Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The deltopectoral (DP) fasciocutaneous flap, also known as the Bakamjian flap, is an important reconstructive tool that has been used for a wide variety of reconstructive problems in head and neck surgery. A variation of this flap that is based on a single perforator of the internal mammary artery is called the “internal mammary artery perforator (IMAP) flap.” The DP flap was initially described for facial reconstruction and resurfacing, as it was found to have an excellent color and thickness match to the native facial skin. In addition, the tissue from this region is thin and pliable, with the potential to provide a large area of well-vascularized tissue that is easily contoured.
This flap was first described in 1917 by Aymard for nasal reconstruction. In the 1930s, Joseph described this flap for head and neck reconstruction. However, it was not until the 1960s that this flap came to be used on a routine basis in head and neck reconstruction. In 1965, Bakamjian described the use of the medially based DP flap in the reconstruction of the laryngopharyngectomy defect, and the DP flap became the “workhorse” flap for resurfacing mucocutaneous defects of the head and neck.
With proper planning, as well as delay techniques in select circumstances, the DP flap can be used for reconstruction of any part of the anterior head and neck below the zygoma. The DP flap has been used in a variety of settings, including, but not limited to, closure of dehiscent wounds and fistulas, restoration of compromised regions including irradiated head and neck defects, and reconstruction of pharyngeal defects. Furthermore, reconstruction of complex head and neck surgical defects may require multiple flaps, and the DP flap may obviate the need for multiple microvascular free flaps. For some time now, the pedicled form of the DP flap has been largely overshadowed by the development of highly reliable regional flaps and the expanded use of free tissue transfer for head and neck reconstruction. Despite these trends, the DP flap remains a reliable option for the head and neck surgeon.
This flap is based on the parasternal fasciocutaneous perforating branches of the internal mammary artery, which perforate the intercostal muscles and the pectoralis muscle to reach the skin. The blood supply to the anterior chest wall comes from perforators from the internal mammary artery that traverse each intercostal space; branches of the thoraco-acromial artery; musculocutaneous branches that traverse the deltoid muscle; the posterior intercostal vessels that give off perforators to the posterior, lateral, and anterior thoracic skin; and minor contributions from the lateral thoracic artery.
second or third perforating branches of the internal mammary artery
Length: 1.5 cm (range 1–2 cm)
Diameter: 1 mm (range 0.8–1.2 mm)
The internal mammary artery (IMA) branches off the subclavian artery.
The IMA diameter of 1–2 mm; accompanying vein diameter of 2–3 mm
Terminates into the musculophrenic and the deep superior epigastric arteries at the sixth intercostal space
At each intercostal space, the IMA has three branches:
Medial branch, which supplies the sternum
Lateral branch, which communicates with the anterior intercostal artery
Anterior branch, which supplies this flap.
The anterior branch pierces the intercostal muscles and the pectoralis fascia running toward the skin. This vessel travels superficial to the fascial covering of the pectoralis major and deltoid muscles and terminates approximately 12 cm from the midline at the anterior axillary line.
The caliber of this perforator ranges 0.5–1.2 mm.
The second and third perforators are usually the largest caliber and run with their associated veins in the intercostal interspaces approximately 1–1.5 cm lateral to the border of the sternum.
The flap is usually based on these large second and third perforators, but can be based on a single vascular pedicle in situations where a clearly dominant perforator is present.
first and fourth perforating branches of the internal mammary artery (see Figs 11.2 and 11.3 )
Length: 1.5 cm (range 1–2 cm)
Diameter: 0.7 mm (range 0.5–1.2 mm)
direct cutaneous artery that arises from the thoracoacromial system
This artery supplies a small area of skin below the lateral aspect of the clavicle overlying the deltopectoral groove.
intercostal perforators
Some of the intercostal vessels send perforators that supply the skin of the anterior chest.
venae comitantes of the perforators from the internal mammary artery
Length: 1.5 cm (range 1–2 cm)
Diameter: 2.5 mm (range 2–3 mm)
The venae comitantes drain into the internal mammary vein, which subsequently drain into the innominate vein.
branch of the thoracoacromial vein
This branch could be used potentially to augment the venous drainage of a free DP flap.
cephalic vein
The cephalic vein runs in the deltopectoral groove between the axial pattern and the random pattern of the DP flap. Drainage through this vessel is presumed to improve blood flow of the distal DP flap.
the supraclavicular nerves of C3 and C4, and the anterolateral intercostal nerves of T2, T3, and T4 (see Figs 11.2 and 11.9 )
this flap does not have a muscle component.
This flap is harvested as a cutaneous or a fasciocutaneous flap. Although not necessary for flap survival, the fascia overlying the pectoralis major muscle is often included with the flap harvest, for the purpose of protecting the nutrient blood supply. There is not a reliable source of bone that can be harvested with this flap.
The anatomy is reliable, and flap harvest is relatively easy.
There is no need for additional patient positioning or preparation when dealing with defects in the head and neck or anterior part of the body.
There is very little donor site morbidity and no significant functional deficits. The donor defect is easily covered by clothes.
The fasciocutaneous flap is thin and pliable.
The lack of a bulky muscular component makes it an excellent choice for replacing cutaneous defects.
The skin of the flap matches the color and texture of the face.
The flap size can be increased if a “delay” procedure or tissue expansion is performed.
Two symmetrical DP flaps can be simultaneously harvested, effectively enlarging the available skin.
The arc of rotation can be extended by removing a portion of rib and dissecting out the internal mammary artery.
The effective pedicle length can be increased through modification referred to as the deltopectoral island flap (see below).
This flap can be used even if a patient has had a pectoralis major flap if care was taken not to cut into the deltopectoral skin, and the internal mammary perforators were protected during harvest of the pectoralis flap (see Fig. 34.5 ).
The DP flap can be used as a large migrating tube flap (“waltzing”).
Skin grafting of the donor site may be necessary if the harvest includes more than four interspaces or about 8 cm of skin. However, skin laxity in certain individuals may allow for more extensive donor defects to be closed primarily.
Distal flap necrosis can occur when the skin paddle is extended over the deltoid region without a delay procedure.
For some patients, hirsute skin can be an issue.
In female patients there is the morbidity of chest skin scarring as well as the potential for alteration in breast symmetry and positioning or nipple distortion.
In general, the DP flap can be used for most head and neck applications without the need for additional studies.
The lateral edge of the sternum ( Fig. 35.1 ) marks the medial aspect of the flap, the clavicle marks the superior aspect of the flap, the lower aspect of the 4th rib denotes the inferior aspect of the flap, and the lateral aspect of the flap, without a delay procedure, is 3–4 cm lateral and parallel to the deltopectoral groove.
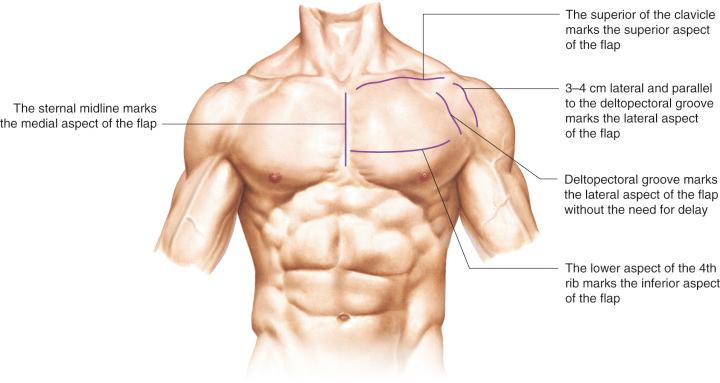
The superior and inferior limits of the flap may be adjusted based on the perforator chosen.
The flap can be centered over one perforator, preferably the largest (the second or third perforator).
A handheld Doppler probe can be used preoperatively to detect the exact location of the perforators and the relative size of each perforator.
The zone located 2 cm lateral to the border of the sternum should not be violated during harvest of this flap in order to avoid injury to these nutrient vessels.
The flap can be designed based on any of the internal mammary perforators and oriented in a lateral, oblique, or inferior direction. The lateral direction toward the acromial process allows for the furthest extension of the flap, whereas the other two designs are limited in length unless a delay is performed.
The DP flap can be raised and transferred in the primary setting with a high degree of reliability, provided that it does not include an extended territory overlying the deltoid muscle.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here