Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Complications of neck surgery have evolved over time with the introduction of new procedures and philosophies in the management of patients with head and neck cancer.
Neck complications can be categorized into four groups: wound, vascular, nerve, and chyle/chest.
Knowledge of the pathophysiology of the various complications provides a framework to best avoid their development.
Awareness, early recognition, and prompt and effective management of surgical complications can have a significant impact on outcomes.
Complications of neck surgery affect every surgeon regardless of experience and technical skill. Despite our best intentions, complications arise as a result of the intricate anatomy of the neck and complexities of the diseases and patients treated. Factors such as medical comorbidities (hypertension, diabetes, and hepatitis), age, substance abuse, prior radiation therapy (RT), aerodigestive tract entry, prolonged anesthesia times, the volume of intraoperative fluid administered, and the need for microvascular free flap reconstruction have been associated with head and neck surgical complications in various studies. Prevention and management of complications that occur both intraoperatively and postoperatively are essential to proper head and neck surgical care.
The history of neck dissection reveals a continuing quest to reduce complications and their sequelae. A systematic approach to cervical lymphadenectomy for the treatment of head and neck cancer was first described by Crile in 1906. In that era, radical neck dissection (RND) with removal of the sternocleidomastoid (SCM) muscle, internal jugular vein, and spinal accessory nerve was considered the standard of care for patients with neck metastasis but resulted in significant functional and cosmetic morbidities. Introduction of the modified radical neck dissection (MRND) and proof that it was oncologically sound led to improved functional outcomes without sacrifice of oncologic effectiveness. Further technical refinements that established selective neck dissection (SND) were based on predictable patterns of spread from specific primary tumor locations. This approach is highly effective for management of the clinically negative neck and may have applications in clinically positive necks as long as postoperative RT is administered. In addition, SND may be the preferred approach for planned neck dissection after concurrent chemoradiation (CRT) for advanced head and neck cancer because these patients have a low incidence of recurrence in the neck. As head and neck surgical techniques have evolved, so have the type and frequency of complications. Shoulder disability from spinal accessory nerve injury was an expected sequela of RND but is now only considered a potential complication of MRND. Internal jugular vein thrombosis and hemorrhage may occur more frequently in the modern era because this structure is more commonly preserved with MRND and SND.
In this chapter, complications of neck dissection are considered primarily and are grouped into four major categories: (1) wound, (2) vascular, (3) nerve, and (4) chyle/chest. This framework provides a structure for the informed consent process, and additional individual components can be applied selectively to any neck surgery, depending on the location and extent of a given procedure.
Carefully designed neck incisions must take into account the location and extent of the primary tumor, adequate exposure for the type of neck dissection planned, carotid artery coverage, excision of previously violated skin when applicable, and cosmesis. Preferred incisions combine limbs that meet at right angles to create skin flaps that preserve the blood supply to neck skin, which includes branches of the facial and occipital arteries superiorly and branches of the transverse cervical and suprascapular arteries inferiorly. Subplatysmal flap elevation should be used in all approaches, when possible, to preserve the blood supply to the skin.
Numerous neck incisions for neck dissection have been described. Early designs, such as the Crile single-Y and the Martin double-Y, provided excellent exposure but placed a trifurcation over the carotid artery. Furthermore, they created tenuous posterior skin flaps and anterior skin flaps that relied partially on blood flow from branches of the contralateral external carotid artery. The Conley-modified Schobinger approach was an improvement that maintained excellent exposure for comprehensive neck dissection with creation of a large, robust anterior flap and placement of the trifurcation posterior to the carotid artery. MacFee introduced the use of two transverse incisions that appear to transect the dominant blood supply, but studies have shown that the central, bipedicled skin flap is resistant to ischemia and may be the preferred approach in the previously irradiated patient. Certain incisions are well-suited to accompany the extirpation of specific primary tumors, such as the apron flap for neck dissection with laryngectomy and the Attie incision for neck dissection with thyroidectomy. For elective neck dissection, esthetics and patient satisfaction can be improved using a transverse cervical incision without significantly affecting the number of lymph nodes removed during surgery.
The principles of adequate exposure and protection of critical structures cannot be overemphasized and are as equally important for comprehensive neck dissection as they are for less extensive procedures. For example, care should always be taken to place submandibular incisions—whether for supraomohyoid neck dissection, submandibular gland resection, or mandibular fracture repair—sufficiently below the lower border of the body of the mandible to avoid injury to the marginal mandibular branch of the facial nerve. Cosmesis must often be considered secondary to successful tumor extirpation and safety. For example, although a small incision for lymph node biopsy of a posterior triangle node is desired, a slightly longer incision with a wider operative bed may improve surgical exposure and facilitate preservation of the spinal accessory nerve. When an excisional lymph node biopsy is made, it should be planned in such a way that it can be extended for a neck dissection if necessary without making a separate incision.
Skin flap survival depends on incision design, surgical technique, and factors intrinsic to the patient. A study of 184 neck dissections using triradiate, modified MacFee, or apron incisions showed a wound dehiscence rate of 11%, 8%, and 0%, respectively, for each approach. The same study showed a statistically significant increase in the overall rate of wound dehiscence in previously irradiated necks, particularly for the triradiate group, which led the authors to recommend the apron flap for neck dissection in patients who have received prior RT. Whether or not preoperative RT increases the complication rate of neck dissection continues to be debated, but several reports indicate that higher total radiation doses are associated with a higher rate of wound complications. Skin loss from involvement with tumor or excision of violated skin may lead to increased tension on the closure. Poor microvasculature secondary to malnutrition, active tobacco use, or uncontrolled diabetes mellitus contributes to the lack of tissue tolerance for surgical manipulation and a higher rate of wound dehiscence or flap necrosis.
Division of lymphatic and adipose tissue during neck dissection allows for formation of seroma, the collection of serous fluid in the potential space between cervical skin flaps and underlying structures. Seromas manifest as enlarging masses under the skin, with or without overlying induration or erythema; loss of the expected postoperative scaphoid appearance of the neck following neck dissection is cause for suspicion ( Fig. 119.1 ). If left untreated, a seroma may lead to skin flap necrosis or infection. Many case series report seroma and hematoma formation together, with rates that range from 3% to 10% with RND to as high as 20% with functional neck dissection. These differences may be explained by the increased amount of native tissue preserved in MRND or SND, compared with RND, that can weep serous fluid into the wound bed. Causes of seroma include incorrect drain placement, drain failure, or premature drain removal. Prevention consists primarily of proper management of closed-suction drains that are left in place until the total output per drain falls below 25 mL in a 24-hour period. Some authors also advocate the routine use of fibrin glue, which has been shown in animal models to prevent seroma formation. Some small seromas can be observed with anticipation of gradual resorption. In most cases, however, management of seroma includes needle aspiration and, in select patients, drain replacement. Pressure dressings do not appear to prevent fluid reaccumulation.

Wound infection may manifest as cellulitis with erythema, warmth, and/or induration of the cervical skin flaps; abscess formation from an infected seroma or hematoma; or fistula. Occasionally, purulent fluid will be seen in a closed-suction drain. Early recognition and proper drainage or diversion of fluid away from the carotid artery and internal jugular vein are critical to prevent both spread of the infection, and potential thrombosis or vascular rupture.
Aerodigestive tract entry is the single most important factor that contributes to the risk of wound infection. Neck dissection without exposure to saliva and oral flora is considered a clean procedure. In a study of 438 patients who underwent parotidectomy, thyroidectomy, or submandibular gland excision, three patients (0.7%) developed a wound infection, one of whom had received perioperative erythromycin. Administration of prophylactic antibiotics for clean neck dissections is reasonable, based on a study of 192 patients in whom 10 of 99 patients (10%) not receiving antibiotics developed a wound infection compared with 3 of 93 patients (3.2%) receiving first-generation cephalosporins, clindamycin, or penicillin, even though this trend did not reach statistical significance. A more recent study confirms the benefit of 24 hours of prophylactic antibiotics after clean neck dissection. Antibiotic prophylaxis in this setting was shown to be cost effective. In terms of duration, no difference in the rate of infection was seen with 1-day versus 4- or 5-day antibiotic regimens for clean procedures. Interestingly, compared with other clean surgical procedures, RND has significantly higher infection rates for reasons that remain unclear.
The risk of wound infection increases significantly with mucosal entry into the oral cavity, pharynx, or larynx, and it ranges from 15% to 87%. Factors associated with wound infection include the performance of bilateral neck dissections and total laryngectomy, advanced stage tumors, and in some studies, a history of prior tracheotomy and malnutrition. Diabetes was not found to be associated with a greater incidence of postoperative infection. A recent evidence-based review of antibiotic prophylaxis in clean-contaminated neck dissections looked at five randomized controlled trials that established clear guidelines for antibiotic use. Antibiotic prophylaxis was shown to reduce the incidence of postoperative infection in these cases if administered before the start of surgery; no evidence supports antibiotic administration beyond 24 hours after surgery. Multiple-drug regimens are acceptable, with first-generation cephalosporins being the most common.
Once a wound infection is detected, action must be taken to minimize the sequelae. Collections must be completely aspirated or incised and drained, wounds should be cultured, and antibiotics need to be initiated that target the potential or confirmed pathogens. Ensuring that the infection does not spread to the major blood vessels and mediastinum is of utmost importance.
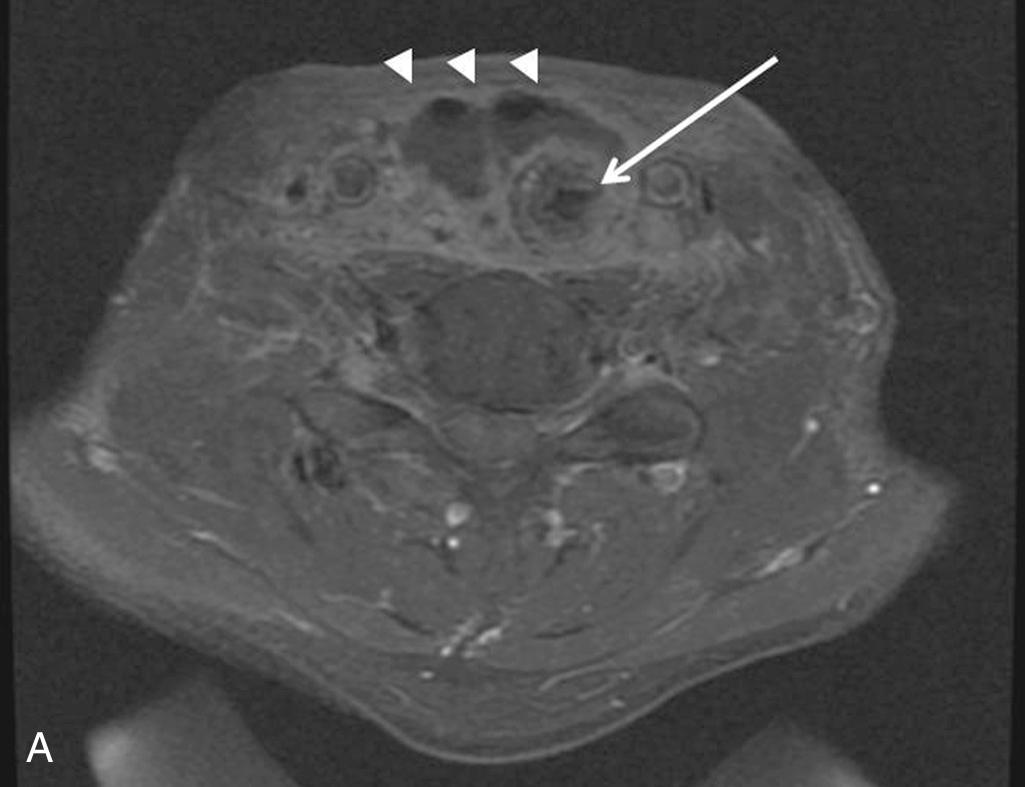
Saliva may enter the wound from either aerodigestive tract communication or parotid leak ( Fig. 119.2 ). With associated infection, an inflammatory response in adjacent tissue occurs rapidly. Common signs are erythema, edema, and induration of skin flaps as well as a change in the character of drain output to that of saliva or purulent discharge.
The risk of pharyngocutaneous fistula formation with aerodigestive tract entry during surgery varies from 10% to 30%. Prevention consists of watertight, inverted, and tension-free closure during the primary surgical procedure and consideration of vascularized tissue coverage if the closure appears tenuous. The recent resurgence of transoral surgery for oropharyngeal carcinoma (transoral laser microsurgery, transoral robotic surgery) with concomitant neck dissection has led to concerns about a greater likelihood of pharyngeal communication with the neck and potential development of pharyngocutaneous fistula. In a group of 148 patients, 29% were found to have an orocervical communication at the time of surgery. These tracts were closed with primary closure, local flap advancement, or fibrin glue, including placement of a cervical drain. Only 4% went on to develop a clinical fistula. More recent study of 113 patients showed a much lower 5% occurrence of intraoperative communication between the pharynx and the neck during concurrent neck dissection. After pharyngeal mucosal flap advancement, the defects were closed with primary closure or local muscle flap, and reinforced with submandibular gland transposition or acellular dermal matrix. Cervical drains were used for all cases and none of the patients developed postoperative fistula. Other studies have supported meticulous reconstruction of the pharyngeal wall in order to prevent postoperative fistulae.
Given the potential risk, studies have looked at timing of neck dissection in the setting of transoral surgery. Safety and efficacy were comparable between concurrent and delayed neck dissections with similar fistula rates and bleeding complications, but length of stay was overall shorter for concurrent procedures. Systematic review of literature also showed that the timing and specifically delaying the neck dissection was not found to have any effect on the overall survival of patients. Timing of the neck dissection continues to be based on operator preference and patient factors that determine surgical logistics.
In contrast to transoral surgery, fistula rates may be as high as 50% following salvage total laryngectomies. Multiple factors—including previous RT and CRT, malnutrition, recurrent cancer, and neck dissections—likely predispose to the high rate of fistulae, which tend to be more severe than in primary laryngectomy patients. A growing body of evidence suggests that placement of vascularized tissue to reinforce the pharyngeal closure helps decrease the frequency and severity of pharyngocutaneous fistulae in this challenging patient population, and many centers are prophylactically placing local, regional, or free flaps to avoid this complication.
When a fistula does develop, conservative management with broad-spectrum antibiotics and continued closed drainage is usually successful, although the clinician should have a low threshold for opening a suture line to divert drainage away from the major blood vessels and gently packing the wound. Nutritional status and glucose control should be optimized, and thyroid-stimulating hormone levels should be checked, particularly in previously irradiated patients. Fistulae refractory to conservative measures require closure with vascularized tissue, either locoregional flaps or free flaps.
Postparotidectomy fistula does not carry a risk of major blood vessel rupture, but it can be annoying to patients. Most are small-volume leaks that exit the divided inferior cervical portion of the parotid gland. These normally respond well to conservative management. Although numerous treatment modalities for persistent leaks have been proposed, parotid gland botulinum toxin injection is usually effective.
Cosmetic principles that apply to neck surgery include placement of incisions in natural skin creases or relaxed skin tension lines; using gently curved vertical limbs to avoid linear scar contracture; and performance of a tension-free, everted skin closure. Lapses in meticulous technique or postoperative wound infection may lead to the development of a hypertrophic scar ( Fig. 119.3A ). There are various approaches to wound closure but the concept of multilayer closure from deep to superficial with appropriate alignment of the dermis and skin is more critical than the material or technique used to close the skin. Formation of a keloid , scar tissue that exceeds the boundaries of the original incision, usually occurs in patients with a personal or family history of exuberant scar formation. Web formation along linear vertical limbs in the lateral neck may also occur (see Fig. 119.3B ). Unilateral deep-plane neck lift and midline platysmaplasty can be considered for rehabilitation of post–neck dissection asymmetry.

Disruption of the cervical lymphatics may result in stagnation and buildup of lymphatic fluid. This is not uncommon after neck dissection, especially if the patient is treated preoperatively or postoperatively with radiation, which further restricts lymphatic drainage. This may manifest externally in 17% to 36% of surgical patients as pitting edema in the area of neck dissection, and it may extend up onto the face above dissected tissue planes. The clinician must be cognizant that lymphedema may also develop internally within the mucosa, submucosa, and muscles of the upper aerodigestive tract. This may manifest as neck stiffness, limitations in range of motion, pain, dysphagia, and, rarely, airway compromise. Furthermore, external and internal lymphedema severity is associated with hearing impairment and decreased quality of life (QOL). Referrals to certified lymphedema therapists, speech-language pathologists, and physical therapists should be made when appropriate.
Lymphedema subsides in most cases with time and therapy but sometimes it does persist and can functionally and cosmetically affect patients after therapy is completed. With continued advances in microvascular surgery, surgical intervention with lymphovenous anastomosis or lymph node transfer is now possible and is commonly used for severe limb lymphedema. When severe head and neck lymphedema persists and affects patient function surgical intervention may be warranted and possible. Lymphovenous anastomosis can improve lymph circulation and has been successfully performed in the head and neck. Future refinements to this surgical procedure may be beneficial for patients with severe facial lymphedema.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here