Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The cranio-orbital region is a complex anatomical area that accommodates structures of great functional importance such as the brain, the internal carotid artery and the cavernous sinus, the optic nerves, and chiasm or the globe. This region can be affected by a variety of tumors that can originate primarily or spread through the anatomical pathways from neighboring structures. Treatment of tumors of the cranio-orbital region is a challenge for the surgeon. In fact, it remains the most complex and controversial aspect of head and neck surgery in terms of disease control and reconstruction. Access and visualization in this area are usually limited and a complete exposure of the surgical site is often difficult to achieve. Endoscopic approaches to the skull base have been introduced with success although open approaches are still necessary in many situations. , For these reasons, oncologic surgery of the cranio-orbital region and skull base must be carefully evaluated and planned, and the reconstructive approach must be thoroughly designed. An optimal reconstruction of the resulting defect is essential to avoid severe complications, such as cerebrospinal fluid (CSF) leak and meningitis. Prior to the advent of computer-assisted design and computer-assisted manufacturing (CAD/CAM) surgery planning, outcomes after traditional surgical planning depended mostly on the surgeon’s experience and were less predictable. Computer-assisted surgery constitutes a major breakthrough, being especially useful in the treatment of tumors affecting the craniofacial region. Computer-assisted surgical planning (CaSP), design of the reconstruction and manufacturing of patient-specific implants (PSI) and cutting guides (CAD/CAM procedures) as well as surgical navigation, provide the possibility of an accurate three-dimensional (3D) preoperative planning of the oncological resection as well as performing complex reconstructions with highly predictable postoperative results. Navigation systems integrate the imaging with the surgical field, allowing the surgeon to visualize the actual position of a surgical pointer in real time on the monitor displaying the computed tomography (CT) and/or magnetic resonance imaging (MRI) data of the patient. It offers a more accurate approach to essential anatomical structures such as the optic nerve, the internal carotid artery, and the cavernous sinus, thus increasing safety of the procedure, which is a critical concept in cranio-orbital surgery. It is necessary to remark that although accurate 3D planning and computer-assisted surgery improve predictability and precision of the procedure, the technical complexity and additional cost could be a major drawback for many institutions.
Management of cranio-orbital tumors requires a thorough knowledge of craniofacial anatomy. Careful presurgical planning including clinical examination, imaging techniques with CT scan and MRI, as well as angiography, if indicated, is mandatory. Radiological evaluation of the craniofacial skeleton should be performed with a submillimeter data set and reconstructed in the axial, coronal, and sagittal planes. ,
The location, invasion, and tumor extension are determining factors in the selection of the surgical approach and resectability of the tumor itself and should be taken into account in preoperative planning. With the current software and tools, the margins of resection can be designed, and vital structures outlined preoperatively with great accuracy, in order to be intraoperatively navigated during tumor ablation, improving the precision of the resection, while minimizing damage to healthy tissue. Surgical planning allows for such resection to be performed with greater confidence when visual cues are absent. In addition, navigation helps reduce the risk of damaging surrounding vital structures. The coupling of real-time 3D-navigation and CaSP further enhances these advantages to provide real-time feedback. ,
Furthermore, the incorporation of other imaging modalities, such as 3D-CT angiography, and MRI, into navigation surgery facilitates the comprehension of vital structures within the surgical field such as the internal carotid artery or the optic nerve. Important landmarks, such as the foramen ovale and foramen rotundum, can be outlined before surgery as well, to help anatomical orientation during the procedure.
As navigation at the skull base is not influenced by shifting of the brain or soft tissue, precision is greater than in other neurosurgical procedures. Once the system is calibrated, surgical navigation allows the enhancement of both surgical precision and accuracy owing to real-time confirmation of position, without the need to obtain additional intraoperative images that expose patients to additional radiation. The use of a navigation system also reduces the duration of surgery at radical resections, although it increases the preoperative preparation time.
Regarding reconstruction, immediate repair of defects in the cranio-orbital region is needed to achieve an adequate aesthetic and functional result. Resections in the orbital region involving a lack of eye globe support need reconstruction of the orbital walls to ensure symmetry and function; in cases of orbital exenteration, filling of the defect is mandatory, in order to isolate the sinonasal cavity. Resections affecting the skull base also need isolation of the intracranial contents from the aerodigestive tract.
Depending on the size and location of the defect, local or regional flaps, such as galeal-pericranial or temporalis muscle flap, can be used. In cases of massive resections, microvascular flaps are usually preferred (either osteocutaneous or musculocutaneous free flaps). In maxillary resections, fibular, scapular, and iliac crest flaps are the most suitable options. In orbital exenterations, a temporalis flap can be chosen, or a bulkier flap such as an ALT or rectus abdominis flap. In cases of complex orbito-zygomatic craniectomies, PSIs provide better (and simpler, surgery-wise) aesthetic results. Computer-assisted surgery is a helpful tool in both the planning and designing of the reconstruction, and the intraoperative checking of the positioning of the flap according to the planning. Currently, high-resolution CT scan and magnetic resonance multiplanar imaging can be merged to visualize and virtually manipulate the tumor, which can be segmented and a preferred surgical margin outlined. A mirror image of the healthy side can be added, for example in cases of orbital exenterations or tumors requiring an orbitozygomatic craniectomy, to plan for a symmetrical reconstruction. A PSI can then be designed: titanium meshes for orbital wall reconstruction can be “drawn” as desired, or an STL (Standard Triangle Language) file can be imported, to fit a true-to-original reconstruction, or patient-specific titanium plates for the fibula segments. Even the cutting guides with drilling holes and screws with different lengths depending on the depth of the bone can be anticipated, providing the optimal angles for fibula flap osteotomies to easily match the desired 3D shape to achieve symmetry in the zygomatic area. Alternatively, a 3D-printing and rapid-prototyping technique can be used to prebend a standard titanium mesh on a stereolithographic model of the patient with the mirrored healthy orbit. This mesh is afterwards sterilized and ready to use, easily fitting into the orbital wall, thus minimizing intraoperative time. In the cranio-orbital region a similar procedure to produce a specific implant made of polyetheretherketone (PEEK) is very useful because of the intricate topography and characteristics of the region. Shape adaptability and biocompatibility make this material a great option to bear in mind when planning reconstruction of the orbital-maxillary-zygomatic and pterional/sphenoid wing area. , In reconstruction of the defect with microvascular bony flaps, CAS has been reported to significantly reduce time of flap ischemia as well as operative time, when compared with non-guided surgery. , ,
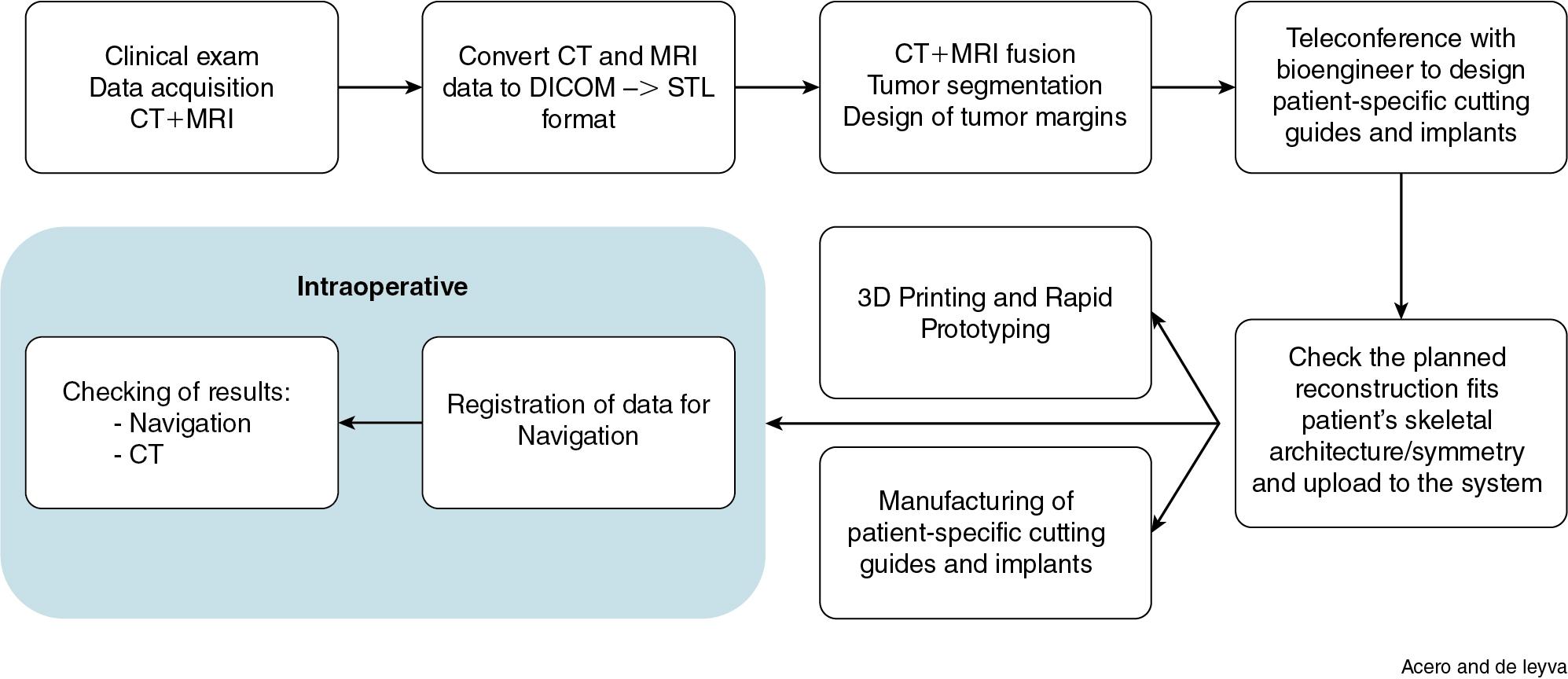
The workflow for CAD/CAM based cranio-facial oncologic resection is shown in Fig. 21.1 .
Accurate planning of the resection and reconstruction is essential in order to obtain an adequate result in the surgical treatment of craniofacial tumors. Conventional surgical procedures are based mainly in the surgeon’s experience and are often associated with imprecise oncologic and reconstructive results as well as certain intraoperative risks. A 3D preoperative plan provides accurate information on tumor location and relationship to critical anatomical structures such as the optic nerve, cavernous sinus, and so on as mentioned before in this chapter. Holographic models with mixed reality technology are being introduced in the computer-assisted planning workflow and will contribute to a better understanding of each case. Moreover, the design of safer resection margins at the workstation is possible with this technology as well as computer-assisted preoperative planning of the reconstruction in the craniofacial region with PSIs or bone flaps to repair the defect.
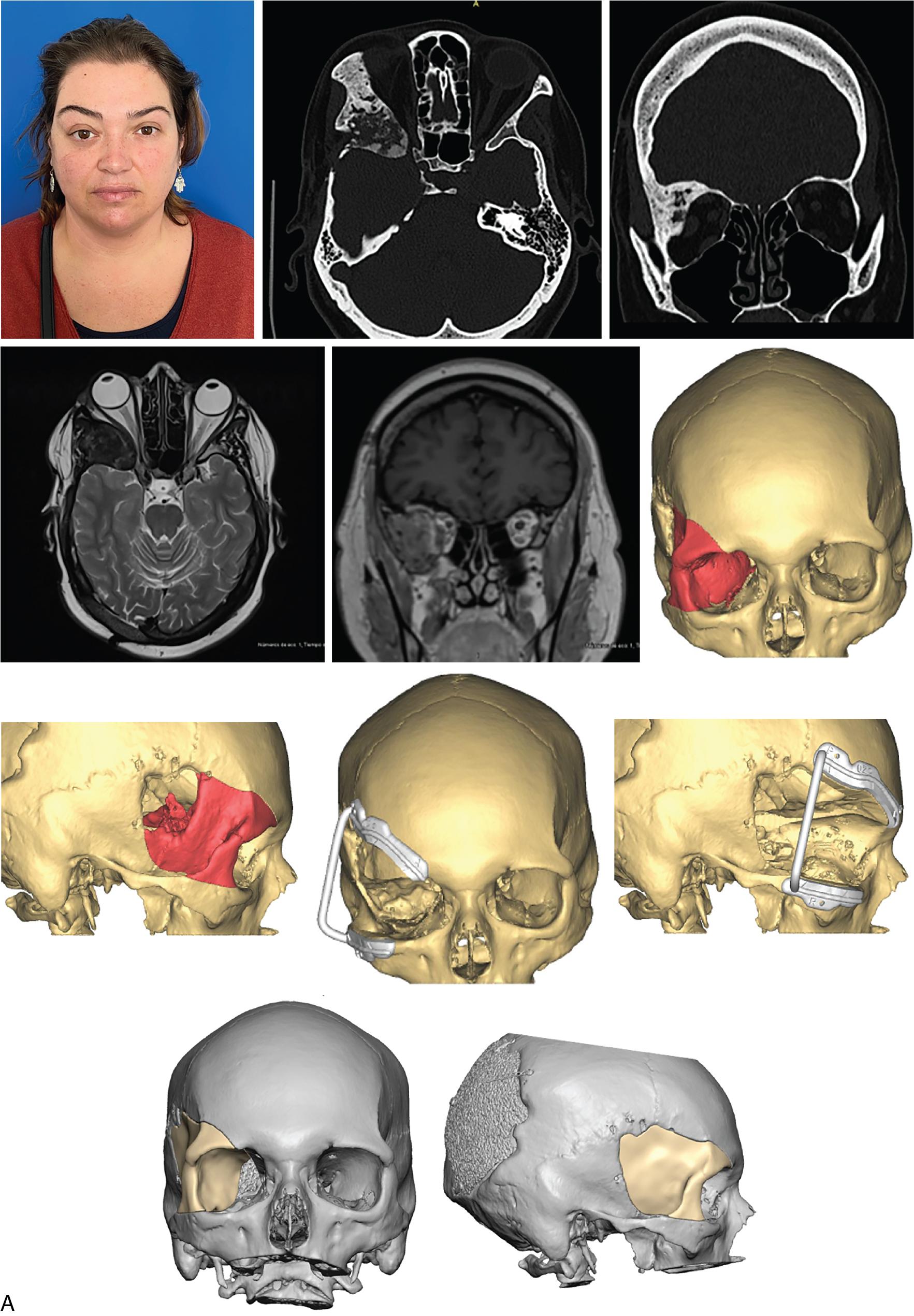
The following CAD planning sequence is based on a case of relapsing fibrous dysplasia with massive orbital involvement ( Fig. 21.2 A) ( ![]() ,
, ![]() ).
).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here