Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The concept of adenocarcinoma in situ (AIS) was first proposed in 1953 by Friedell and McKay on the basis of two cases of cervical adenocarcinoma that also appeared to contain a noninvasive precursor lesion. However, in the ensuing decades, despite remarkable progress in the understanding of the development of cervical squamous carcinoma, AIS remained obscure. It was not until the 1980s that AIS began to receive widespread recognition, highlighted by a detailed description of 72 cases by Jaworski et al. in 1988. AIS is now acknowledged to be the precursor to most invasive adenocarcinomas of the cervix on the basis of the following observations:
The cells of AIS appear neoplastic, and AIS is often found adjacent to early invasive adenocarcinomas.
Human papillomavirus (HPV) is detected in most AIS cases and with similar frequencies and subtypes (primarily types 16 and 18) in AIS and adenocarcinoma.
Retrospective reviews of biopsies and Papanicolaou (Pap) smears preceding cases of invasive adenocarcinoma have found examples of unrecognized AIS.
The average age of women with AIS is approximately 38 years, whereas the average age of women with early invasive adenocarcinoma is approximately 43 years (summarized by Lee and Flynn ), consistent with AIS being an antecedent to invasion.
p16ink4 staining, which is strongly associated with high-risk HPV, marks AIS and most adenocarcinomas.
At least 90% of cervical adenocarcinomas contain HPV. Types 16 and 18 account for approximately 80% to 90% of cases. Thus, as with squamous carcinoma, HPV is the most important risk factor for cervical adenocarcinoma. However, several features distinguish these two cancer types:
Adenocarcinoma of the cervix is increasing in incidence relative to squamous carcinoma.
Since the 1960s, the frequency of cervical adenocarcinoma has been increasing in the United States and other developed countries, where it currently accounts for 20% to 25% of all invasive cervical cancers. In a Canadian study, Liu et al. observed that from 1970 to 1996 the incidence of squamous carcinoma declined from 13.4 to 6.6/100,000, whereas the incidence of adenocarcinoma increased from 1.3 to 1.8/100,000. This increase has been especially evident among young white women. Although the causes of this increase are not clear, they are likely to include the combined effect of an increased incidence of AIS and the relative ineffectiveness of the Pap smear in detecting early glandular neoplasia.
As indicated, a high percentage of cases of adenocarcinoma are accounted for by HPV types 16 and 18, whereas squamous cell carcinoma is frequently associated with other high-risk HPV types as well.
Not all adenocarcinomas are associated with HPV—specifically, gastric-type, mesonephric, and clear cell carcinomas and some adenocarcinomas with intestinal differentiation.
There are several different subtypes of adenocarcinoma, possibly with different causes and natural histories. Ander-sson et al. have found that the index of HPV positivity in adenocarcinomas is age-related, decreasing from 89% in women younger than 40 years to 42% in women older than 60 years.
Contrary to squamous carcinomas, cigarette smoking has not been implicated as a risk factor for adenocarcinomas.
Some studies have supported a relationship between adenocarcinoma and its precursors and oral contraceptive use and, depending on the study, the associated risk increases as a function of length of use and current use.
This association may be stronger than that seen with squamous carcinomas, although this has not been supported in more recent studies, in which both neoplasms are associated with contraceptive use. One study of older women did not link cervical adenocarcinoma with estrogen replacement therapy. Thus, at this point, although oral contraceptives seem to be associated with the risk of both types of cervical cancer, the specific factors, other than smoking, that distinguish the risk of squamous versus adenocarcinoma are unclear.
In contrast to the previous understanding of cervical carcinogenesis as one in which disruption of the surface cervical keratinocytes renders the basal layer susceptible to infection by HPV and the resultant development of neoplasia, it is now thought that the residual embryonic stem cell populations of the cervical squamocolumnar junction (SCJ) play a pivotal role. The evidence for this is multifactorial:
The cells of the cervical SCJ have an identical immunophenotype (strongly CK7 positive) and genetic signature to squamous intraepithelial lesions (SILs) and invasive carcinoma, implying a continuum of changes in carcinogenesis.
Cervical SCJ cells are notably susceptible to HPV infection due to being a cuboidal monolayer, with differentiation potential and susceptibility to neoplastic transformation.
The cell population of the SCJ may be immunologically different from cervical keratinocytes.
For example, defensin 5 (HD-5), a small peptide with microbicidal activity that inhibits entry of HPV virions, is prominently expressed in the normal ectocervix, vulva, and vagina and is absent in cervical SCJ; the reasons for this are undetermined. It has been suggested, in light of data emerging over the past few years, that SCJ cells could be infected by HPV and serve as a nidus for early lesion development. Presumably these cells are capable of undergoing columnar or, via reserve cell differentiation, squamous differentiation. However, how they become selectively vulnerable to columnar neoplasia remains unclear.
A cytologic interpretation of atypical endocervical cells, adenocarcinoma in situ, and adenocarcinoma connotes increasingly serious conditions and merits increasingly greater scrutiny. However, because these are often difficult to separate cytologically, the exclusion of glandular neoplasia ultimately requires a colposcopic examination and, often, a cone biopsy. This is in contrast to the spectrum of squamous abnormalities, the options for which include cytologic follow-up, colposcopy, and, currently, HPV testing. Thus, because diagnostic and nondiagnostic glandular atypias require a similar initial follow-up approach, they merit discussion as a single group and will be addressed together in this section ( Box 14.1 ).
Neoplastic lesions
Adenocarcinoma in situ
Cervical adenocarcinoma
High-grade squamous intraepithelial lesion
Endometrial hyperplasia, carcinoma
Extrauterine adenocarcinomas
Non-neoplastic lesions
Tubal metaplasia
Direct sampling of lower segment epithelium
Menstrual endometrium
Reactive endocervical lesions (e.g., cervicitis, microglandular hyperplasia, Arias-Stella, radiation effect)
Atrophy
In principle, adenocarcinoma of the cervix can be prevented through the detection and elimination of its precursor, AIS. However, in contrast to squamous cell carcinoma, in the United States, an increased incidence of AIS has not been accompanied by a decrease in invasive adenocarcinoma to date. Because of the low number of cases, more time may be needed to assess the impact of improved detection of AIS on the incidence of invasive adenocarcinoma. Data from the United Kingdom support a decrease in the incidence of cervical adenocarcinoma that is attributable to increased screening, although the effect is of lesser magnitude and duration than that seen with squamous cell carcinoma. Ultimately, HPV vaccination may provide the most effective means of preventing cervical adenocarcinoma, given the fact that HPV types 16 and 18 are associated with more than 80% of these neoplasms.
Unfortunately, Pap smears are not as sensitive for glandular precursors as they are for squamous cells. We calculated a smear sensitivity of 55% to 70% for AIS and of 45% to 76% for invasive adenocarcinoma in our studies. This lack of sensitivity is primarily related to two factors:
Deficient endocervical sampling, which has contributed significantly to low sensitivity in the past
However, the combination of newly designed collection instruments and heightened awareness of the importance of sampling the transformation zone have reduced this component of the problem.
Underappreciation of glandular atypia on smears
We found a screening and interpretive false-negative frequency of 40% to 50% after a retrospective review of prior negative Pap smears in women with AIS or invasive adenocarcinomas. Others have reported similar findings. This observation reflects the difficulties mentioned earlier that are inherent in distinguishing benign from malignant glandular-appearing cells.
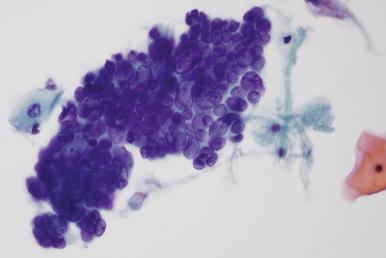
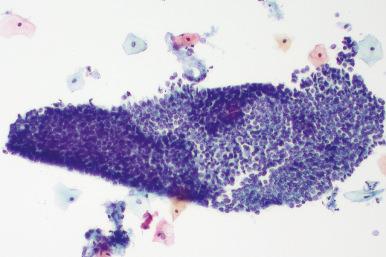
AIS cells aggregate in hyperchromatic crowded groups. Features of endocervical glandular differentiation in these groups include the following:
Strips of columnar cells with crowded, basally oriented nuclei and pale, foamy, or vacuolated cytoplasm
Feathering—the perpendicular orientation of the long axis of the cells around the periphery of the group such that the nuclei and small wisps of cytoplasm protrude radially
Rosettes—glandlike structures with radially oriented nuclei around a central space
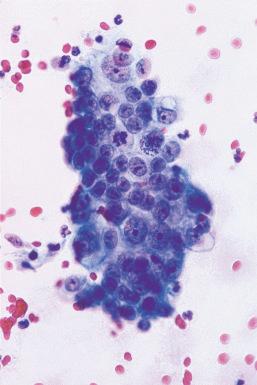
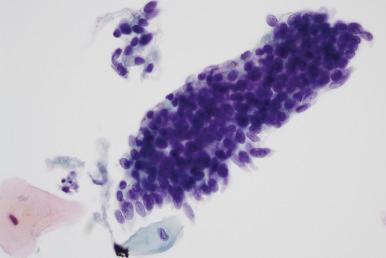
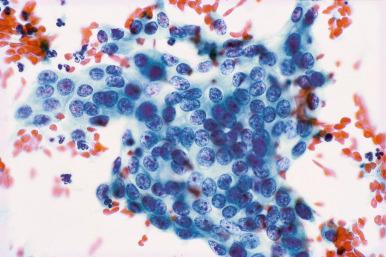
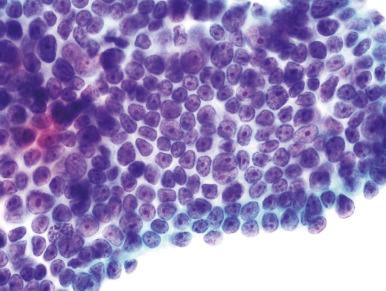
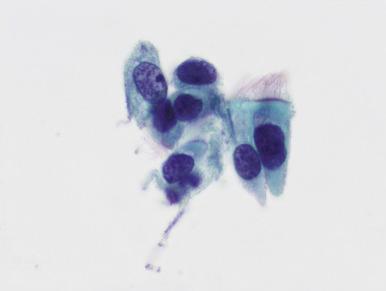
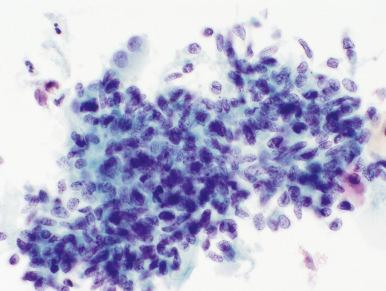
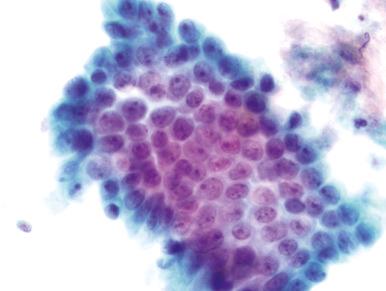
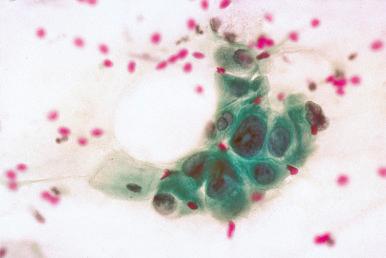
Neoplastic nuclear features are essential for confirmation. With AIS, there is usually extreme nuclear crowding, often with molding of nuclei around one another. Nuclei are slightly enlarged, ovoid or irregular, and hyperchromatic, with diffusely dispersed, slightly to moderately coarse chromatin particles. Nucleoli are usually inconspicuous but are prominent in some cases. Mitotic figures may be found in about 40% of cases but often only after a diligent search ( Figs. 14.1 to 14.6 ).
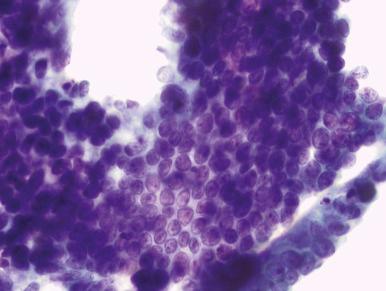
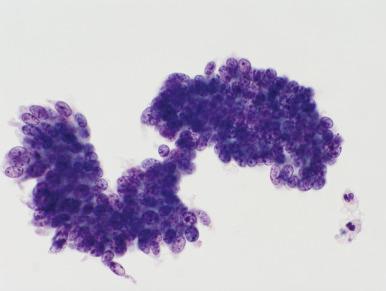
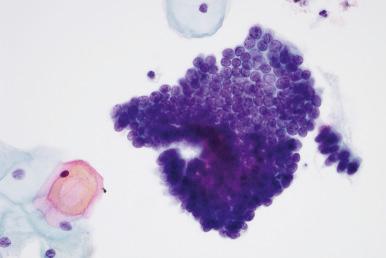
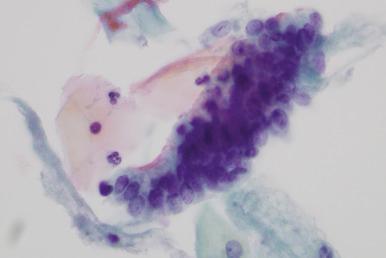
In liquid-based preparations, AIS groups are smaller and architectural clues, such as columnar cells in strips and rosettes, are not as obvious; the chromatin is finer and nucleoli are more obvious. Importantly, however, extreme cell crowding and feathering remain pronounced in liquid-based preparations. Also, the chromatin remains coarse relative to that of normal endocervical cells and thus can be readily perceived. It is important to emphasize, however, that the distinction between AIS and invasion cannot be made with certainty on the basis of the cytologic evaluation alone.
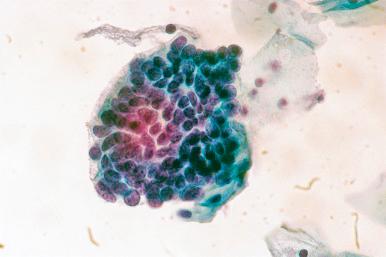
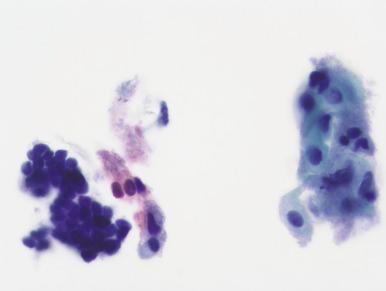
The smear presentation is more variable than in AIS, being dependent on the cell type and grade of the adenocarcinoma. A bloody or necrotic-appearing background is often absent, especially with early adenocarcinoma, and cannot be relied on to confirm invasion. Conversely, a bloody smear with only a few poorly preserved groups should not be dismissed as unsatisfactory without careful scrutiny because some advanced adenocarcinomas present with this picture.
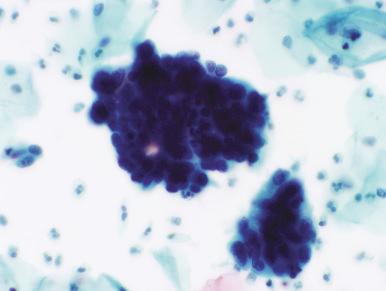
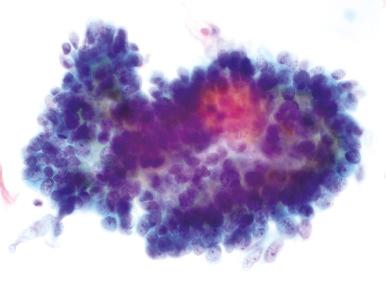
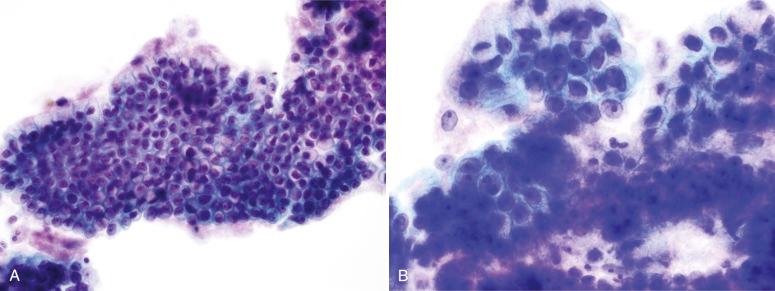
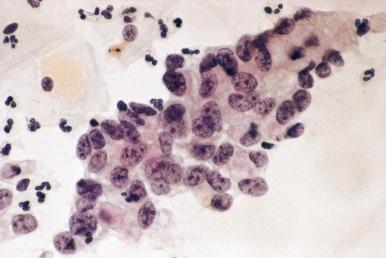
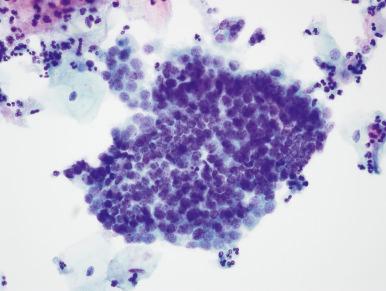
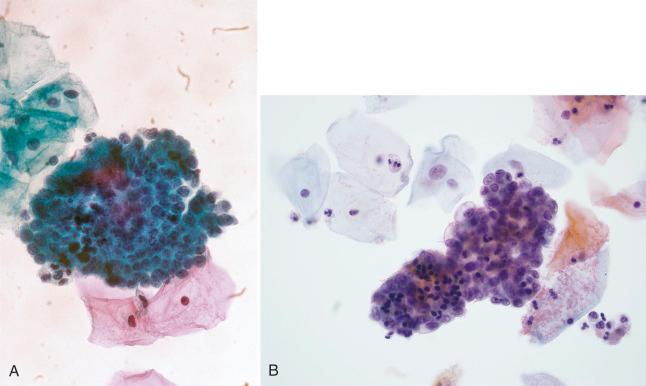
Usually, the cell groupings in adenocarcinoma are numerous, similar to one another, and lack the orderly honeycomb pattern of normal or reactive endocervical cells. Large branching or papillary groups, even if composed of AIS-like cells, suggest invasion. In some cases, single cells and very small groups predominate.
These cells are usually larger than those of AIS. The cytoplasm is pale to eosinophilic and is sometimes vacuolated. From case to case, nuclear chromatin ranges from vesicular to coarse, nucleoli vary from absent to prominent, and mitotic figures may be frequent or scant ( Figs. 14.7 to 14.9 ).
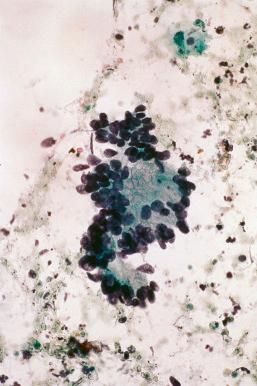
In some cases of well-differentiated adenocarcinoma, the features that distinguish it from reactive endocervical cells may be subtle. The finding of numerous groups of similar-appearing, only slightly atypical glandular cells should at least raise the possibility of carcinoma ( Fig. 14.10 ).
Specific subtypes of adenocarcinoma such as adenoma malignum, well-differentiated villoglandular, or serous may have characteristic findings. These are important insofar as their recognition invokes the possibility of carcinoma. However, adenocarcinoma subtypes cannot be reliably identified on the basis of their cytologic appearance.
The most serious error is mistaking AIS or adenocarcinoma for a benign process. Usually, this occurs because the cells are considered to be endometrial cells or reactive endocervical cells.
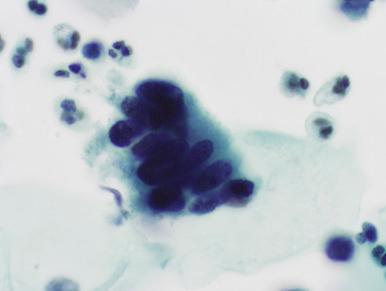
In AIS, as with menstrual endometrium, the cells are extremely crowded but, unlike the latter, the cells in AIS have well-preserved nuclei and at least subtle feathering or small rosettes. The absence of endometrial stromal fragments, cells in honeycombed sheets, or three-dimensional tubular groups rules against direct sampling of the endometrium (discussed later; Figs. 14.11 and 14.12 ).
In AIS or adenocarcinoma, the abnormal cell population is relatively monomorphous, not a spectrum, as is commonly seen with reactive endocervical cells. Neoplastic groups have overlapping or crowded nuclei that have a range of chromatin coarseness and either small or prominent nucleoli ( Figs. 14.13 to 14.16 ). In some cases, this distinction is admittedly difficult. Smears with only slightly atypical endocervical-appearing cells (see Fig. 14.10 ) or bloody smears with only a few atypical cells are two patterns of adenocarcinoma that are often underdiagnosed.
Mistaking benign lesions for AIS or adenocarcinoma is a more common error than false-negative interpretations.
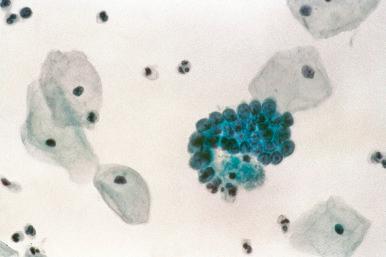
In the most common benign mimic of AIS, tubal metaplasia, the cells, although enlarged and crowded, are usually less so than in AIS. Nuclear chromatin is finer than in AIS, and feathering and rosettes are absent ( Figs. 14.17 and 14.18 ). Cytoplasmic cilia are a key finding, confirming tubal metaplasia, but often are difficult to visualize. One needs to see discrete hairlike cytoplasmic processes because adherent background debris can mimic cilia.
Cells directly scraped from the lower segment of the endometrium are not uncommon. This is especially true in women who have had a cone biopsy. They appear in fragments that may resemble those of AIS and may include cells with mitotic figures. However, in lower segment endometrium, the cells are arranged in flat sheets or three-dimensional tubules that lack feathering or rosettes ( Fig. 14.19 ). Cells are small, uniform, and evenly dispersed, with fine or dense (India ink) nuclear chromatin ( Fig. 14.20 ). Groups of endometrial stromal cells (tangles of spindled cells with bland oval nuclei and wispy cytoplasm), attached to or independent of the epithelial groups, are an important clue ( Fig. 14.21 ).
Perhaps surprisingly, clusters of menstrual endometrial cells may sometimes be difficult to separate from AIS or a high-grade squamous intraepithelial lesion ( Fig. 14.22 ). Also, sometimes, large pseudopapillary endometrial fragments are encountered that are frightening in their similarity to adenocarcinoma. In these situations, as in all difficult cytologic interpretations, evaluation of the worrisome cells in the context of the entire spectrum of cells on the smear is critical. Most groups of menstrual endometrial cells have small molded nuclei with scant or absent cytoplasm and interspersed pyknotic nuclear fragments or are in tight balls of stromal cells surrounded by larger epithelial cells. Hyperchromasia is present but is degenerative, with dense, smudged, or beaded chromatin. Feathering, rosettes, or strips of columnar cells, characteristic of AIS, are absent.
Reactive endocervical cells, whether from cervicitis, endocervical polyps, microglandular hyperplasia, irradiated endocervix, or the Arias-Stella reaction, may resemble AIS or adenocarcinoma. As opposed to neoplasia, in cervicitis or polyps there are sheets of repair-like cells containing evenly distributed nuclei with fine chromatin, sometimes prominent nucleoli, and delicate nuclear membranes. Nuclear size may vary both within and among groups, but the nuclear-to-cytoplasmic ratio is generally retained ( Fig. 14.23 ).
Microglandular hyperplasia may yield groups with enlarged, sometimes vacuolated cells that raise the possibility of adenocarcinoma. However, nuclei are variably sized, rather than monomorphic, the chromatin is fine, and there may be adherent crowded reserve cells or immature metaplastic cells, some with recognizable intercellular bridges ( Fig. 14.24 ).
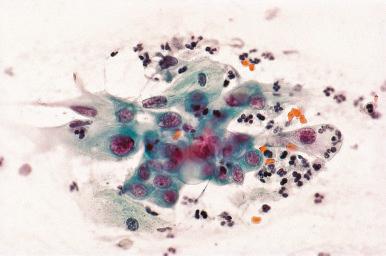
With irradiation and the Arias-Stella reaction, there are gigantic cells with voluminous, sometimes vacuolated cytoplasm. Nuclei vary from normal-sized to very large, often within the same group, and have smudged chromatin and intranuclear vacuoles ( Fig. 14.25 ).
Aside from the well-known problem of benign nuclear atypia in atrophy mimicking squamous dysplasia, atrophic cells may sometimes shed some or all of their cytoplasm and aggregate in pseudoglandular groups, which may be mistaken for endometrial cells, endometrial carcinoma, or even metastatic carcinoma. The atrophic nuclei are small, bland, and uniform. Importantly, they are identical to those of the intact cells and cells that have lost only part of their cytoplasm that are present in the background ( Fig. 14.26 ).
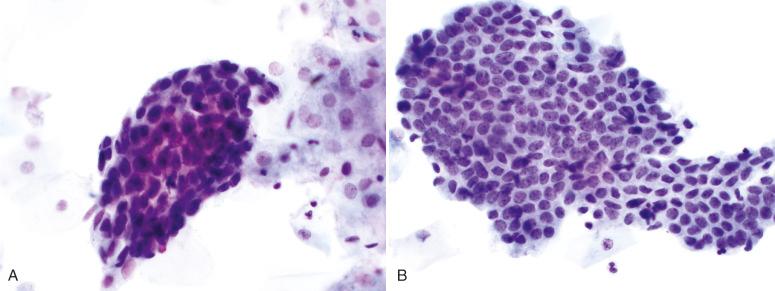
A high-grade squamous intraepithelial lesion (HSIL) is the most frequent neoplastic mimic of AIS. Most biopsies that contain a neoplastic lesion following a report of glandular atypia in Pap smears have HSIL without AIS. In AIS-like HSIL, the abnormal cells are in very crowded groups, with coarsely hyperchromatic nuclei and scant cytoplasm ( Fig. 14.27A ), or are loosely arranged, with a pale, finely vacuolated cytoplasm (see Fig. 14.27B ); both appearances mimic glandular differentiation. However, the absence of distinctly columnar shapes, pronounced feathering, or rosettes argues against this. As a general rule, if there is uncertainty as to whether the cells are HSIL or AIS, they are likely to be the former. As a corollary, glandlike HSIL may be mistaken for reactive rather than neoplastic glandular cells (similar to the problem of false- negative interpretations with AIS, discussed later).
The reported frequencies of atypical glandular cells (AGCs) from individual laboratories have varied widely, from 0.08% to 5.96%, with an overall average of 0.29%. Aside from this wide spectrum of sensitivity, an AGC interpretation is poorly reproducible. In two retrospective reviews of smears initially interpreted as AGC, expert reviewers not only disagreed with the initial AGC interpretation in most cases but also disagreed among themselves as to which cases should remain as AGC. Notably, several cases from both studies that had been reclassified by some reviewers as benign were from high-grade squamous or glandular lesions.
However, as noted earlier, biopsy follow-up after an AGC interpretation often indicates a high-grade squamous rather than a glandular lesion. Thus, a smear interpretation of AGC, although lacking specificity and reproducibility, carries a significant risk for high-grade neoplasia. In light of this finding, the 2006 consensus guidelines for Pap smear follow-up recommended colposcopy and biopsy as the initial response to all smears interpreted as atypical glandular cells or atypical endocervical cells. In women older than 35 years, endometrial sampling is also recommended.
The Bethesda 2014 terminology for reporting glandular lesions remains similar to the Bethesda 2001 terminology ( Box 14.2 ). Of note, the reporting of a finding of otherwise benign-appearing endometrial cells has been moved from an age of 40 years at initiation (in the 2001 Bethesda classification) to an age of 45 years to improve the predictive value of the result.
Epithelial cell abnormality—glandular
Atypical glandular cells, NOS (specify endocervical, endometrial, or not otherwise specified)
Atypical glandular cells, favor neoplastic (specify endocervical or NOS)
Endocervical adenocarcinoma in situ (AIS)
Adenocarcinoma, specify as appropriate (endocervical, endometrial, extrauterine, NOS)
NOS, Not otherwise specified.
In addition, endocervical adenocarcinoma in situ is a separate diagnostic category now that enough experience with its cytologic appearance has accrued. Despite recognition of AIS as a distinct category, in practice this diagnosis is more difficult to recognize than other serious diagnoses. Nevertheless, the 2001 Bethesda classification scheme overall is more likely to correlate with a significant lesion than the 1991 terminology.
Most cytologic preparations are now liquid-based. A comparison of conventional smears, ThinPrep and SurePath (BD Diagnostics, TriPath, Burlington, NC), and liquid-based preparations found similar criteria applied for detecting endocervical glandular neoplasia in all three specimen preparations. ThinPrep was less likely to exhibit large dark sheets of cells and individual cells than the other two methods, whereas feathering was more pronounced in conventional smears.
The 2012 consensus guidelines from the American Society for Colposcopy and Cervical Pathology (ASCCP) for the initial management of all categories of atypical glandular cells, except atypical endometrial cells, did not recommend high-risk HPV triage for initial presentations of atypical glandular cells. Based on two large US studies, 25% of cases in the AGC category test positive for high-risk HPV, of which the most prevalent genotypes are 18 and 45, followed by 16. Although several studies have indicated that the presence of high-risk HPV is highly predictive of high-grade lesions (glandular and squamous) following AGC, and that false-negative interpretations are infrequent, caveats are that in some cases, the atypical glandular cells are from endometrial, tubal, or even ovarian carcinomas that are not HPV-related. Also, a significant minority of cervical adenocarcinomas in situ and invasive cervical adenocarcinomas are HPV negative. Thus, reliance on a negative HPV test result to avoid colposcopy or endometrial biopsy following the reporting of atypical endocervical cells or atypical glandular cells on a smear may lead to underdiagnosis of a serious lesion. In fact, the heterogeneity of the lesions associated with AGC means that no single approach is adequately sensitive for detecting disease in this high-risk category. Consequently, all patients with AGC are recommended to undergo initial colposcopy with endocervical sampling, and endometrial sampling if older than 35 years, with or without initial colposcopy. In patients for whom a high-grade lesion (cervical intraepithelial neoplasia [CIN]2+) is not identified, two HPV co-test results are then used to determine the need for colposcopic evaluation and the interval for subsequent cytology screening.
Unlike squamous lesions of the cervix, the colposcopic criteria for AIS are not well defined, and negative colposcopy cannot be relied on to exclude a neoplasm following a cytologic diagnosis of abnormal glandular cells or AIS. However, most women with AIS will have a colposcopic abnormality. In one study, 67 of 90 women (74%) with AIS who underwent colposcopy had an abnormal examination result. However, a glandular abnormality was suspected prior to colposcopy in only 19 (28%). As discussed earlier, only a minority of Pap smears showing atypical glandular cells will show a histologically significant glandular abnormality on follow-up biopsy. In a review of 16 studies with biopsy follow-up after a cytologic diagnosis of atypical glandular cells of undetermined significance (AGUS), favor reactive, or AGUS not specified, only 3.2% of patients had either AIS or invasive endocervical adenocarcinoma, whereas 3.9% had endometrial carcinoma and 25% had cervical intraepithelial neoplasia (CIN), with most of the latter being high grade. However, if the AGUS interpretation was qualified as favor neoplastic, 62% had AIS or invasive adenocarcinoma, and an additional 18% had CIN. Additionally, a large study from Taiwan has examined more than 100,000 consecutive smears. Approximately 0.1% of cases were categorized as atypical glandular cells—Bethesda 2001 terminology was used; of these, 80% had adequate histologic follow-up. Nearly 10% of patients were found on biopsy to have endocervical adenocarcinoma or AIS, suggesting that the Bethesda 2001 system leads to an increase in the clinical significance of the diagnosis of atypical glandular cells. Moreover, women diagnosed with atypical glandular cells, favor neoplasia, were more likely to have more significant pathology than women diagnosed with atypical glandular cells, not otherwise specified.
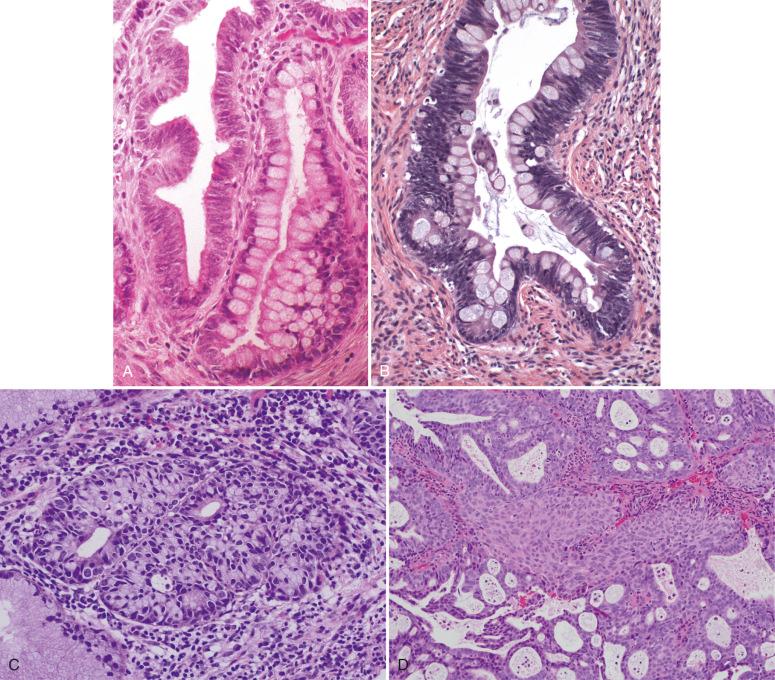
Although it may spread widely within the endocervix, AIS almost always involves the region close to the SCJ, most likely arising from HPV-infected columnar cells or progenitor SCJ cells that have become committed to glandular differentiation. AIS probably originates in developmentally vulnerable cells in the surface epithelium and then extends into underlying crypts, sometimes juxtaposed with normal epithelial cells within the deeper portion of the affected crypt ( Fig. 14.28A ). It may then extend circumferentially around the cervix and proximally up the canal, sometimes all the way out of the uterus. Rarely, AIS initially develops high in the canal or is multifocal. About 50% of cases have a concomitant high-grade CIN; the AIS is almost always located adjacent and usually proximal to the CIN (see Fig. 14.28A ).
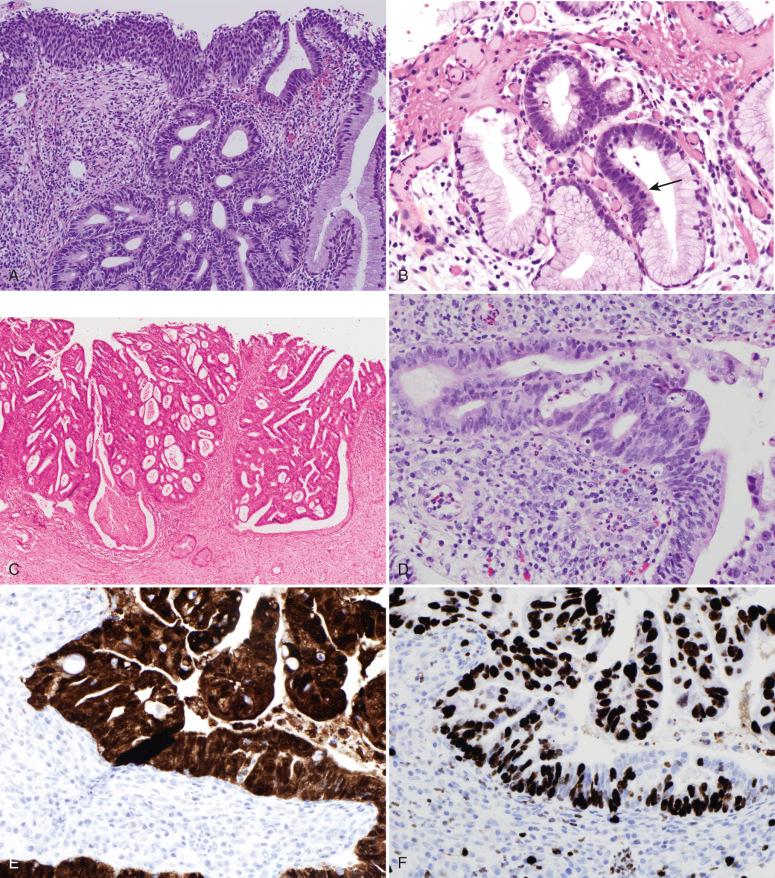
This occurs with stratification or pseudostratification (see Fig. 14.28B ).
Nuclei are variably enlarged and are oval, elongated, or irregular.
Nucleoli are usually small or absent but may be prominent in some cases.
These are invariably present, often easily visualized at the luminal pole of the cell, but there may be as few as one or two to five high-power fields.
Located in the basal portion of the gland, these are present in about 70% of cases ; one should require a definitive eosinophilic body containing sharply delineated dark fragments of chromatin so as not to confuse degenerated leukocytes with apoptotic bodies (see Fig. 14.28B ).
These sometimes include papillary or cribriform intra-glandular growth and may be quite florid, suggesting invasive carcinoma. However, the stromal interface of the AIS gland maintains the smooth, well-demarcated appearance of the original benign gland it has replaced (see Fig. 14.28C ). The stroma underlying AIS may contain variable concentrations of acute or chronic inflammatory cells. Their presence alone does not connote invasion.
In addition to the preceding situations, there are several AIS subtypes; often, these are mixed within the same case. It is important to be aware of these and to be able to identify them all as AIS; however, they have not been shown to differ in their propensity to invade or in the subtype of adenocarcinoma they produce. Therefore, there is no compelling reason to separate them in the diagnostic report other than to call attention to particularly unusual patterns, such as intestinal or endometrioid types.
This is named for its resemblance to endocervical cells and is the most common. The cells have a columnar cytoplasm that is mucinous-appearing or eosinophilic (see Fig. 14.28B ).
This has more nuclear stratification and less cytoplasm, mimicking neoplastic endometrial glands.
This is distinguished by a variable proportion of goblet cells ( Fig. 14.29A ). Immunohistochemical staining for CDX2 in intestinal-type AIS typically demonstrates positive staining in AIS epithelium, both in areas of obvious intestinal differentiation and in areas without prominent goblet cells (conventional-type AIS adjacent to intestinal-type AIS). This suggests that morphologic changes of intestinal differentiation may not be evident early in the process. There is less nuclear crowding and hyperchromasia in this variant, making confirmation more difficult. However, intestinal differentiation alone is an important clue to AIS, because benign intestinal metaplasia of the cervix is rare. Occasionally, gastric (pyloric) or pancre-aticobiliary differentiation will be seen (see Fig. 14.29B ). The intestinal-type AIS often stains less intensely with p16. Interestingly, patients with intestinal-type endocervical AIS are on average older (44.5 vs. 32.6 years), and multiple studies have shown that the frequency of HPV detection in intestinal-type AIS is less than that for other forms of AIS, with a corresponding lower rate of p16 diffuse positivity. Together, these data suggest more than one pathway of pathogenesis for this AIS subtype.
This has been described, but AIS with conspicuous tubal differentiation would be exceedingly uncommon, and the diagnosis should be made only if there are unequivocal nuclear features of AIS, including mitotic figures. Most ciliated lesions are non-neoplastic (see later discussion of benign mimics).
This variant (see Fig. 14.29C ) has also been informally termed stratified mucin-producing intraepithelial lesion (SMILE). At low magnification, the lesion appears similar to a squamous intraepithelial lesion, but on close inspection, the stratified neoplastic cells contain intracellular mucin. This variant may be a form of AIS, particularly because many have conventional AIS and HSIL in the specimen. Currently, we report these as “AIS, stratified variant.” We found the association with invasive carcinoma to be stronger than for HSILs, but experience was limited. Others have linked this entity to adenocarcinomas, distinguishing it from conventional HSILs.
True adenosquamous carcinoma in situ, containing intimately admixed glandular and squamous differentiation in the same focus, is uncommon (see Fig. 14.29D ). Most are combinations of spatially distinct HSIL and AIS, which we would diagnose separately rather than classify the lesion as adenosquamous.
It is reasonable to assume that in its earliest form, AIS may not manifest with the full range of atypia that characterizes well-established lesions. We previously reported a variant of AIS termed superficial or early AIS, which had the following characteristics: (1) occurrence in younger women, with a mean age in the low 20s; (2) a more restricted distribution, which was principally superficial; and (3) less conspicuous mitotic activity, nuclear atypia, and apoptosis. Like other forms of AIS, these lesions were HPV positive and contained a discrete punctate nuclear signal, with high-risk HPV probes characteristic of integrated DNA. At its most recognizable form, early AIS manifests as discrete hyperchromatic and nonciliated foci on the surface, with apoptosis or mitotic activity ( Fig. 14.30A and B ). Less conspicuous are lesions that are not hyperchromatic but demonstrate small but discrete differences in nuclear morphology, with mitotic activity (see Fig. 14.30C and D ). Immunostains for MIB-1 and p16 are typically strongly positive and can be helpful in confirming the diagnosis (see Fig. 14.30B ).
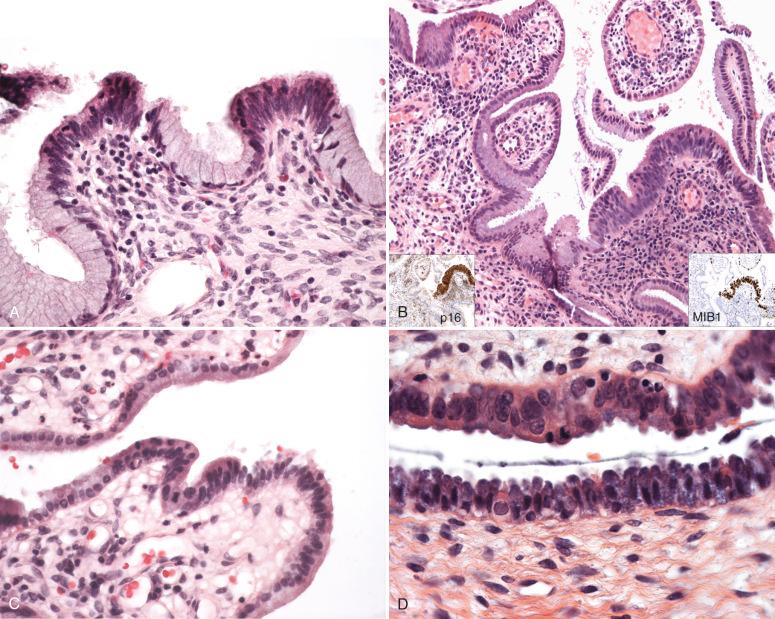
Because they are strongly associated with HPV, most AIS will stain strongly for p16. This biomarker is occasionally used to distinguish AIS from tubal or tubal-endometrial metaplasia from AIS. The latter will stain but typically in a heterogeneous fashion.
One series has concluded that although benign proliferations (e.g., reparative or inflamed endocervical epithelium, microglandular hyperplasia, tubal metaplastic epithelium) typically have a proliferative index less than 10%, the proliferative index in AIS often exceeds 50%. There are exceptions, however, particularly with inflamed endocervical mucosa, and we rely principally on p16 to aid in making the distinction between reactive and neoplastic columnar epithelium.
Stathmin-1 is a microtubule destabilizing protein shown to be overexpressed in a number of cancer types. A single series has shown that all cases of benign endocervix are negative for the biomarker, whereas all cases of AIS show diffuse positivity and all cases of adenocarcinoma show patchy or diffuse positivity. The initial results are promising; further studies with larger sample sizes will be needed to corroborate and generalize these findings.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here