Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A variety of cystic lesions may occur in and around children's orbits. By far the commonest is the dermoid cyst, but other cystic choristomas may occur, including those lined by conjunctival and respiratory epithelium. Other cystic lesions include microphthalmos with cyst, congenital cystic eyeball, lacrimal ductal cyst, meningocele and meningoencephalocele, sinus mucocele, and teratoma. In some parts of the world, parasitic cysts involving organisms such as Echinococcus (hydatid cyst) and Cysticercosus are common. Hemorrhage within orbital venous–lymphatic malformations (lymphangiomas) may give rise to “chocolate” cysts and pseudocystic lesions of the orbital bones may be seen in fibrous dysplasia, ossifying fibroma, and aneurysmal bone cyst.
Dermoid cysts of the orbit and periorbital region are common in childhood, accounting for between 3% and 42% of orbital lesions in children in different reported series. A population-based study from Minnesota found a birth incidence for dermoid cysts of 1 in 638 live births. Most (81.5%) occurred at the superotemporal orbital rim, and 11.1% superonasally. Other sites are much rarer. They are developmental cystic choristomas, arising from ectodermal rests trapped at suture lines or within mesenchyme during orbital development.
Dermoid cysts are lined by keratinized stratified squamous epithelium with adnexal structures such as hair follicles, sebaceous and sweat glands found within their wall. They enlarge over time. Cyst leakage or rupture may give rise to an acute inflammatory response, followed by a chronic low-grade granulomatous inflammation. This inflammatory response is often subclinical, but is commonly seen surrounding longer-standing and larger dermoid cysts or those with bone changes.
Dermoids may be superficial or deep. Superficial dermoids usually overlie the orbital rim, without a component deep to the orbital septum, and are therefore strictly periorbital. Most dermoids presenting in childhood are superficial.
Some orbital cystic choristomas are lined by other types of epithelium, such as conjunctiva or respiratory epithelium, or even a mixture of these with stratified squamous epithelium (see below).
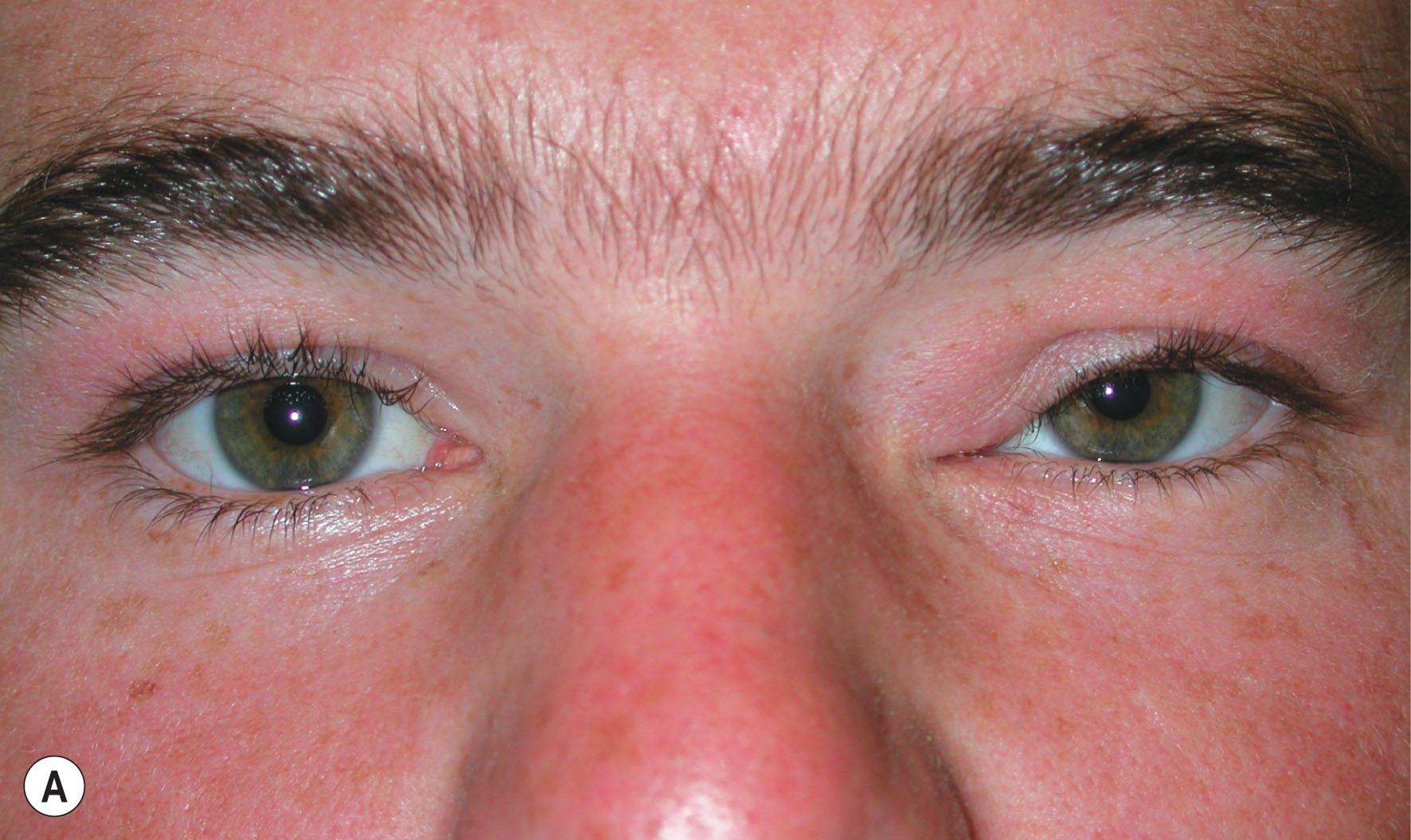
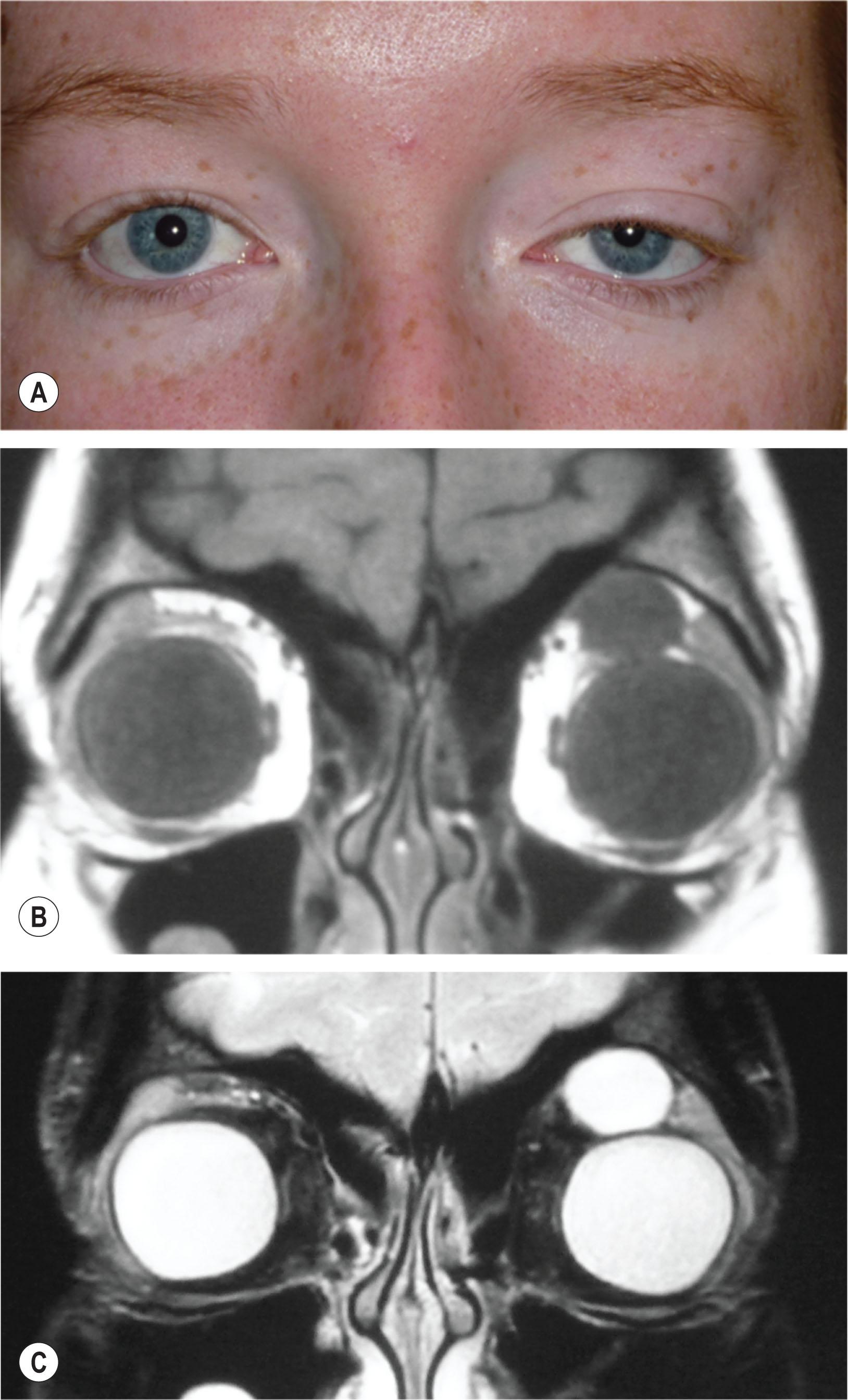
These often present in infancy as a rounded mass, typically at the sup-erotemporal ( Fig. 27.1 ) margin of the orbit. Between 10% and 25% arise in the superomedial orbit ( Fig. 27.2A,B ). They are painless, smooth, non-tender, firm, often mobile, or in some cases relatively fixed to the underlying periosteum and bone. Superotemporal periorbital dermoids are situated outside the orbit, and cause no displacement of the globe. The orbital rim is usually palpable behind their posterior edge. Unsuspected deep extension into the temporal fossa, posterior orbit, or even intracranial space occasionally occurs in apparently superficial dermoid cysts, but these deeper-extending dermoid cysts are usually clinically more deeply located, less mobile, and it is not possible to pass a finger behind their posterior margin to palpate the orbital rim.

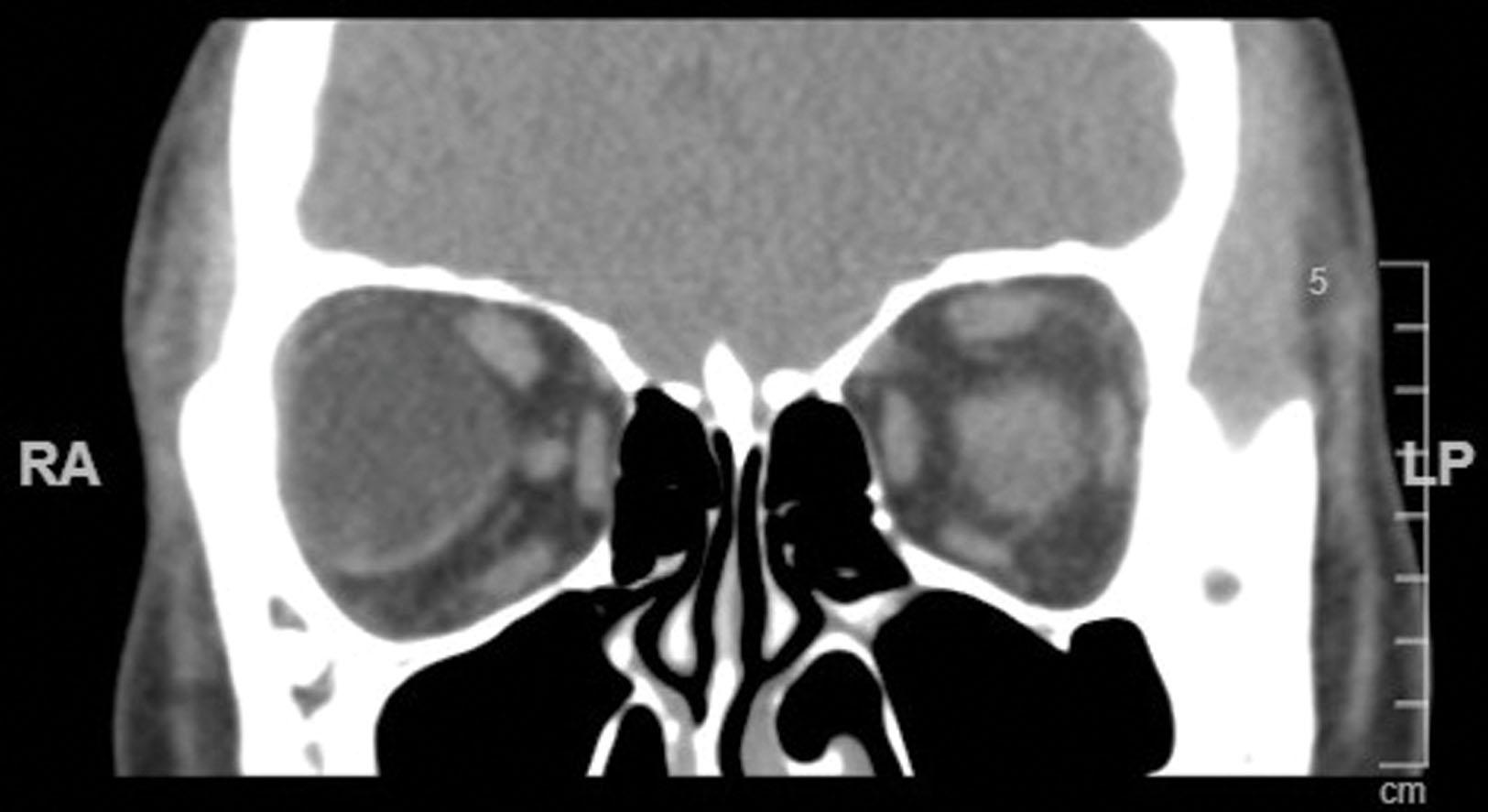
The radiologic appearance of a dermoid cyst is characteristic: on computed tomography (CT) scan, the best modality to highlight bony features, a rounded discrete mass is associated with thinning and smooth erosion or remodeling of the underlying bone. The contents are often of heterogeneous density on CT and magnetic resonance imaging (MRI). Fat lucency is noted in 71%, and its presence within the cyst is considered diagnostic. Fluid levels within the cyst may sometimes be seen as the lighter oily secretions of sebaceous glands float upon more aqueous fluid.
Preoperative assessment of any dermoid cyst is essential to rule out deep extension. If the cyst is small, mobile, and easily palpable for its entire extent, imaging may not be necessary. Larger cysts with ill-defined, deep margins, and medially placed dermoids, are best assessed with a CT scan or MRI.
Excision of superficial dermoid cysts is relatively simple (see Fig. 27.2C ). Surgical excision by the age of 5 years reduces the risk of accidental rupture or inflammatory episodes related to spontaneous leakage. The incision may be situated directly over the lesion, above, below, or through the eyebrow. A skin-crease approach or endoscopic removal leave a less conspicuous postoperative scar, but often these lesions lie beyond the natural upper lid crease. Although excision of the intact cyst is desirable, intraoperative rupture is not disastrous if the contents and the entire cyst wall are carefully removed. Decompression of larger cysts may be helpful to expose the underlying bone or posterior aspects of the lesion. Failure to excise the cyst wall completely, or residual cyst contents, can elicit a chronic inflammatory reaction with sinus formation and persistent discharge.
These usually present in adolescence and adulthood with gradual enlargement and displacement of orbital contents, and bony remodeling (see Fig. 19.12 ), but they can present similarly in infancy. Deeper cysts may have only a squamous epithelial lining, and are therefore classified as epidermoid cysts. Deep dermoids are often not palpable, but sometimes their smooth and rounded anterior margin can be palpated, although they may extend to the orbital apex. Proptosis and/or globe displacement are predominant features but ocular motility, visual disturbances, and pain may occur. Dermoid cysts rarely may be within ( Fig. 27.3 ) or attached to the lateral rectus muscle.
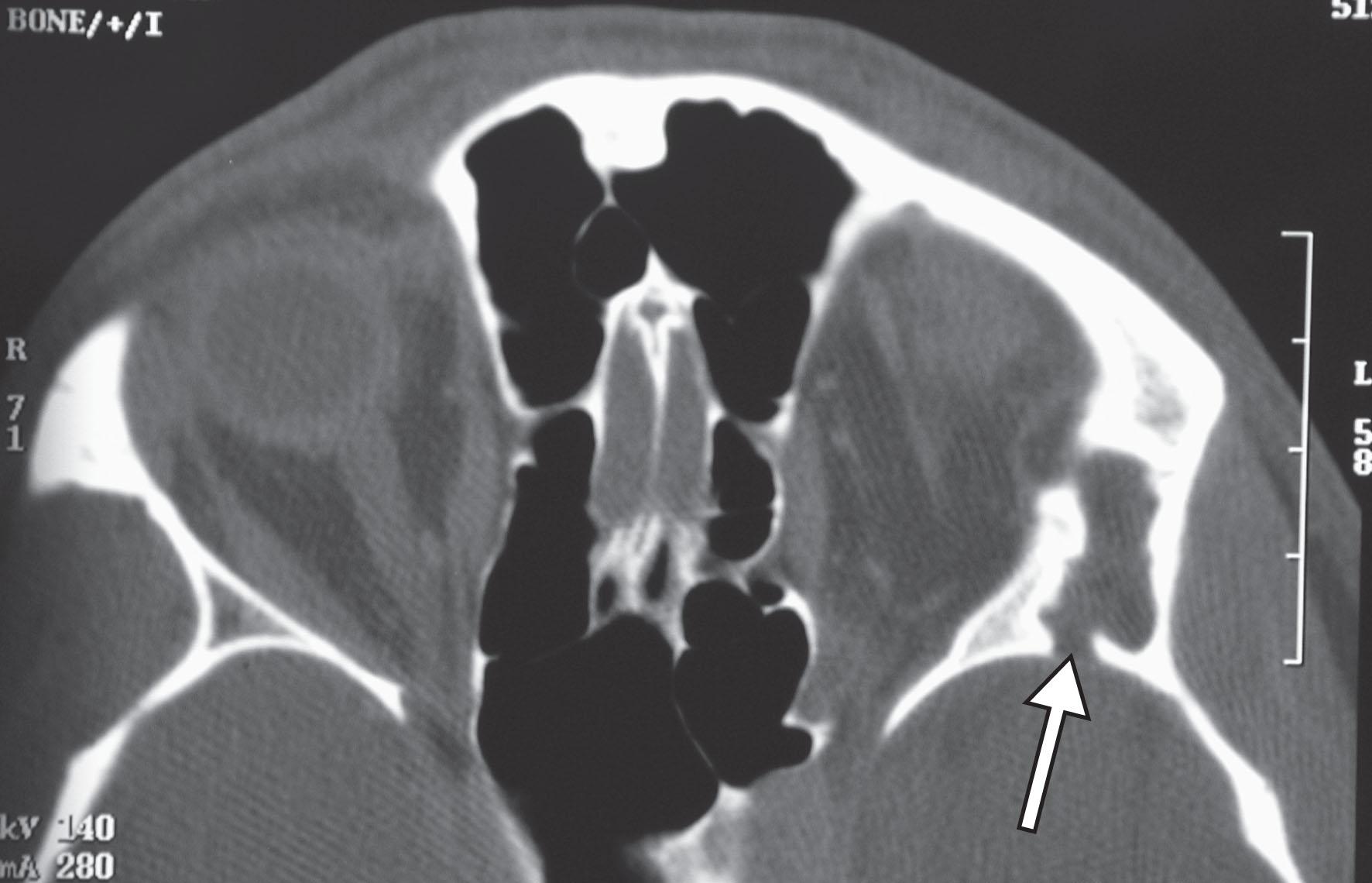
Some orbital dermoids may straddle the orbit and temporal fossa, with a communication between the two parts passing through the lateral orbital rim or wall ( Fig. 27.4 ). These “dumbbell” dermoids may present with the typical signs of a more superficial dermoid, but extend into the temporal fossa in an hour-glass configuration (see Fig. 27.4 ) and may be associated with temporalis swelling. , Very rarely, proptosis with or without diplopia triggered by mastication (masticatory oscillopsia) can result from pressure on a communicating cyst by temporalis muscle contraction with chewing. Presentation with orbital cellulitis related to a discharging sinus tract arising from an orbital dermoid has been reported. , Simultaneous orbital and temporalis fossa dermoid cysts without communication may very rarely occur.
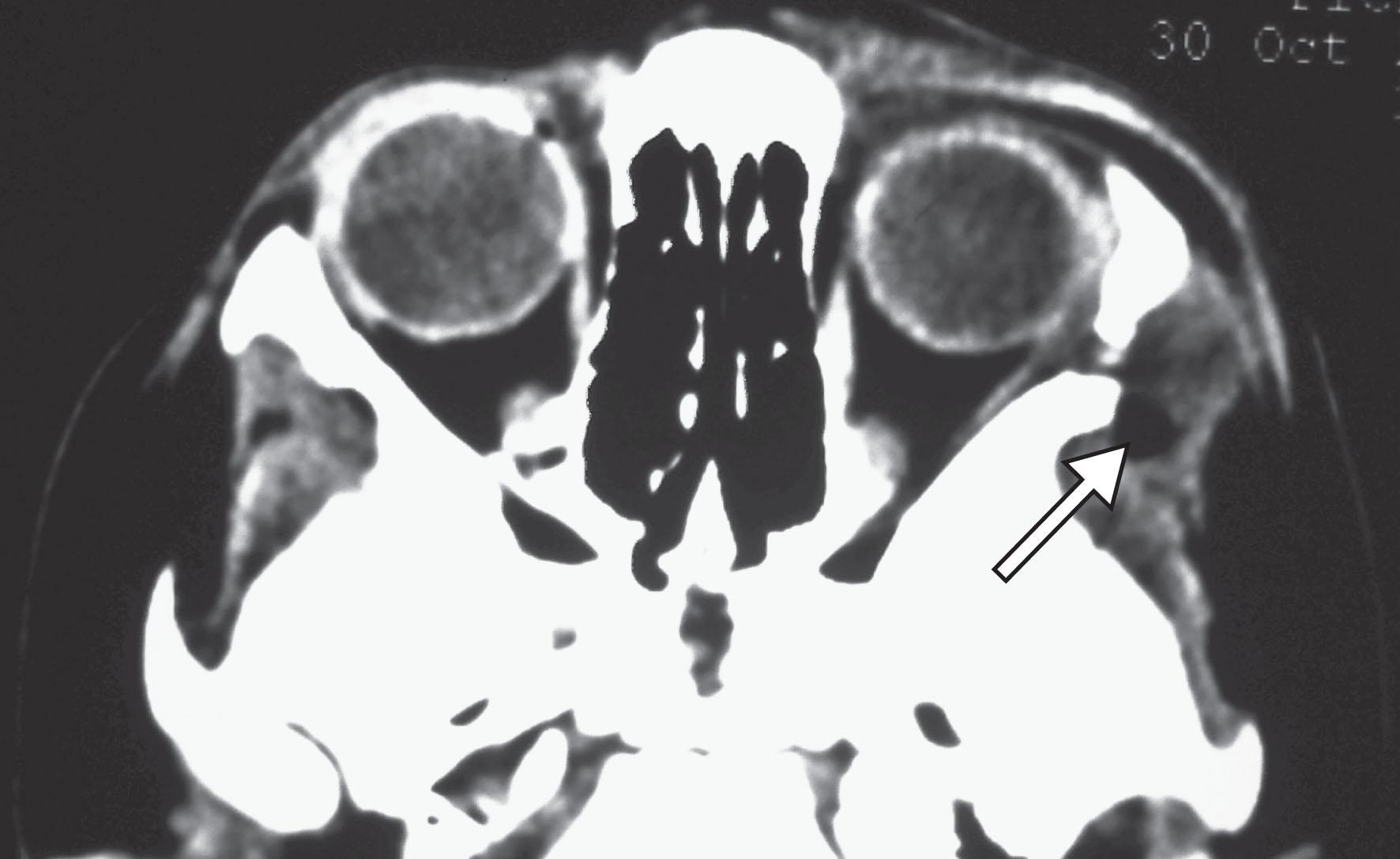
The CT findings of deep dermoids are similar to those of superficial dermoids except for the frequent presence of irregular orbital wall defects as well as sclerosis, irregular scalloping, or notching of the underlying bone ( Fig. 27.5 ). The walls of large dermoid cysts may demonstrate irregular “egg-shell” calcification. There may be evidence of surrounding inflammation and scarring from subclinical episodic leakage of the cyst contents. On MRI, cyst contents are of low signal on T1-weighted images, and on T2, are isointense or hypointense to vitreous, and hyperintense to fat ( Fig. 27.6 ). The cyst wall often enhances.
Surgical removal of deep dermoids can be difficult. Preoperative clinical and radiologic assessment is essential to plan the appropriate surgical approach, which may involve combined anterior and lateral orbitotomies or focal marginotomies. Incomplete excision can lead to a chronically discharging sinus with episodes of infection ( Fig. 27.7 ). A neurosurgical approach with craniectomy may be necessary for safe and complete excision of an orbital dermoid extending intracranially.
Cystic choristomas lined by conjunctival epithelium are usually called “conjunctival dermoids.” One-half of these arise in the medial orbit, usually in teenagers and young adults ( Fig. 29.8 ). They are not attached to the orbital bones, and are lined by typical conjunctival epithelium with goblet cells and, sometimes, adnexal structures with mucinous or mixed content in the cyst. They are managed by complete excision ( Fig. 29.8D ). These cysts may have a mixture of conjunctival and dermal lining. Congenital cysts lined by conjunctiva in the region of the common sheath of the superior rectus and levator palpebrae muscles have been described.
Conjunctival dermoids should not be confused with conjunctival inclusion cysts, which are acquired lesions due to the implantation of conjunctival epithelium within the orbit after trauma or surgery, most commonly strabismus or vitreoretinal surgery. They may present many decades after trauma or surgery.
Cysts lined by respiratory epithelium can occur in the orbit as congenital lesions, but also may occur after trauma, with the implantation of respiratory epithelium from the nasal cavity or paranasal sinuses. A mucocele arising from the paranasal sinuses is also lined by respiratory epithelium, often very attenuated, but is a different entity (see below).
Congenital respiratory epithelial cysts are rare. They may present in childhood or later in adult life, particularly deeper lesions.
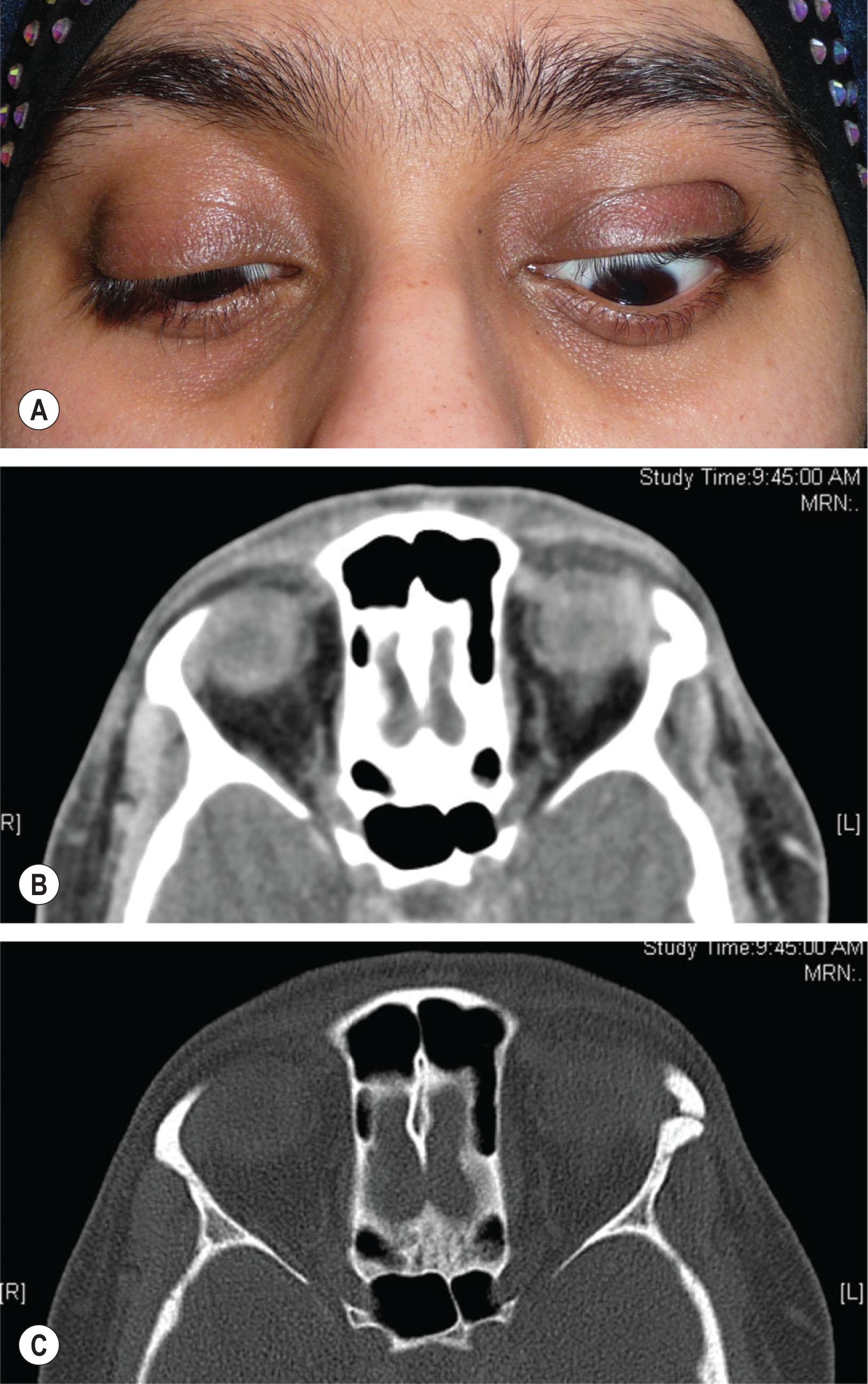
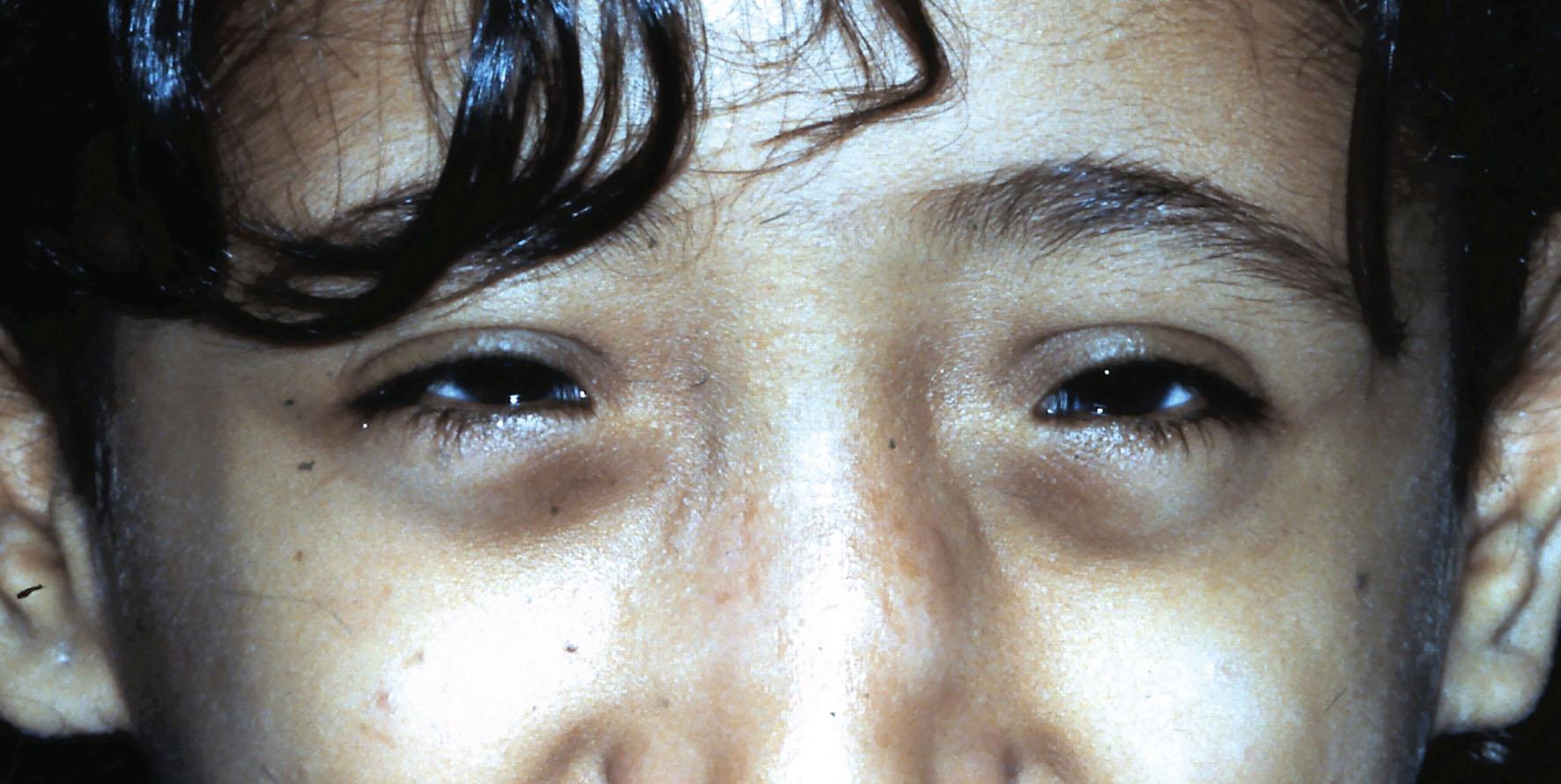
These rare abnormalities may be congenital or acquired. Congenital lesions arise from a presumed defective separation of neuroectoderm from surface ectoderm, resulting in a bony dehiscence with a “cystic” herniation of dura into the orbit, either alone (meningocele) or with brain tissue (meningoencephalocele, MEC). The commonest form is a frontoethmoidal MEC, and these occur much more frequently in south-east Asia. They may be associated with an optic disc anomaly ; basal encephalocele should always be excluded in a child with a morning glory disc, especially if there is a midline facial anomaly such as telecanthus and/or hypertelorism ( Fig. 27.9 ), notched or cleft lip or palate (see Chapters 26 and 53 ). Significant cerebral vascular anomalies may accompany the presence of a morning glory disc.
Orbital encephaloceles may be acquired as a result of head injury and orbital fracture, with herniation of the dura, with or without brain, through the bony defect. Occasionally, after relatively trivial trauma, an orbital roof fracture in a child may progressively expand (a “growing fracture”) as the leptomeninges herniate into the fracture, forming a “cyst.” This may expand, leading to progressive proptosis which may be pulsatile.
Congenital orbital meningoencephaloceles may be anterior or posterior. Anterior lesions herniate through single or multiple defects in the region of the sutures dividing the frontal, ethmoid, lacrimal, and maxillary bones. They usually present as a congenital cystic swelling of the medial orbit extending onto the face, accompanied by telecanthus and, frequently, epiphora. They may present in infancy and early childhood with gradually increasing forward and lateral globe displacement. Atypical presentations may occur, such as the 10 mm bluish cystic mass in the superonasal fornix of a 1-month-old patient, which was found to be a meningoencephalocele.
Classically, the cyst increases in size on straining or crying. It may be fluctuant, pulsatile, reducible with gentle pressure, and it may transilluminate. Anterior encephaloceles are important in the differential diagnosis of any medial canthal swelling. They may be mistaken for sinus mucoceles, dermoid cysts, or nasolacrimal duct mucoceles. A bony defect with intracranial communication is evident on CT or MRI scan. Three-dimensional CT reconstruction may be helpful in planning surgery, which is usually performed by craniofacial, neurosurgical and/or maxillofacial teams. Posterior encephaloceles herniate into the orbit via the optic foramen, orbital fissures, or a bony defect. They present with slowly progressive, sometimes pulsatile, proptosis. Occasionally, posterior encephaloceles present later in life.
CT or MRI scans demonstrate the size and contents of the cyst. Posterior encephaloceles are particularly associated with the sphenoid wing dysplasia of neurofibromatosis type 1 (NF1). Most will have visual impairment, and all have an associated plexiform neurofibroma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here