Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Organizing pneumonia (OP) is a histologic pattern characterized by the presence of intraluminal granulation tissue polyps within alveolar ducts and surrounding alveoli associated with chronic inflammation of the surrounding lung parenchyma. Because the granulation tissue polyps frequently also involve the bronchioles, the pattern was previously known as bronchiolitis obliterans organizing pneumonia (BOOP). However, given the confusion of this entity with bronchiolitis obliterans (synonym: obliterative or constrictive bronchiolitis), this terminology has fallen out of favor. OP may occur in association with several underlying conditions, including infections, connective tissue diseases, inflammatory bowel disease, inhalational injury, hypersensitivity pneumonitis, drug reaction, radiation therapy, and aspiration. In some patients, no underlying cause is found, however, and the condition is termed cryptogenic organizing pneumonia (COP) ( Box 29.1 ).
Idiopathic (cryptogenic organizing pneumonia)
Connective tissue disease
Drug reaction
Infection (including bacteria, Mycoplasma, fungi, and Pneumocystis )
Human immunodeficiency virus related
Aspiration
Hemorrhage
Hypersensitivity pneumonitis
Malignancy (solid tumor and hematologic)
Posttransplantation (particularly stem cell transplantation)
Postradiation
Inhalational injury (toxic fume or smoke inhalation)
Vasculitis syndromes (particularly granulomatosis with polyangiitis and eosinophilic granulomatosis with polyangiitis [Churg-Strauss syndrome])
Inflammatory bowel disease
Nonspecific reaction adjacent to other lesions (e.g., infarct, abscess, and neoplasm)
Cocaine abuse
Anthrax vaccination (rare)
COP accounts for 4% to 12% of cases of idiopathic interstitial pneumonias. The exact incidence and prevalence of COP is not known as many cases are undiagnosed, and cases described in the literature are often based on presumptive diagnosis. Although COP and secondary OP are thought to occur at similar rates, the cause for secondary OP is often difficult to identify or not exhaustively sought after. A population-based epidemiologic review of OP in Iceland estimated that the mean annual incidence of OP was 1.97 per 100,000 population, including 1.10 cases of COP and 0.87 cases of secondary OP per 100,000 population, respectively. COP has an equal sex distribution and is approximately twice as common in nonsmokers than in smokers. The average age of presentation is 50 to 60 years (range, 20–80 years). Occasionally, COP may have seasonal recurrence. In one study the authors reported 12 patients with seasonal recurrence of COP for 3 to 11 years. In all 12 patients symptoms recurred between late February and early May every year, tending to increase in severity each year. One case has been reported of recurrent COP starting 2 to 3 days before the menstrual period and resolving within 5 to 10 days.
Patients usually present with cough and progressive dyspnea of relatively short duration (median, <3 months). The cough may be dry or productive of clear sputum. Other common manifestations include weight loss, chills, and intermittent fever. The clinical presentation mimics that of community-acquired pneumonia. Auscultation usually reveals localized or widespread crackles. Finger clubbing is absent.
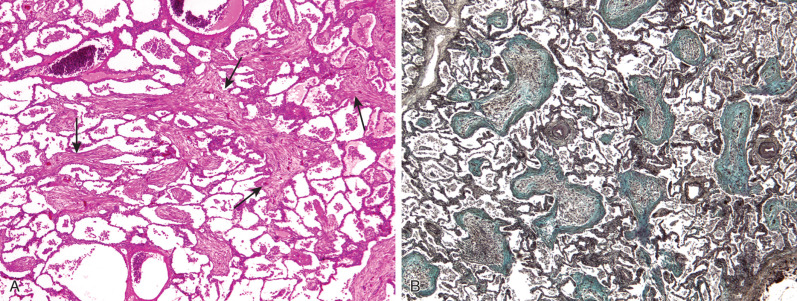
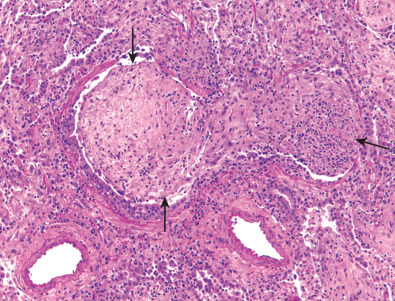
OP is characterized histologically by the presence of intraluminal plugs of granulation tissue within alveolar ducts and surrounding alveoli ( Fig. 29.1 ), with or without concomitant granulation tissue polyps within the respiratory bronchioles ( Fig. 29.2 ). The distribution is typically patchy, and the connective tissue is of the same age. Mild associated interstitial inflammation is typically present with type II cell metaplasia and an increase in alveolar macrophages. Even though the American Thoracic Society/European Respiratory Society consensus statement classifies COP as a form of idiopathic interstitial pneumonia, the abnormalities are mainly intraalveolar.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here