Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Developmental dysplasia of the hip (DDH) is a common pediatric condition that encompasses a spectrum of hip pathology ranging from increased hip laxity to hip dislocation. If diagnosed early, most of these infants can be successfully managed with brace treatment. However, if brace treatment is unsuccessful or the child is not diagnosed by the time that they are ambulatory, children will often require open surgical treatment to reduce the hip and promote further development of the hip joint. This chapter will focus on the many obstacles and complications that may arise in the open treatment of DDH.
The first step in avoiding complications when treating DDH is to not miss the diagnosis. Although newborns are screened for DDH if they have positive risk factors or the presence of instability on examination, older children with DDH often have fewer risk factors and present with complaints that do not directly implicate hip pathology. This is complicated by the fact that a hip dislocation does not usually become painful until adolescence or young adulthood. For example, a patient with a unilateral hip dislocation may present with a history of a painless limp, leg length discrepancy, or toe walking. Similarly, a patient with a bilateral hip dislocation may present with an abnormal waddling gait and hyperlordosis. If a patient has already been diagnosed with hip dysplasia prior to presentation, it is pertinent to determine how and when they were diagnosed and what treatment was initiated. A complete patient and family history is important to obtain, as many conditions are associated with hip dysplasia.
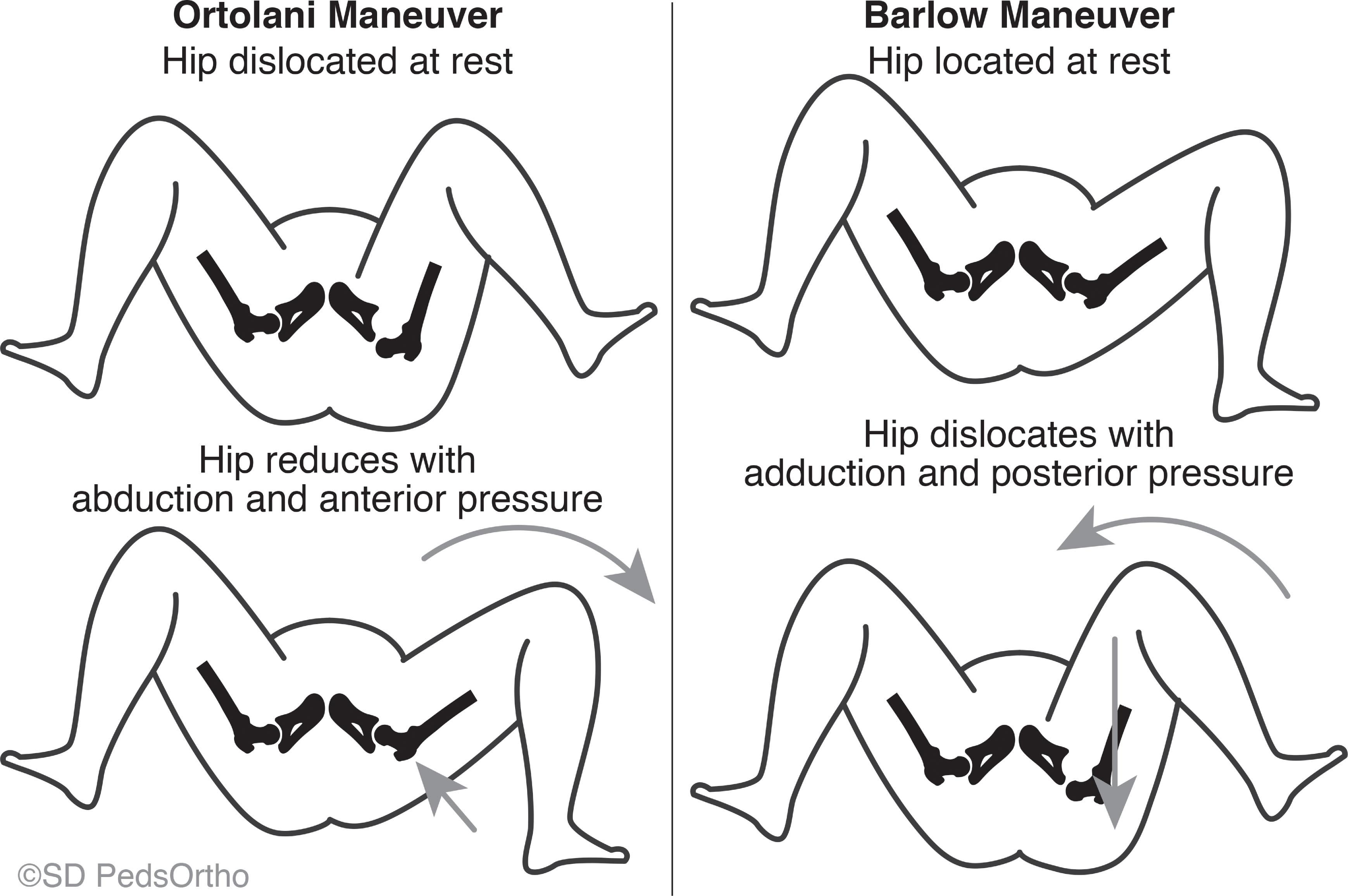
The Ortolani and Barlow maneuvers are used to test hip stability in infants ( Fig. 27.1 ). It is important to make sure the infant is warm, well-fed, and in a quiet environment to optimize the sensitivity of the exams. With the Ortolani maneuver a dislocated hip is reduced by gently abducting and translating the hip anteriorly. With the Barlow maneuver a reduced hip is gently dislocated with adduction and posterior pressure on the thigh. The examiner should be able to feel the femoral head gliding over the cartilaginous acetabular anlage. The femur must be held delicately with the examiner’s thumb on the inner thigh and long finger on the greater trochanter. Trainees should feel as many positive Ortolani and Barlow maneuvers as possible to gain comfort with the examinations. Even experienced examiners should verify their physical findings with an expertly performed hip ultrasound.
The physical findings in a child older than age 12 months are different from those in the newborn. Soft tissue contractures may have developed, making the Ortolani and Barlow maneuvers unreliable, with limited hip abduction being the most common physical exam finding. In unilateral cases, hip abduction will be decreased compared to the contralateral side. These patients will also have a positive Galeazzi sign, with the thigh on the side of the dislocated hip being shorter when examined with the hips and knees in a flexed position ( Fig. 27.2 ). Bilateral cases are more difficult to detect on physical exam, as abduction will be symmetric (although limited), and the Galeazzi sign will not be present. Physical examination should include complete musculoskeletal and neurologic examinations to identify any underlying etiology for the hip dislocation.

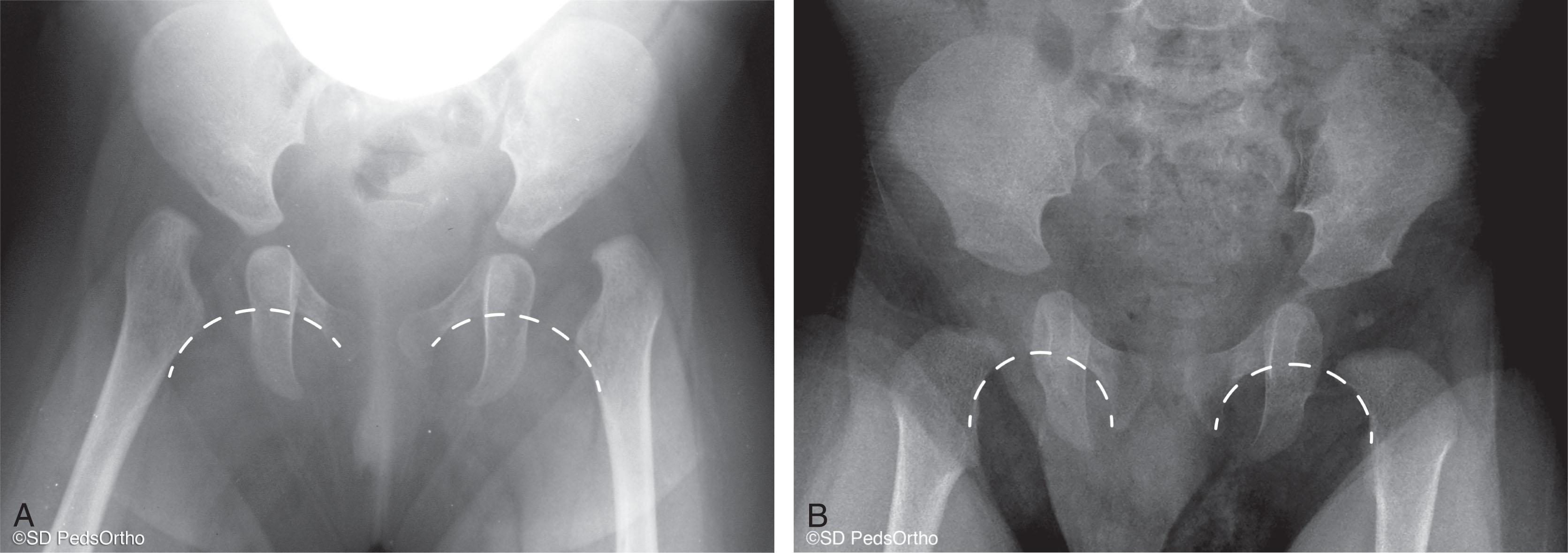
After 6 months of age, plain radiographs are the primary imaging modality once the femoral head has begun to ossify. Standard anteroposterior and frog lateral views of the pelvis are typically adequate to classify the severity of the dislocation. Delayed ossification of the femoral head is common in children with a dislocated hip, so the proximal femoral metaphysis can be used as a reference point in its place. Other radiographic parameters used are Shenton’s line and the acetabular teardrop. Shenton’s line describes the arc formed by the proximal femoral metaphysis and the superior border of the obturator foramen. The acetabular tear drop is composed of a medial line that represents the quadrilateral surface and a lateral line that represents the inner wall of the acetabular fossa ( Fig. 27.3 ). In the presence of a hip dislocation, Shenton’s line is broken, and the teardrop becomes shaped like a “V” instead of a “U.” These parameters are important because they can also be followed after open reduction of the hip to ensure that the hip is continuing to develop properly. Smith et al. evaluated 47 dislocated hips and found that radiographic appearance of the acetabular teardrop within 6 months of reduction was associated with a stable, concentric reduction, whereas delayed appearance was associated with persistent instability and need for secondary procedures.
Late-neglected dislocations in older children create a challenging situation due to the limited remodeling potential of the maturing hip. While this potential is somewhat limited beyond the age of 4 years, there is enough growth remaining to warrant surgical intervention for the dislocated hip based on the skeletal maturity of the patient. In general, open reduction is recommended up to age 8 years for bilateral dislocations and up to age 10 years for unilateral dislocations. After this time, some studies have demonstrated superior outcomes in hips left dislocated compared to ones that are managed surgically. In these cases, the risks and benefits of surgery should be considered, and the surgeon must set realistic expectations for what open treatment will be able to accomplish.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here