Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
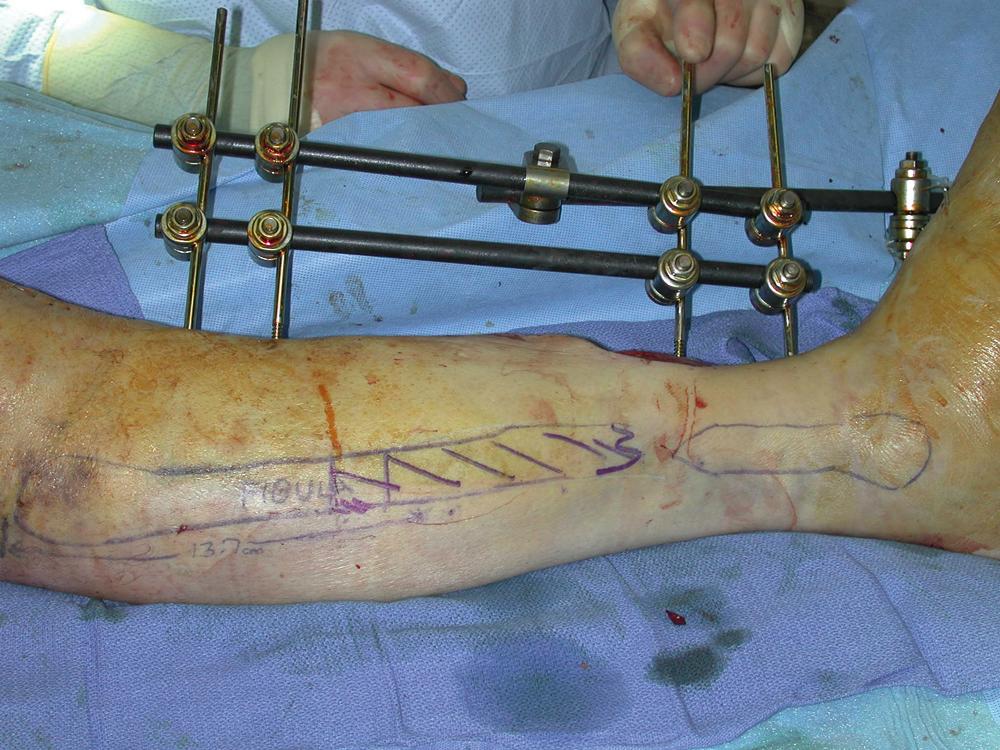
A 21-year-old White male had an extensive middle tibia wound of his right leg associated with an open fracture as a result of a motor vehicle accident. He had a 13 × 6 cm middle tibia wound of the right leg with exposed tibial fracture site. A rigid fixation of the tibia fracture was performed with an intramedullary rod by the orthopedic trauma service after the initial wound debridement ( Fig. 47.1 ). The plastic surgery service was consulted for soft tissue reconstruction of this large middle tibia wound within 1 week after the definitive bony reconstruction performed by the primary service.

For this large middle tibia wound with exposed fracture site and hardware, a single adjacent local muscle flap, such as a medial gastrocnemius or medial hemisoleus muscle flap, is not large enough to provide adequate soft tissue coverage for the exposed fracture site and hardware. However, because both local muscle flaps are commonly used for lower extremity soft tissue reconstruction, the combination of both local muscle flaps has been used by the author as an alternative approach to a free tissue transfer for a large middle tibia wound. The medial gastrocnemius muscle could be used to cover a relatively proximal middle tibia wound and the medial hemisoleus muscle could be used to cover a relatively distal middle tibia wound. The combined medial gastrocnemius and medial hemisoleus muscles flaps can be a valid and less extensive reconstructive option for a large middle tibia wound and can be performed in 2 to 3 hours by most surgeons without microsurgical expertise.
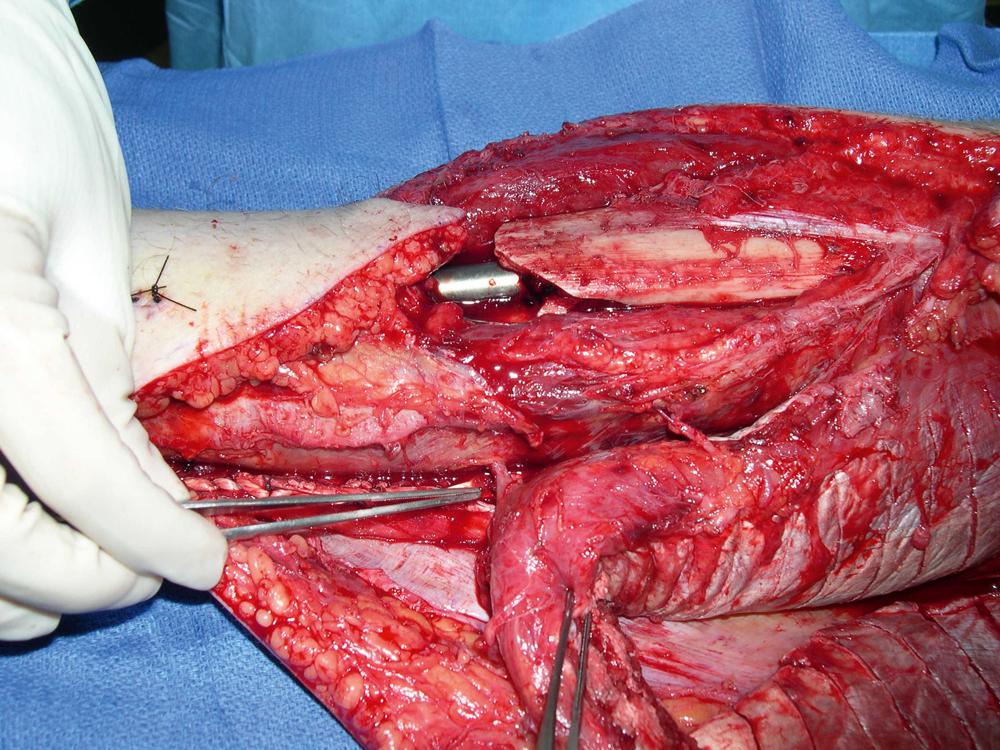
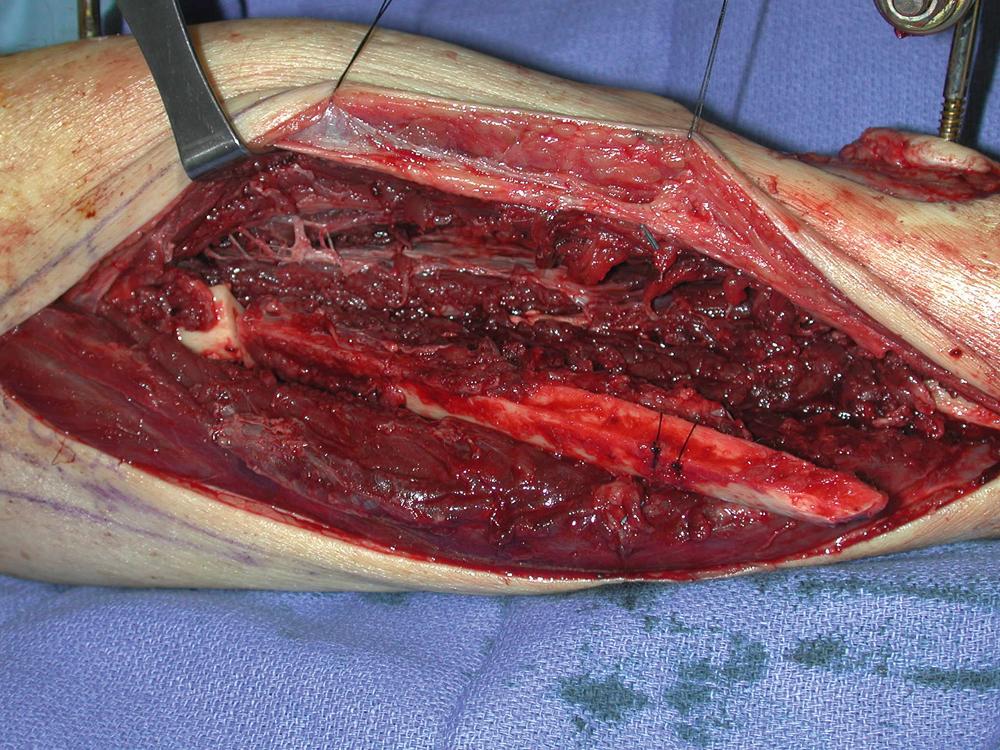
Under general anesthesia with the patient in the supine position, the right middle tibia wound was debrided. All unhealthy-looking skin and colonized tissues were removed. The open tibia wound appeared to be fresh and clean after a definitive debridement performed by the plastic surgery service ( Fig. 47.2 ).

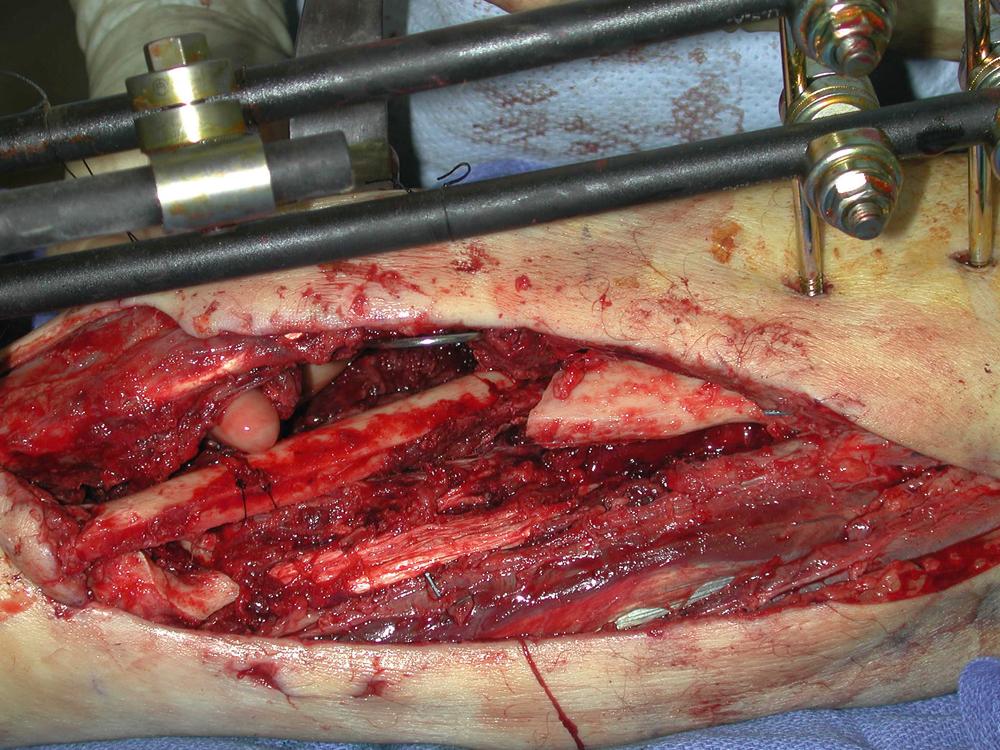
Both flap dissections were performed under tourniquet control. The existing open wound was extended into the incision both proximally and distally. The proximal incision was made toward the knee. The distal skin incision was made just above the Achilles’ tendon. After opening the fascia of the posterior compartment, both the medial gastrocnemius and the medial half of the soleus muscles were identified. The gastrocnemius muscle was easily separated from the underlying soleus muscle. The proximally based medial gastrocnemius muscle was dissected free and then split from the lateral gastrocnemius muscle along its raphe. The tendon portion of the gastrocnemius muscle was divided from the conjoined tendon. The fascial layer over the medial gastrocnemius muscle belly was scored. With the aid of this maneuver, the medial gastrocnemius muscle could reach the proximal portion of the middle tibia wound.
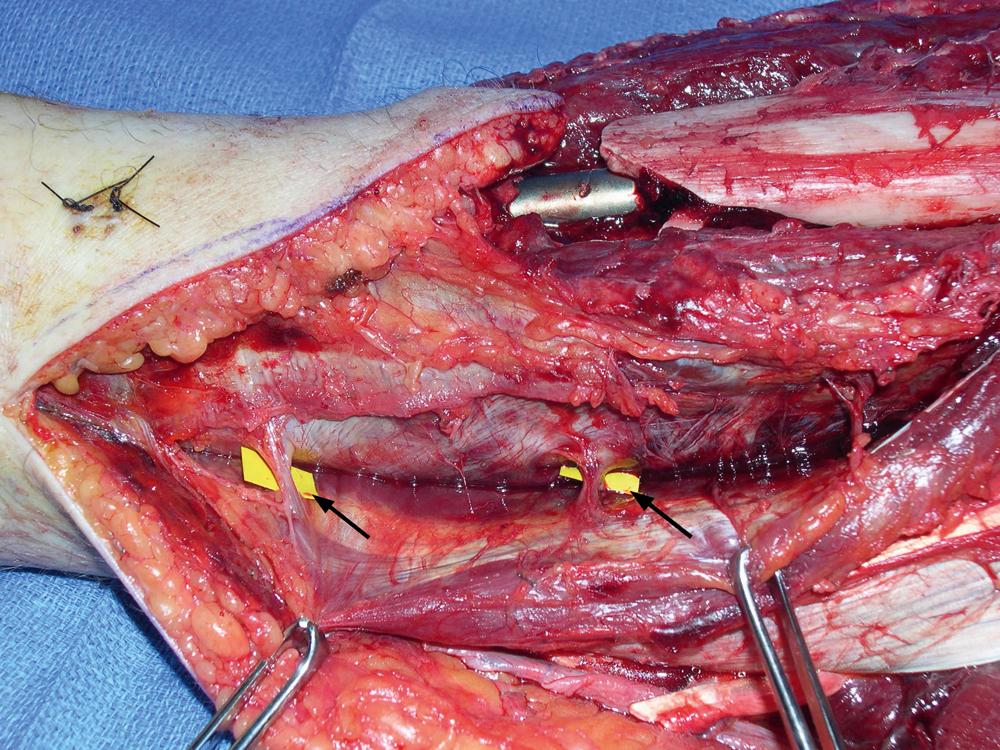
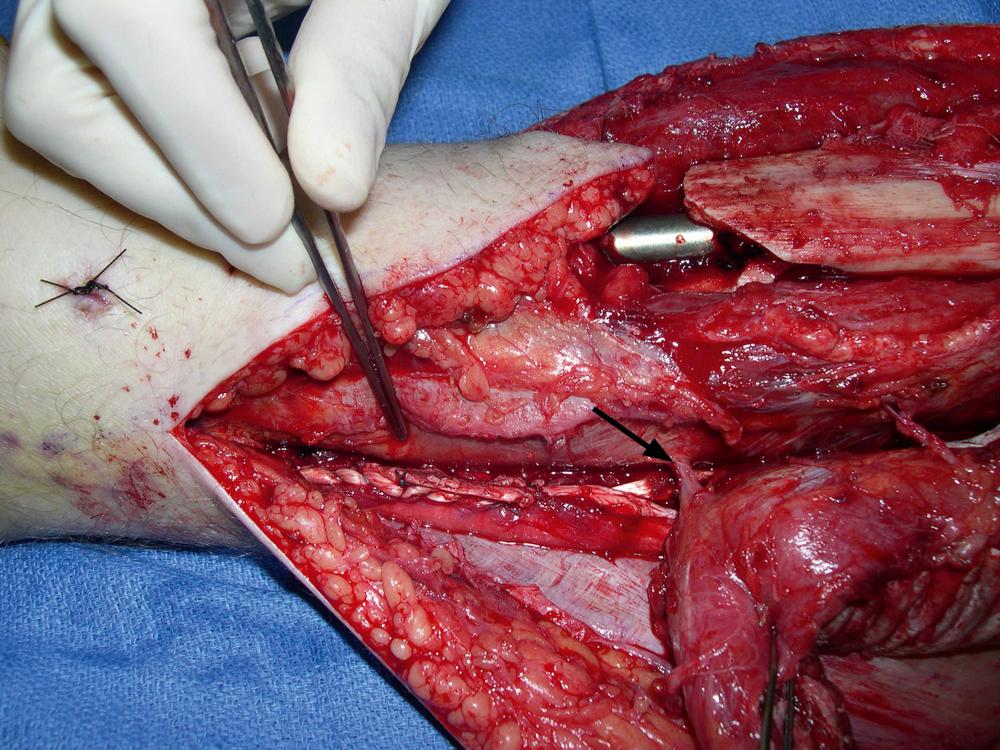
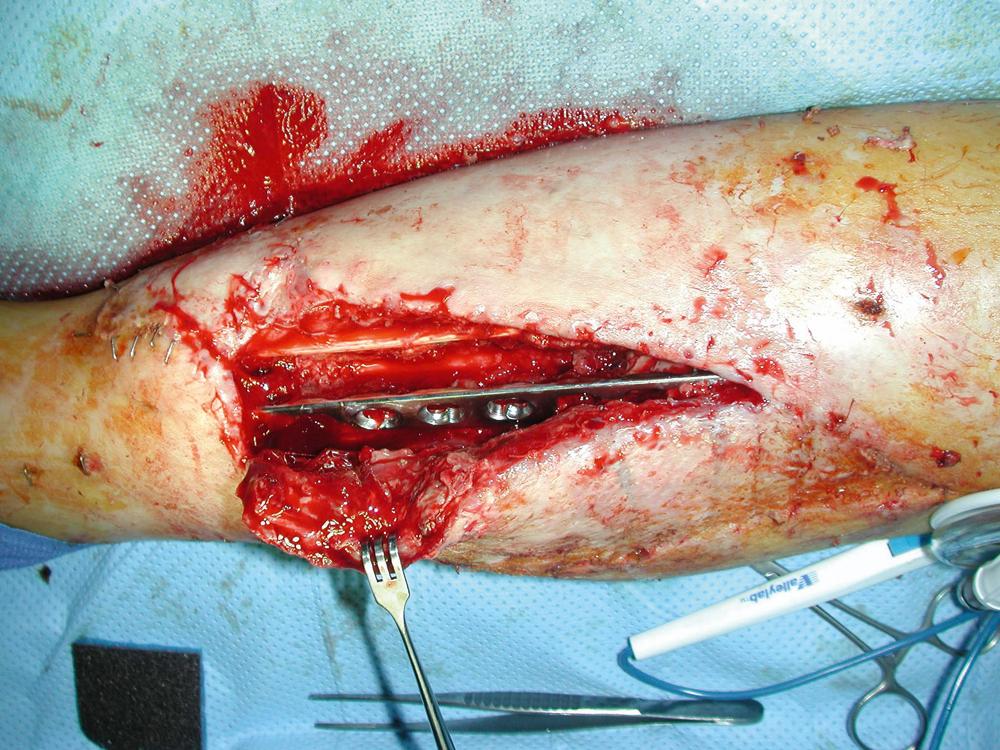
The medial half of the soleus muscle was dissected free from the flexor digitorum longus muscle. The medial half of the distal soleus muscle was sharply dissected with a knife and freed from the conjoint tendon distally. Only the muscular portion of the soleus was used as the flap and the remaining conjoint tendon was left intact. The insertion of the distal soleus muscle was divided close to the Achilles’ tendon depending on the arc of the flap rotation required to cover a more distal part of the middle tibia wound. The flap was based proximally and its dissection was completed with additional splitting of the medial half of the soleus muscle from the remaining lateral half of the muscle longitudinally depending on the need for coverage of the distal part of the middle tibia wound. The flap was only elevated to just at or above the level of the distal middle tibia wound where two major perforators from the posterior tibial vessels to the flap were identified ( Fig. 47.3 ). One of the adjacent perforators acted as a pivot point of the flap rotation and was preserved while allowing adequate arc of flap rotation to cover the middle tibia wound ( Fig. 47.4 ). The fascia was scored over the surface of the medial hemisoleus muscle belly to facilitate flap rotation. The left intact conjoint tendon from the distal medial half of the soleus muscle was then approximated to the remaining lateral half of the soleus muscle with nonabsorbable sutures ( Fig. 47.5 ).
Both muscle flaps were transposed into the middle tibia wound sequentially. The medial gastrocnemius muscle flap was placed proximally to cover the most proximal portion of the middle tibia wound and the medial hemisoleus muscle flap was placed distally to cover the most distal portion. Both flaps were inset into the medial tibia wound using absorbable half-buried horizontal mattress sutures ( Fig. 47.6 ).

A drain was placed under both muscle flaps. All muscle flaps were covered with split-thickness skin grafts. Split-thickness skin grafts were harvested with a dermatome from the right lateral thigh and meshed to 1:1.5 ratio. They were placed over the muscle flaps and secured with skin staples. All incisions for each flap dissection were closed in two layers ( Fig. 47.7 ).

The patient did well postoperatively without any issues related to the two-muscle flap reconstruction for the extensive middle tibia wound closure. He was discharged from hospital on postoperative day 5. The right middle tibia wound healed well and the skin grafts took uneventfully. He was followed by the plastic surgery service for routine postoperative care and by the orthopedic trauma service for fracture healing.
During further follow-up, the right middle tibia wound after the two-muscle flap reconstruction healed well with good contour and minimal scarring. There were no wound breakdown, recurrent infection, or contour issues ( Fig. 47.8 ). The patient has resumed his weight-bearing status and has returned to work as instructed.

The combined medial gastrocnemius and medial hemisoleus muscle flaps may provide the same quality of soft-tissue coverage for an extensive middle tibia wound as a free tissue transfer. Its cosmetic outcome after such local muscle flap reconstructions can also be quite pleasing. In general, a medial gastrocnemius muscle flap can be used to cover the proximal part of the wound and a medial hemisoleus muscle flap can be used to cover the more distal portion of the wound even to the junction of the middle and distal thirds of the leg. Obviously, in certain orthopedic trauma patients, these muscles may frequently be within the zone of injury, especially the soleus muscle. It has been the author’s preference to explore this muscle for its feasibility as a local muscle flap. If the medial gastrocnemius or the medial soleus muscle appears to be hemorrhagic and swollen, neither muscle can be used as a local flap. A preoperative magnetic resonance imaging scan of the muscles may be helpful to provide such information.
Scarifying both medial gastrocnemius and medial hemisoleus muscles as local flaps for soft-tissue coverage of an extensive tibia wound may lead to functional donor-site morbidity of the leg. Because only half of the gastrocnemius muscle and half of the soleus muscle are sacrificed and the remaining lateral halves of the gastrocnemius muscle and the soleus muscle are still intact, such a function loss may not be significant and can be well tolerated by most patients. In addition, the left intact conjoint tendon from the distal medial half of the soleus muscle is approximated to the remaining lateral half of the soleus muscle with nonabsorbable sutures. With this repair, potential functional impairment of the leg may be reduced.
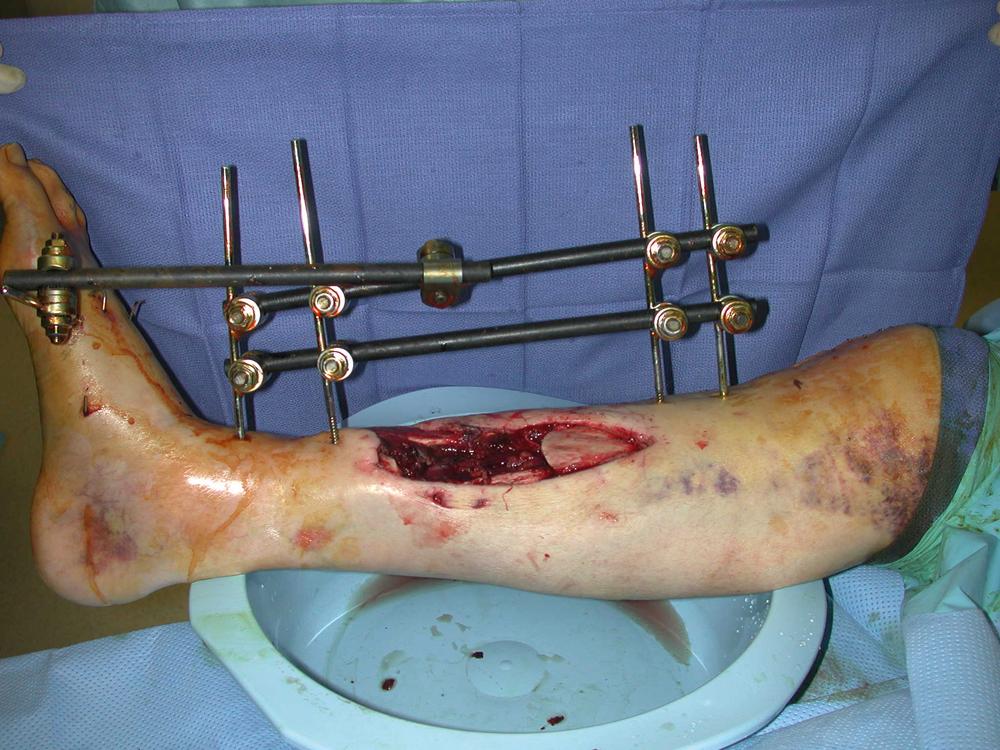
A 55-year-old White male, with severe cirrhosis of liver, sustained a traumatic injury to his right leg from a motor vehicle accident. He was initially managed by the orthopedic trauma service for bony and soft tissue debridement. He had a composite tissue loss in the middle third of the leg with a large soft tissue wound, measuring 15 × 6 cm and a segmental middle tibial fracture with a potential bony gap measuring 10 cm ( Fig. 47.9 ). He had also sustained a distal fibular fracture ( Fig. 47.10 ). An external fixator was placed for temporary bony stabilization and the patient was admitted to hospital for possible limb salvage procedure. The plastic surgery service was consulted for soft tissue reconstruction of the middle tibia wound immediately after the definitive bony fixation by the primary service. Because of his underlying medical conditions, more extensive limb salvage procedures, such as free tissue transfer, might not be indicated and the possibility of a below knee amputation (BKA) could be high.

For a composite defect of the middle third tibia wound with a large soft tissue defect and tibial gap, a free fibular osteocutaneous flap from the contralateral leg would be the classic option as a one-stage procedure for a composite reconstruction. However, this would be a lengthy operation involving microvascular free tissue transfer. In addition, the donor leg may be weakened after a free fibular osteocutaneous flap harvest. It might present a significant problem if this patient eventually has to undergo a BKA as a result of infected nonunion or an unsuccessful free flap reconstruction. After several extensive discussions with the orthopedic trauma surgeon, we all agreed that a less lengthy and extensive procedure would be more appropriate for the limb salvage procedure and a classic option, such as a free fibular osteocutaneous flap from the contralateral leg, would not be a good option for this patient. One of the interesting findings for this patient was that he also had a distal fibular fracture. Could the fibula be harvested as a pedicled vascularized bone flap to reconstruct the middle tibial bony defect? If this were feasible, the soft tissue defect in the middle third of the leg could also be reconstructed with a pedicled medial hemisoleus muscle flap. Thus, this composite tissue defect could be reconstructed as a one-stage orthoplastic approach from the same leg. No free tissue transfer would be needed and no donor site morbidity would result in the contralateral leg. The pedicled fibular flap could provide a vascularized bone for the best chance of bony union in the middle tibia after internal fixation with a reconstructive plate. The medial hemisoleus muscle flap would also provide an adequate soft tissue reconstruction for the middle tibia wound. A preoperative angiogram should be performed to evaluate patency of the peroneal artery as well as of the posterior and anterior tibial arteries.
Under general anesthesia with the patient in the supine position, the open tibia fracture wound was debrided by the plastic surgery service. All colonized tissues and skin edges were sharply debrided and the wound was then irrigated with Pulsavac ( Fig. 47.11 ). This was a combined orthoplastic procedure with close interaction between the plastic surgery and orthopedic surgery services in the operating room.

The ipsilateral pedicled fibula bone flap was designed and a 12-cm fibular segment in the middle leg was marked ( Fig. 47.12 ). Under tourniquet control, the skin incision was made over the lateral leg down to the fascia. After opening the fascia , the surgical dissection was performed to free the muscle attachment to the fibula from the soleus muscle. The distal fibular fracture site was dissected free. Once the peroneal vessels close to the fibular fracture site had been identified, further surgical dissection was performed to release the hallucis longus muscle’s attachment to the fibula. The peroneal vessels and the fibula were dissected free and protected. The proximal osteotomy was performed 10 cm distal to the fibular head. A 12-cm segment of the pedicled fibular bone flap was obtained ( Fig. 47.13 ). At this point, the fractured segmental tibia was removed by the orthopedic trauma service. Once the proximal peroneal vessels had already been dissected free, this pedicled fibular bone flap could easily be moved parallel to the tibial bony defect without difficulty ( Fig. 47.14 ).
The fibular bone flap was placed into the tibial bony gap after trimming each end and was then fixated to proximal and distal native tibia with a reconstruction plate and multiple screws by the orthopedic trauma service ( Fig. 47.15 ). Such a rigid fixation of the fibular bone flap appeared to be satisfactory.

The exposed fibular bone flap and reconstruction plate were then covered with the proximally based medial hemisoleus muscle flap. Under tourniquet control, the skin incision for the flap elevation was extended from the existing open wound in the middle tibia proximally and distally and through the skin, subcutaneous tissues, and fascia to expose the medial hemisoleus muscle. Once the medial hemisoleus muscle had been identified and dissected free from the medial gastrocnemius muscle and the flexor digitorum longus, its insertion was divided distally at the Achilles tendon. During dissection, the plantaris tendon was visualized between the gastrocnemius muscle and the underlying soleus muscle. The medial half of the soleus muscle was split along its anatomic midline. The medial hemisoleus muscle flap was elevated with emphasis on the preservation of as many minor pedicles from the posterior tibial vessels as possible to the flap in the middle tibia wound while allowing adequate arc rotation of the flap to cover the exposed fibular bone flap and reconstruction plate. Scoring the fascia over the medial hemisoleus muscle belly was also performed to enhance the flap’s arc of rotation. The flap was inset into the soft tissue defect with interrupted 3-0 Monocryl horizontal mattress sutures ( Fig. 47.16 ).

One drain was inserted into the flap donor site. The muscle flap was then covered with split-thickness skin grafts. Split-thickness skin grafts were harvested with a dermatome from the right lateral thigh and meshed to 1:1.5 ratio. The incision for the flap dissection was closed in two layers and all skin grafts were secured with skin staples ( Fig. 47.17 ). The entire orthoplastic procedure by two services took only 6 hours.

The patient tolerated the procedure well and remained medically stable. Unfortunately, he developed a distal tip necrosis of the medial hemisoleus muscle flap over the next 3 weeks presumably as a result of trauma to the distal muscle ( Fig. 47.18 ). He was taken back to the operating room by the two services 3 weeks later. The necrotic portion of the flap was debrided and the flap was largely elevated again ( Fig. 47.19 ). The fibular bone flap appeared to be viable and the medial hemisoleus muscle flap after debridement was inset into the soft tissue defect and approximated with interrupted sutures in the same fashion and a small area over the muscle flap was covered with a split-thickness skin graft ( Fig. 47.20 ).


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here