Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Pathogenesis: direct eye contact with infected secretions; most common isolates are S. pneumoniae , S. aureus , H. influenza , and Moraxella catarrhalis ; uncommon but serious are gonococci and meningococci.
Diagnosis
Presentation: acute onset of redness, grittiness, burning and sticky discharge affecting first one then both eyes.
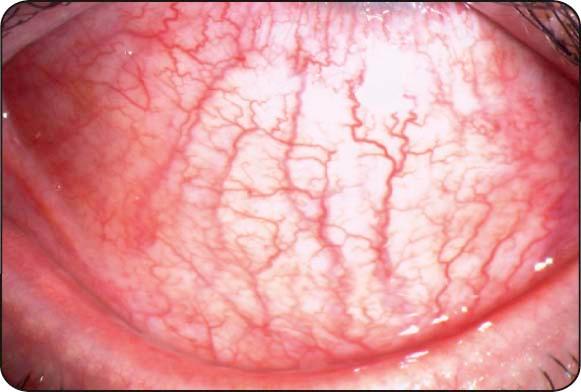
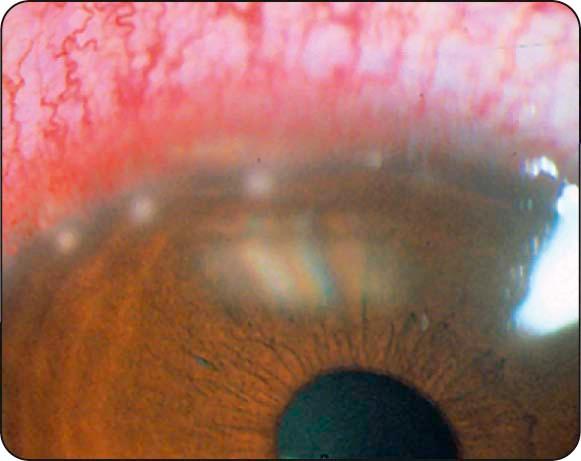
Conjunctival injection: maximal toward the fornices ( Fig. 5.1 ).
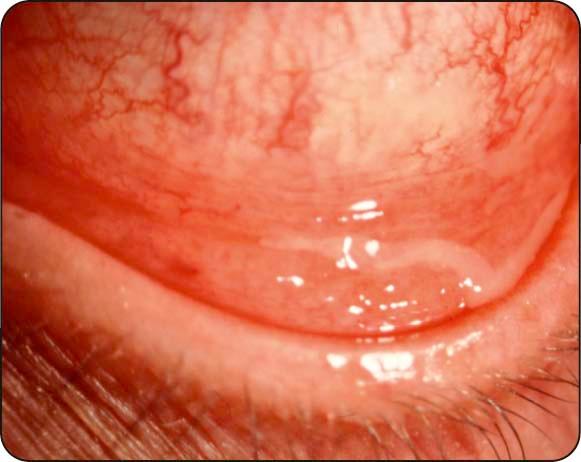
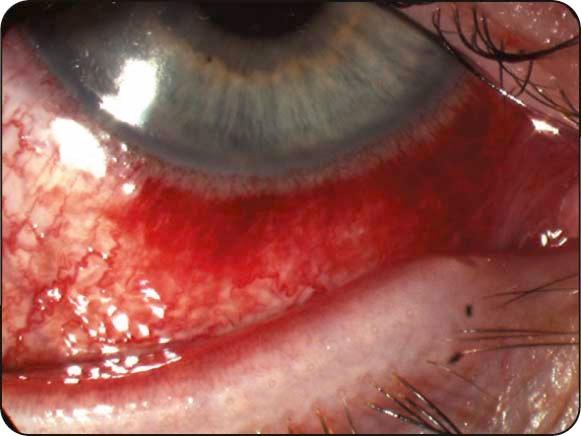
Discharge: (a) typically mucopurulent ( Fig. 5.2 ); (b) hyperacute purulent ( Fig. 5.3 ) in gonococcal or meningococcal infection.

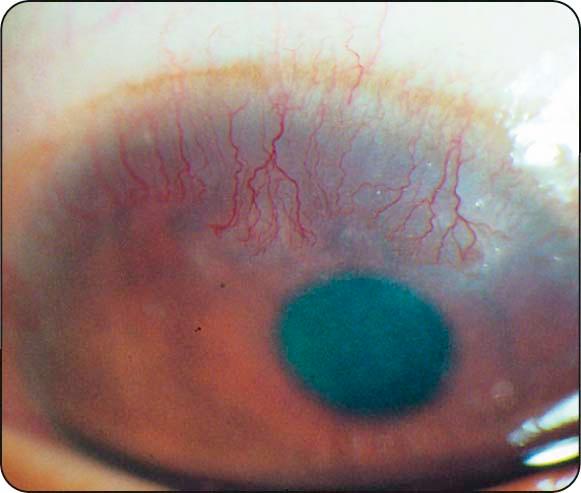
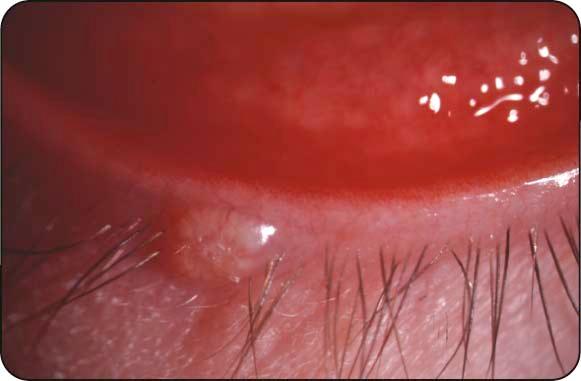
Eyelids: oedema and erythema ( Fig. 5.4 ) in severe infection.

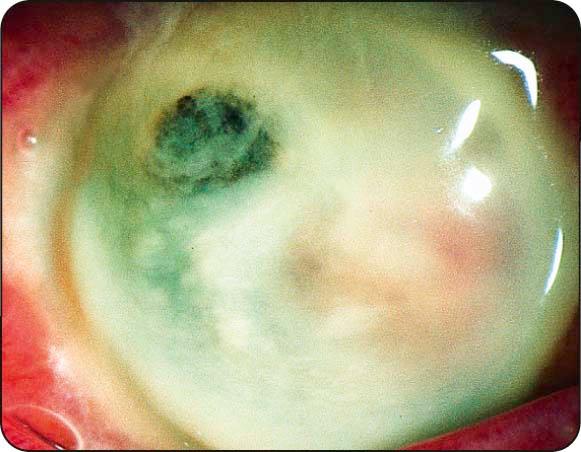
Cornea: (a) mild punctate epithelial erosions; (b) ulceration ( Fig. 5.5 ) may occur in gonococcal and meningococcal infection.
Investigations: not performed routinely but may be indicated in severe or atypical cases (e.g. urgent Gram staining to exclude gonococcal or meningococcal infection), and polymerase chain reaction (PCR) for Chlamydia .
Treatment
Topical antibiotics: options include (a) chloramphenicol, (b) aminoglycosides (gentamicin, neomycin), (c) quinolones (ciprofloxacin, ofloxacin, levofloxacin, lomefloxacin, gatifloxacin, moxifloxacin), and (d) polymyxin B, fusidic acid, or bacitracin. Some practitioners believe that chloramphenicol should not be used for routine treatment because of a possible link with aplastic anaemia. Gonococcal and meningococcal conjunctivitis require a quinolone, gentamicin, chloramphenicol, or bacitracin 1–2 hourly as well as systemic therapy.
Systemic antibiotics: (a) gonococcal infection is treated with a third-generation cephalosporin, (b) H. influenzae , particularly in children, requires oral amoxicillin with clavulanic acid, and (c) meningococcal infection with intramuscular benzylpenicillin.
Topical steroids: may reduce scarring in severe conjunctivitis.
Pathogenesis: oculogenital infection usually caused by serovars (serological variants) D–K of Chlamydia trachomatis. Transmission is usually by autoinoculation from genital secretions. In males, chlamydial infection is the most common cause of nongonococcal urethritis, and is frequently asymptomatic; in females, chlamydial urethritis typically causes dysuria and discharge.
Diagnosis
Presentation: subacute onset of unilateral or bilateral redness, watering and discharge.
Discharge: watery or mucopurulent.
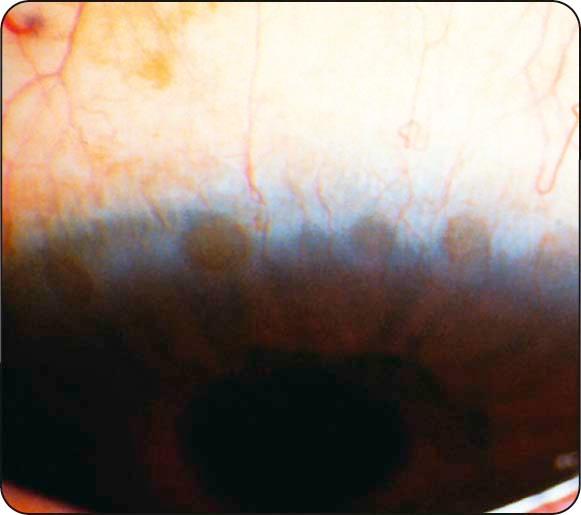
Conjunctiva: (a) large follicles are typical ( Fig. 5.6 ); (b) chronic cases have less prominent follicles and may develop mild conjunctival scarring and superior corneal pannus ( Fig. 5.7 ).

Cornea: superficial punctate keratitis is common, and peripheral subepithelial corneal infiltrates ( Fig. 5.8 ) may appear 2–3 weeks after onset.
Tender preauricular lymphadenopathy: very common.
Investigations: (a) conjunctival scraping with Giemsa staining for basophilic intracytoplasmic bodies, (b) PCR, (c) immunoassay, and (d) cell culture and serology in selected cases.
Treatment
Systemic antibiotics: options include (a) azithromycin 1 g repeated after 1 week (second or third course required in 30%), (b) doxycycline 100 mg twice daily for 10 days (avoid in pregnancy/breast-feeding and children), and (c) erythromycin, amoxicillin, and ciprofloxacin as alternatives.
Topical antibiotics: supplementary erythromycin or tetracycline for rapid relief of ocular symptoms.
Pathogenesis: recurrent infection occurring in individuals living in poor overcrowded communities eliciting a chronic immune response, particularly in vulnerable young children. Trachoma is associated principally with infection by serovars A, B, Ba, and C of C. trachomatis ; the fly is an important vector.
Diagnosis
Active stage: (a) mixed follicular/papillary conjunctivitis ( Fig. 5.9 ), (b) mucopurulent discharge, and (c) superior epithelial keratitis and pannus formation.

Cicatricial disease: (a) conjunctival scars, most prominent on the upper tarsus (linear/stellate ( Fig. 5.10 ), or broad and confluent [Arlt lines; Fig. 5.11 ]), (b) superior limbal follicles which may leave a row of depressions (Herbert pits; Fig. 5.12 ), (c) trichiasis, distichiasis, and cicatricial entropion, (d) dry eye (goblet cells and lacrimal gland ductule destruction), and (e) eventual severe corneal vascularization and opacification ( Fig. 5.13 ).



World Health Organization grading of trachoma
TF = trachomatous inflammation (follicular): five or more follicles (>0.5 mm) on the superior tarsus.
TI = trachomatous inflammation (intense): diffuse involvement of the tarsal conjunctiva, obscuring 50% or more of the normal deep tarsal vessels; papillae are evident.
TS = trachomatous conjunctival scarring: easily visible fibrous white tarsal bands.
TT = trachomatous trichiasis: at least one lash touching the globe.
CO = corneal opacity sufficient to blur details of at least part of the pupillary margin.
Treatment
SAFE strategy: (a) s urgery for trichiasis, (b) a ntibiotics for active disease, (c) f acial hygiene, and (d) e nvironmental improvement.
Antibiotics: (a) systemic azithromycin (single dose of 20 mg/kg up to 1 g) or erythromycin 500 mg twice daily for 14 days; (b) tetracycline ointment is less effective than oral treatment and should be given for 6 weeks. More than one antibiotic may be required, and communities may need to receive annual treatment to suppress infection.
Hygiene: personal and environmental.
Surgery: for entropion and trichiasis; bilamellar tarsal rotation is commonly performed.
Pathogenesis: conjunctival inflammation developing within the first month of life, usually as the result of infection transmitted from mother to baby during delivery. Staphylococci are usually responsible for mild conjunctivitis, but severe systemic involvement can result from infection with C. trachomatis , N. gonorrhoeae , and herpes simplex virus (HSV); chemical conjunctival irritation from infection prophylaxis may also occur.
Diagnosis
Presentation: (a) chemical irritation—first few days, (b) gonococcal—first week, (c) staphylococci and other bacteria—end of the first week, (d) herpes simplex—1–2 weeks, and (e) chlamydia—1–3 weeks.
Discharge: depends on cause.
Eyelids: (a) severe oedema may denote gonococcal infection ( Fig. 5.14 ); (b) vesicles in HSV infection.

Investigations in moderate to severe cases: (a) conjunctival scrapings for Gram and Giemsa staining, (b) conjunctival swabs for bacterial culture (chocolate agar if N. gonorrhoeae suspected), (c) Papanicolaou smear, (d) separate scrapings for PCR if indicated, and (e) viral culture for HSV of conjunctival scrapings or skin vesicle fluid.
Treatment
Prophylaxis: single instillation of povidone–iodine 2.5%, erythromycin 0.5%, tetracycline 1% ointment, or silver nitrate 1% is utilized in areas where gonococcal infection is common; a single intramuscular dose of benzylpenicillin is given when maternal infection is present.
Chemical conjunctivitis: no treatment apart from artificial tears.
Mild conjunctivitis (sticky eye): may require a broad-spectrum topical antibiotic (e.g. fusidic acid, chloramphenicol).
Chlamydial conjunctivitis: oral (± topical) erythromycin for 2 weeks.
Gonococcal conjunctivitis: hospital admission and systemic third-generation cephalosporin; co-treatment for chlamydia is prudent.
Herpes simplex infection: should always be regarded as a systemic condition and treated with high-dose intravenous and topical aciclovir; early diagnosis and treatment of encephalitis may be life-saving or prevent serious disability.
Co-management: paediatrician, microbiologist, and genitourinary specialist.
Pathogenesis: highly contagious disease that may be sporadic or epidemic. Transmission is by contact with respiratory or ocular secretions, including fomites such as contaminated towels.
Diagnosis
Nonspecific acute follicular conjunctivitis: most common form, usually mild; sore throat may be present.
Pharyngoconjunctival fever (PCF): spread by droplets from patients with associated upper respiratory tract infection; keratitis (usually mild) occurs in approximately 30%.
Epidemic keratoconjunctivitis (EKC): most severe type, associated with keratitis in approximately 80% of cases; (a) eyelid oedema, (b) tender pre-auricular lymphadenopathy, (c) petechial conjunctival haemorrhages ( Fig. 5.15 ), (d) chemosis, and (e) pseudomembranes ( Fig. 5.16 ).

Chronic/relapsing conjunctivitis: nonspecific follicular/papillary lesions; can rarely persist for years.
Keratitis: (a) nonstaining epithelial microcysts (early), (b) punctate epithelial keratitis (resolves within 2 weeks), and (c) focal white subepithelial infiltrates ( Fig. 5.17 ) that may persist or recur over months or years.

Differential diagnosis: (a) acute haemorrhagic conjunctivitis (tropical areas, enterovirus or coxsackievirus), (b) herpes simplex infection (usually unilateral, may have skin vesicles), (c) systemic viral infections (varicella, measles, mumps), and (d) molluscum contagiosum (see below).
Investigations: usually unnecessary but may include the following: (a) Giemsa stain shows mononuclear cells in adenoviral and multinucleated giant cells in herpetic disease, (b) PCR is sensitive and specific for viral DNA, (c) viral culture is expensive and slow but highly specific, and (d) ‘point-of-care’ immunochromatography test is rapid and accurate.
Treatment
Reduction of transmission risk: meticulous hygiene and avoidance of towel sharing.
Topical steroids: for symptomatic keratitis do not speed resolution, and the lesions commonly recur after early discontinuation; may extend the infectious period.
Other measures: (a) artificial tears for symptomatic relief, (b) discontinuation of contact lens wear, (c) removal of symptomatic pseudomembranes, (d) topical antibiotics for secondary bacterial infection, (e) povidone–iodine is effective against free adenovirus, (f) ganciclovir shows some activity against adenovirus.
Pathogenesis: skin infection caused by a DNA poxvirus that typically affects children. Transmission is by contact with subsequent autoinoculation. Virus shedding from a lesion on the lid margin may be associated with conjunctivitis.
Diagnosis
Presentation: chronic unilateral ocular irritation and mild mucoid discharge.
Signs: (a) waxy umbilicated nodule on the lid margin, and (b) follicular conjunctivitis ( Fig. 5.18 ).
Treatment: expression, facilitated by a small nick at the lesion apex.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here