Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
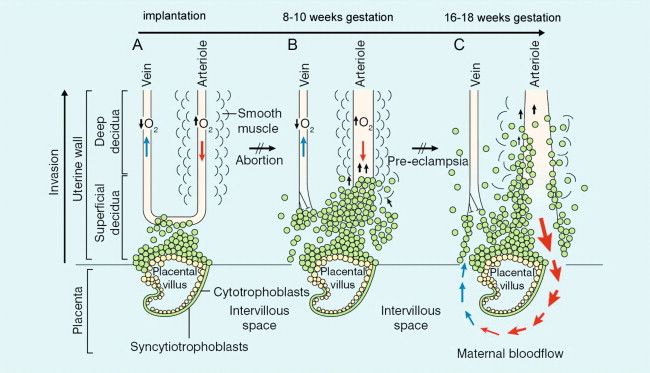
The circulatory changes that occur during pregnancy involve modification of vascular structure within the uterus (spiral arteries), the development of a neocirculation (the placenta and the fetus), a redistribution of blood flow and alteration in circulating blood volume such that the placenta in the third trimester receives 20% of the total maternal circulation and maternal blood volume increases by a similar value. Certain disease processes and certain complications of pregnancy are at least in part mediated by a microvascular abnormality. Thus, for example, impaired trophoblast migration of the spiral arteries is a major component in pre-eclampsia. As a result Doppler studies are now essential tools in the detection of complications of pregnancy, detection and characterisation of certain fetal abnormalities, as well as detection and management of maternal disease.
The uterine artery is a branch of the anterior division of the internal iliac artery, and divides further into four arcuate arteries, each of which divides into more than 25 spiral arteries. There are therefore between 100 and 200 spiral arteries which enter the intervillus space. During early pregnancy, trophoblast cells invade this space and disrupt the wall of the spiral arteries as part of the process of placental formation. There are two separate waves of invasion. Between implantation and 10 weeks, the trophoblastic invasion is limited to the decidual layer. From about 14 weeks until 22 weeks, the invasion extends as far as the spiral arteries. This invasion of the spiral arteries affects the resistance to blood flow within the spiral arteries and thereby in the arcuate and main uterine arteries ( Fig. 15-1 ).
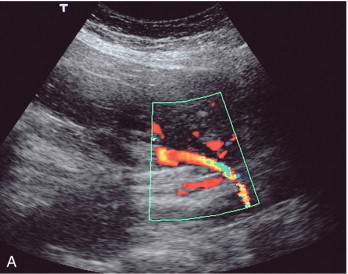
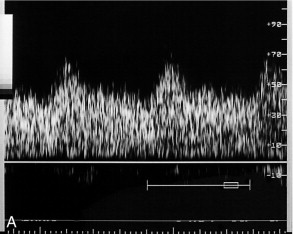
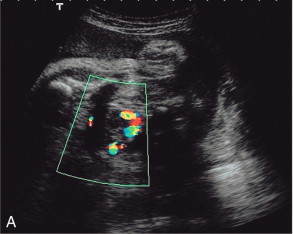
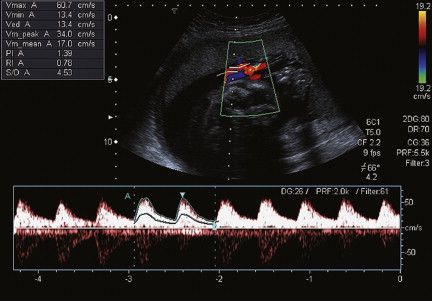
The complexity of the uteroplacental circulation makes accurate identification of the vessel under study difficult with either continuous wave or duplex Doppler ultrasound. Originally flow velocity waveforms were obtained using these modalities by angling the transducer towards the cervix on either side of the lower quadrant of the uterus. , However the uterine arteries are more accurately identified using colour Doppler, which is now the recommended technique to study this artery. The region lateral to the lower uterus is examined and the external iliac artery and the adjacent vein are identified. The uterine artery crosses the external iliac artery on its course from the internal iliac artery to the body of the uterus. It is important to angle the transducer to improve the angle of insonation whilst maintaining vessel identification on colour Doppler. Spectral waveforms are obtained by placing the pulsed Doppler range gate within the vessel at this point ( Fig. 15-2A ). The spectral waveform from the normal uteroplacental system is unidirectional, of low pulsatility, and demonstrates frequencies throughout the cardiac cycle ( Fig. 15-2B ). This is a result of the trophoblastic invasion of the spiral arteries; end-diastolic frequencies increase to a maximum at 24–26 weeks of gestation (see Fig. 15-7 ).
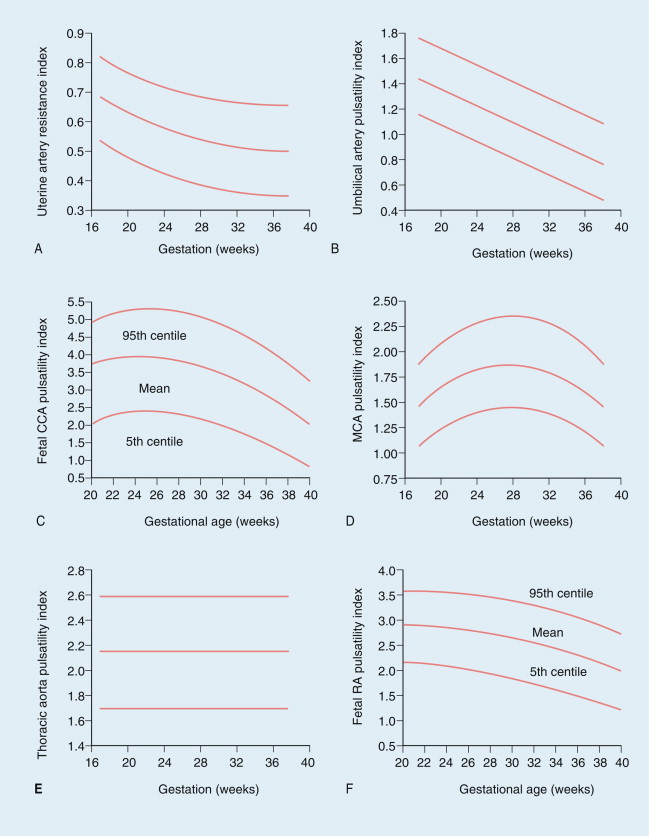
It is possible to calculate several indices to quantify blood flow; however, the most commonly used in the uterine artery is the resistance index (RI) (see Fig. 15-7A ). After 26 weeks of gestation the normal range of the resistance index is between 0.45 and 0.58. Decreased end-diastolic flow with a consequently raised resistance index above 0.58 is considered abnormal, as is a notch in early diastole in either uterine artery, suggesting failure of trophoblastic invasion of the spiral arteries ( Fig.15-3 ). ,
A comparative histological study of third-trimester placental biopsy at caesarean section has demonstrated that the uterine artery flow impedance reflects impaired trophoblast migration. Nonetheless, there are a number of reasons for caution. Impedance to flow varies throughout the uteroplacental circulation, with the lowest value seen in the arcuate vessels on the placental side of the uterus and the highest value seen in the uterine arteries on the non-placental side of the uterus. The physiological variations and anatomical complexities of the uteroplacental vascular tree make it difficult to obtain accurate and reproducible measurements using continuous wave Doppler, with interobserver variations ranging from 3.9 to 17%. , In later pregnancy, between 37 and 40 weeks, maternal position may also alter flow patterns, with the umbilical artery resistance being higher in the supine position than in the decubitus. Furthermore, variations in uterine activity ( Fig. 15-4 ), maternal heart rate and exercise also significantly alter the waveform. , The examination should therefore be performed with the mother resting and only during a period of uterine inactivity. The effect of exercise is more marked in complicated pregnancies, but there are no data evaluating the effect of exercise to improve sensitivity or specificity of Doppler in predicting fetal outcome. The time of day, or recent eating by the mother do not appear to have an effect on the uterine artery flow. , Most of the antihypertensive drugs appear to have no effect on fetomaternal blood flow. However, nifedipine appears to produce a reduction in umbilical artery resistance, and this has therefore been suggested as a better drug to use during pregnancy. The effect of smoking on blood flow has been somewhat controversial with researchers reporting either no effect or a significant effect from smoking a cigarette. , However, because of the dispute and the potential for cigarette smoking to alter flow patterns in chronic smokers, this author advocates that patients should not smoke for at least 1 hour prior to a Doppler study.
Although superficially attractive, the use of uterine artery Doppler, even in primiparous mothers where the risk of hypertensive complications is greater, is neither sensitive nor specific in the detection of pre-eclampsia, or small-for-gestational-age infants. This is typical for results seen in low- and moderate-risk pregnancies. The routine use of uterine artery Doppler studies to screen low-risk populations for subsequent development of pre-eclampsia and intrauterine growth retardation (IUGR) has a poor positive predictive value. Furthermore, screening can only be useful if there is an intervention available which will improve the outcome, and treatment options for both conditions are limited with, currently, no proven interventions to prevent either pre-eclampsia or IUGR. Therefore, in low-risk populations, using uterine artery Doppler studies as a screening tool is not recommended by national authorities, such as the National Institute for Health and Clinical Excellence (NICE) in England and Wales.
However, in a high-risk population, the presence of abnormalities in the uterine artery studies beyond 24 weeks of gestation may indicate the need for more intensive maternal and fetal surveillance to allow early identification of IUGR or pre-eclamptic toxaemia. This screening technique could potentially be used to rationalise patient care pathways dependent upon their uterine artery Doppler studies.
Uterine artery Doppler appears to be of significantly greater utility when there is pre-existing maternal disease. In chronic renal disease, for example, an abnormal artery waveform predicts pre-eclampsia and IUGR with a high degree of accuracy. Only 8% of patients with negative Doppler findings in one study developed complications of pregnancy. By contrast, although the resistance index is increased in the uterine arteries of diabetics with a morphological vasculopathy, there is no relationship with short- or long-term diabetic control and it is not a good predictor of diabetes-related fetal morbidity; presumably because these changes are reflecting the risk of acidosis as a result of hypoxia rather than metabolic acidosis. , In patients with pre-existing, essential hypertension, uterine artery Doppler appears to be useful in defining groups of patients who are at risk of developing complications. If the systolic blood pressure is greater than 140 mmHg, then resistance indices in both uterine arteries is increased. If the systolic blood pressure is less than 140 mmHg, three separate groups may be identified: those with (a) bilateral or (b) unilateral abnormalities of the waveform within the uterine arteries; and (c) those with an entirely normal uterine artery flow. The prognosis appears to be related to the degree of abnormality of uterine artery flow. In systemic lupus erythematosus, one study suggests that an abnormal uterine artery Doppler will identify all those pregnancies with an adverse outcome.
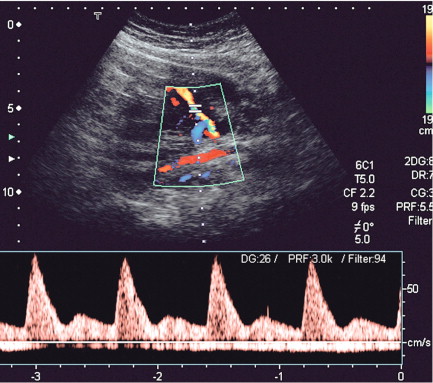
The placenta rather than the lungs is the organ of gaseous exchange in the fetus. Two umbilical arteries convey deoxygenated blood from the fetus to the placenta, and one umbilical vein returns oxygenated blood from the placenta to the fetal inferior vena cava. The umbilical arteries take origin from the fetal internal iliac arteries coursing alongside the lateral walls of the bladder in the urachus to the umbilical insertion. The umbilical vein courses posteriorly and cephalad in the falciform ligament to join the left branch of the portal vein. The oxygenated blood is then shunted through the liver to the inferior vena cava by the ductus venosus. Colour Doppler confers some advantages in the evaluation of the umbilical artery over duplex Doppler alone. Identification of a free loop of umbilical cord and the umbilical artery on colour Doppler allows unambiguous sampling of the correct vessel at the most appropriate angle to get the best waveform. Spectral waveforms are obtained by placing the pulsed Doppler range gate within the vessel. Research studies correlating abnormal umbilical artery Doppler findings to prenatal outcome relate to sampling of a free loop of umbilical cord. In clinical use, Doppler waveforms must therefore be recorded from a free loop of the cord. However in situations where there is oligohydramnios, and particularly in twin pregnancies with a ‘stuck twin’, sampling flow from the umbilical arteries within the fetal abdomen as they course alongside the bladder may be the only option to achieve satisfactory Doppler signals ( Fig 15-5 ).
Doppler waveforms within the umbilical artery change with gestational age in a similar fashion to those of the uterine artery ( Fig. 15-6 ). Resistance and pulsatility indices demonstrate a gradual reduction with increase in gestational age. Normal values of the pulsatility index are shown in Figure 15.7 .
Variations in fetal heart rate and the presence of fetal breathing movement may significantly alter the arterial waveforms, although within the physiological range of 120–160 beats per minute it is not necessary to correct indices for fetal heart rate. Nonetheless, it is important to examine umbilical artery waveforms during a period of fetal inactivity and in the absence of fetal breathing; duplex and colour Doppler ultrasound are of value in enabling the waveform to be sampled rapidly and accurately. Measurement of three consecutive cardiac cycles reduces the coefficient of variation of measurements to less than 5%.
All Doppler devices have inherent filtration which removes low-frequency noise and vessel wall movement artefact. On most current machines the high-pass filter can be varied, but it is important not to set this higher than 100 Hz and preferably lower than 50 Hz, if a false impression of absent diastolic flow is not to be created.
(See Tables 15-1–15-3 .)
| Uterine artery | Umbilical artery | Middle cerebral artery |
|---|---|---|
| High risk screening | Intrauterine growth retardation | Intrauterine growth retardation |
| Pre-existing disease, e.g. renal disease, systemic lupus erythematosus | Post dates | Fetal anaemia |
| Previous IUGR | Fetal abnormality | |
| Trophoblastic disease |
| Uterine artery | Umbilical artery | Middle cerebral artery |
|---|---|---|
| Raised indices | Raised indices | Decreased indices |
| Notch | Absent end-diastolic flow | Raised maximum velocities |
| Reversed end-diastolic flow |
| Uterine artery | Umbilical artery | Middle cerebral artery |
|---|---|---|
| Pre-existing disease | Fetal activity | Direct cerebral compression |
| Exercise | Breathing | |
| Uterine activity | Cord compression | |
| Antihypertensives ?Cigarettes |
?Cigarettes |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here