Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The persistent sciatic artery (PSA), first described by Green in 1832, is a rare congenital anomaly resulting from the failure of regression of the sciatic artery during the embryonal period. Diagnosis can be difficult, and life-and limb-threatening complications are well recognized. Descriptions and management of PSAs have been limited to several isolated case reports in the literature. The reported incidence of this condition has been estimated to occur in only 0.025% to 0.05% of the general population.
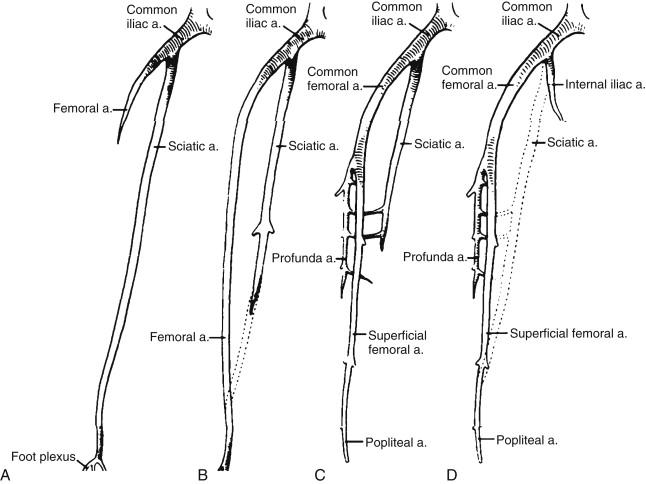
During embryonal development, the sciatic artery is the main blood supply to the lower extremity until the 6th week of gestation. Beyond this period, the artery begins to regress, and its remnants contribute to the formation of the inferior gluteal, deep femoral, popliteal, peroneal, and pedal arteries. The sciatic artery can fail to involute in either complete or incomplete forms.
A complete sciatic artery, occurring in 63% to 79% of cases, provides the main blood flow to the lower extremity. It originates off the internal iliac artery, courses through the greater sciatic foramen, runs along the adductor magnus muscle, and joins the popliteal artery distally lateral to the insertion of the adductor magnus. The superficial femoral artery is often hypoplastic and terminates in the thigh.
The incomplete PSA is hypoplastic and ends in the thigh, and the superficial femoral artery provides the main blood supply to the popliteal artery ( Figure 1 ). Bilateral PSAs occur in about 20% of cases. Associated venous anomalies are present and can include a persistent sciatic vein or large communicating veins between the deep femoral vein and the popliteal vein.
PSAs are asymptomatic in up to 40% of patients. However, they are prone to early atherosclerosis and aneurysm formation. This is thought to be partially caused by congenital hypoplasia of the wall as well as repetitive traumatic forces to the artery during sitting and hip flexion and extension. The presence of a mass in the buttock, claudication, acute ischemia, gangrene, and sciatica are all reported symptoms that can develop.
Aneurysms are the most common cause of symptoms in patients with a PSA, and patients with aneurysms have a high associated rate of complications and limb loss. The estimated incidence of PSA aneurysm formation is between 15% and 44%. They form posteriorly at the level of the greater trochanter and are often palpable. Distal embolization, thrombosis, and rupture into the gluteal region are possible complications. With larger aneurysms, compression of the adjacent sciatic nerve can lead to sciatica, foot drop, or progressive loss of function of the extremity. Progressive atherosclerosis can also occur in a sciatic artery as in any lower extremity artery. The resulting arterial insufficiency can range from claudication to tissue loss and gangrene.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here