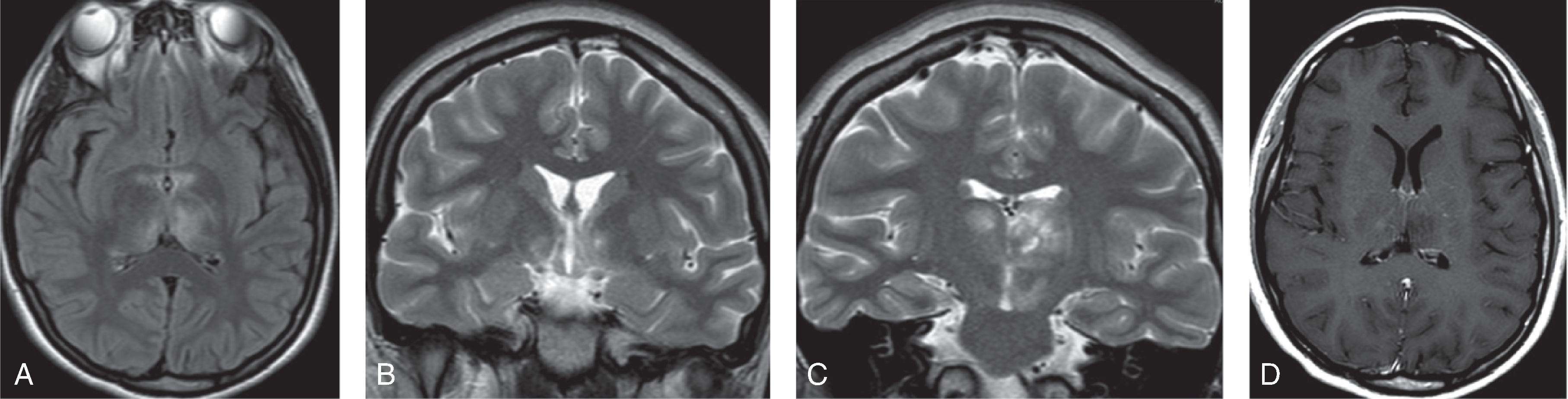
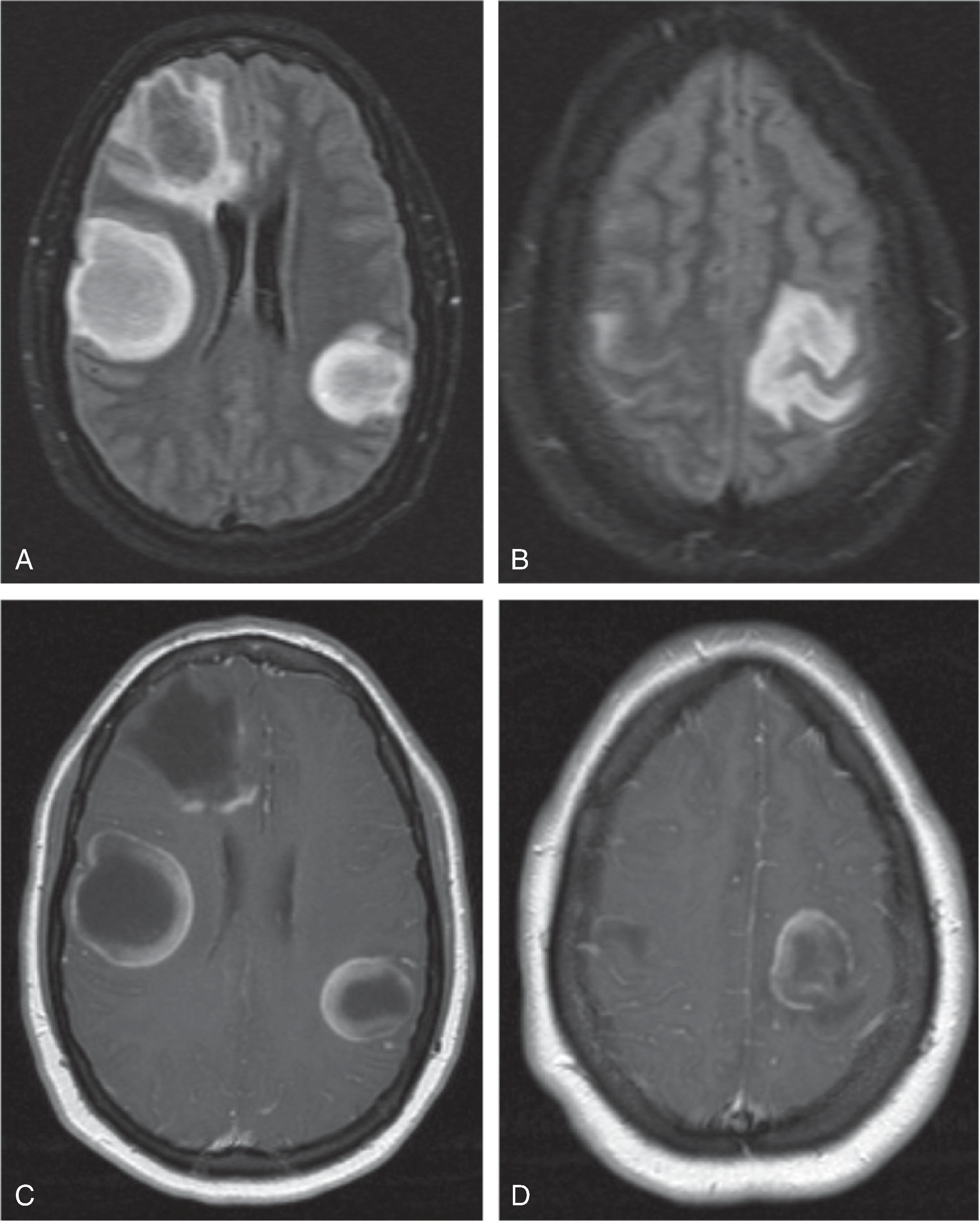
T2W hyperintense ill-defined to well-defined lesions of variable size (often 1–2 cm) involving white matter > gray matter, preferentially juxtacortical white matter; occasionally lesions may show restricted diffusion; variable contrast enhancement
Rarely symmetric central gray matter involvement may occur
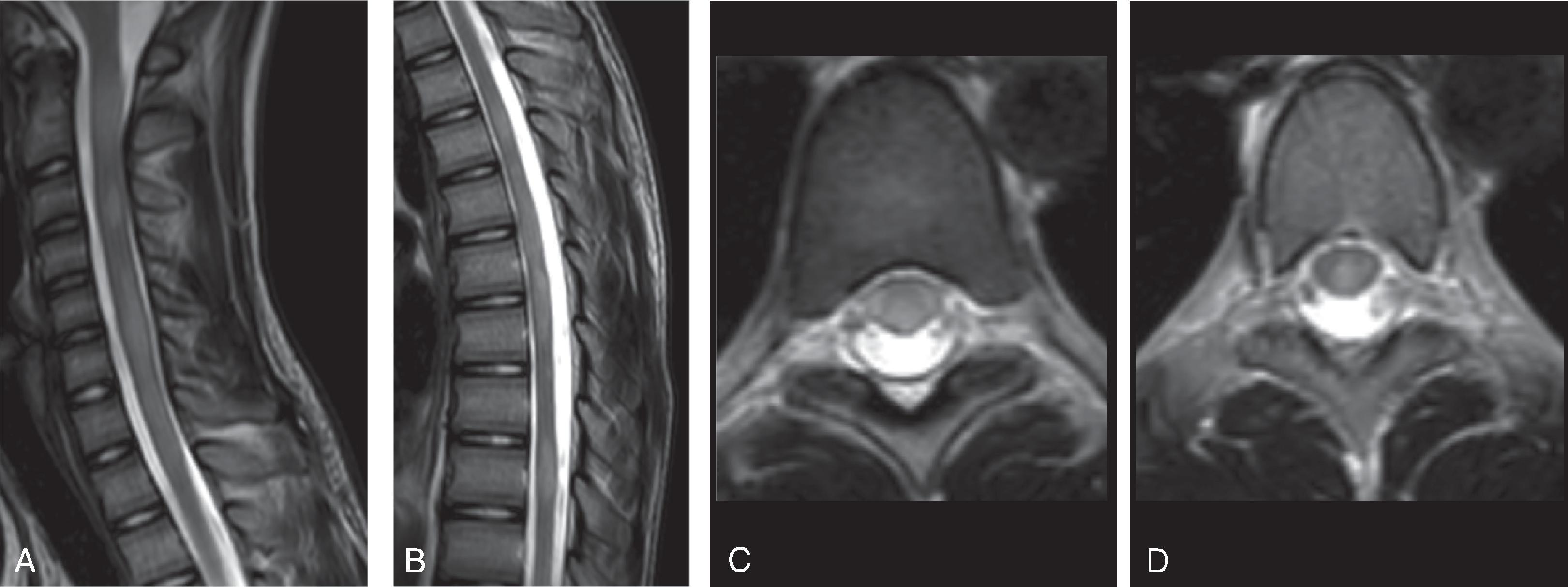
Spinal cord involvement is often longitudinally extensive, involving gray and white matter; may have dominant central gray matter involvement
Differential Diagnosis: Encephalitis, vasculitis, posterior reversible encephalopathy syndrome (PRES), other demyelinating disorders (MS, NMO)
Figures 6.4 A-P
Chronic autoimmune condition with genetic predisposition triggered by unknown factors affecting patients typically between the ages of 20 and 40 years
Highest prevalence in North America and Europe
15% primary progressive (PPMS) course, 85% relapsing-remitting (RRMS) course
CIS (clinically isolated syndrome): First presentation isolated in time and not preceded by prior neurologic event, often presenting with optic neuritis, brainstem syndrome, or transverse myelitis
Lesions per the McDonald criteria are >3 mm
Dissemination in space
can be demonstrated by one or more T2W-hyperintense lesions that are characteristic of multiple sclerosis in two or more of four areas of the CNS: (1) periventricular, (2) cortical or juxtacortical, and (3) infratentorial brain regions, and (4) the spinal cord
Dissemination in time
can be demonstrated by the simultaneous presence of gadolinium-enhancing and nonenhancing lesions at any time or by a new T2W-hyperintense or gadolinium-enhancing lesion on follow-up MRI, with reference to a baseline scan, irrespective of the timing of the baseline MRI
Clinical diagnostic criteria for RRMS and PPMS are per the 2017 revisions of the McDonald criteria
Cognitive dysfunction, including problems with attention, language, memory, and executive functions, occurs in 30% to 50% of pediatric MS and is associated with lesion load
Pediatric MS versus adult MS: •Male:female ratio is closer to 1 in children <10 to 12 years of age•Greater ADEM-like onset, more brainstem and cerebellar involvement, and less destructive lesions (less T1 hypointense supratentorial lesions) with pediatric MS •Children <12 years have greater numbers of relapses, more severe clinical involvement, worse prognosis, and polysymptomatic onset•Oligoclonal bands are detected in 40% to 70% of pediatric MS compared to 90% of adult patients with MS
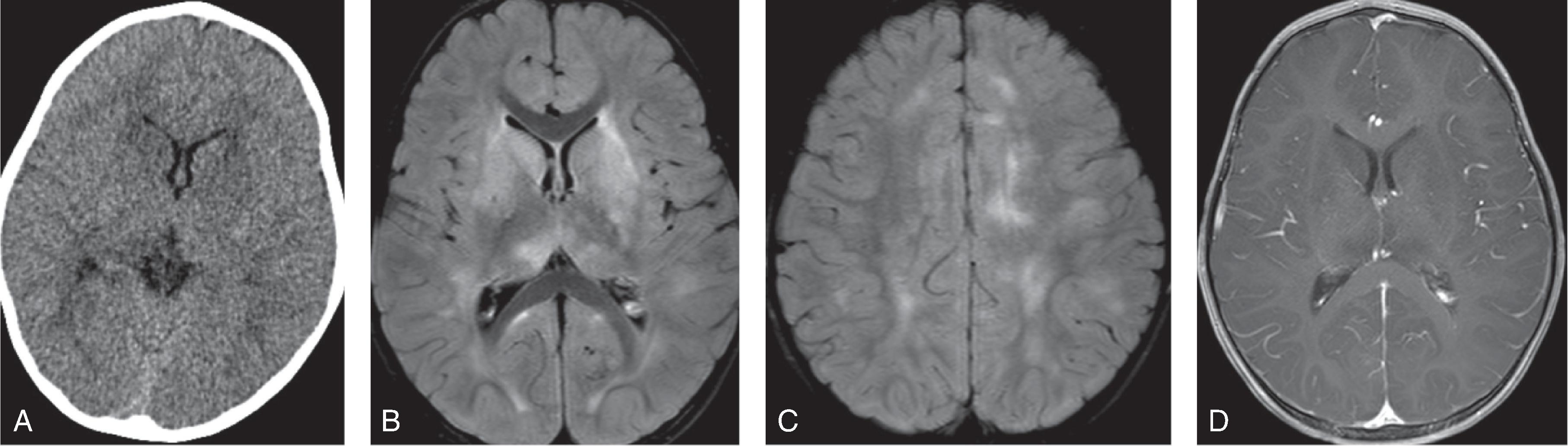
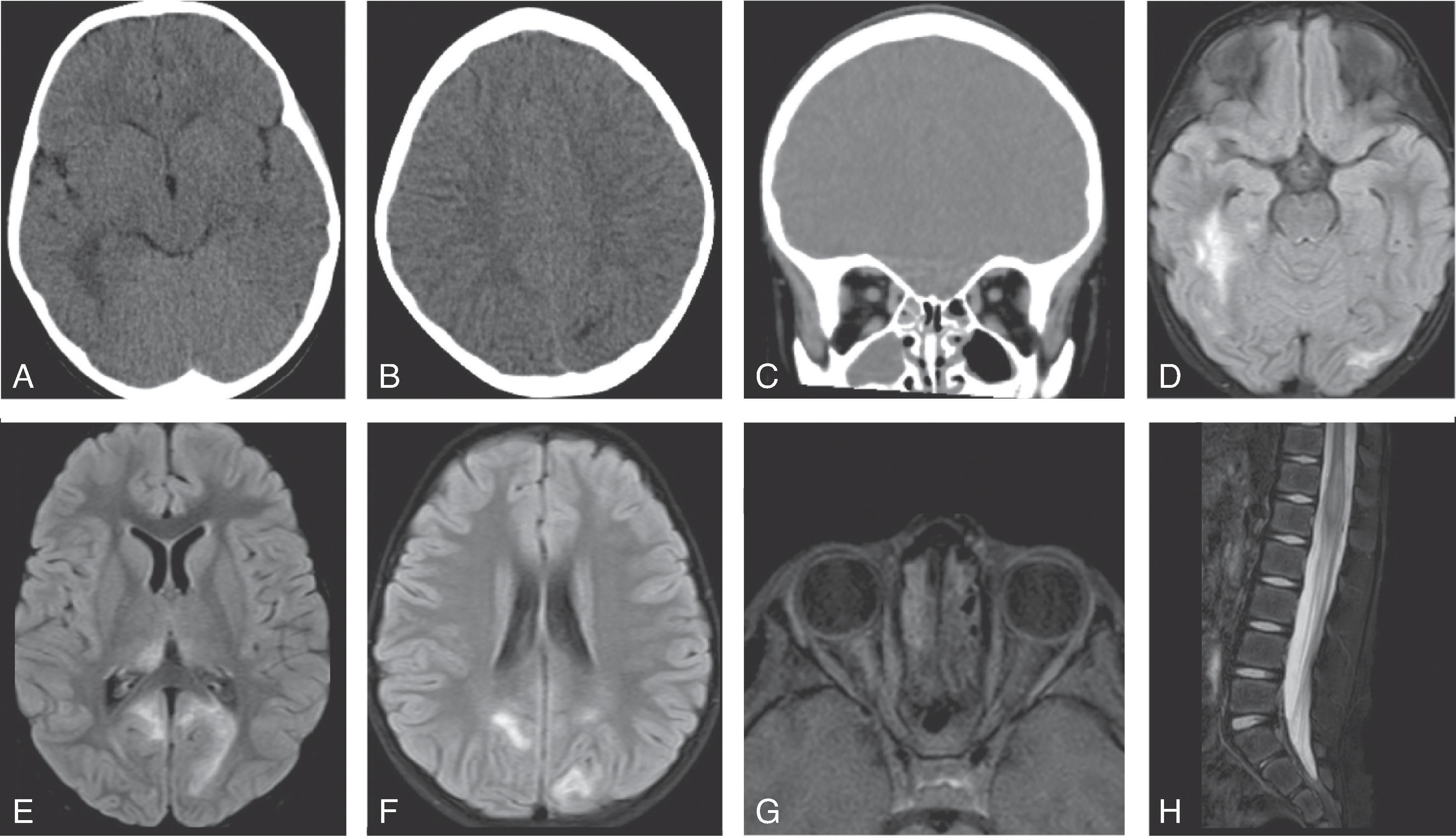
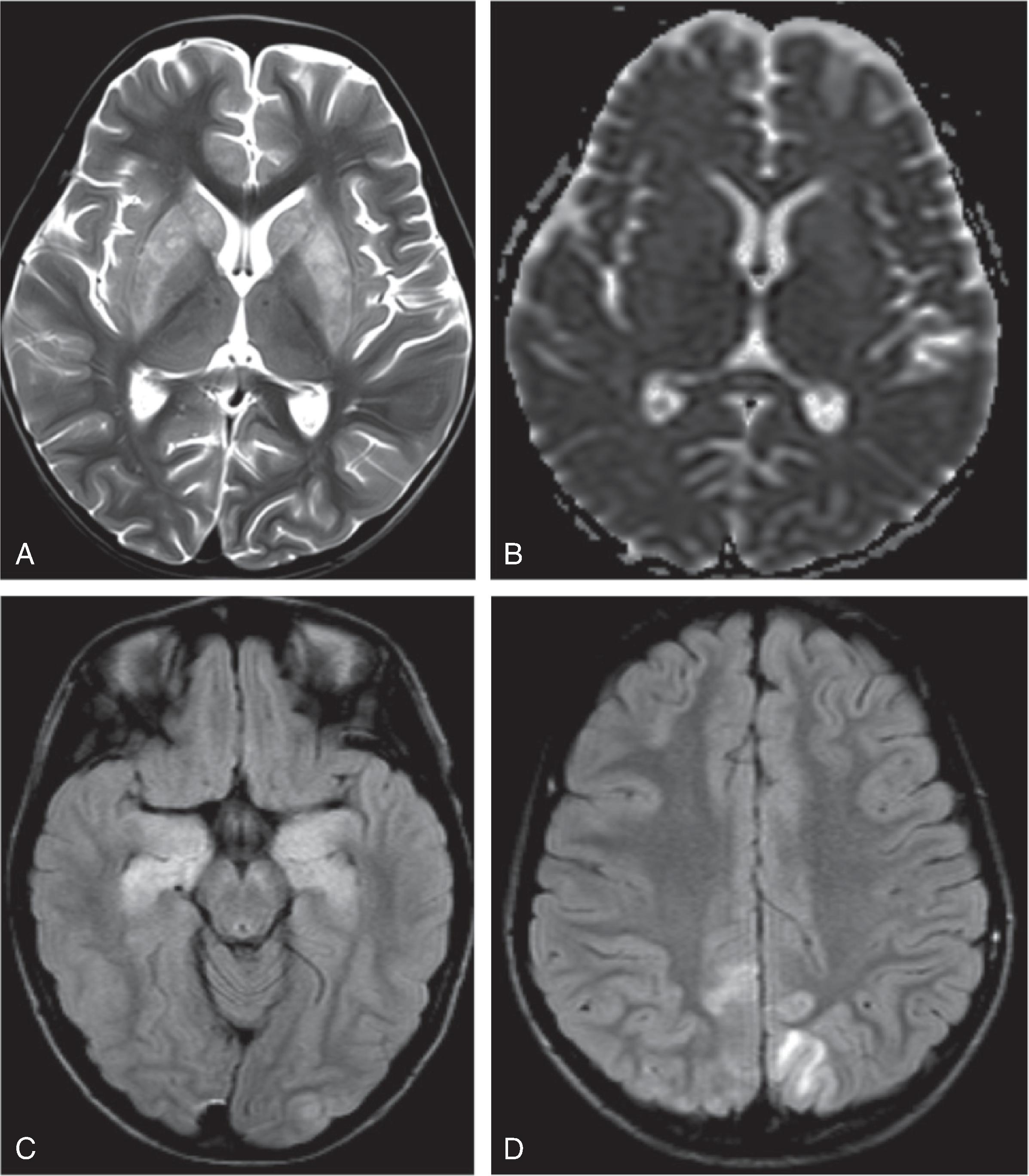
T2/FLAIR hyperintense ovoid lesions most commonly involving the juxtacortical, subcortical, and periventricular white matter and corpus callosum. Dawson’s fingers refers to white matter lesions perpendicular to the ventricles.
Posterior fossa lesions often in the cerebellar white matter and middle cerebellar peduncles.
Enhancement of lesions is nodular, homogenous, or incomplete ring-like.
Tumefactive MS lesions are more common in children than adults.
Thalamic and basal ganglia lesions may occur with extensive disease.
Upper cervical cord and lower thoracic cord most commonly affected; often located in the lateral and posterior columns of the cord; gray matter may be involved; multifocal and short craniocaudal cord involvement
NMO, ADEM, anti-MOG, Susac, cerebral autosomal dominant arteriopathy with sub-cortical infarcts and leukoencephalopathy (CADASIL), cerebral amyloid angiopathy (CAA), Lyme disease, primary angiitis of the central nervous system (PACNS), chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS), PML, methotrexate leukoencephalopathy, neurosarcoidosis, and vasculitis
Figures 6.7 A-H
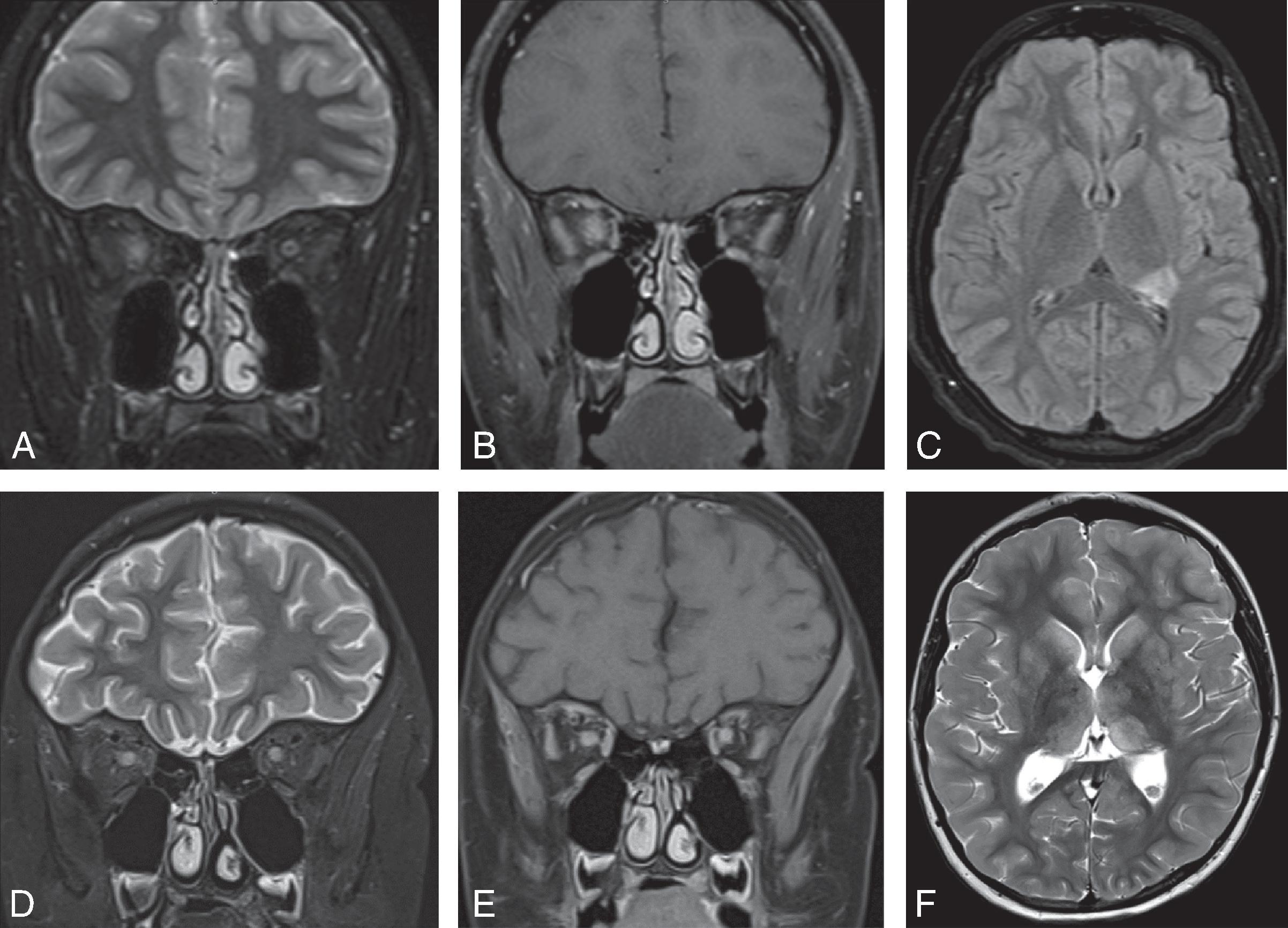
Figures 6.8 A-F
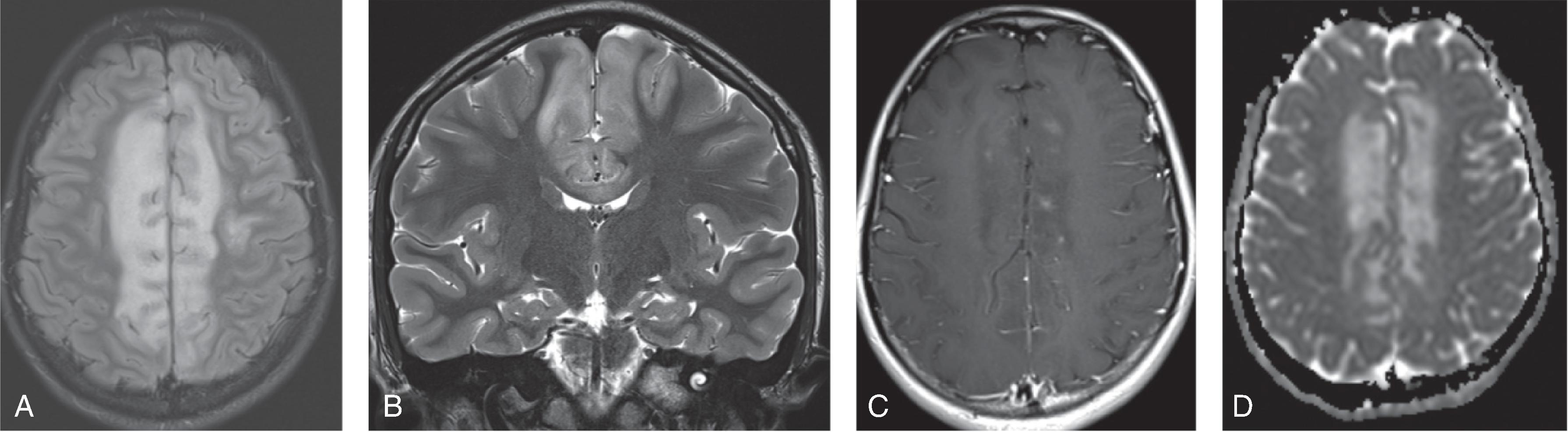
figure 6.9 A-D
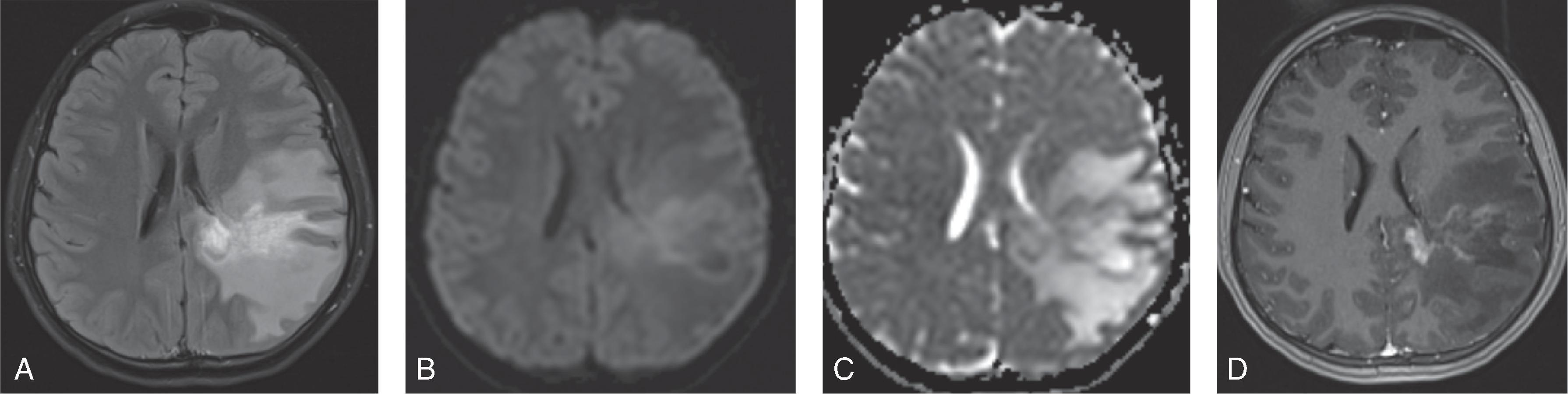
figure 6.10 A-D
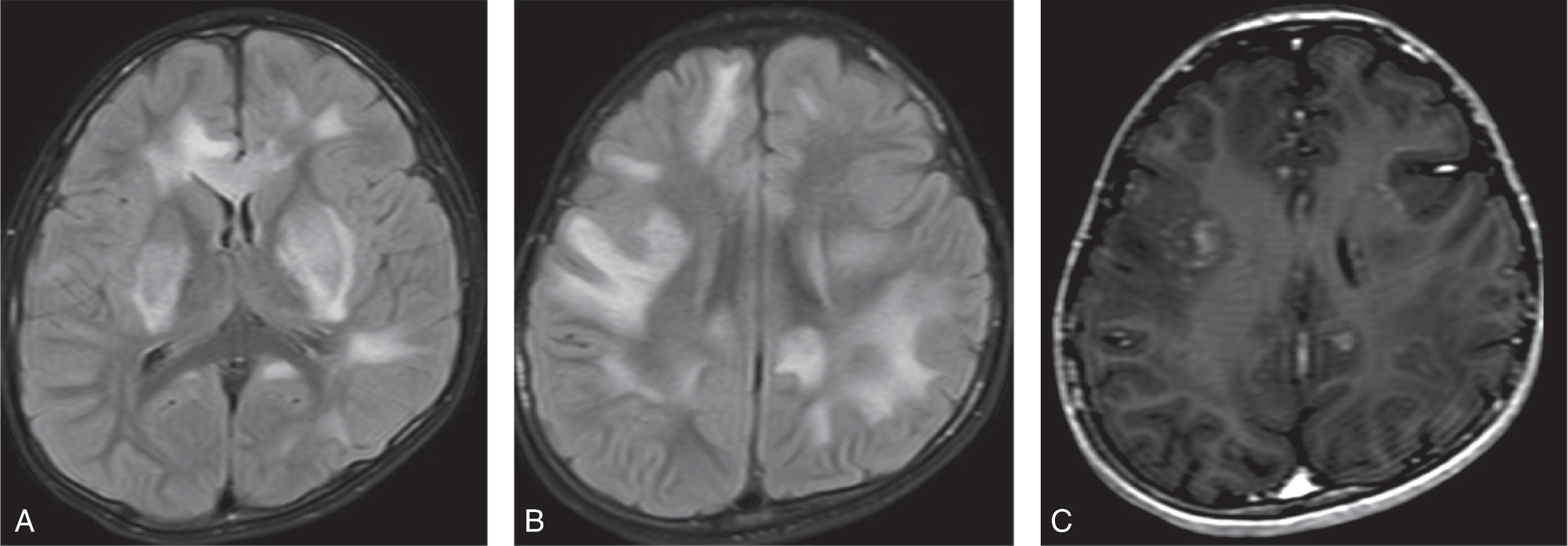
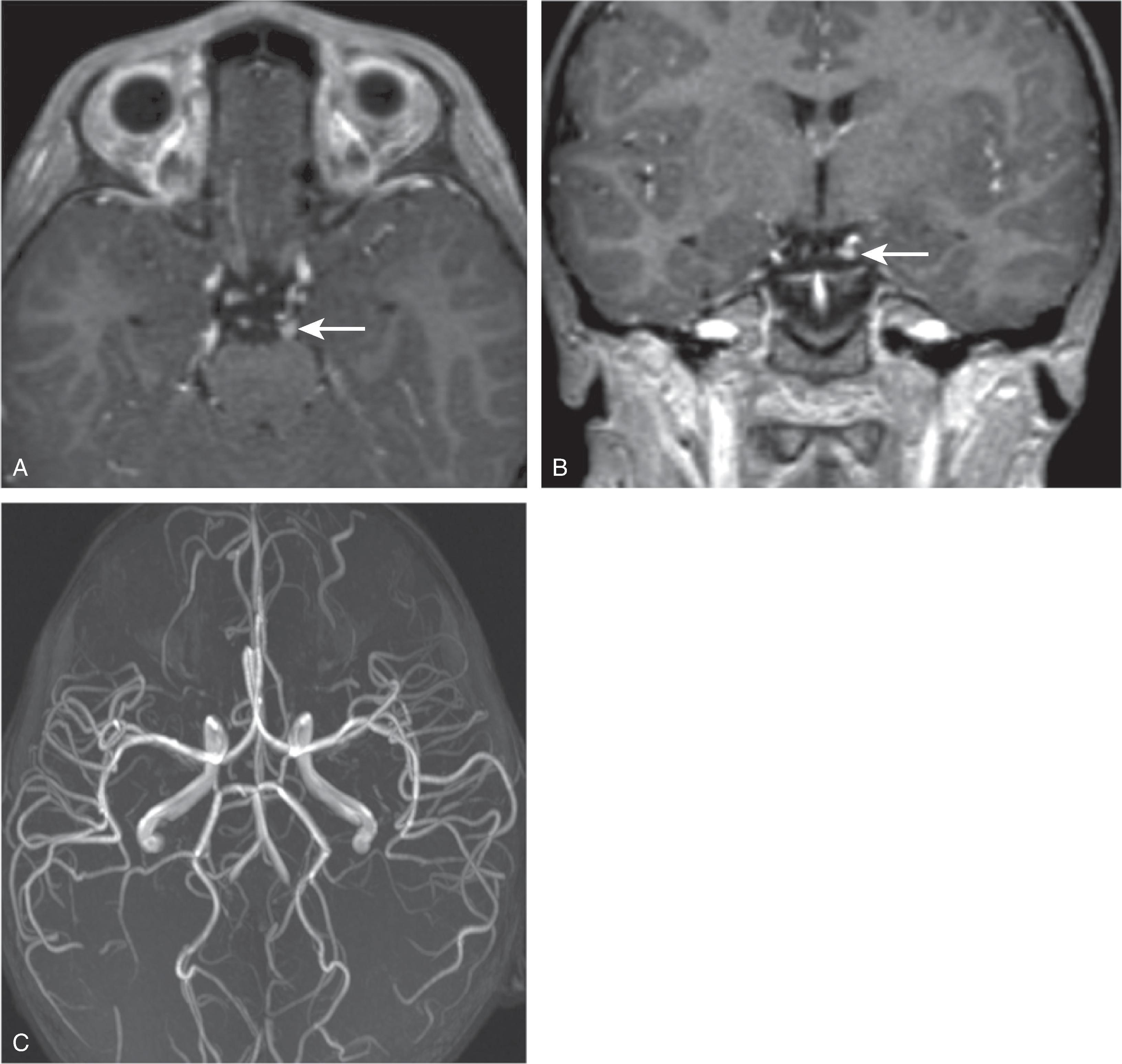
Figure 6.11 A-C
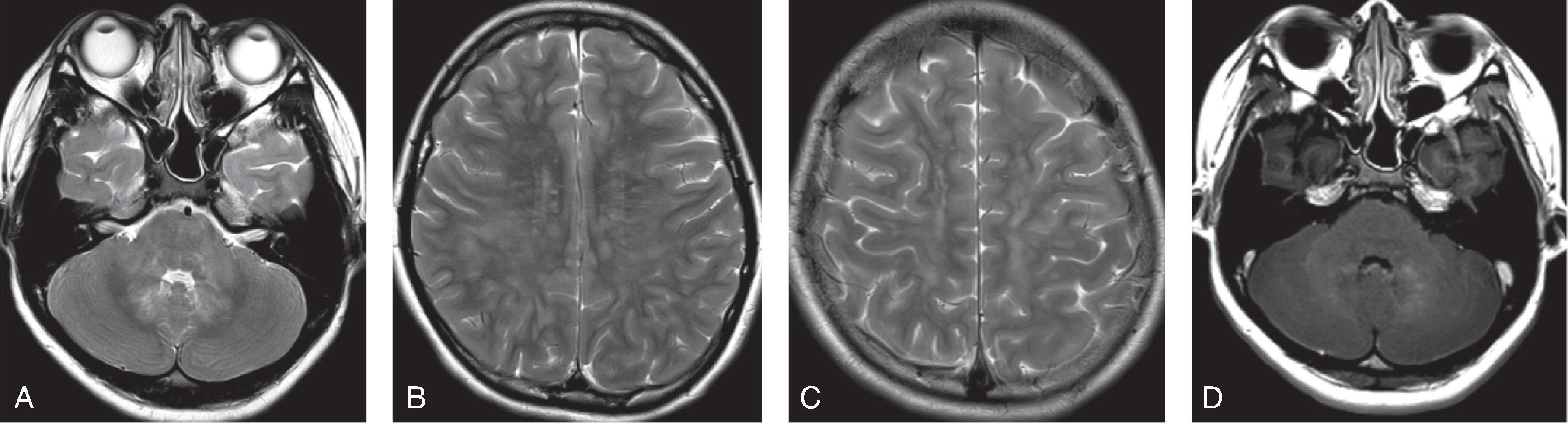
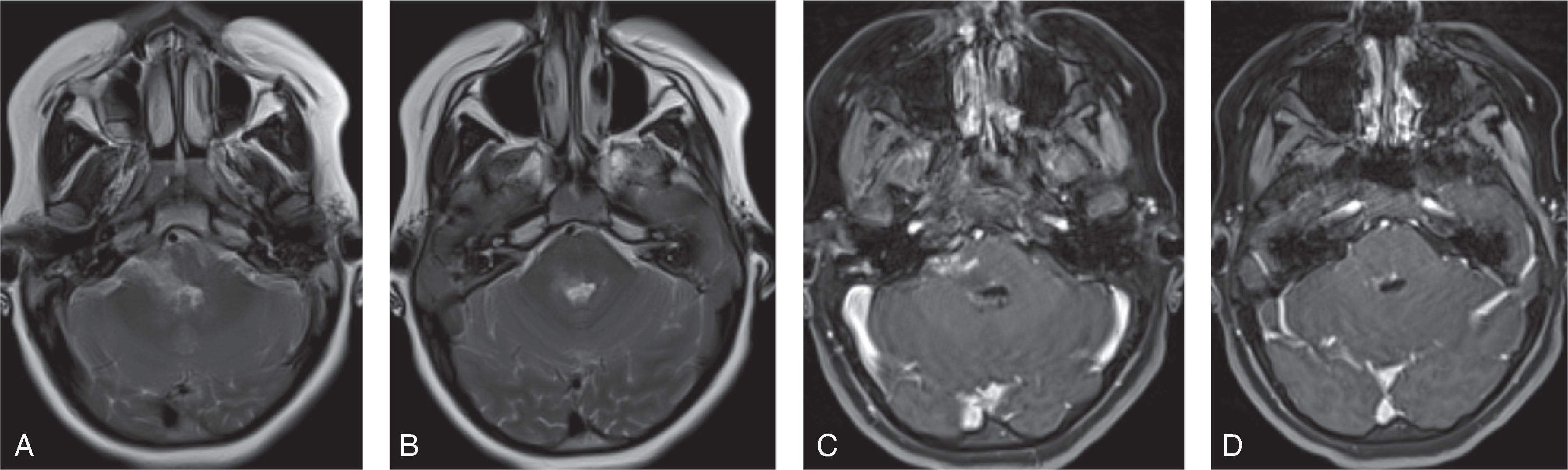
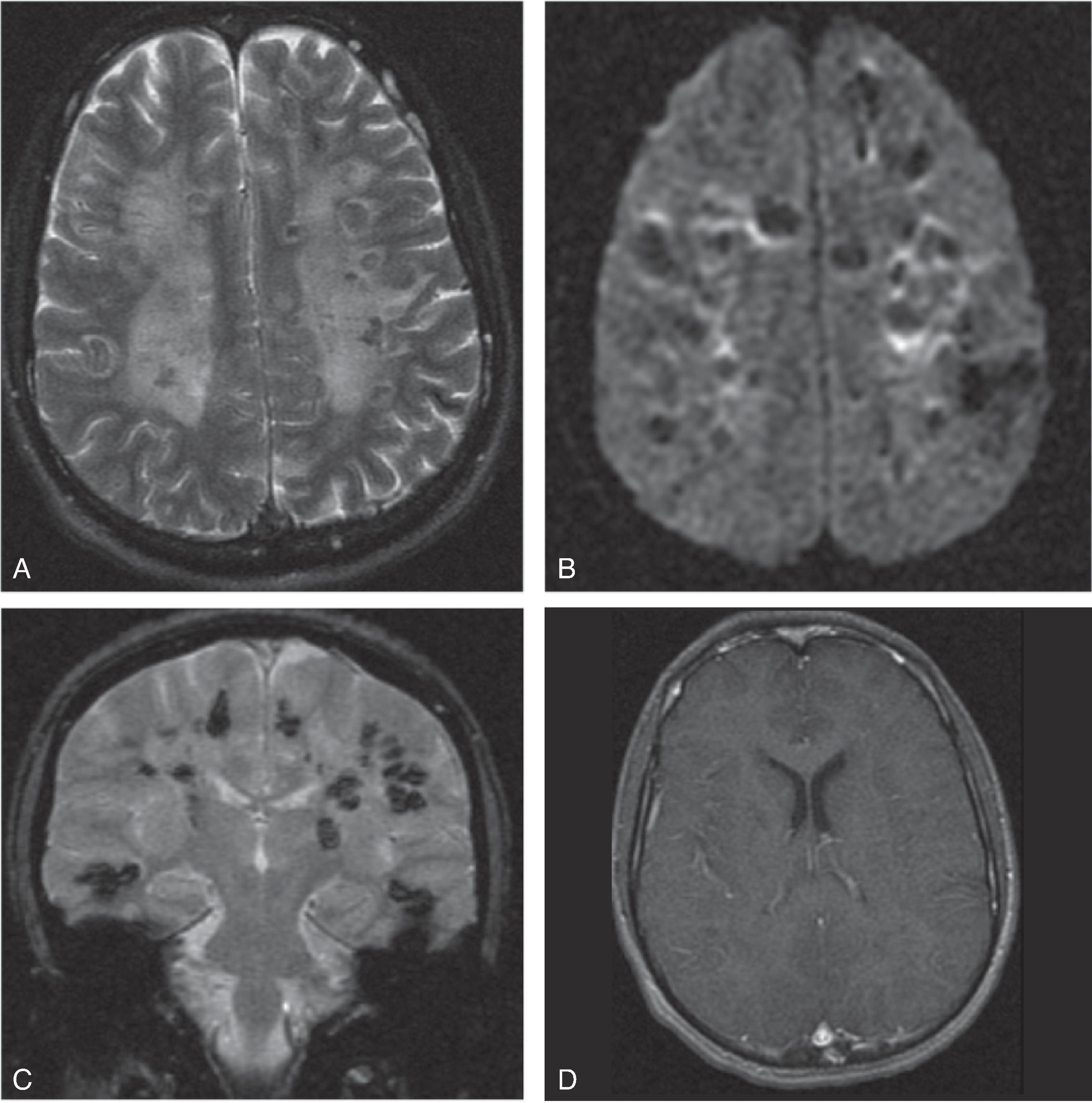
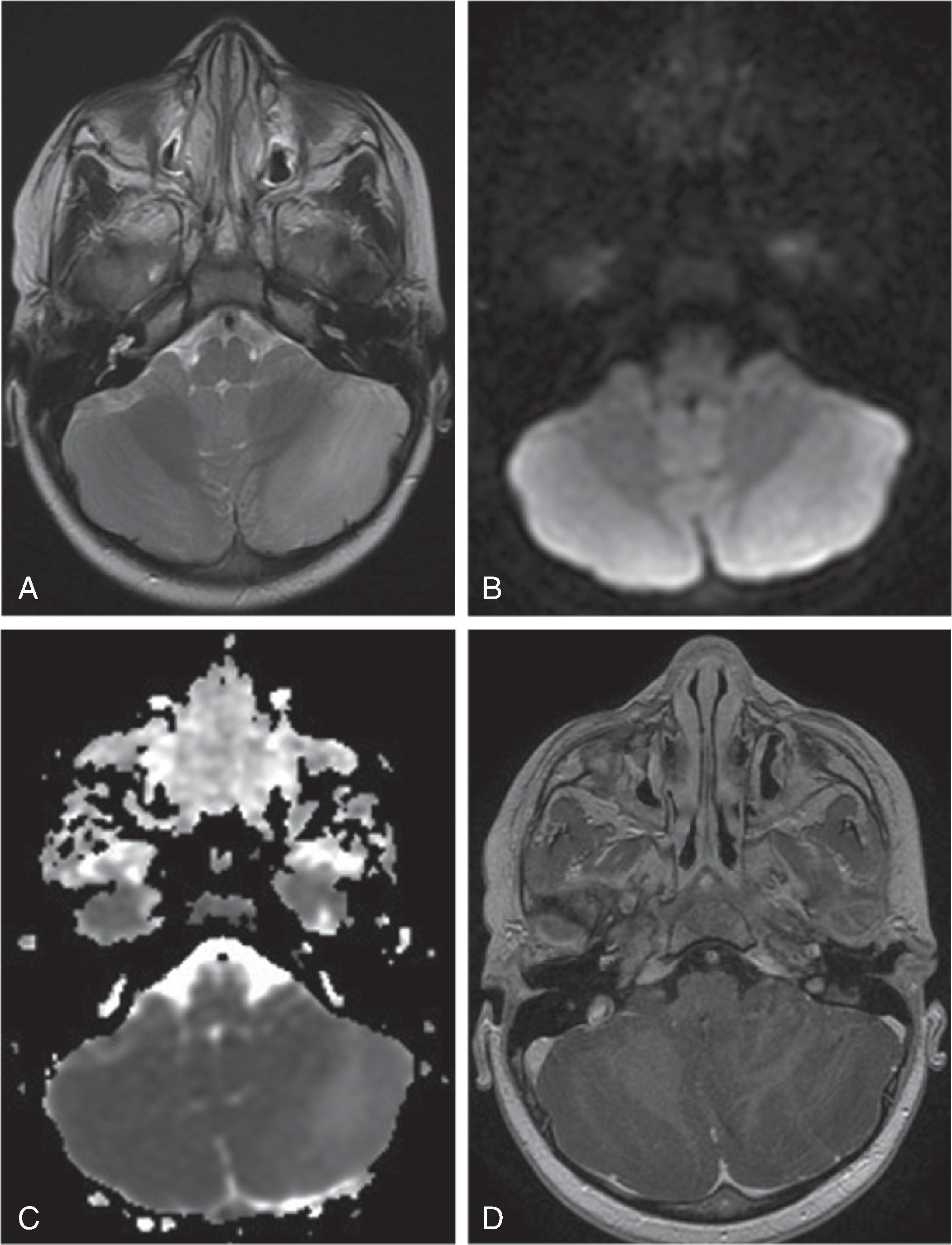

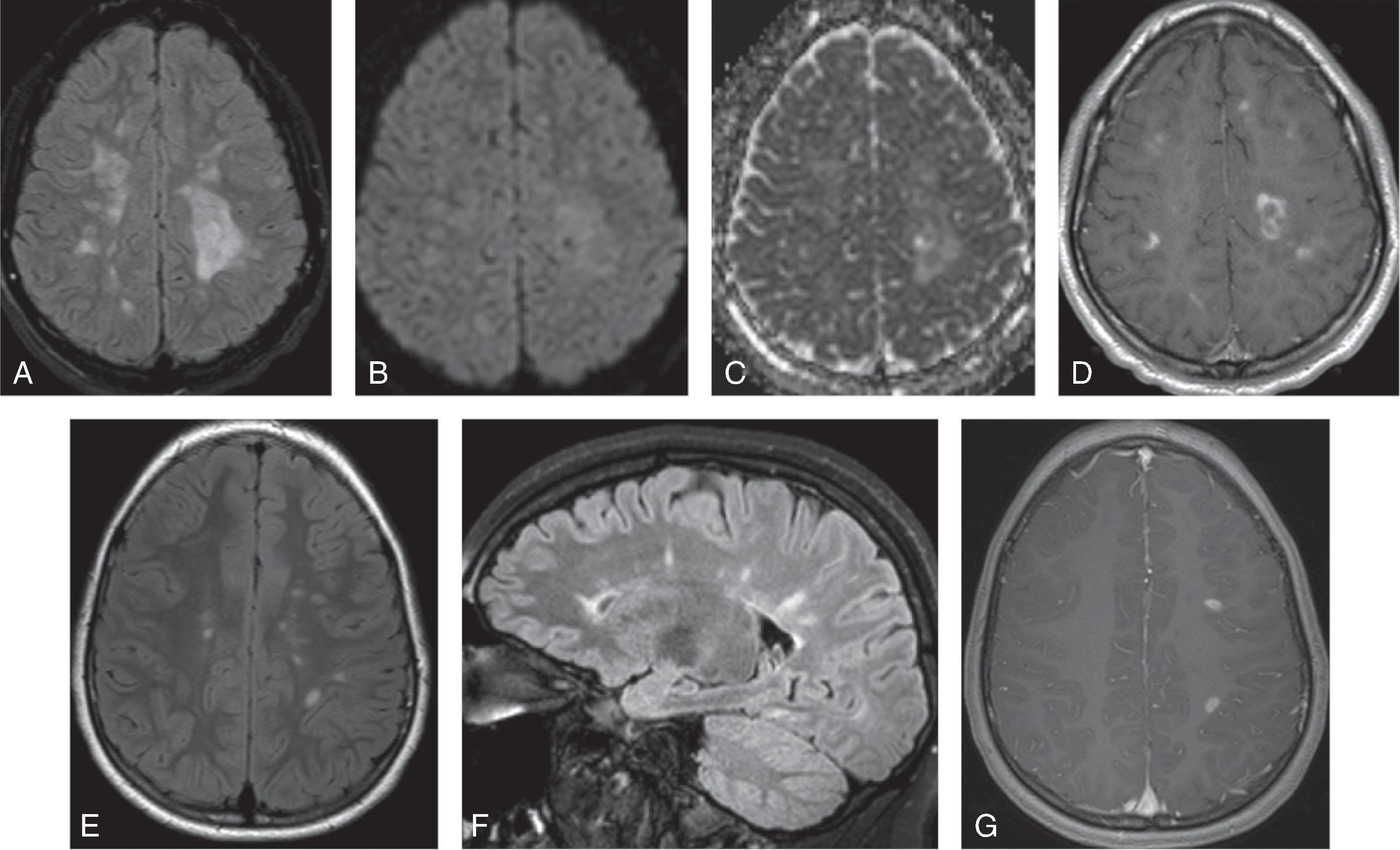
Inflammatory and demyelinating disorder associated with antibodies to myelin oligodendrocyte glycoprotein (MOG).
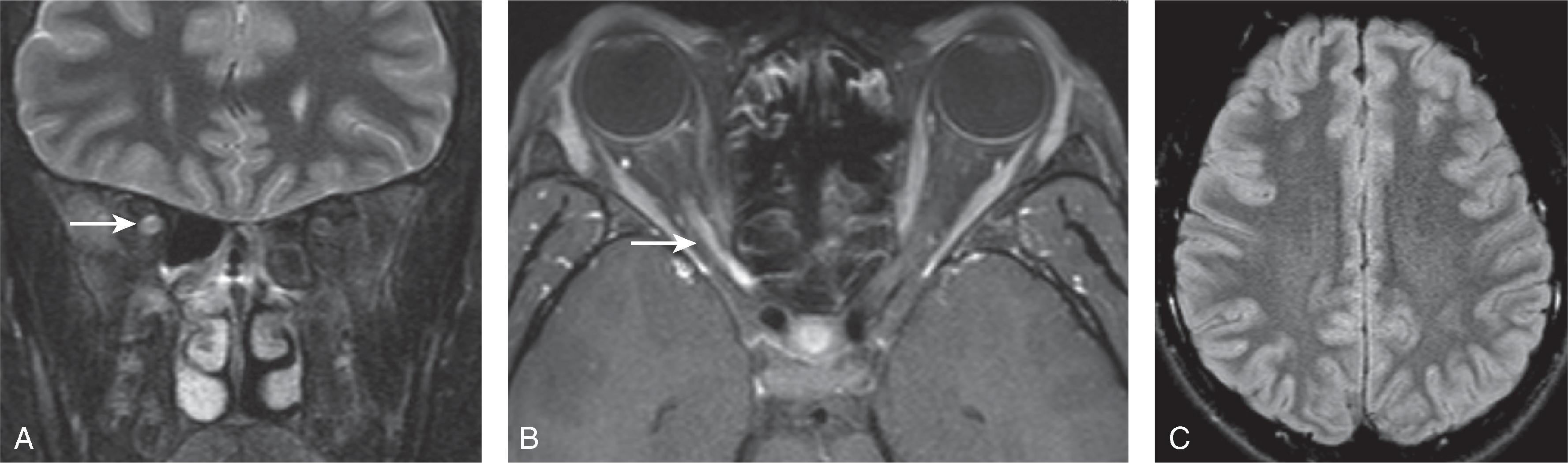
Clinicoradiologic patterns include ADEM, ADEM-like, optic neuritis, myelitis, neuromyelitis optica spectrum disorder (NMOSD), and encephalitis
Clinical presentation depends on CNS region effected and can include altered consciousness, headache, behavioral changes, seizures, neurologic deficits, vision loss, and lower extremity weakness
Disease course can be monophasic or relapsing remitting
Young children most often present with ADEM pattern, while children >10 years more frequently present with optic nerve and spinal involvement
Anti-MOG optic neuritis has good prognosis in >90% of children
Anti-MOG antibodies are detected in ∼20% of aquaporin-4–negative NMOSD. Compared to aquaporin-4–positive NMO, the aquaporin-4–negative anti-MOG–positive NMOSD has more equal male:female ratio, more isolated optic neuritis or myelitis, less severe clinical course, better steroid response, and monophasic disease
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here