Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A detailed history and neurologic exam can be used to isolate the level at which the underlying pathology originated. Understanding the presenting symptoms can help one to appreciate the significance of the extent of degeneration present and therefore start to formulate the most efficient treatment plan.
Nonoperative treatment is a feasible first course of action to address the clinical manifestations of new-onset degenerative spinal disease symptoms. Typically this involves medical management (antiinflammatory and pain medications) and physical therapy.
Surgical intervention to treat symptoms that result from degenerative spine disease includes diskectomy, laminectomy, and fusion procedures. Despite continuing controversy surrounding which procedure is most effective in providing long-term relief, the authors believe that the best course is to understand the underlying pathology and select the least invasive procedure to target the area of pathology.
Although the causes and manifestations of lumbar spine disease are numerous, this chapter focuses on degenerative spinal stenosis, disk herniation, and acquired spondylolisthesis, as these are three of the most common indications for lumbar spine surgery in the United States. Spinal stenosis is defined as a narrowing of the vertebral canal and can be the result of several etiologies, frequently degenerative disk disease. Spondylolisthesis, although it often presents as spinal stenosis, specifically refers to forward displacement of one vertebra relative to its neighbor. Between 2004 and 2009 the number of inpatients discharged with a primary diagnosis of lumbar spinal stenosis increased from 94,011 to 102,107. The same study also found an increase in the prevalence of patients with concomitant spondylolisthesis. Lumbar disk herniation, although a less frequent cause of spinal stenosis, is the root cause of a vast number of complaints of low back pain. According to data from the 2010 National Hospital Discharge Survey, more than 342,000 procedures for the excision or destruction of intervertebral disks were performed in the United States. Given the ubiquitous nature of these conditions, expertise in the identification and management of lumbar spine disease is essential to any neurosurgical practice.
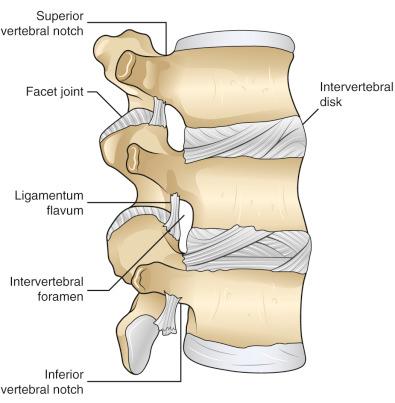
The lumbar spine consists of five vertebrae and intervening intervertebral disks. The vertebral bodies are large, with a transverse diameter greater than the anteroposterior diameter. The neural arch is composed of the two pedicles, laminae, and the spinous process. The laminae are connected via the ligamentum flavum ( Fig. 36.1 ). The inferior articular processes of the lumbar vertebrae are positioned posterior and medial to the superior articular processes. The facet joints in the upper and middle lumbar spine are oriented in the sagittal plane, which allows flexion and extension while resisting rotation and lateral bending. The facet joints at L5 to S1, however, are oriented in the coronal plane, which facilitates rotation while resisting anterior-posterior translation.
The intervertebral disk is composed of the nucleus pulposus, annulus fibrosus, and the cartilaginous end plates. The annulus consists of 10 to 12 concentric layers of fibrous tissue and fibrocartilage and is reinforced ventrally by the anterior longitudinal ligament and dorsally by the posterior longitudinal ligament. The nucleus pulposus is contained within the annulus and is located slightly posterior to the midpoint of the intervertebral disk. A remnant of the notochord, the nucleus pulposus is semiliquid in childhood but becomes more solid and fibrous with age. The intervertebral disk attaches to the vertebral bodies above and below via a thin layer of hyaline cartilage. In the lumbar spine the intervertebral disk height is approximately 11 mm with an end plate area of approximately 15 cm 2 , although the size of the vertebral body increases from L1 to L5.
The caudal end of the spinal cord extends to the level of L1. Below L1, the spinal canal contains the descending lumbar and sacral rootlets collectively known as the cauda equina. Each lumbar and sacral root exits the dural sac laterally, approximately one vertebral level above where it will exit the spinal canal (eg, the L4 root exits at the level of the L3–L4 intervertebral disk). The nerve root then travels farther laterally to exit caudal to its respective pedicle (eg, the L5 root exits in the L5–S1 intervertebral foramen).
One of the common mechanisms of symptomatic lumbar spine disease is compression of neural elements, including the spinal cord, cauda equina, or individual nerve roots leading to pain, weakness, and numbness. The mechanisms by which compression induces neural dysfunction are not clearly elucidated, although mechanical damage, vascular insufficiency, and inflammation are likely contributors.
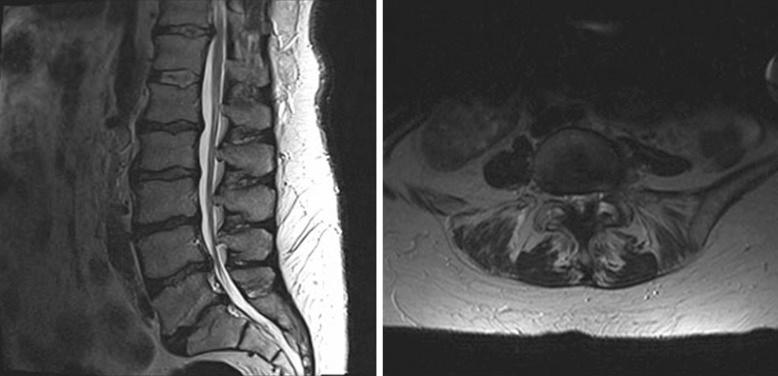
Intervertebral disk herniation begins initially with tearing of the annulus. As small tears in the inner rings of the annulus expand, the nucleus pulposus herniates into this space. Eventually, the outer rings of the annulus are weakened sufficiently that the nucleus pulposus causes focal bulging, known as disk protrusion. If the nucleus pulposus herniates further, it may escape from the confines of the annulus in a process known as disk extrusion. Most commonly, the disk herniates in a posterolateral direction ( Fig. 36.2 ). This is typically attributed to the slightly posterior location of the nucleus pulposus relative to the midpoint of the vertebral body and reinforcement provided by the posterior longitudinal ligament at the midline posteriorly. Posterolateral disk herniation typically results in compression of the ipsilateral nerve root as it exits the dural sac. Consequently, a posterolateral herniation of the L4 to L5 intervertebral disk typically results in compression of the L5 root. Far lateral herniations, however, typically cause compression of the ipsilateral nerve root exiting the neural foramen. Thus a far lateral herniation of the L4 to L5 intervertebral disk would result in compression of the L4 root. Unlike posterolateral and lateral herniations, large, centrally located herniations can result in compression of the entire contents of the vertebral canal at that level.

Degenerative spondylolisthesis occurs most commonly at L4 to L5, followed by L3 to L4, and then L5 to S1. Early hypotheses concerning the progression of the disease postulated that instability at the disk space caused initial slip. As a result of this instability, the facet joints and ligamentum flavum undergo secondary hypertrophy to prevent additional slip which exacerbates spinal stenosis ( Fig. 36.3 ). Further studies demonstrated no differences in disk dysfunction in patients with and without slippage. In addition, hypertrophy of the facets and ligamentum flavum requires hypermobility to develop. McGregor and colleagues, however, have shown that slip actually predisposes toward hypomobility.

Alternatively, spondylolisthesis may result from degenerative changes of the facet joint inclination and alignment. As the facets become more sagittally aligned (in excess of 45 degrees) the risk of developing degenerative spondylolisthesis increases 25-fold. More recent studies have shown that facet tropism, a difference in facet alignment of 7 degrees or more from one side to another, may predispose the affected level to increased disk or facet joint stress under external movements and anterior shear forces.
Degenerative disk disease is the most common cause of lumbar stenosis. As the intervertebral disk degenerates, it is less capable of withstanding axial and translational forces. This results in increased load bearing by the facet joints, which, in turn, causes arthritic changes. These initial arthritic changes are then followed by capsular laxity, subluxation of the facet joints, and enlargement of the articular surface area, thought to be a compensatory attempt to provide stabilization. Consequently, further stress is placed upon the intervertebral disk. The nucleus pulposus is broken down and resorbed and osteophytes develop from the end plates to stabilize the motion segment. Neural compression can thus result from osteophyte impingement, bulging of the intervertebral disk, or facet hypertrophy. Importantly, hypertrophy of the inferior articular process typically results in central canal stenosis due to encroachment upon the lateral recess and central canal, whereas hypertrophy of the superior articular process typically impinges upon the exiting nerve root within the neural foramen causing foraminal stenosis ( Fig. 36.4 ). Further exacerbating both foraminal and central stenosis, as the disk space narrows, the facet joints sublux partially, decreasing the area of the neural foramen, and the ligamentum flavum folds inward often becoming hypertrophied and less frequently, calcified potentially compressing the dural sac.
All the aforementioned pathologies result in some degree of neural compression and, consequently, overlap significantly in terms of clinical presentation. Common manifestations of these diseases are radiculopathy, neurogenic claudication, and cauda equina syndrome.
Radiculopathy results from the impingement of a single nerve root as it exits the dural sac or neural foramen. Radiculopathy presents clinically as pain, numbness, or weakness in the distribution of the affected root. The most common manifestation of radicular pain is “sciatica,” in which pain is generally localized to the posterior thigh and calf. Radicular pain is often exacerbated by standing and walking and partially alleviated by laying supine with the legs elevated and knees bent. It is important to distinguish radicular pain affecting the hip and buttocks from a primary hip joint pathology.
Neurogenic claudication, attributed to central canal compression, is characterized by fatigue and sometimes pain in the lower extremities with ambulation or prolonged standing. If the patient does not rest or sit, numbness and weakness may develop. Flexion of the spine increases the dimensions of the vertebral canal and neural foramina and can relieve the symptoms of neurogenic claudication. Consequently, patients presenting with neurogenic claudication may report improved walking stamina if they take a stooped posture and are often asymptomatic while sitting.
The cauda equina syndrome results from compression of the rootlets constituting the cauda equina. This syndrome presents with perineal numbness, urinary retention, and incontinence. Concomitant radiculopathy may be present. Urgent recognition and treatment of this syndrome are of great importance, as the prognosis for complete recovery largely depends on the duration of compression.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here