Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Development of the spine and spinal cord is a complex process determined by an intricate chain of embryologic stages under precise genetic control. Although congenital abnormalities of spine development are frequently classified according to the specific derangement responsible for the anomaly, the pathogenesis of some abnormalities is not well understood. We review these anomalies while classifying them from clinical and imaging perspectives. These include three major categories: open spinal dysraphism (OSD), which presents clinically with a usually low lumbosacral skin defect with neural tissue exposed at this site; closed spinal dysraphism (CSD) with a subcutaneous mass that typically manifests clinically as a low lumbar skin-covered mass situated above the gluteal cleft and extending asymmetrically into one buttock; and CSD without a subcutaneous mass, which may come to clinical attention secondary to spinal cord tethering or other neurologic symptoms, associated cutaneous stigmata, or congenital spinal deformities. Within each of these categories, we will organize the described malformations depending on their responsible embryologic derangements.
Spinal cord development occurs during gestational weeks 2 to 6 and follows three consecutive steps: gastrulation (weeks 2-3), primary neurulation (weeks 3-4), and secondary neurulation with retrogressive differentiation (weeks 5-6).
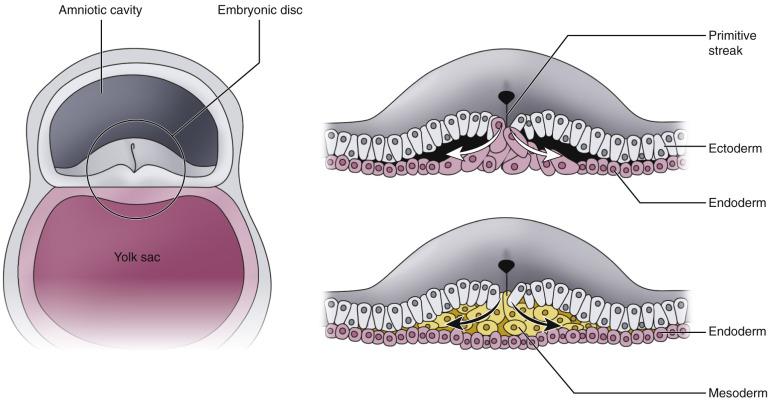
During the first 10 to 14 days of life, the embryo consists of two cell layers: the ectoderm facing the amniotic cavity and the endoderm facing the yolk sac. Gastrulation occurs at weeks 2 to 3 of gestation and transforms the embryo into a trilayered structure with formation of an intervening third layer, the mesoderm. This happens as follows: the primitive streak is a strip of thickened ectoderm that forms in the midline of the caudal aspect of the dorsal surface of the embryo. The primitive streak is composed of totipotential cells and is an area of active mitotic activity. Its cranial end thickens and forms a knoblike structure, Hensen's node, that contains a central depression called the primitive pit. Ectodermal cells migrate to the primitive streak and transit inward through the primitive pit. Once they reach the interface between ectoderm and endoderm, they migrate laterally to form the mesoderm. Subsequently the paired mesodermal anlages join in the midline to form the notochord. The notochord is a transient embryologic structure that is essential for patterning of surrounding tissues by secreting a signaling molecule called sonic hedgehog (shh) . The notochord regulates development of ectoderm-derived structures (in particular differentiation of the neural plate), patterning of mesoderm-derived structures including differentiation of somites (which form the vertebral column and paraspinal musculature), and development of the cardiovascular system and endoderm-derived organs including organs of the respiratory and gastrointestinal tract.
At the beginning of the third gestational week, the notochord induces the differentiation of the neuroectoderm from the ectoderm. The neuroectoderm is originally flat and forms the neural plate, which is continuous laterally on both sides with the remainder of the ectoderm. The neural plate progressively invaginates along its central axis, forming a neural groove, with its margins forming neural folds that approximate each other in the midline. The neural folds finally fuse and form the neural tube. The process of neural tube closure was traditionally thought to start at the level of the craniocervical junction and proceed rostrally and caudally in a zipperlike fashion. Recent pathologic and epidemiologic evidence suggests that neural tube closure occurs at multiple sites rather than being a continuous bidirectional closure. This multisite closure theory better explains the pathogenesis of human neural tube defects. The caudal end of the neural tube (posterior neuropore) closes at 27 to 28 days of gestation—after the cranial end (anterior neuropore), which closes at about 24 to 25 days of gestation. Closure of the entire neural tube terminates the process of primary neurulation. The neural tube formed during primary neurulation will later develop into the brain and the upper 90% of the spinal cord.
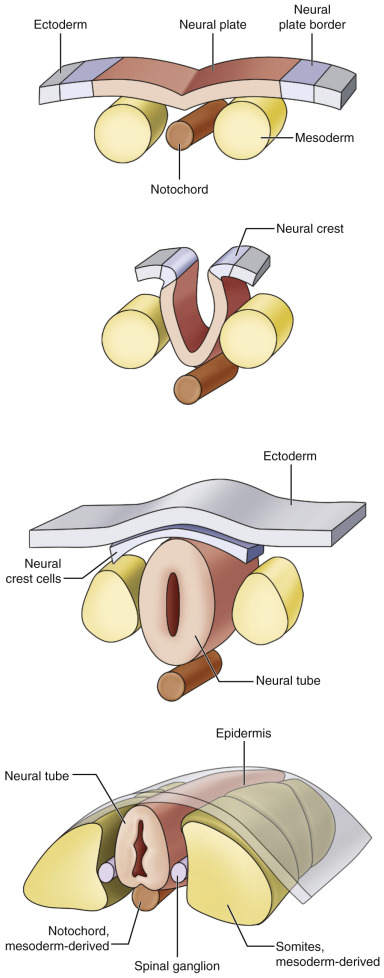
While the neural tube is closing, it detaches from the surface ectoderm, and the latter closes dorsal to the neural tube to provide a continuous skin covering of the neural tube. This process is called disjunction . The mesenchyme that migrates dorsally between the skin and neural tube forms the meninges, neural arches, and the paraspinal muscles.
The cells at the bilateral margins between ectoderm and neuroectoderm form the neural crests. While the neural plate invaginates during its closure, the neural crests detach from the ectoderm and neural plate and fragment on both sides of the neural tube to form the sensory ganglia.
Secondary neurulation is responsible for the formation of the tip of the conus medullaris and filum terminale. It refers to formation of a secondary neural tube at the caudal aspect of the posterior neuropore. This starts as a caudal cell mass of undifferentiated totipotential cells originating from the caudal end of the primitive streak. The caudal cell mass undergoes canalization with formation of a central canal. The central canal of the caudal mass merges with the neural tube canal formed during primary neurulation.
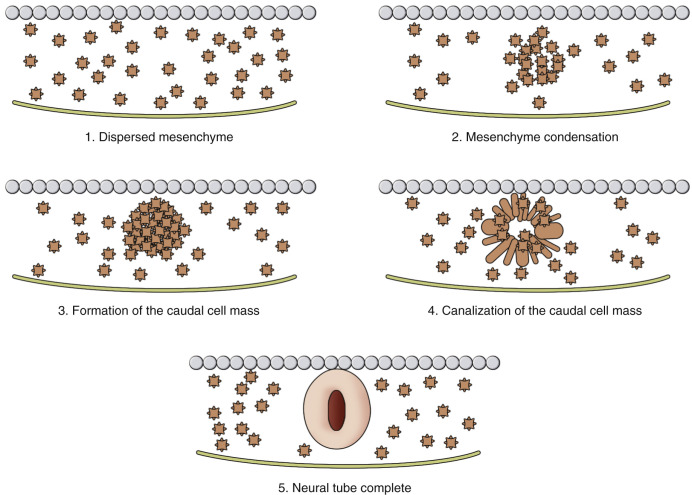
Retrogressive differentiation is the step that follows secondary neurulation. This is an apoptotic process where there is regression and differentiation of the distal segment formed during secondary neurulation, which eventually becomes the tip of the conus medullaris and the filum terminale. At this stage, the ventriculus terminalis is a focal expansion of the central canal present at the distal conus. It will subsequently regress in the majority of individuals.
Formation of the anorectal and genitourinary tract from the cloaca occurs simultaneously and in close proximity to the caudal cell mass. The caudal spine should therefore always be evaluated in the presence of anomalies of the anorectal and/or lower genitourinary tract.
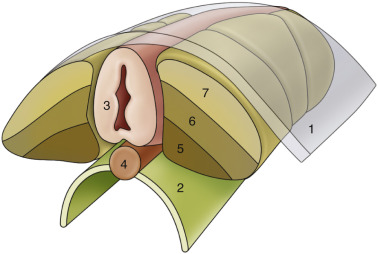
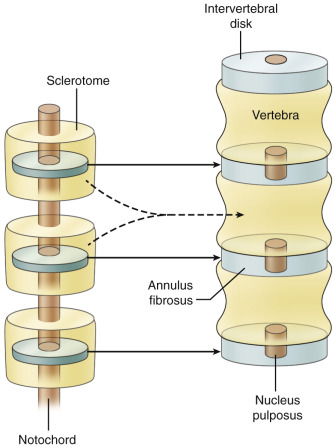
The mesoderm forms a somite plate on each side of the neural tube and notochord. This paired plate becomes segmented into individual somites in a cyclic process that progresses from the cranial to the caudal end of the embryo. Each somite separates into a sclerotome, a dermatome, and a myotome. Sclerotomes migrate toward the midline to surround the notochord and overlying neural tube and form the vertebral bodies. Dermatomes and myotomes remain in place at the lateral aspect of the neural tube and notochord. The myotomes give rise to the paraspinal musculature. Each sclerotome separates into two halves. The caudal half of each sclerotome joins the cephalic half of the subjacent sclerotome to form a vertebral body. The intervertebral disk is formed in the space between the separated two halves of each sclerotome. Mesenchymal cells migrate in this space to form the anulus fibrosus, and the notochord remnants form the nucleus pulposus. Thus, formation of a normal vertebral body is the result of the intersegmental union between two adjacent sclerotomes. The portions of the sclerotomes that surround the neural tube form the neural arches, which form the posterior bony elements of the spinal column. During the sixth week of gestation, signals from the notochord and neural tube lead to chondrification, which ultimately leads to ossification of the spinal column, at which point the notochord disintegrates, with its remnants forming the nucleus pulposus. Aberrations in this intersegmental formation of vertebral bodies are at the origin of vertebral segmentation anomalies, which will be discussed later in this chapter.
Dysraphism refers to a defect of neural tube closure. Therefore, all dysraphic disorders consist of abnormalities of primary neurulation. In the OSD group of malformations, neural tissue is directly exposed at the skin surface and leakage of cerebrospinal fluid (CSF) is observed.
OSDs include four types of malformations of different pathogenesis as follows:
Disorders of primary neurulation: myelomeningoceles and myeloceles
Disorders of gastrulation and primary neurulation: hemimyelomeningoceles and hemimyeloceles
The vast majority of cases of OSD are myelomeningoceles (98.8% of cases). OSD is always associated with the presence of a placode, which corresponds to a segment of cord at the neural plate stage that did not undergo closure and failed to detach from the surface ectoderm, hence it is adherent to the skin surface. There is a midline skin defect where the placode is directly visible. As the mesenchyme fails to migrate behind the neural tube, bones, cartilage, and muscles develop anterolateral to the neural tissue and typically appear everted.
A placode can be segmental—that is, at any level along the cord or terminal at the caudal end of the cord. It is most often terminal, with the myelomeningocele being lumbosacral ( Fig. 35-6 ). The ventral surface of the placode is covered by pia-arachnoid, and nerve roots originate from this surface, coursing through the subarachnoid space to reach their neural foramina. The occurrence of purely lumbar, thoracolumbar, and thoracic myelomeningoceles where the placode is segmental and the spinal cord distal to the placode normally neurulated cannot be explained by the traditional theory of primary neurulation, where closure of the neural tube is believed to proceed in a zipperlike pattern cranially and caudally in a continuous fashion. These cases of OSD can be explained by the concept of multisite closure of the neural tube suggested by Van Allen et al., which supports that the neural tube closes independently at five different sites.
A myelomeningocele can clinically be differentiated from a myelocele. In cases of myelocele, the flat neural placode is level with the skin surface, whereas in myelomeningocele, the neural placode is pushed above skin level by the more anterior expansion of the CSF space. Hemimyelocele and hemimyelomeningocele refer to the very rare cases where OSD affects one of the hemicords in a split cord malformation (SCM). They therefore represent a more complex anomaly involving the gastrulation stage (resulting in the SCM) and primary neurulation (causing the OSD). Opposite to myelomeningocele and myelocele—where the diagnosis is clinically obvious—a hemimyelocele and a hemimyelomeningocele are diagnosed by imaging, which demonstrates the split cord anomaly.
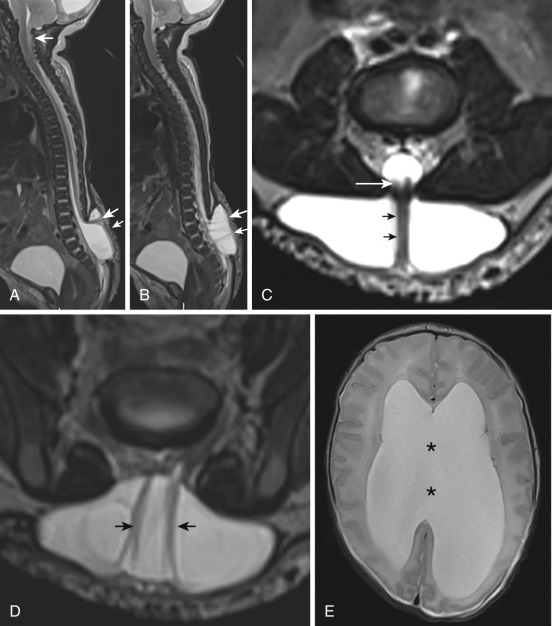
Almost all cases of OSD are associated with an Arnold-Chiari II malformation (see Fig. 35-6 ). It is believed that the chronic leakage of CSF at the neural placode during intrauterine life results in defective expansion of the developing rhombencephalic vesicle (developing fourth ventricle), which prevents normal development of the posterior fossa. The resultant Chiari II malformation has a spectrum of anomalies that include a small posterior fossa, hindbrain herniation with downward displacement of the cerebellar vermis, fourth ventricle, and medulla into the spinal canal, as well as several variably associated structural brain abnormalities. The posterior fossa malformation is often complicated by hydrocephalus.
Diagnosis of OSD and Chiari II malformation is usually confirmed prenatally by fetal ultrasound and if needed by magnetic resonance imaging (MRI). In utero repair of the myelomeningocele before 26 weeks' gestation is increasingly performed in an attempt to reduce the severity of the associated Chiari II malformation. Intrauterine repair reduces the need for shunting and improves mental development, motor outcome, and hindbrain herniation. This suggests a two-hit hypothesis where the final neurologic outcome depends on the failure of neural tube closure and spinal cord injury resulting from repetitive mechanical trauma and chemical trauma related to prolonged exposure of neural tissue to the amniotic fluid.
In the CSD group of malformations, the malformed neural tube is covered by skin (ectoderm) and subcutaneous fat (mesoderm). Midline lumbosacral skin lesions are frequently associated, including subcutaneous lipomas, skin tags, vascular nevi, dimples, and hair patches, which aid in orienting the clinician to the diagnosis.
From a pathogenetic standpoint, this group includes three categories of disorders as follows:
Disorders of primary neurulation: lipomyeloschisis (or lipomyelocele) and lipomyelomeningocele
Disorders of secondary neurulation and retrogressive differentiation: terminal myelocystocele
Disorders of unknown etiology: meningocele
These malformations most commonly occur in the lower lumbar region immediately above the gluteal cleft and present clinically as a midline subcutaneous mass extending asymmetrically into one buttock. This group includes two common conditions, lipomyeloschisis (or lipomyelocele) and lipomyelomeningocele, collectively referred to as lipomas with a dural defect; and two uncommon conditions, terminal myelocystocele and meningocele. Very rarely these malformations involve the cervical spine, where cervical myelocystoceles and cervical myelomeningoceles have been described ( Fig. 35-7 ).
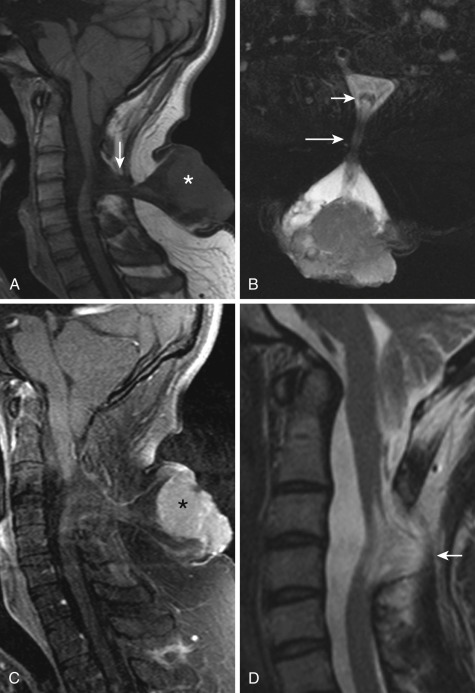
In both lipomyeloschisis and lipomyelomeningocele, a large subcutaneous lipoma extends into the spinal canal through a wide spina bifida and tethers the spinal cord. These lipomas do not represent lipomatous tumors but rather hamartomatous lesions that can grow along with changes in the fatty pool in the body (i.e., with weight gain or pregnancy). They are believed to be secondary to premature disjunction of the neural tube from the neuroectoderm before neural tube closure. This allows mesenchymal cells to gain access to the neural tube before its closure. The interaction of mesenchymal cells with the neural tube induces formation of a variable-sized lipoma. Depending on the size of the lipoma and the degree of expansion of the subarachnoid space, the interface lipoma-placode may be in the spinal canal (lipomyeloschisis) or outside the spinal canal within a meningocele when the subarachnoid space is expanded (lipomyelomeningocele). In lipomyeloschisis ( Fig. 35-8 ) the placode is terminal and the placode-lipoma interface may span multiple vertebral levels. The subarachnoid space ventral to the placode is not expanded. In lipomyelomeningocele the placode is usually segmental and the ventral subarachnoid space is expanded. The placode is most frequently rotated toward the lipoma on one side, so that the meninges herniate on the contralateral side. Spinal roots arising on the side of the meninges are longer and at risk of trauma, whereas those arising on the side of the lipoma are short and may cause tethering of the spinal cord.
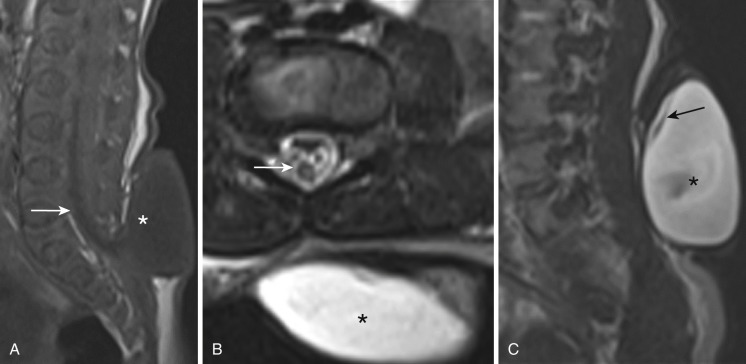
Terminal myelocystocele is an extremely rare form of CSD. It is, however, very important to recognize this malformation when present, because infants are usually neurologically normal at birth, and early surgical repair permits preservation of neurologic function. In this form of CSD, the subcutaneous mass represents an excessively dilated terminal ventricle lined by ependyma that herniates through a wide posterior spina bifida. The upper portion of the myelocystocele is a dilatation of the subarachnoid space, forming a meningocele lined by arachnoid and dura. The lower portion corresponds to the cystlike dilated terminal ventricle protruding beyond the confines of the thecal sac and covered by subcutaneous fat of variable thickness. This malformation is frequently associated with other abnormalities, mainly from the OEIS complex (omphalocele, cloacal exstrophy, imperforate anus, and spine defects). The pathogenesis is thought to be a deficient retrogressive differentiation, causing the terminal ventricle to be severely distended by CSF because its terminal end remains closed. It subsequently bulges posteriorly and ruptures the dorsal mesenchyme, preventing the posterior spinal elements from developing. There is a possible relationship of myelocystoceles to teratogens such as loperamide HCl and retinoic acid.
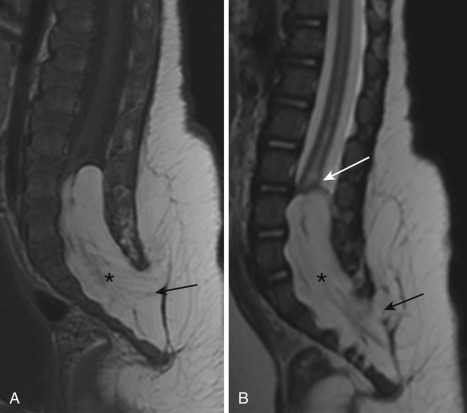
Posterior meningoceles ( Fig. 35-9 ) are rare and seen most commonly in the lumbar or sacral region. They represent herniation of a CSF-filled sac lined by arachnoid and dura through a posterior spina bifida. The spinal cord is normal and does not herniate in the meningocele sac, although it can be tethered to its neck.
Simple dysraphic states represent the most common group of spinal dysraphisms and present clinically with different degrees of spinal cord tethering due to excessive tension on the cord. From an embryologic standpoint, they include the following two groups of disorders:
Disorders of primary neurulation: intradural lipomas
Disorders of secondary neurulation and retrogressive differentiation: lipoma of the filum terminale, tight filum terminale, and persistent terminal ventricle
The conus medullaris position relative to the vertebral column ascends gradually during fetal life. It reaches its normal adult level by 40 postconceptional weeks, and no further ascent is observed thereafter. The conus medullaris should be positioned no lower than the inferior endplate of the L2 vertebra. Otherwise a tethering mass, bony spur, or thick filum terminale should be sought.
This represents absent fusion of the posterior vertebral neural arches, usually at L5 and/or S1, and is seen in 4% of the population. It is usually an incidental finding unless there are clinical symptoms or signs of spinal cord tethering, when it can point to the presence of another CSD. It should be noted that the L5 laminae may normally remain unfused until age 5 to 6 years.
A persistent terminal ventricle represents persistence of the normal terminal ventricle, a small cystic expansion of the central ependymal canal at the level of the conus that fails to undergo normal regression during secondary neurulation. They are usually asymptomatic and seen as a nonenhancing ovoid small cystic expansion of the central ependymal canal in a normally positioned conus. Symptomatic cases are associated with obstruction of the ventriculus terminalis, which loses its connection to the central ependymal canal. The obstructed ventriculus terminalis becomes expanded and results in thinning of the surrounding cord parenchyma.
Filar cysts are simple cysts of the filum terminale, commonly seen on spinal sonography of infants. When isolated, they are generally asymptomatic and regress spontaneously at follow-up.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here