Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
2.1 , , and
Visit Expert Consult ( expertconsult.inkling.com ) for videos on topics discussed throughout the text.
Expertise in oculoplastic and orbital surgery starts with anatomy. Learning anatomy can be very difficult—remembering it is even harder. It is easy to get bogged down in the details before you know why a particular anatomic feature is important in taking care of your patients. One way to learn anatomy is to understand how the anatomy makes the normal tissues function (e.g., a certain amount of horizontal tension or “tightness” is required to hold the normal lower eyelid up against the eyeball). The next step is to understand how an anatomic and functional abnormality may be related to a clinical problem (e.g., with age, the canthal tendons lengthen, which causes the normal lower eyelid tension to be lost, allowing eversion, or ectropion, of the lower eyelid). It is not difficult to move to the final step: understanding how to repair the anatomic abnormality and restore the function (e.g., tightening the lower eyelid by removing some of the redundant tendon shortens the lax lower eyelid to correct the ectropion). These clinical anatomic correlations are not just useful teaching tools—they are the basis for most reconstructive procedures. A real understanding of anatomy comes when you start to apply what you have read to the case on which you are working. This is one of the fun parts of operating ( Box 2.1 ).
Understand how the anatomy makes the normal tissues function.
Understand how an anatomic and functional abnormality is related to a clinical problem.
Understand how to repair the anatomic abnormality and restore the function.
Your real understanding comes when you apply what you have learned in books to the operation you are doing.
Throughout this chapter and in the remainder of the book, the anatomy is applied to the clinical problem, and vice versa. Periocular and orbital anatomy is complex. There are many levels of understanding of anatomy, some of which cannot be achieved without seeing the structures in the “living flesh” and actually performing the surgery. While reading this chapter, try to get the big picture. Understand the principles. There is a tremendous amount of information here, and if you are a beginner and unfamiliar with periocular anatomy and clinical oculoplastic surgery, it can be overwhelming. I have read over this chapter more than 30 times in preparation for the final text, and I am overwhelmed myself at the amount of material. In fact, this is the longest chapter in the book. Please scan the chapter a few times before diving in deeper for the details. Remember to learn in layers. You continue to discern nuances in anatomy throughout your entire surgical career.
In subsequent chapters, the anatomy pertinent to the clinical problem or procedure being discussed is presented again, so you don’t need to worry about learning it all the first time through. This repetition may be unnecessary for some, but most of us can use it when it comes to remembering anatomy. I expect that by the time you finish this book, this material will seem very easy. Remember, it is the application of the anatomy to the clinical problem that makes you a successful reconstructive surgeon. A photographic memory helps in learning anatomy, but that alone is not enough to get the job done for your patients.
The anatomy covered in this chapter and throughout the book is the essential material that you need to get a good understanding of eyelid, lacrimal, and orbital surgery. Obviously, we cannot cover all of the anatomy in a text like this. I have not discussed ocular anatomy, neuroanatomy, or much of the anatomy related to the extraocular muscles or deep anatomy of the face and neck. There are many good textbooks on periocular, orbital, and head and neck anatomy (see the Suggested Reading at the end of this chapter); please refer to these as necessary. My hope is that the anatomy described here is presented in a way that is useful for learning the principles of oculoplastic and orbital surgery.
This chapter starts with a description of the external features of the periocular area to give a point of reference for the deeper tissues. Rather than discuss the anatomy from anterior to posterior, as is often done, we look at the anatomy from a more functional approach. The orbital bones are covered next, because it is helpful to learn about the soft tissues relative to the bones. Most of the eyelid and orbital tissues either attach to or pass through openings in the orbital skeleton. Next, the muscles that close the eyes are discussed, followed by a section on the muscles that open the eyes. After that, the nerves, vessels, and lymphatics are covered. Lastly, the support system of the facial tissues is explored. These principles will become important as your surgical adventures move out of the orbit and lids into the periocular and facial regions. We use the clinical examples as a way to learn the anatomy. In the chapters that follow, we spend more time on the clinical problems themselves. The video for this chapter offers a tour of some of the surgical anatomy that you will see in your daily practice. It gives you a taste of what is to come!
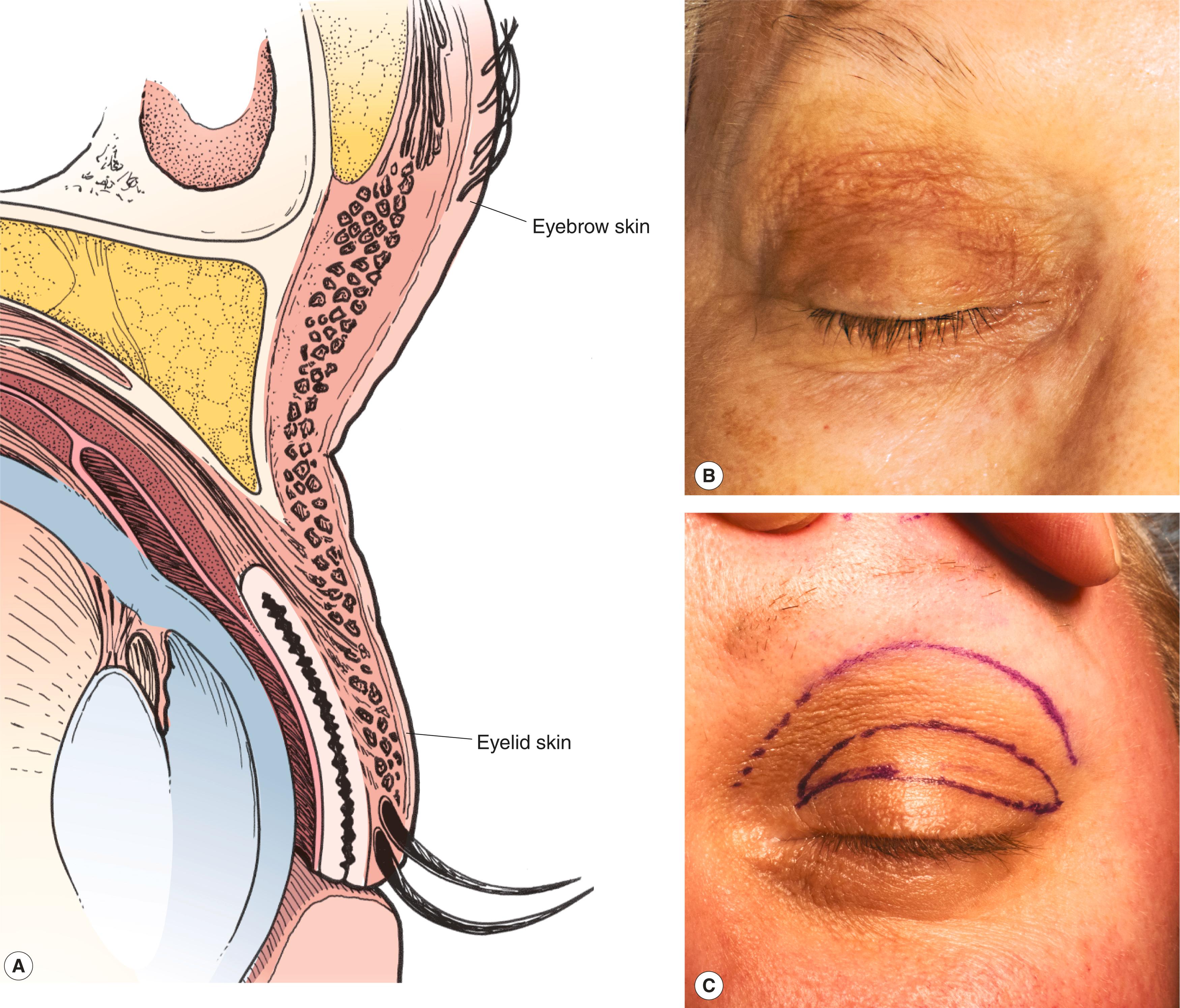
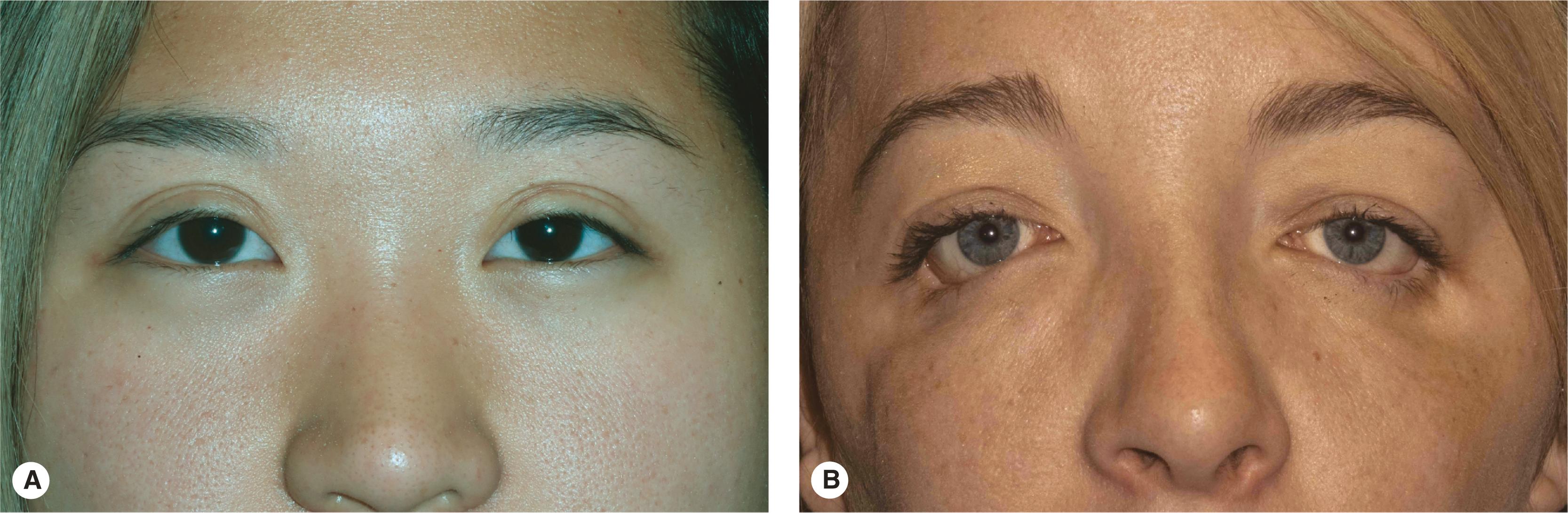
Several lines on the skin serve to anatomically define the periocular and facial anatomy. The upper eyelid skin crease separates the upper eyelid skin fold from the flat pretarsal component of the upper eyelid ( Figure 2.1 ). The upper eyelid crease is an anatomic landmark that is commonly referred to in oculoplastic surgery. Incisions hidden in this crease for upper eyelid ptosis repair or blepharoplasty and other procedures are among the most common incisions used in oculoplastic surgery.
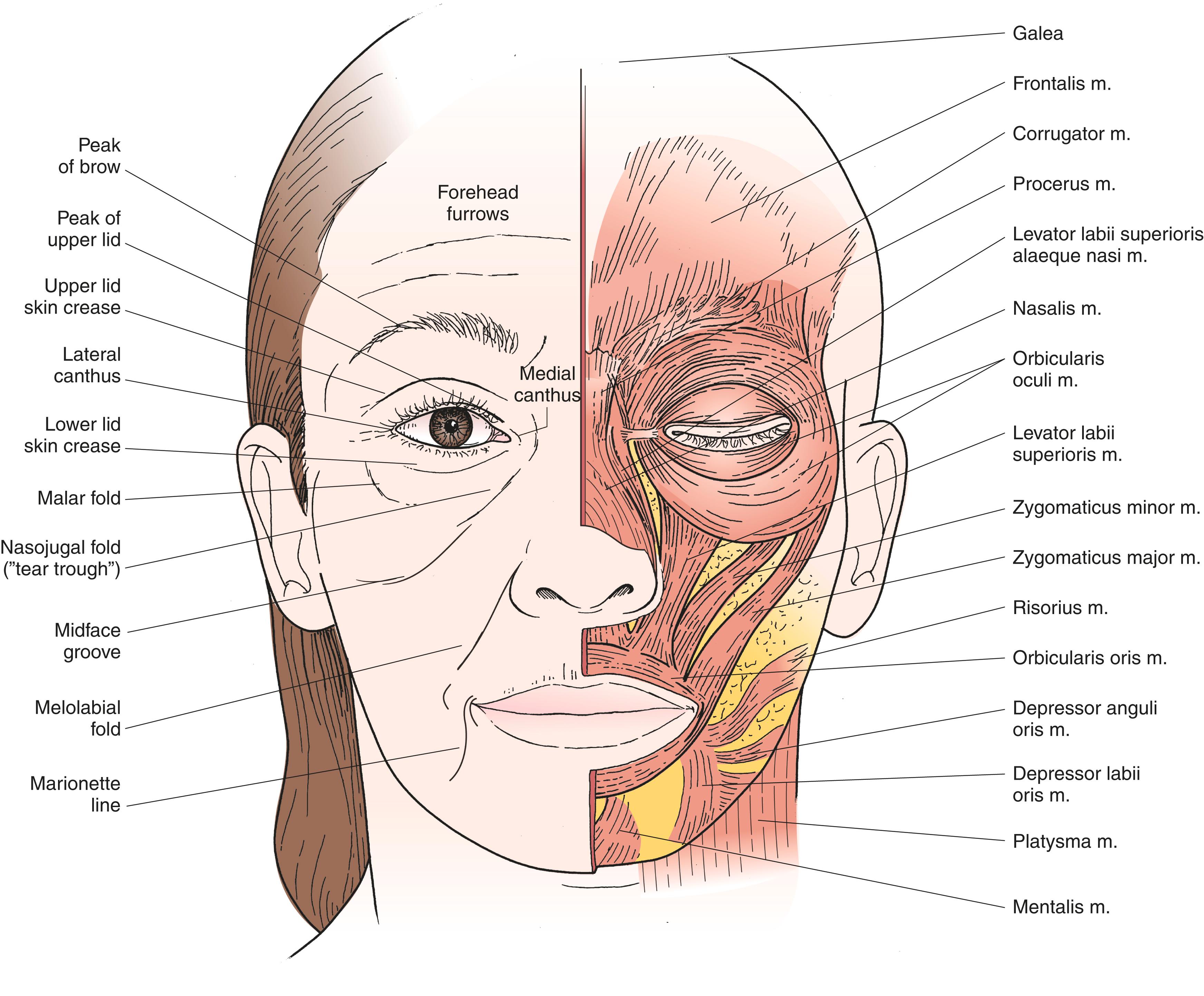
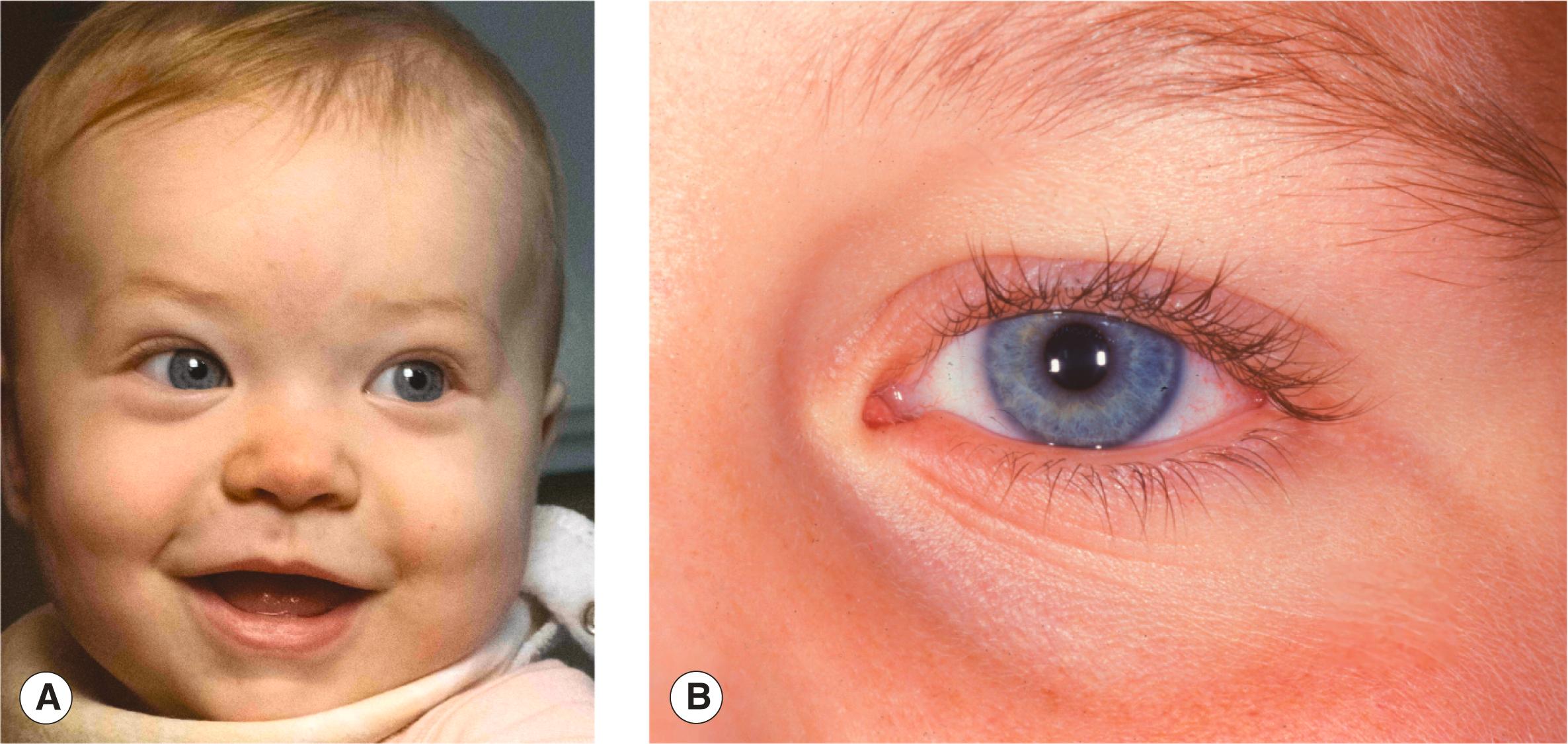
The eyelid skin above and below the crease is the thinnest in the body. The skin must be thin to allow for the spontaneous quick blinking movements of the eyelids. A lower eyelid crease is common in children ( Figure 2.2 ) but is usually not visible in adults. The eyelid skin becomes thicker as you move further away from the eyelid margins toward the brow and cheek. The nasojugal and malar folds separate the thin lower eyelid skin from the thicker skin of the cheek. In younger patients, the inferior orbital rim contour is not visible or easily palpable. With age, the malar fat pad (and the deeper suborbicularis oculi fat [SOOF]) descends and deflates and the rim becomes more noticeable, both visually and by palpation (compare some of your 20-year-old patients with your 50-year-old patients in this regard). As the nasojugal fold becomes deeper it is often termed the tear trough . Thinner patients show more “hills and valleys.” As thinner patients age, a hollow diagonal furrow or groove forms, separating the malar fat from the nasolabial fold (the midface groove). These “valleys” correspond to areas where the soft tissues are more tightly bound down to the underlying facial soft tissue or bone. In this case, the tethering is by the zygomatic cutaneous ligaments, or the connective tissue that more tightly attaches the skin to the underlying muscle here than at the surrounding areas; this causes the hollow that forms. The melolabial fold extends inferolaterally from the ala of the nose to the corner of the mouth. Subtle facial asymmetry resulting from paralysis of the facial nerve is often evident in the melolabial fold, where the fold is softer or absent. This fold is also known as the nasolabial fold . A hollow or line develops from the corners of the mouth, slanting laterally to the mandible, and is known as the marionette line . Associated with the development of marionette lines, you see jowling of the cheek posterior to the marionette line. As these tissues descend, the smooth mandibular border that is associated with youth is lost.
As you learn the anatomy of the face, you start to become aware of what makes your patients look “old.” The youthful face has long, smooth contours with graceful transitions from one area to the other. For example, the cheek and lower eyelid blend together without an obvious division. The landmarks that we have been discussing appear with age, separating the anatomic areas of the face in hills and valleys belying the patient’s age. Later in the book, you learn techniques using Botox, filler, and surgery that push the clock back a bit, re-creating those smoother contours of youth.
Skin creases ( rhytids or wrinkles ) form as a result of the movement of the underlying muscles of facial expression. The most familiar of these creases are the “crow’s feet” arising at the lateral canthus caused by contraction of the orbicularis muscle. The direction of these wrinkles can be predicted by recognizing that they always form perpendicular to the underlying muscle fibers (see Figure 2.1 and also see Figure 2.16 ). This explains the radial orientation of the crow’s feet lines to the circular orientation of the orbicularis muscle. Other prominent creases caused by underlying muscle contraction include the horizontal forehead furrows (from the frontalis muscle). The horizontal and diagonal lines of the glabella are caused by the contraction of the procerus and corrugator muscles, respectively. These lines suggest redundancy in the tissue perpendicular to the lines. That redundancy represents lax tissue that is “tightened” to reverse aging changes. The same redundancy is what you are looking for when you are trying to close a tissue defect after excision of a facial skin cancer. You also learn to hide incisions in these creases so that the resulting scar is not easily seen. We will discuss how Botox and other neuromodulators can be used to improve facial wrinkles by relaxing the underlying muscles.
The brows, technically a part of the scalp, are divided into three anatomic parts:
Head
Body
Tail
The orientation of the brow hairs varies in each part of the brow. The brow hairs in the head of the brow tend to be vertical. As you move toward the tail of the brow, notice that the hairs tend to lie flatter or slightly downward. It has been suggested that incisions made within the brow hairs should be oriented parallel to the shafts of the hairs to minimize the number of follicles damaged. This seems reasonable but makes closure of the wound more difficult.
The eyebrows are an important feature of an individual’s facial appearance and are primary indicators of facial expression and mood ( Figure 2.3 ). Many texts include variations of this “happy face” eyebrow model. If you look at your friends’ brows carefully, you see, and are impressed by, how the slope, shape, and position of the eyebrows give you an immediate impression of mood. Lifting a drooping tail of the brow makes a melancholic-appearing patient look happier. We see this later in Chapter 6 .
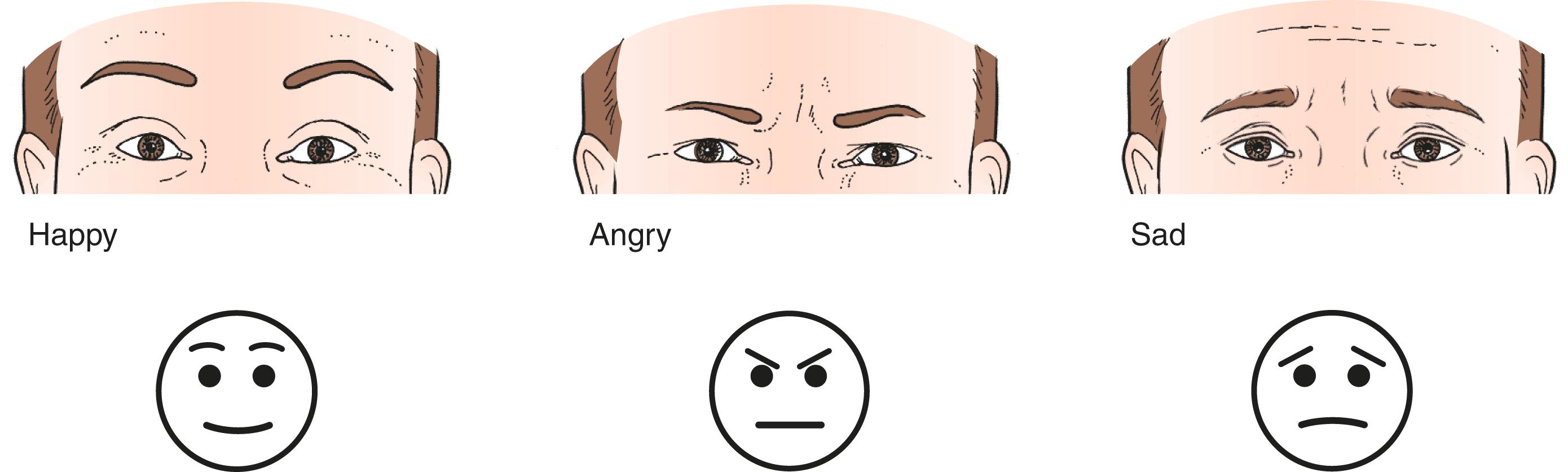
The male and female brows differ in shape and position ( Figure 2.4 ). The normal male brow is flat and full in contrast to the thinner and more arched female brow. The superior margin of brow hairs is “feathered” in men and smooth in women. The male brow sits squarely at the superior orbital rim. The female brow is typically arched, with the highest point being above the lateral canthus or slightly more medial to it. The position of the female brow is well above the rim, especially temporally, where the superior lateral part of the bony rim contour is visible and easily palpable. The male rim is generally more prominent than the female rim because of a larger frontal sinus. The male brow tends to encroach upon the otherwise hairless glabella between the brows.
The features of the brow are secondary sexual characteristics that differ in men and women. Women manicure the brows to make the female face more attractive. Epilation of the brow hairs accents differences between male and female brows in thickness, smooth margins, arched contour, and position. Although the shape and position of the brow change somewhat with the current fashion, I suspect we all have the same image of male and female movie supermodel eyebrows. With age, the appearance of the brow changes also. The normally high arch of the young woman is lost as the brow tends to droop temporally. A ptosis of the brow accentuates the upper eyelid skin fold and fills in the deep superior sulcus of the upper eyelid seen in younger patients. Lifting a drooping eyebrow always improves the appearance of a cosmetic blepharoplasty. With a severe brow ptosis, as in facial nerve palsy, the superior visual field is obstructed. Lifting the brow helps to restore the visual field. Your appreciation of the eyebrow anatomy is important for you to perform cosmetic or reconstructive surgery of the face.
Identify in your mind or on a patient the following features:
Upper eyelid skin crease and skin fold
Lower eyelid skin crease
Thin and thick eyelid skin
Nasojugal fold (tear trough)
Malar fold
Midface groove
Melolabial fold (nasolabial fold)
Marionette lines
Each eyebrow is divided into three parts. What are these parts? Remind yourself of the differences between male and female eyebrows.
The function of the eyelids is to protect the eyes and distribute the tears. It is important for you to understand the normal anatomy of the eyelids and to recognize conditions that may prevent normal function.
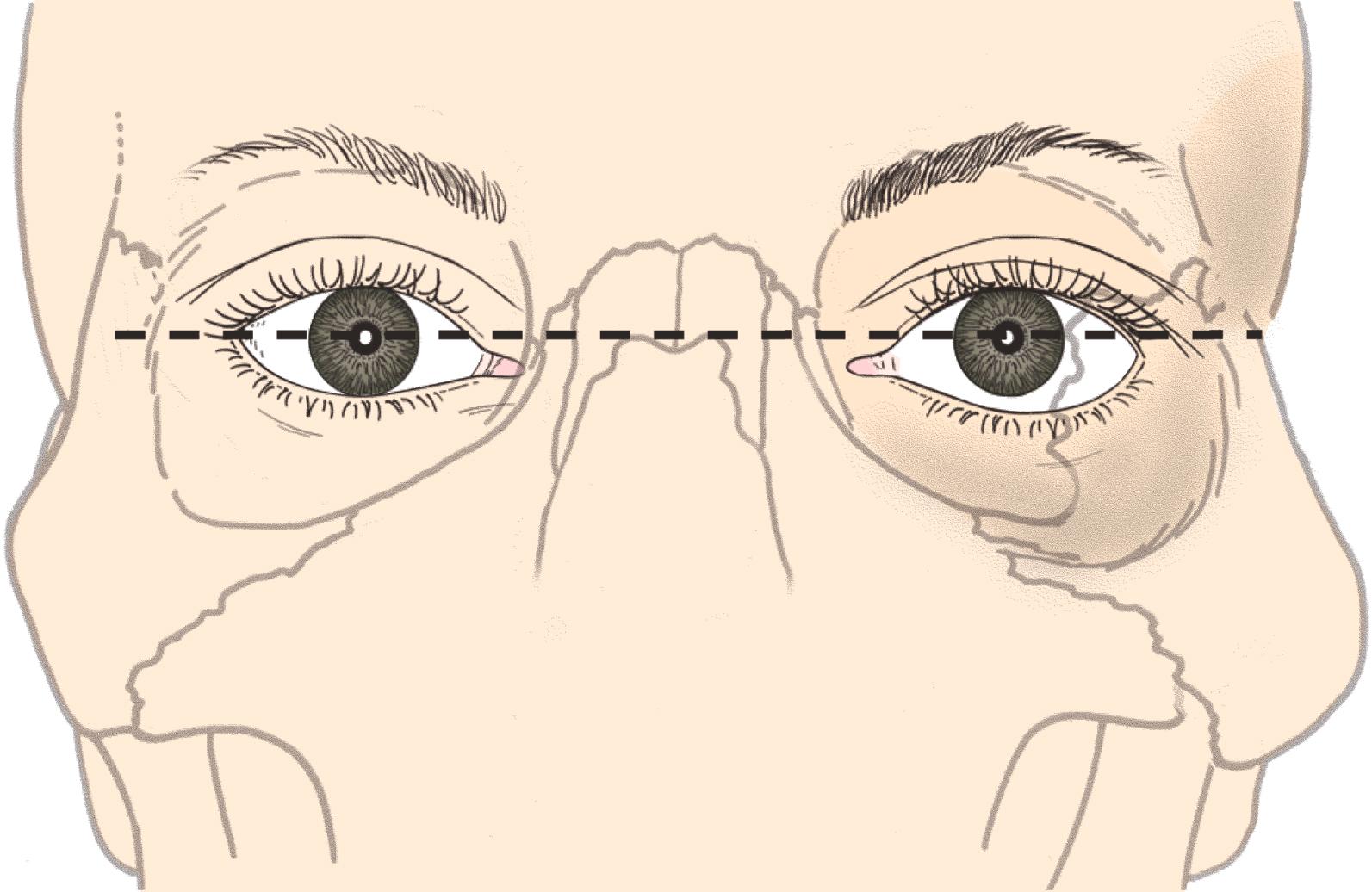
The lateral canthus is usually slightly higher than the medial canthus, although the slope of the eyelid fissures can vary widely among individuals (see Figure 2.1 ). The upper lid contour is more arched than that of the lower lid. The peak of the upper lid is just nasal to the pupil. The lowest point of the lower eyelid is below the lateral limbus. The normal contour of the eyelid must be re-created in a variety of procedures, including ptosis repair and reconstruction of the lateral canthal angle.
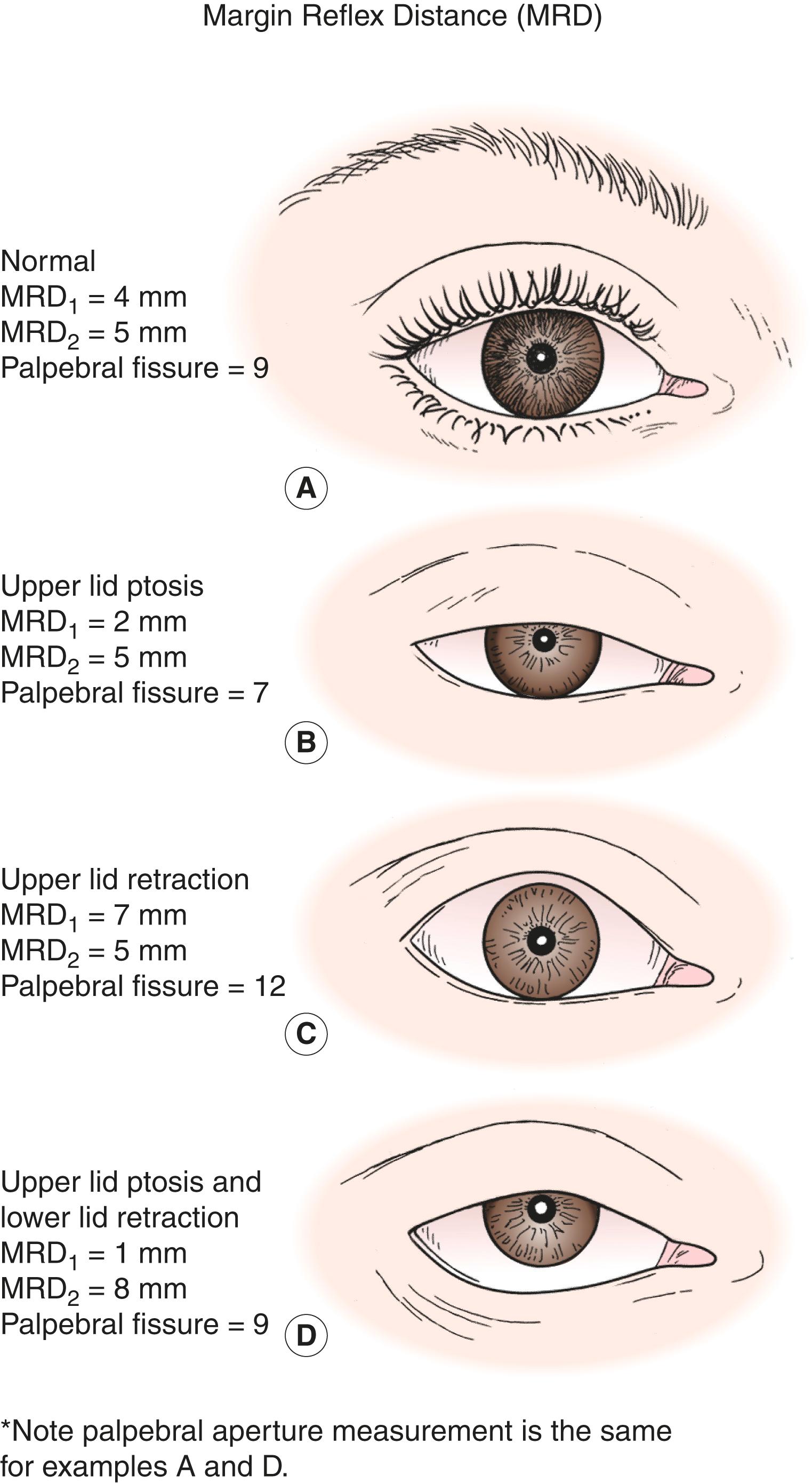
The horizontal length of the eyelids is 30 mm. The distance between the upper and lower eyelids, the palpebral aperture or fissure , is about 10 mm. A useful way to measure the position of the upper and lower eyelids is the margin reflex distance . This distance is the number of millimeters from the corneal light reflex to the lid margin. The upper lid margin reflex distance (MRD 1 ) usually measures 4 to 5 mm. That means that the upper lid margin rests slightly below the limbus. The lower lid rests at the lower limbus, making the lower lid margin reflex distance (MRD 2 ) 5 mm ( Figure 2.5 ). These distances can be measured with a ruler or estimated. When you estimate the distance, keep in mind that midway between the corneal light reflex and the limbus is 2.5 mm. The eyelid aperture measurements, especially the MRDs, are an essential part of the eyelid examination and one of the eyelid vital signs . A drooping upper eyelid is known as ptosis or blepharoptosis. An upper eyelid resting above the upper limbus or a lower eyelid resting below the lower limbus is said to have lid retraction . The white between the limbus and the lid is known as scleral show .
The eyelid skin is the thinnest in the body, allowing rapid eyelid blinks ( Figure 2.6 ). There is no subcutaneous fat in the eyelid. Superiorly the eyelid skin thickens to become eyebrow skin. As part of the eyelid examination you should measure the amount of eyelid skin present. When performing a blepharoplasty to remove excess eyelid skin, it is necessary to leave enough of the thin eyelid skin to allow quick passive blinks. Many (actually most) older patients have a sagging brow contributing to the appearance of a droopy brow. In these patients, an eyebrow lift (browplasty) is an important addition to the skin removal (blepharoplasty) (more on this in later chapters). Worth noting now is that the complaint of “droopy eyelids” can be the result of eyelid ptosis, redundant eyelid skin, or a sagging eyebrow, or a combination of these.
There are three or four rows of eyelashes along the upper lid margin and one or two rows of eyelashes along the lower lid margin. The eyelashes extend from just lateral to the puncta to the lateral canthus. Misdirection of the eyelashes against the eye, also known as trichiasis , causes a foreign body sensation. In some cases, trichiasis can cause severe corneal problems. Treatment is focused at redirecting or eliminating the eyelashes.
The eyelids attach to the orbital bones via the medial and lateral canthal tendons . The tendons attach to the tarsal plates , which are the fibrous skeleton of the eyelids. A favorite board examination question asks if the tarsal plates are made of cartilage (which they are not; they are made of fibrous tissue). The upper lid tarsal plate is about 10 mm high, corresponding with the skin crease height. The lower lid tarsal plate is about 4 to 6 mm high. Within the tarsal plates are the meibomian glands , modified sebaceous glands that secrete the majority of the oil layer of the tear film. The eyelash follicles originate on the anterior surface of the tarsal plate and exit the eyelid on the margin. The orbicularis muscle is tightly bound to the anterior surface of the tarsus.
At this point, you should have a good understanding of the landmarks of the periorbital area. See if you know the answers to these questions:
What is the definition of the margin reflex distance (MRD)?
What are the normal values for MRD 1 and MRD 2 ?
Where is the peak of the upper eyelid?
Where is the lowest point of the lower eyelid?
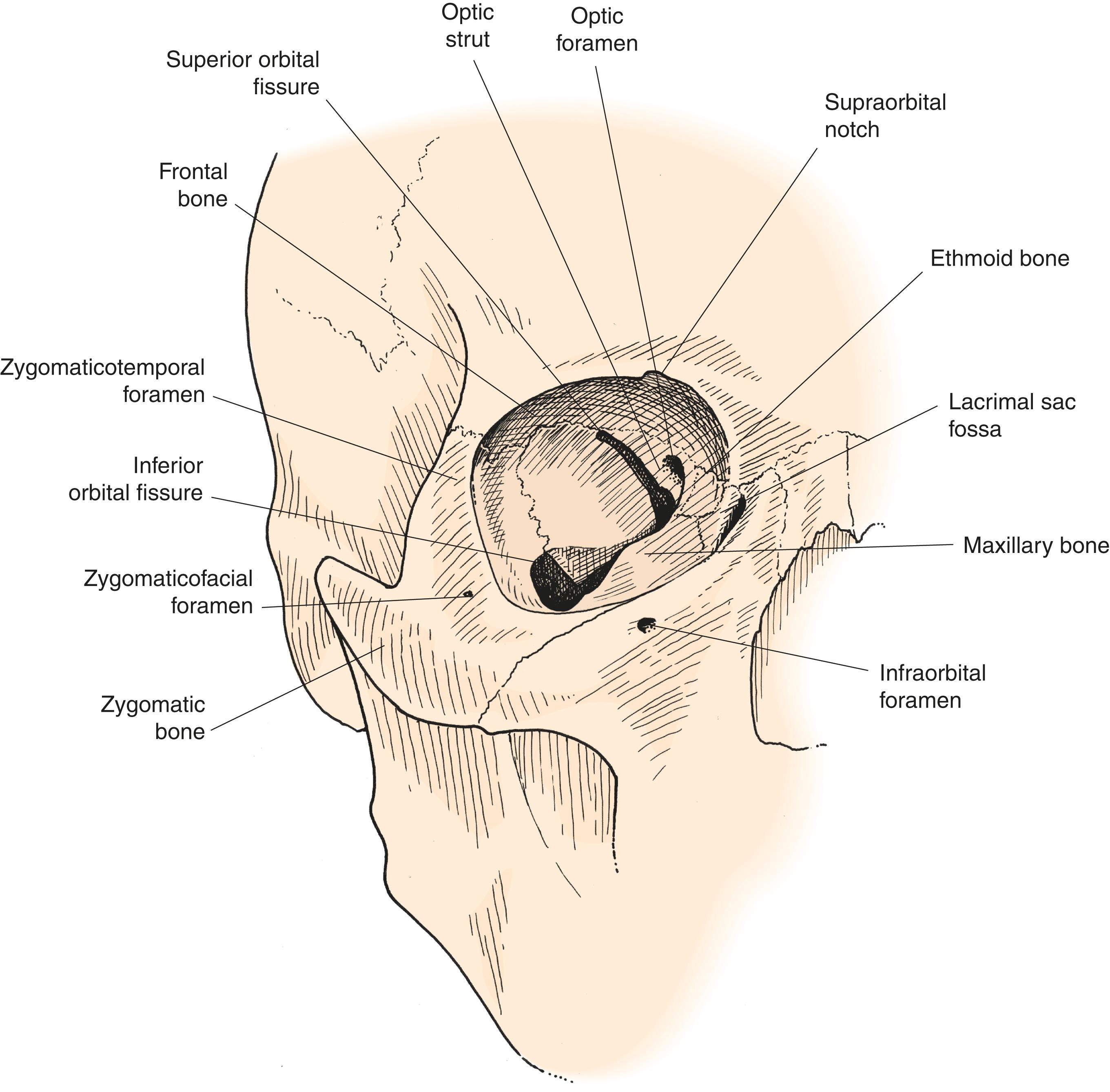
Let’s move from the superficial anatomy to the deep anatomy, the orbital bones. The orbit is made of a strong bony rim and relatively weak orbital walls . Several openings, foramina , into and out of the orbit allow the passage of the veins, arteries, and nerves that supply the orbital tissues. The orbital rims, walls, and foramen are discussed in the paragraphs below.
The orbital rim provides protection for the eye without compromising the visual field. The rim is made of thick, strong bones, especially the superior and lateral rims, where protection from injury is needed most. The superior orbital rim protects the eye from blows from above, as well as sunlight (you rarely see skin cancers on the upper eyelid). The lateral orbital rim curves posteriorly so that there is good peripheral vision at the sides. The inferior rim is posterior enough so that the inferior visual field is not blocked for close work and reading. The orbital rim is made of three bones, the frontal, the zygomatic, and the maxillary ( Figure 2.7 ).
Rarely do the bones of the superior and lateral rims themselves break. More commonly, the suture lines between the bones separate. The most common facial fracture is a zygomaticomaxillary complex fracture ( ZMC fracture ) ( Figure 2.8 ). In this fracture, the zygoma is separated from the other orbital bones at the sutures connecting the zygoma to the rim. Fracture or separation occurs superiorly at the frontozygomatic suture and inferiorly at the zygomaticomaxillary suture . A fracture also occurs along the zygomatic arch posteriorly at the suture line between the temporal bone and zygoma. Because three suture lines are fractured, this type of fracture is also known as a tripod fracture . The bones of the medial and inferior rims are not as strong as the superior and lateral rims. Injury to the medial and inferior rims may cause the bones to fracture in many pieces, a comminuted fracture . The body of the zygoma is very strong and is rarely comminuted.
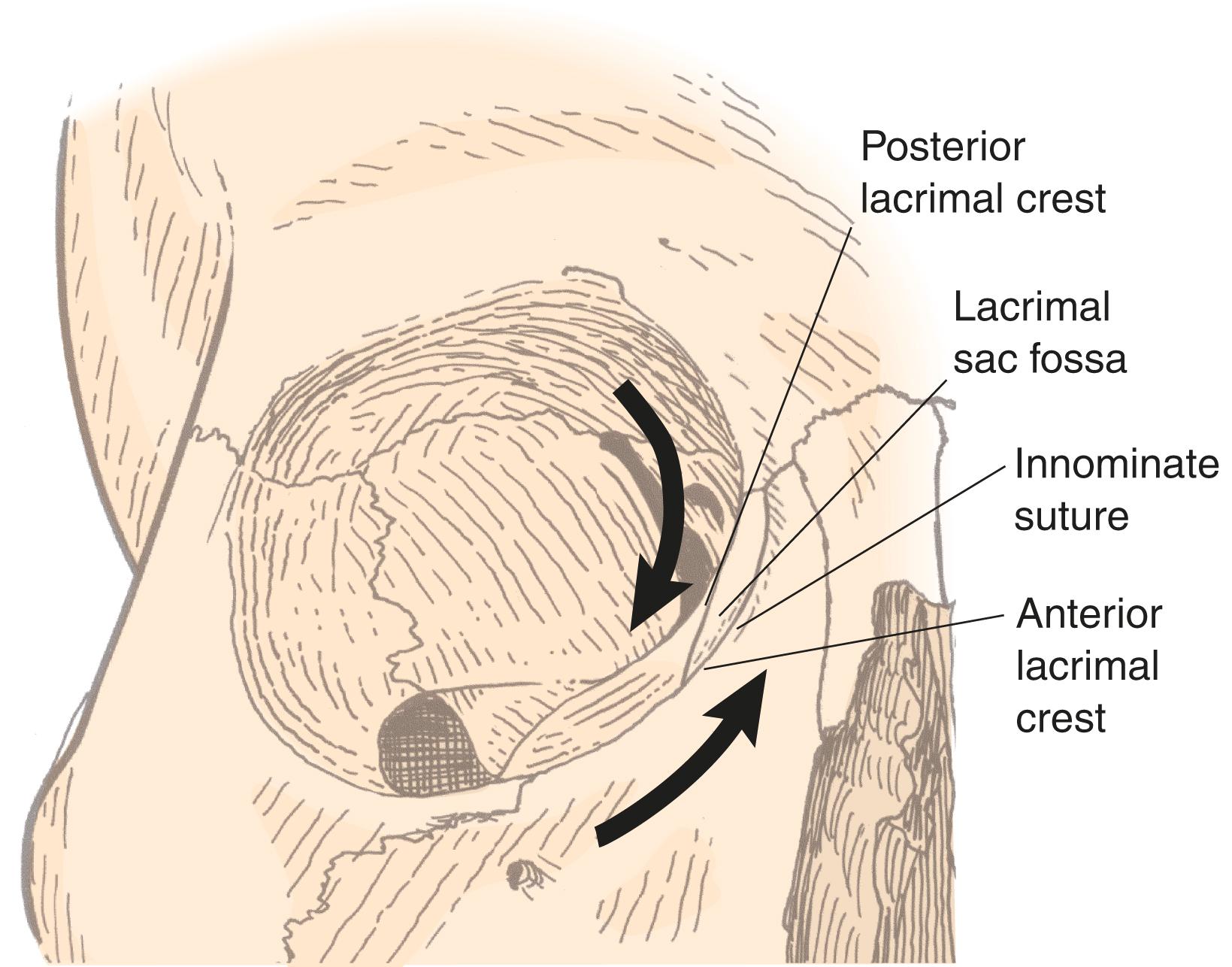
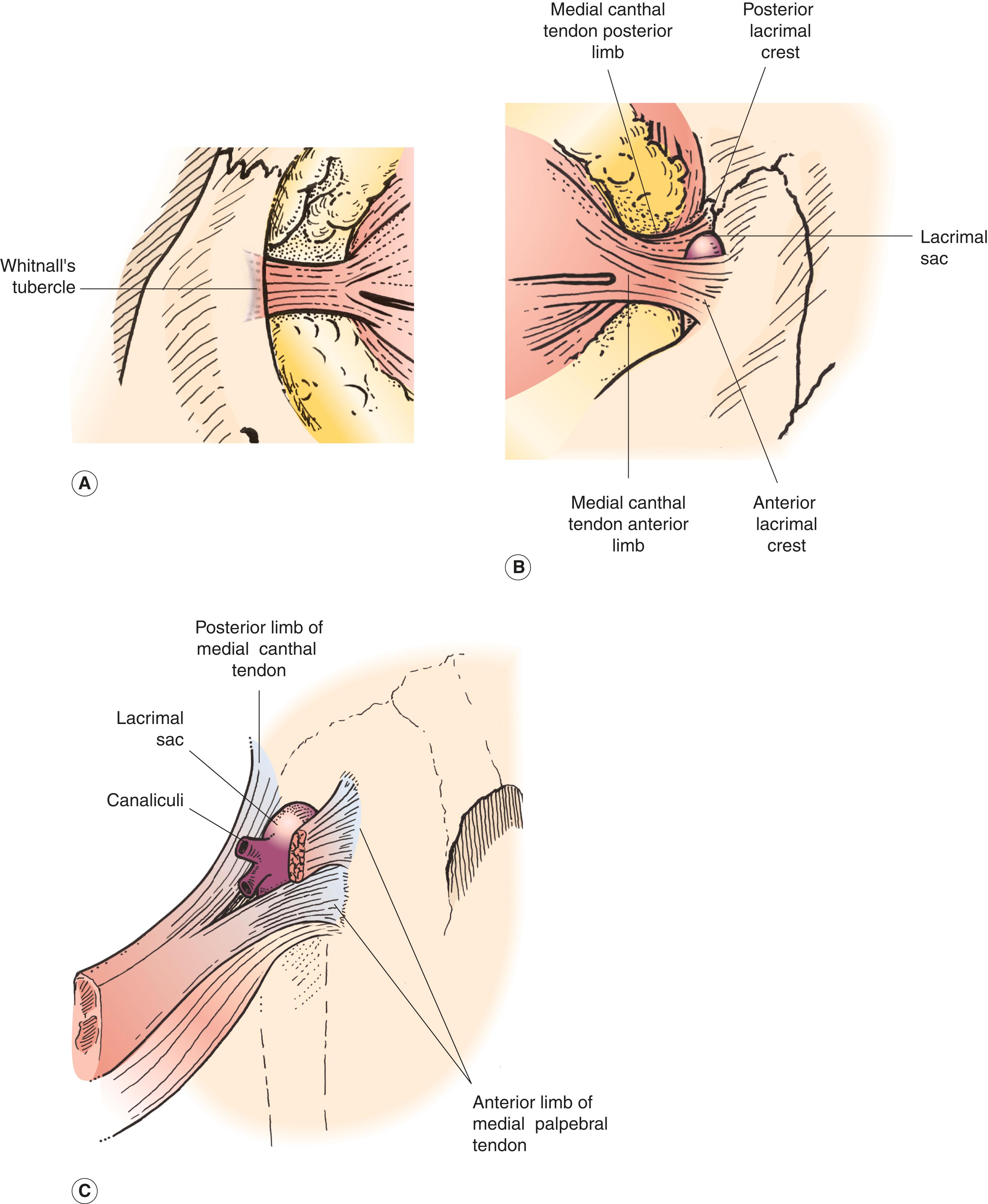
The orbital rims provide the sites for attachment of the medial and lateral canthal tendons. Look at a skull or Figure 2.9 . Follow the inferior and superior rims as they form the medial orbital rim and notice that the paths of the rims diverge. The superior rim moves posteriorly to form the posterior lacrimal crest . The inferior rim moves anteriorly to form the anterior lacrimal crest . The fossa between the two crests is the lacrimal sac fossa , where the lacrimal sac sits. The medial canthal tendon splits into two limbs, the anterior and posterior limbs , which attach to the lacrimal crests, respectively, surrounding the lacrimal sac ( Box 2.2 ).
Superior rim
Frontal bone
Lateral rim
Zygomatic bone
Medial rim
Frontal bone
Maxillary bone
Inferior rim
Zygomatic bone
Maxillary bone
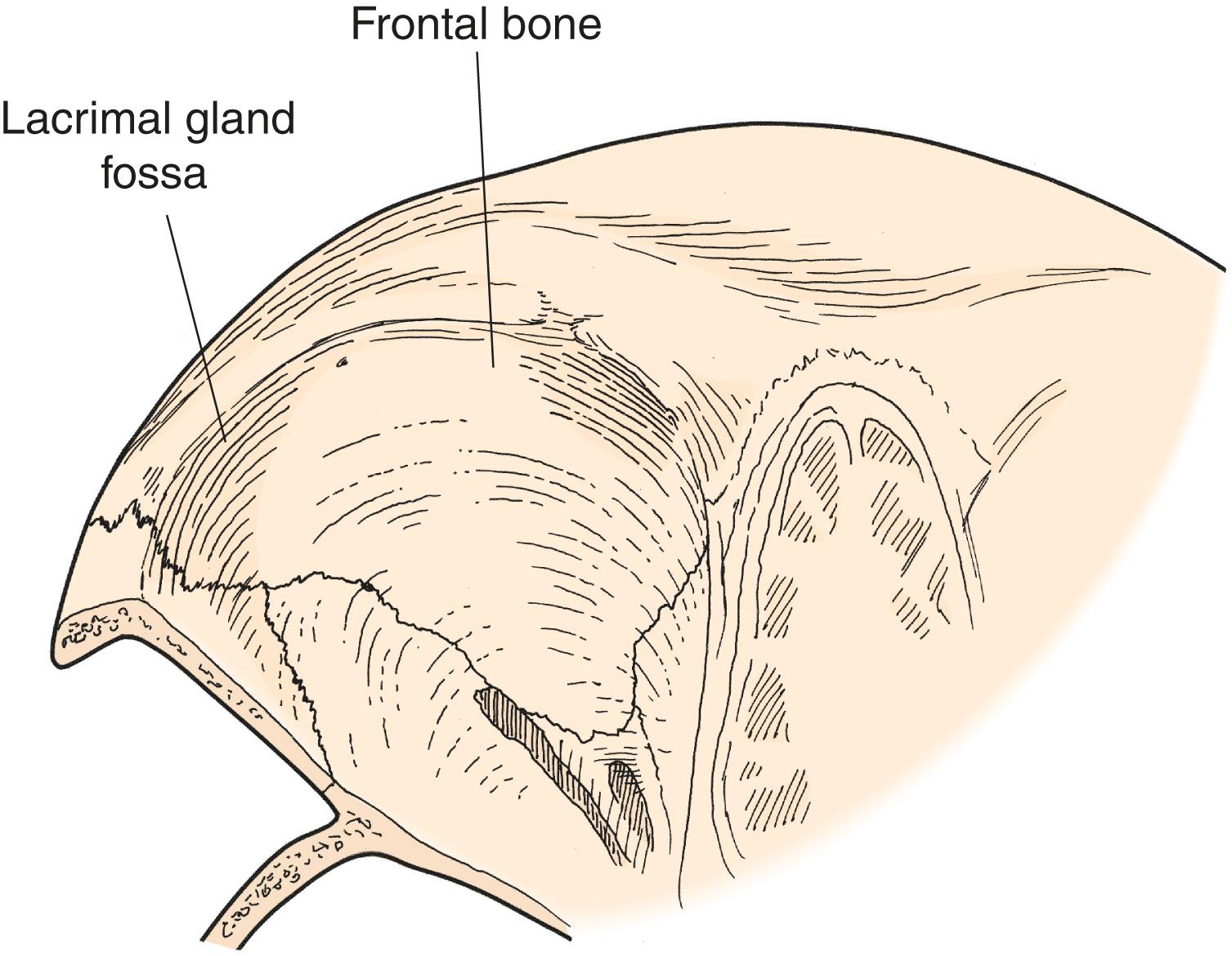
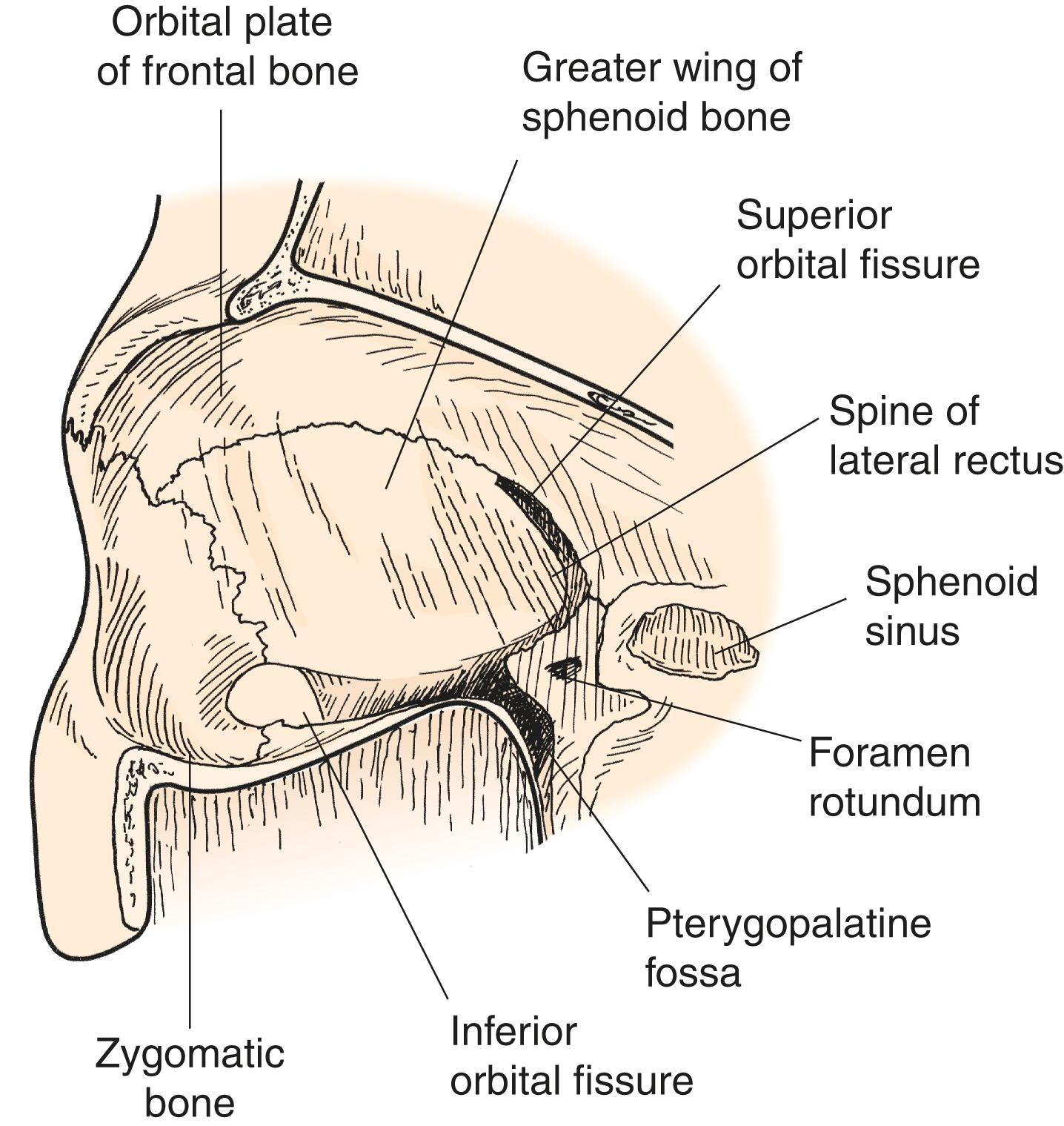
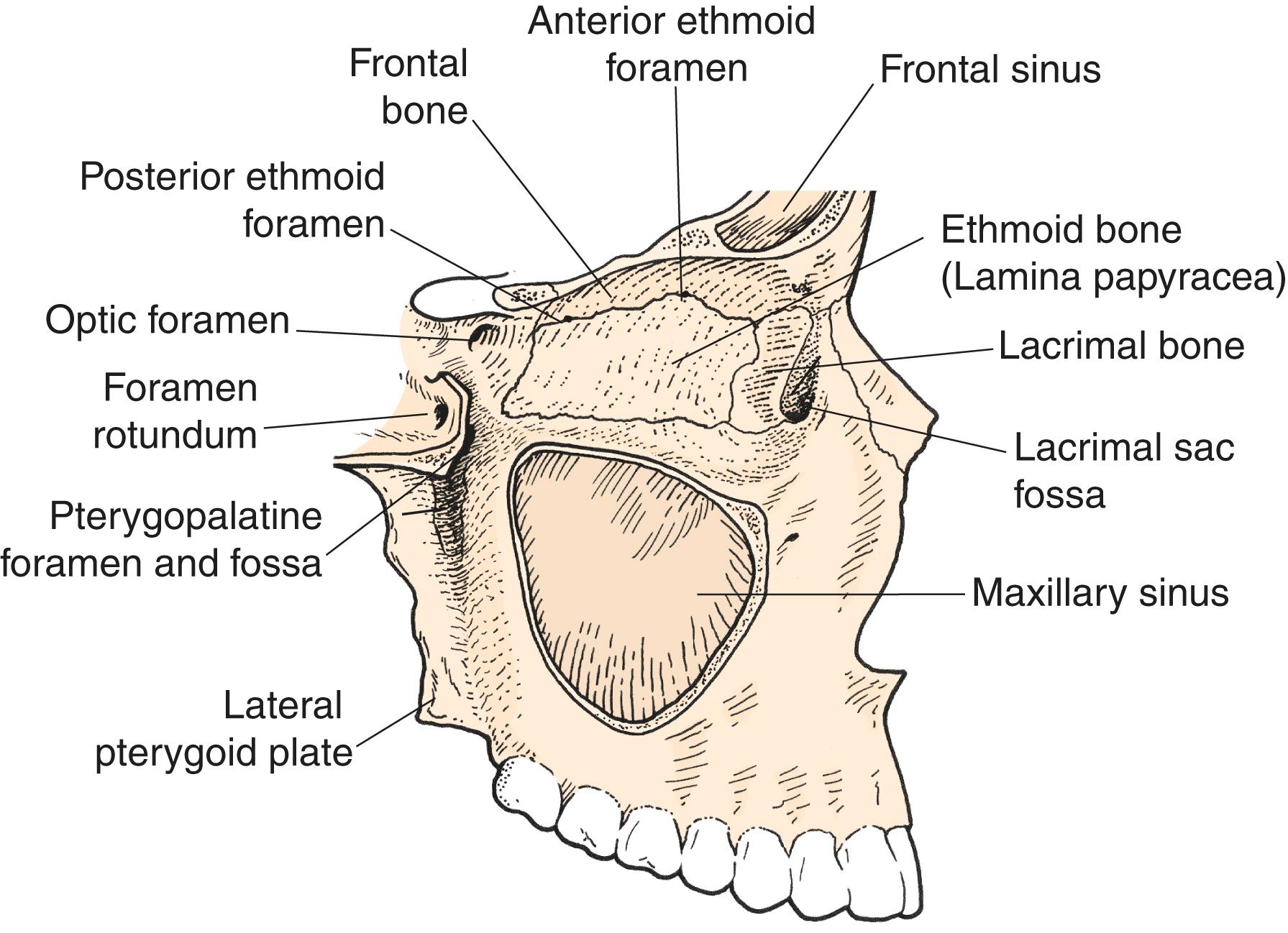
There are four orbital walls. The walls angle posteriorly to form a conical or pyramidal orbit. The orbital roof is concave in contour and forms the floor of the anterior cranial fossa. The concavity of the orbital roof is particularly steep laterally and anteriorly where the lacrimal gland sits in the lacrimal gland fossa. The orbital roof is separated from the lateral orbital wall by the superior orbital fissure ( Figure 2.10 ; see also Figure 2.8 ). The lateral orbital wall ( Figure 2.11 ; see also Figure 2.7 ) is relatively flat on the orbital side, but concave on its exterior surface to accommodate the temporalis muscle. There is a small point of bone along the edge of the superior orbital fissure where the lateral rectus originates; this is the spine of the lateral rectus. The inferior orbital fissure separates the lateral wall from the orbital floor ( Figure 2.12 ). The orbital floor is the roof of the maxillary sinus. The orbital floor slopes upward posteriorly to the apex and medially toward the medial orbital wall. The medial orbital wall is the lateral wall of the ethmoid sinus. Notice that both the medial wall and the floor are normally convex. The anatomic separation of the medial wall and orbital roof is the suture line separating the ethmoid bone and the frontal bone (the frontoethmoid suture) ( Figure 2.13 ). This suture line is easy to see because the anterior and posterior ethmoid arteries and nerves travel through the foramina in the suture line.

A simple way to think of the orbit and the foramen is that of a pyramidal “box.” The inferior orbital fissure separates the lateral wall from the floor. The superior orbital fissure separates the lateral wall from the roof. You can see that the lateral wall extends from the inferior orbital fissure to the superior orbital fissure. At the posterior end of the superior orbital fissure is the optic canal. The roof is separated from the medial wall by the anterior and posterior ethmoidal foramina. The medial wall becomes the floor where the ethmoid sinus meets the maxillary sinus, forming a thick edge of bone known as the strut. (More information about this structure is given when we discuss orbital fractures and orbital decompression surgery for the correction of the proptosis of thyroid eye disease.) Obviously, this is an oversimplification, but it is helpful to me.
In contrast to the thick orbital rims, the orbital floor and medial wall are extremely thin. The medial wall of the orbit is made of mainly the lamina papyracea, or “paper plate,” of the ethmoid bone, so called for its distinctively thin wall. The infraorbital nerve separates the orbital floor into a thin medial portion and a thicker lateral portion. The thin bone of the orbital floor and the medial wall is commonly fractured in trauma. The most common type of orbital fracture seen in ophthalmology is a blowout fracture. This fracture, by definition, does not involve the orbital rim. The classic blowout fracture is caused by a blow to the orbit with an object larger than the orbital diameter, such as a ball or fist. The rims are not fractured, but pressure placed on the orbital contents causes the thin floor or medial wall to “blow out” into the adjacent sinus. Orbital tissue may become incarcerated into the fracture site, causing diplopia as a result of tethering (restriction) of the eye. Fracturing the walls into the adjacent sinus causes the size of the bony orbit to expand, which may lead to enophthalmos (remember that the floor and medial wall are normally convex, bowing into the orbit). Injury to the infraorbital nerve usually accompanies a blowout fracture, causing characteristic numbness of the cheek and upper teeth. I discuss blowout fractures in more detail in Chapter 13 .
Learning the bones of the orbital walls is more complicated than learning those of the orbital rims. Seven bones make up the orbit.
| Roof | Frontal bone |
| Lateral wall | Zygoma anteriorly |
| Sphenoid wing posteriorly (the greater wing) | |
| Floor | Maxilla |
| Medial wall | Ethmoid bone |
| Lacrimal bone (in the lacrimal fossa) | |
| Palatine bone (deep in the apex) |
Some important bony anatomy that we have not mentioned yet covers the orbital apex. I discuss the apex in the next section, which deals with the openings into and out of the orbit.
There are several openings into and out of the orbit ( Table 2.1 ). I like to think about the functions of these openings. What spaces are connected by the openings? Once you know what spaces are connected, it is easier to remember what goes through the openings. The most obvious of these are the superior and inferior orbital fissures. These fissures form a V on the lateral side of each orbit that defines the limits of the lateral orbital wall. The superior orbital fissure separates the roof from the lateral wall, and the inferior orbital fissure separates the floor from the lateral orbital wall. See if you can visualize this (if not, look at Figure 2.7 ). Because the superior orbital fissure connects the orbit to the brain, it must carry cranial nerves to the orbit (cranial nerves III, IV, and VI). The inferior orbital fissure connects the orbit to the infratemporal fossa and the pterygopalatine fossa (behind and around the maxillary sinus—posterior and lateral to the maxillary sinus).
| Opening | From orbit to | Contains |
|---|---|---|
| Superior orbital fissure | Cavernous sinus | Cranial nerves III, IV, and VI |
| Superior ophthalmic vein | ||
| Inferior orbital fissure | Pterygopalatine fossa | Inferior ophthalmic vein |
| Foramen rotundum | Brain | Maxillary nerve (V 2 ) |
| Optic canal | Chiasm | Optic nerve (cranial nerve II) |
| Anterior ethmoidal foramen | Sinus mucosa | Anterior ethmoidal artery, vein, and nerve |
| Posterior ethmoidal foramen | Sinus mucosa | Posterior ethmoidal artery, vein, and nerve |
| Zygomaticotemporal foramen | Superior lateral orbital rim tissues | Nerve, artery, and vein |
| Zygomaticofacial foramen | Inferior lateral orbital rim tissues | Nerve, artery, and vein |
| Bony nasolacrimal duct | Inferior meatus of nose | Membranous nasolacrimal duct |
At the apex of the V formed by the superior and inferior orbital fissures is the infraorbital groove (see Figure 2.12 ). As the groove extends anteriorly along the orbital floor, it gets a bony covering and is known as the infraorbital canal . The canal leaves the orbit at the infraorbital foramen . As you would assume, the infraorbital nerve travels in the infraorbital groove and through the infraorbital canal. The infraorbital nerve is the major sensory nerve of the second division of the trigeminal nerve. Go back to the apex of the V. Follow the infraorbital groove posteriorly and you will be in the pterygopalatine fossa . This fossa, as mentioned earlier, is the space posterior to the maxillary sinus and anterior to the skull base (the bottom of the cranial vault). The second division of the trigeminal nerve (V 2 ) leaves the cranium through the foramen rotundum , entering the pterygopalatine fossa. The nerve then crosses the fossa and enters the orbit via the posterior portion of the inferior orbital fissure, the infraorbital groove.
Let’s talk about the other important opening out of the orbit into the cranium, the optic canal . The optic nerve leaves the orbit via the optic canal to enter the cranial vault . Look at Figure 2.7 or at a skull. The optic canal is the most posterior landmark in the orbit. The length of the optic canal is 10 mm. Medially, the posterior ethmoid foramen is 4 to 7 mm anterior to the optic canal; it is an important surgical landmark when operating deeply along the posterior orbital wall (see Figure 2.13 ). Laterally, the optic canal is separated from the superior orbital fissure by a small piece of bone, the optic strut . If you follow the optic strut posteriorly and superiorly, it becomes the anterior clinoid process. Although not important for you now, if you approach the optic canal from an intracranial exposure with your neurosurgical colleagues, knowledge of this relationship may help you. (Next time you pick up a skull, look at how the optic strut extends to form the anterior clinoid process. It will help you learn some of this complicated anatomy.) When you look at a computed tomography (CT) scan, the thin piece of bone separating the optic canal from the superior orbital fissure is the optic strut. Earlier, we said that the posterior portion of the lateral orbital wall was made up of the greater wing of the sphenoid bone ( Figure 2.14 ). The optic strut and the optic canal are parts of the lesser wing of the sphenoid bone. The sphenoid bone forms a large part of the skull base and posterior orbit. Its shape is complicated. For now, just remember that the greater wing lies lateral to the superior orbital fissure and the lesser wing lies medial to the superior orbital fissure .

Look at the CT scan shown in Figure 2.14 . It is easy to recognize the superior orbital fissure because it opens into the intracranial space. Similarly, it is easy to recognize the inferior orbital fissure because it opens into the space posterior to the maxillary sinus (the pterygopalatine fossa) and into the infratemporal fossa laterally. The inferior orbital fissure does not open into the brain. The optic canal is adjacent to the anterior clinoid processes (seen on the same CT cut). The optic canal also opens into the intracranial space.
There are two other sets of foramina. All carry the related arteries, veins, and nerves. These foramina are:
Anterior ethmoidal
Posterior ethmoidal
Zygomaticotemporal
Zygomaticofacial
The anterior and posterior ethmoidal foramina are important surgical landmarks that separate the medial wall and roof of the orbit. These foramina are found in the frontoethmoid suture. If you break the medial wall inferior to the suture, you are in the ethmoid sinus. If you break the bone above the suture, you are in the brain (causing a cerebrospinal fluid [CSF] leak). The anterior-posterior location of the foramina is a helpful indicator of how far posterior an orbital dissection along the medial wall is proceeding. The anterior ethmoidal foramen is about 24 mm posterior to the anterior lacrimal crest. The posterior ethmoidal foramen is another 10 to 12 mm posterior. As we have already mentioned, the optic canal is 4 to 7 mm more posterior. A helpful way to remember is 24 – 12 – 6 mm. During an operation, it is easy to overestimate your position on the medial orbital wall, so these numbers are surprisingly helpful as you learn orbital surgery. When you operate along the medial orbital wall, it is important to recognize the ethmoidal vessels because significant bleeding can occur if they are inadvertently torn. The ethmoidal veins are valveless and permit flow into the orbit from the ethmoid sinus. Purulent sinusitis can spread into the orbit through these vessels or directly into the orbit through the thin lamina papyracea of the medial orbital wall. I talk more about the vessels and sensory nerves that travel in these foramina later.
The zygomaticotemporal and zygomaticofacial foramina transmit the arteries, veins, and nerves of the same name. The nerves are sensory branches of the trigeminal nerve (V 2 ). The arteries are small branches that originate off the lacrimal artery (a main branch of the ophthalmic artery, which arises directly off the internal carotid artery). You see these foramina when you lift the periorbita off the lateral wall. Cauterization is appropriate before you cut the arteries. If the artery retracts into the foramen, bleeding can be stopped by packing the foramen with a bit of bone wax. Cutting these nerves during a lateral orbitotomy results in some hypesthesia of the surrounding area that is minimal because of collateral innervation. Note that the overlap of these vessels and nerves with adjacent vessels and nerves of differing origin is typical of the collateral innervation and vascularization of the facial area. The medial and inferior branches of the infraorbital artery (from the internal maxillary artery) overlap with the branches of the ophthalmic artery and ophthalmic nerve (V 1 ). Anastomoses of the zygomaticotemporal nerve (from V 2 ) with the lacrimal nerve (from V 1 ) have sensory overlap. This overlap of blood and nerve supplies helps to preserve function after accidental trauma. Incisions can be made and flaps formed with a relatively low risk of ischemia or permanent sensory loss.
The bones of the orbit are covered with periosteum like all the other bones of the body. The periosteum covering the inside of the orbit is known as the periorbita . The periorbita is tightly adherent to the bone at the orbital suture lines and along the orbital rims. Over the orbital walls, the periorbita is loosely adherent. You see these differing degrees of adhesion when pus or blood accumulates under the periorbita as a result of infection or trauma. In these situations, the periorbita is elevated off the orbital walls in a characteristic dome-shaped elevation ending at suture lines where the periorbita is adherent ( Figure 2.15 ). The orbital septum is an extension of fibrous tissue continuous with the periosteum, extending from the orbital rim to the lids. The structure formed where the orbital septum attaches to the rim is known as the arcus marginalis . Three structures meet at the arcus marginalis, the orbital septum, the periorbita, and the periosteum. The orbital septum is discussed in more detail later.
Imagine having a skull in your hand. You should be able to point out 5 or 10 minutes’ worth of bone anatomy and some of the clinically relevant features:
Name the bones of the orbital rims. Which bone rarely breaks? Point to the fracture lines of a ZMC fracture.
Describe the boundaries of the orbital walls. Name the bones of the walls. Where does a blowout fracture occur? Why is hypesthesia of the infraorbital nerve and subcutaneous emphysema common? What are other signs of a blowout fracture?
Name three openings in the orbital walls and describe what spaces they connect. Try to identify these on each orbital axial CT scan:
Optic canal
Superior orbital fissure
Inferior orbital fissure
What two openings in the orbit form a V?
What structure separates the superior orbital fissure from the optic canal?
Which foramina separate the medial wall from the roof of the orbit?
If you know the answers to these questions, you are doing very well. If not, review the last section. This is basic information that you should know.

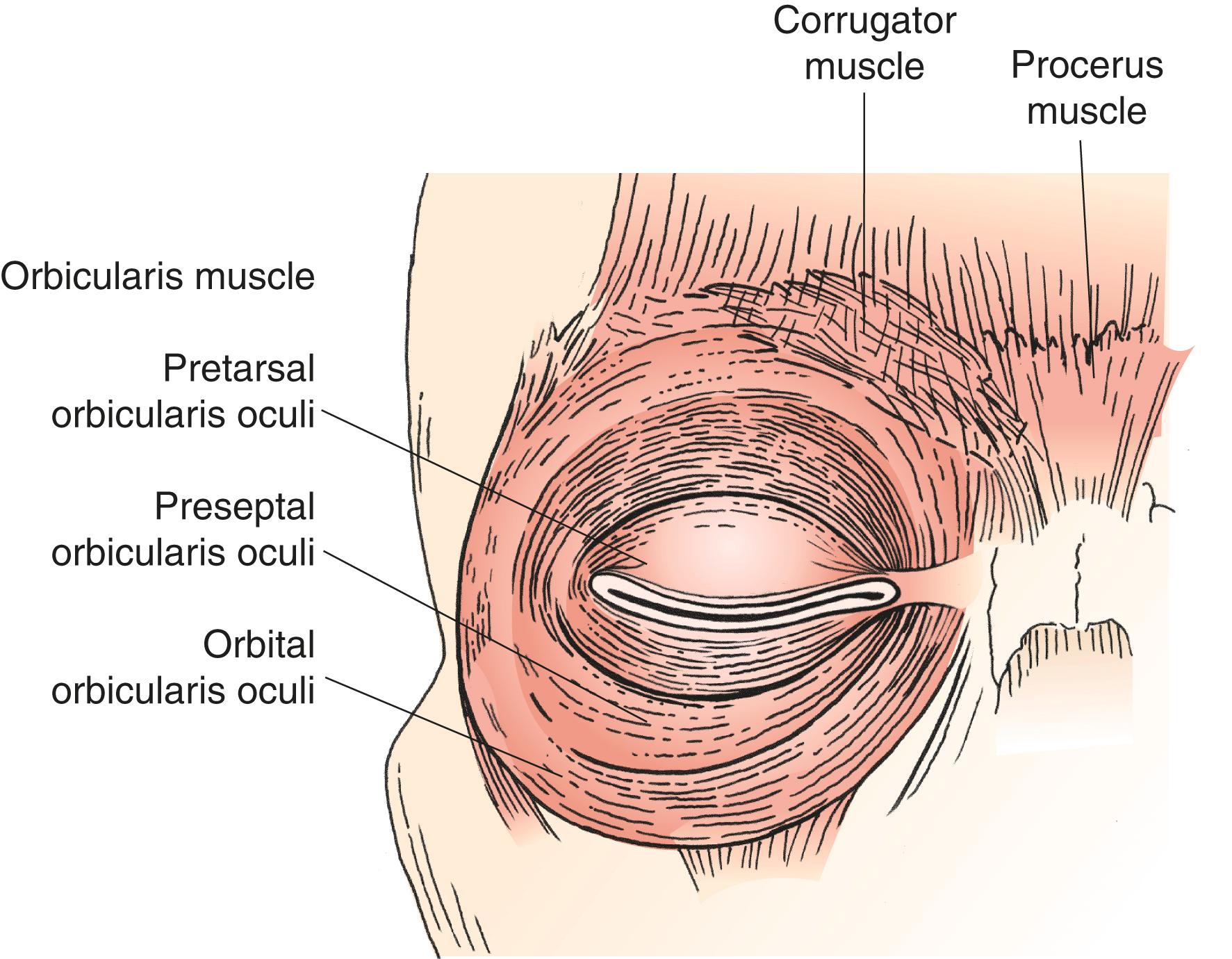
For the eyelids to function, there must be muscles that close the eye and muscles that open the eye. The orbicularis muscle ( Figure 2.16 ) is the muscle primarily responsible for closing the eyelids. The orbicularis muscle is anatomically divided into the pretarsal portion, the preseptal portion, and the orbital portion. The pretarsal and preseptal portions overlay the tarsus and the septum, respectively. These muscles are responsible for involuntary spontaneous blinking. The orbital portion covers the orbital rims and is responsible for forced eyelid closure. All parts of the orbicularis muscle are innervated by the facial nerve with innervation entering from the underside of the muscle as for all muscles of facial expression.
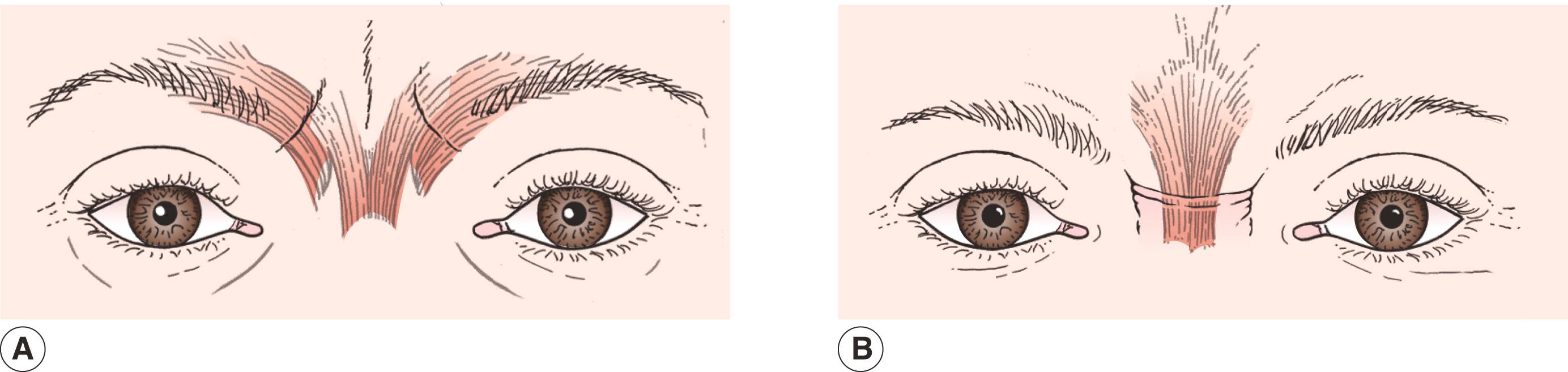
Other protractors of the eyelids (protractors being the opposite of retractors, which open the eyes) include the corrugator muscle and the procerus muscle (see Figure 2.16 ). The corrugator muscle originates on the bone of the superonasal rim and inserts into the skin of the head of the eyebrow. Firing of the corrugator muscle pulls the heads of the eyebrows together and makes the vertical/diagonal furrows of the glabella ( Figure 2.17 ). The procerus muscle originates on the frontal bone above the glabella and inserts into the skin of the glabella. The action of these vertically oriented muscle fibers pulls the heads of the brows inferiorly and causes the horizontal furrows of the glabella. Check out your own glabellar furrows in the mirror as you squeeze your eyebrows together. Can you see contributions from both the corrugator and procerus muscles?
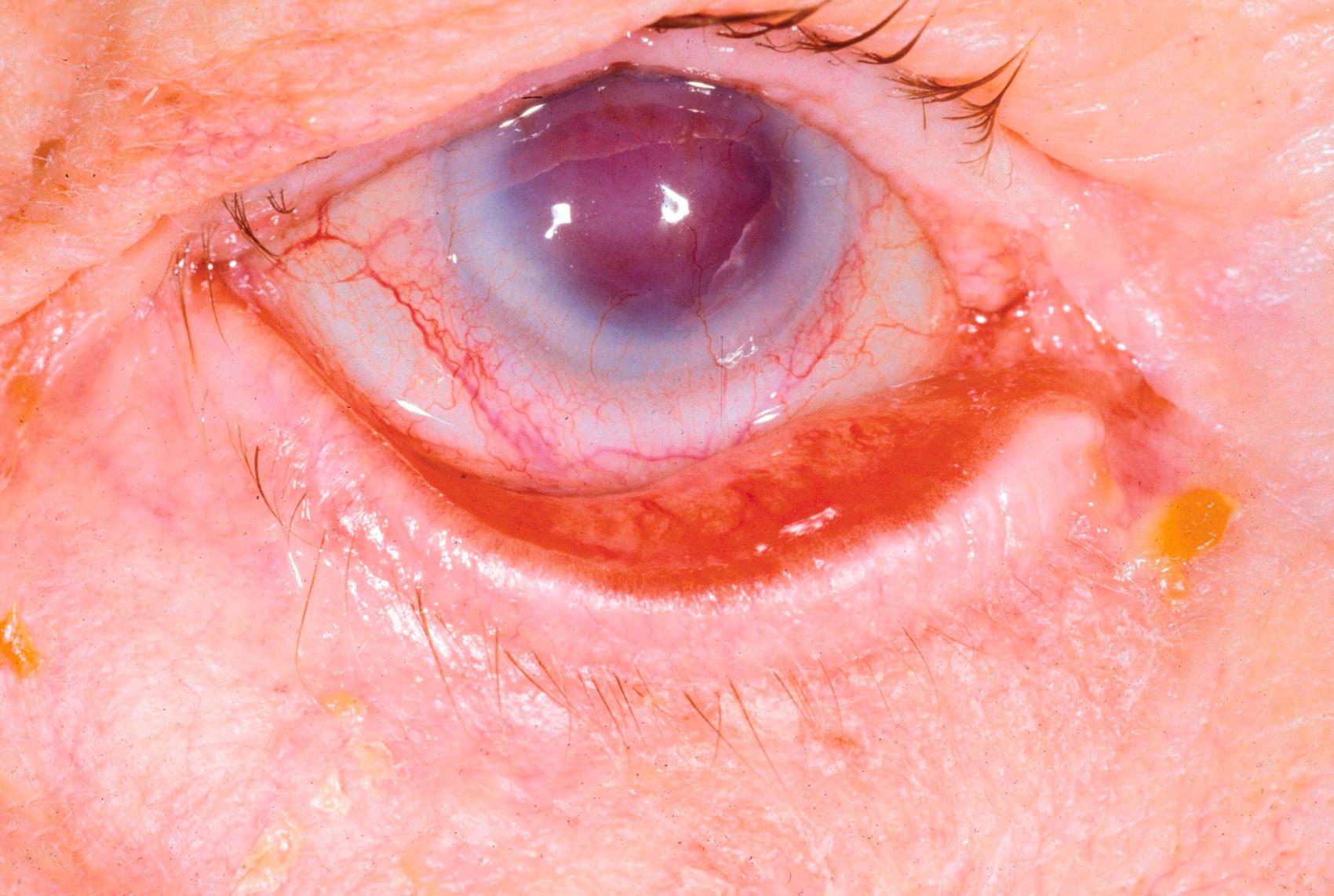
A number of clinical problems result from underactivity or overactivity of the muscles that close the eyes. Facial nerve palsy ( Figure 2.18 ) results in poor eyelid closure seen as lagophthalmos (the eyelids do not close with passive lid closure) or an incomplete spontaneous blink (quick normal blinks that do not completely cover the cornea). All the facial muscles on the affected side are also weakened, resulting in the brow ptosis, ectropion, flattening of the melolabial fold, and drooping of the corner of the mouth that you have seen in patients.

The disorders resulting from overactivity of the orbicularis muscles are orbicularis myokymia , facial tics , essential blepharospasm , and hemifacial spasm. Probably you have suffered from orbicularis myokymia at one time or another. Hyperexcitability of the muscle, caused by stress, too much caffeine, or lack of sleep, causes a quick twitch of a few muscle fibers. Orbicularis myokymia is self-limited and usually lasts a few days or less. The other conditions involve different patterns of overactivity of the facial muscles, including the orbicularis muscle. These are discussed in detail later in Chapter 9 .
The last section is straightforward. You should know:
The muscles that close the eyes
The muscles responsible for the horizontal and vertical glabellar furrows
The problems associated with underactive and overactive facial muscles
You see these conditions commonly in practice. You learn the diagnosis and treatment of these problems in detail in Chapter 8 .
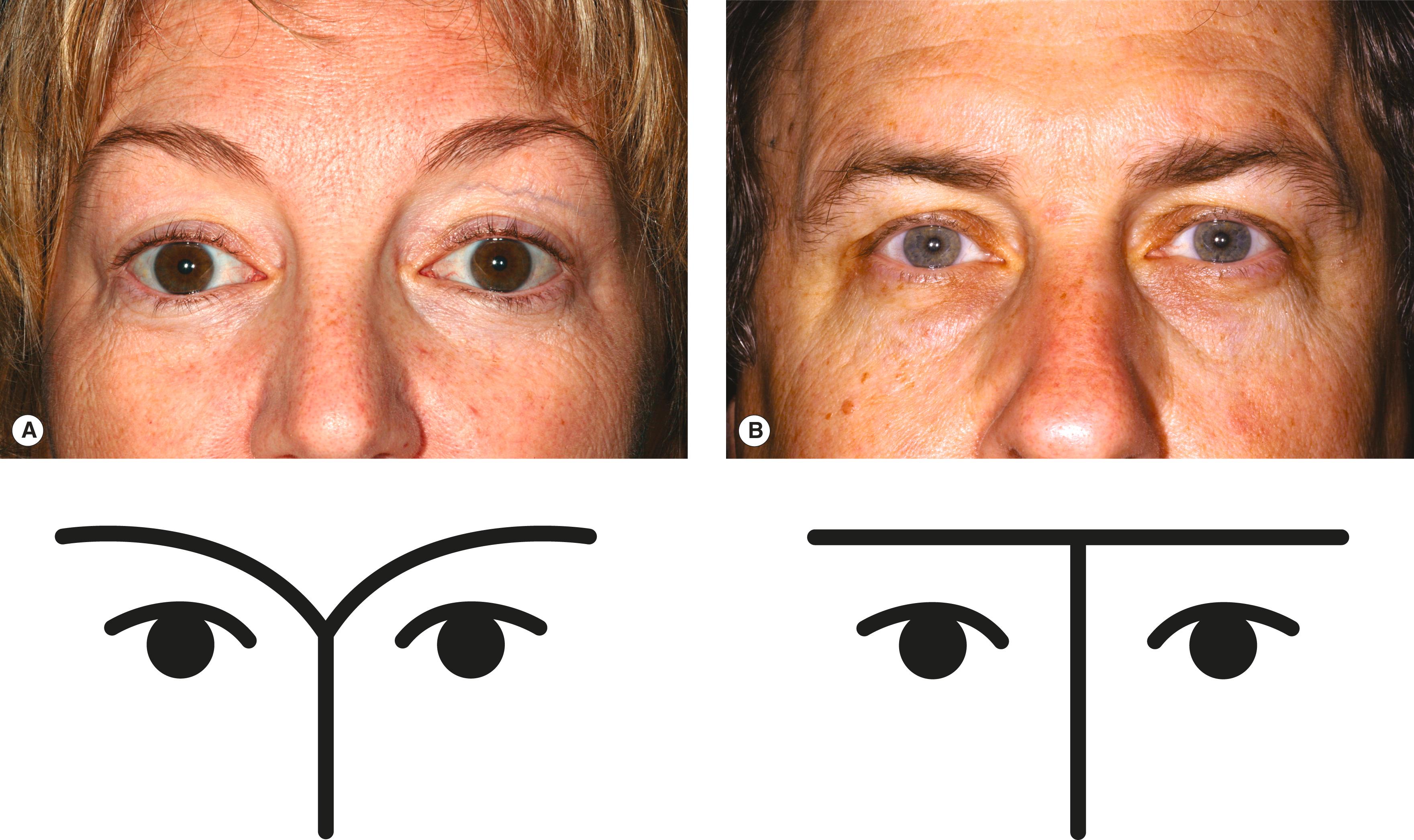
Before we leave the topic of the orbicularis muscle, a discussion of the canthal tendons is needed. As I have already noted, the canthal tendons attach the eyelids to the lateral and medial orbital rims ( Figure 2.19 ). The tendons are extensions of the orbicularis muscle that attach to the periorbita overlying the bone. The anatomy of the lateral canthal tendon is easy to understand ( Figure 2.20A ). The pretarsal and preseptal portions of the orbicularis muscle of each eyelid taper to form the superior limb and inferior limb of the lateral canthal tendon . The upper and lower limbs unite to form the lateral canthal tendon, which attaches to the inner aspect of the lateral orbital rim on Whitnall ’s tubercle . Imagine the lateral canthal tendon complex as a Y lying on its side with contributions from both the upper and the lower eyelids.
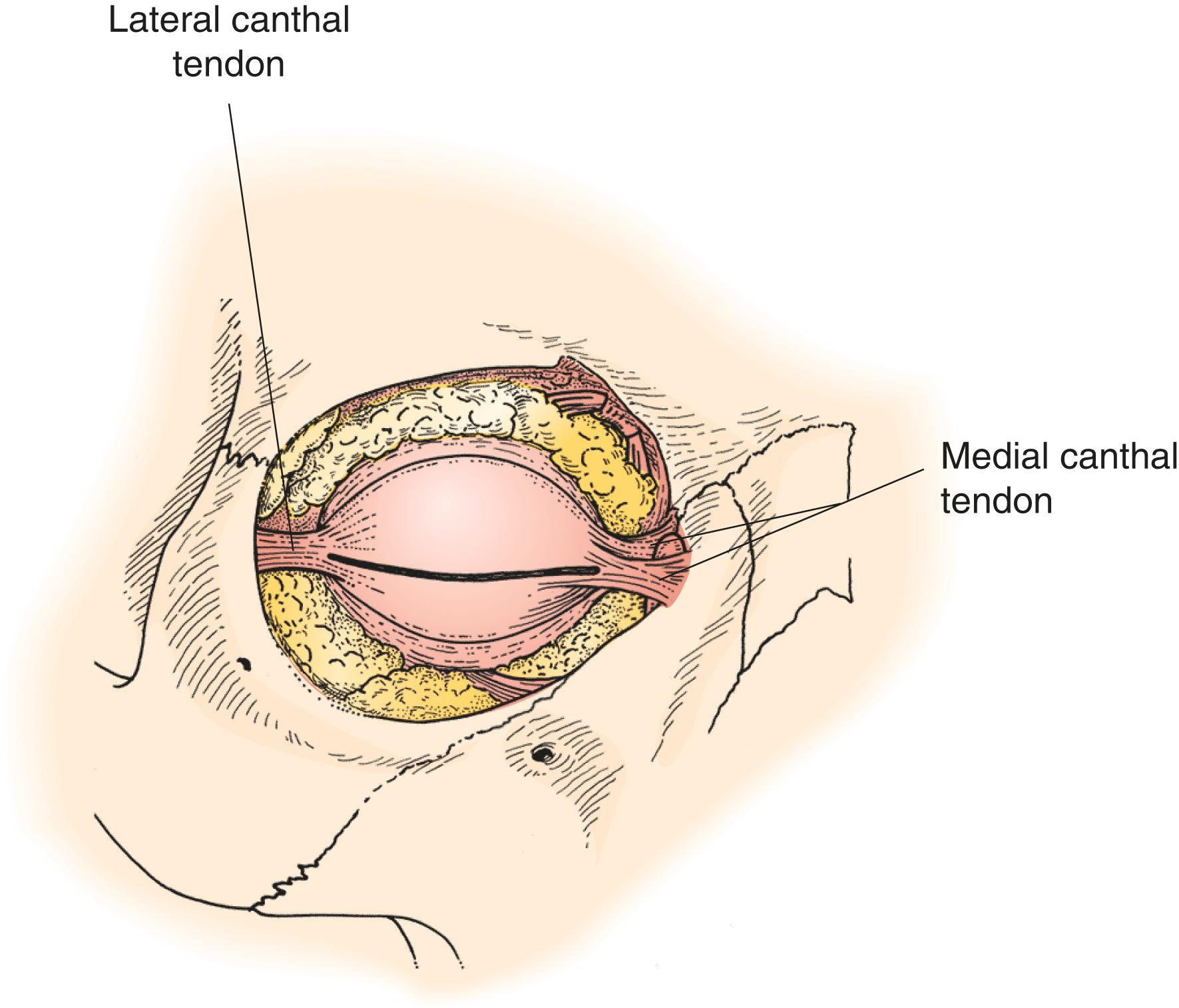
There is a wide variability of the “normal” slope of the eyelids. The lateral canthal tendon is normally at the same level or a few millimeters higher than the medial canthal tendon ( Figure 2.21A ). A downward slant toward the lateral canthal tendon is known as an “antimongoloid slant.” It is seen in a number of syndromes (such as Treacher Collins syndrome; see Figure 2.21 , B) and is also a variation of normal. An upward slant toward the lateral canthal tendon is known as a mongoloid slant. You want to re-create the patient’s symmetric natural slant to the eyelids when you work on the canthal tendons.
In the following chapters, you learn that proper horizontal tension on the lower eyelid is necessary for the eyelid to maintain its position. Laxity of the lower eyelid is the major cause of lower eyelid eversion or ectropion ( Figure 2.22 ). This laxity does not occur from stretching of the tarsal plate; rather, it is attributable to lengthening of the lateral canthal tendon with age. You may have heard of older patients stating that their eyes look smaller than they did in their youth. You have probably already noticed that, with age, the upper eyelid droops (ptosis) and the lower eyelid actually rises up a bit (stretching of the lower eyelid retractors). Less apparent, but equally common, is a horizontal narrowing of the eyelid as a result of stretching of the canthal tendons. Thus, the “small eyes” that your older patients may notice are caused by both horizontal and vertical narrowing of the palpebral fissure. You might recall that big eyes are “pretty” eyes, a sign of youth.
Attributable in part to the simplicity of attachment of the lateral canthal tendon to the bone, the aim of lower eyelid tightening operations is to shorten the lateral canthal tendon. In this procedure, known as a lateral tarsal strip operation , a horizontal cut is made at the lateral canthus. This incision, known as a lateral canthotomy , splits the Y of the lateral canthal tendon into a V. Then the lower leg of the V (the lower limb, or crus , of the lateral canthal tendon) is cut. This cantholysis releases the lower lid from the lateral orbital rim. A portion of the tendon and sometimes the tarsus itself is then shortened and resutured to the periorbita at Whitnall’s tubercle. Remember that Whitnall’s tubercle is on the inner aspect of the lateral rim. It is important to reattach the strip on the inside of the rim so that the lid does not pull away from the eye. When working on one eye, remember to reposition the lateral canthal tendon to create a symmetric slope. In most patients the lateral canthal tendon is placed slightly higher than the medial canthal tendon to re-create a slight upward slant to the lateral canthus.
Trauma to the orbital rims may cause displacement of the canthal tendons. The separation of the frontal and zygomatic bones seen with the zygomaticomaxillary complex (tripod) fractures discussed above causes the lateral canthal tendon to be displaced downward (lateral canthal dystopia).
The medial canthal tendon is much more complex than the lateral canthal tendon because of the relationship of the medial canthal tendon to the lacrimal drainage system. The pretarsal and preseptal portions of the orbicularis muscle extend medially to form the two limbs of the medial canthal tendon (see Figure 2.20B ). The discussion of the anatomy of the medial orbital rim states that the anterior limb attaches to the frontal process of the maxilla along the anterior lacrimal crest. The posterior limb attaches at the posterior lacrimal crest. Remember that the two limbs of the tendon surround the lacrimal sac (see Figure 2.20C ). As the eyelid blinks, the limbs of this tendon cause the lacrimal sac to contract and relax. This action is known as the lacrimal pump. Incomplete “pumping” of the sac due to age, trauma, or facial nerve palsy contributes to tearing problems.
Laxity of the lower eyelid is usually not caused by medial canthal tendon stretching. Occasionally, laxity of the medial canthal tendon is seen. As the lower eyelid is pulled laterally, the lower eyelid punctum is seen to extend to or beyond the medial limbus. Although procedures to tighten the medial canthal tendon have been devised, they are seldom used because of the difficulty in working on the medial canthal tendon without damaging the canaliculi or the lacrimal sac.
Fractures at the medial canthus generally cause the medial canthus to be displaced laterally, resulting in telecanthus , an increase in the distance from the canthus to the midline. The medial canthal tendon is at about the same position vertically as is the cribriform plate. In any operation that involves removing or repositioning bone at or superior to the medial canthal tendon, there is the risk of an inadvertent CSF leak.
Many problems related to the canthal tendons require treatment. Some points to remember are:
The lateral canthal tendon is simpler than the medial canthal tendon. You should have an anatomic concept of what this tendon looks like to help you understand the procedures that are done at the lateral canthus.
Ectropion of the lower eyelid is one of the most common problems that you see. Use your anatomic concept of the lateral canthal tendon to visualize canthotomy, cantholysis, and other steps in the lateral tarsal strip operation.
Again, visualize your conceptual anatomy of the medial canthal tendon surrounding the lacrimal sac. Do you remember where the anterior and posterior limbs of the medial canthal tendon insert?
Which is more common—medial canthal tendon laxity or lateral canthal tendon laxity?
How might facial nerve palsy contribute to tearing?
Poor lacrimal pump
Ectropion
Incomplete blinking resulting in corneal exposure
How are lateral canthal dystopia and telecanthus similar?
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here