Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
With ongoing advances in the diagnosis and treatment of childhood cancers, increasing numbers of children and adolescents diagnosed with cancer are becoming long-term survivors. However, even as higher cure rates are achieved, there is increasing recognition that the diagnosis and treatment of cancer during childhood and adolescence can have lifelong implications for health and well-being. Cancer therapy administered during critical periods of growth and development render childhood cancer survivors vulnerable to a variety of physical and emotional disorders often referred to as “late effects.” Some late effects can be diagnosed soon after completion of cancer-directed therapy, and others may not manifest until decades later. The severity of late effects ranges from minor disabilities to chronic conditions and even life-threatening morbidities, including second cancers, cardiac disease, and pulmonary dysfunction. Severe late effects can reduce a survivor's life expectancy.
Although remarkable progress has been made in advancing our understanding of the adverse health outcomes associated with treatment of childhood cancer, survivors continue to experience significant long-term morbidity related to late effects. Increasingly it is recognized that the care of the child or adolescent diagnosed with cancer does not end with the completion of therapy but continues on the path into adulthood. Clinical focus during survivorship care shifts from treatment of the primary cancer and screening for its recurrence to the prevention, detection, and management of adverse consequences of prior therapy. Ultimately, ongoing research may result in the reduction or even elimination of late effects and in improved quality of life for childhood cancer survivors.
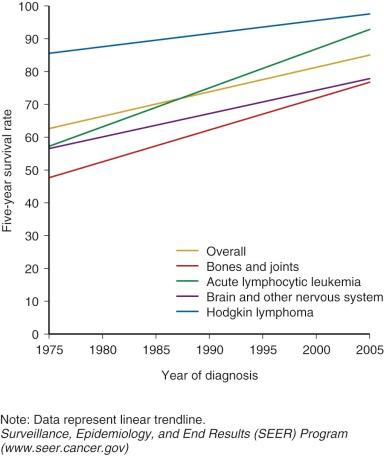
Prior to 1950, children and adolescents who developed cancer rarely survived. The first generation of survivors primarily consisted of children with Hodgkin lymphoma, sarcoma, and Wilms tumor who were successfully treated with surgery and high-dose, large-field radiation therapy. The widespread use of multiagent chemotherapy, beginning in the 1970s, resulted in dramatic increases in survival for the most common childhood cancer, acute leukemia, and continued improvement in survival for other pediatric cancers as well. By the mid-1970s, many forms of childhood cancer became treatable, and potentially curable. Continuing advances in treatment options for childhood cancer have continued to improved survival. Children with cancer have also benefited from improvements in diagnostic testing, resulting in earlier and more precise diagnosis and more timely delivery of necessary treatment. Enhanced supportive care including advances in intensive care, blood banking, and management of infectious disease and acute toxicities of therapy also contributed to successful outcomes. Currently, the overall 5-year survival for childhood cancer exceeds 80%, and for some cancer diagnoses 5-year survival is above 95% ( Fig. 72-1 ). There are estimated to be more than 300,000 adult survivors of childhood cancer in the U.S. population, and this number continues to grow by approximately 10,000 survivors each year.
Along with these remarkable advances in survival there is a growing recognition that treatment for childhood cancer is associated with long-term complications or “late effects.” Late effects can be defined as adverse health outcomes experienced by childhood cancer survivors associated with previous cancer–directed therapy; these outcomes reduce survival or affect the “quality” of survival. Some late effects can be life threatening and contribute to the increased risk for early mortality observed in adults who are long-term survivors of childhood cancer. Other late effects, such as neurocognitive impairment, physical deformity, and infertility, can limit survivors' social or economic opportunities and impair their overall quality of life. In contrast, some late effects may be “positive” effects, such as increase in psychological resiliency and decrease in smoking rates and the rates of other high-risk behaviors compared with those in the rest of the population.
Second cancers, cardiopulmonary disease, and infertility were among the first treatment-associated late effects recognized in childhood cancer survivors. These first descriptions were based on clinical observations in small numbers of the earliest survivors of childhood cancer treated primarily with surgery and irradiation in the 1960s. Early clinical observations created awareness about late effects and identified the need for further research defining treatment-related health outcomes in the growing numbers of survivors of childhood cancer.
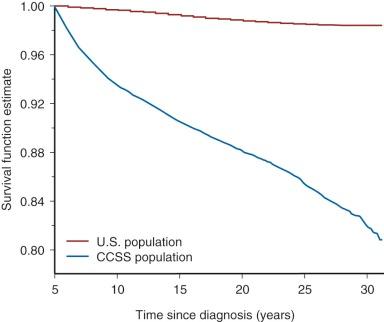
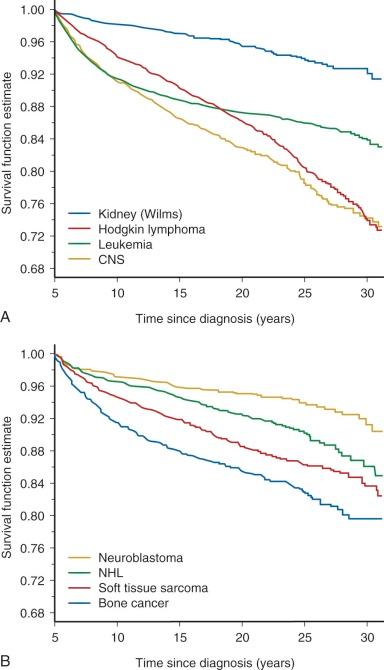
Follow-up studies of the earliest cohorts led to the observation that childhood cancer survivors are at risk for early mortality. These studies showed that late recurrence of the primary cancer and treatment-associated complications resulted in decreased long-term survival, 80% at 20 years after diagnosis compared with 97% expected survival in the age-matched general population. The majority of premature deaths observed in survivors in these early studies were attributed to late relapse, whereas treatment-associated second cancers and major organ toxicity accounted for 30% of deaths. It was also recognized that the risk for dying of a treatment-related cause increased with increasing intensity of therapy. Although late recurrence accounts for the majority of premature deaths observed in childhood cancer survivors, the risk for relapse diminishes over time while the risk for therapy-related mortality persists beyond 25 years of follow-up. Figure 72-2 depicts all-cause mortality in 5-year survivors of childhood cancer, and Figure 72-3 demonstrates all-cause mortality by underlying cancer diagnosis. It remains to be determined if current treatment protocols that are specifically designed to reduce late effects will continue to improve very long-term survival by reducing the risk for therapy-related mortality.
After the early descriptive studies, registry-based investigations of larger groups of childhood cancer survivors were undertaken with the aim of identifying specific risk factors for late effects. These included the National Cancer Institute's “Five Center Study,” a registry-based cohort that enrolled 2490 adult 5-year survivors diagnosed with cancer between 1945 and 1975 at age younger than 20 years who were followed prospectively for reproductive outcomes, second cancers, and mortality ; the “Late Effects Study Group,” a multiinstitutional cohort that analyzed the occurrence of second cancers in 9170 two-year survivors of childhood cancer diagnosed between 1936 and 1979 ; and cancer registry–based studies in the United Kingdom, the Netherlands, and the Nordic countries (Denmark, Finland, Iceland, Norway, Sweden) from the same early treatment era and beyond. These epidemiologic studies analyzed the association between specific treatments and adverse health outcomes of interest. Relative risks were calculated to compare rates of outcomes under study in cancer survivors with rates in a control population. Collectively these investigations made significant contributions to the understanding of late effects. Limitations of such studies of late-occurring outcomes included that recruitment was often not complete, resulting in a possible overrepresentation of childhood cancer survivors who were experiencing health conditions related to their prior therapy. In addition, some of the late effects observed in these cohorts were associated with historic treatments that have been replaced by more modern modalities. However, despite such limitations, these studies identified the relationships, now well accepted, between cancer therapy and early mortality, radiation therapy and secondary cancers, and alkylating agents and gonadal dysfunction.
To address the limitations of prior studies, the development of “survivor” cohorts to be followed prospectively was undertaken by investigators in North America and Europe. In North America, a multiinstitutional follow-up study of a cohort of over 14,000 childhood cancer survivors (the Childhood Cancer Survivor Study [CCSS]) was created, evaluating late effects in survivors diagnosed from 1970 to1986, at age younger than 21 years, and surviving at least 5 years from diagnosis. A recent expansion of the CCSS to include survivors treated between 1986 and 1999 will yield important analyses of the effects of more “modern” therapies, as well as reflect a more ethnically and racially diverse population in North America. The CCSS uses self-reported questionnaires to obtain health outcomes and analyzes the association between outcome and treatment variables documented in abstracted medical records. The primary end points investigated by the CCSS included second cancers, mortality, and heart disease. Large registry-based cohort studies of childhood cancer survivors treated in Great Britain, France, the Netherlands, and the Nordic countries are ongoing and continue to contribute to our understanding of survivorship. Within these cohort studies, the prevalence of and the risk factors for the development of late effects after childhood cancer have been better elucidated.
Advances continue to be made in recognizing and categorizing adverse health outcomes in childhood cancer survivors. However, the study of late effects in cancer survivors has inherent challenges that must be considered when interpreting research findings. First, there is not universal implementation of a definition for “cancer survivor.” The definition chosen for a particular investigation determines eligibility for studies and dictates how results can be interpreted and generalized to specific populations of survivors. The Office of Cancer Survivorship at the U.S. National Cancer Institute considers an individual a cancer survivor from the moment of cancer diagnosis through the balance of his or her life regardless of degree of cancer control. Although this definition is meaningful, particularly from an advocacy perspective, it is not effective for the purposes of understanding late outcomes in a cured population. Survival 5 years beyond cancer diagnosis is the definition of cancer survivor that is often, but not universally, used for the purpose of research on late effects.
Another consideration is how investigators measure the late effect or outcome of interest. Self-report is frequently used to measure outcomes in epidemiologic studies of late effects. Although it is cost-effective, self-report can lead to reporting bias that results in inaccurate assessments of the incidence or severity of outcomes. Studies of smaller groups of survivors utilizing direct observation to delineate outcomes help to confirm self-reported outcomes, refine our understanding of these outcomes, and allow direct measurement of asymptomatic or early morbidity not evident by self-report. The disadvantages of this type of clinical studies are cost, complexity, and small sample size, which can limit interpretation of results.
The timing of assessments can also influence the results and interpretation of late effects research. Although it can be efficient to recruit survivors for follow-up studies during or soon after treatment, some late effects are not observed until decades after initial therapy. Studies with inadequate periods of follow-up might yield results that underestimate or overestimate late effects. Retaining survivors in observational cohorts over long periods of follow-up is challenging, and results may be biased toward retention of patients experiencing the outcomes under investigation. Consideration of the duration of follow-up is particularly important when applying results to populations of pediatric survivors, in whom late effects may emerge in the course of developmental change.
Another challenge when interpreting the results of late effect studies is that most results are reported as relative risks, the rate of an outcome observed in a cohort of survivors relative to the rate of the outcome observed in a control population. Elevated relative risks must be interpreted and communicated with caution, because even the smallest increase in an otherwise very rare outcome results in a very large relative risk; however, even a small or statistically insignificant increase in relative risk might have important clinical implications.
Finally, an inherent difficulty with studying late effects is that treatments for cancer continue to evolve; therefore the health outcomes of interest in follow-up studies are often reflective of historic or outdated treatments. Methodology does not exist to address this issue, so treatment era must be taken into consideration when interpreting the results of these investigations. Duration of follow-up, treatment era, cohort eligibility, and outcome measures are all aspects of study design that merit careful consideration when interpreting results of late effects research studies.
Epidemiologic studies investigating the association between treatment and risk for adverse health outcomes have led to general principles that contribute to our thinking about an individual survivor's potential for developing late effects ( Box 72-1 ). A childhood cancer survivor's risk for developing late effects depends on the nature of prior treatment as well as individual characteristics, such as age at exposure, gender, or time since exposure.
First, the dose and intensity of the treatment is frequently correlated with risk for late effects. In general, survivors exposed to larger doses of therapy have worse outcomes. For example, risk for male infertility after treatment with gonadotoxic chemotherapy is directly related to dose; males exposed to the highest cumulative doses have the greatest risk for future infertility. In addition, a survivor's likelihood for late effects is increased if there is exposure to more than one modality with related toxicities. For example, survivors treated concurrently with mediastinal radiation and cardiotoxic chemotherapy are at greater risk for cardiac late effects than those treated with either of those modalities alone.
Organ toxicity associated with a single treatment exposure can manifest clinically as different late effects depending on the timing of the clinical assessment. For example, consider a postmenarchal female adolescent treated with gonadotoxic chemotherapy. During treatment she might experience acute reversible amenorrhea. Years later, after resolution of acute menorrhea, the woman might experience infertility secondary to premature menopause. Over time, the same woman might have osteoporosis as a secondary late effect of chronic estrogen deficiency. Neurocognitive impairment after central nervous system (CNS) therapy provides another example of how the timing of assessment influences detection of late effects. Children treated with CNS therapy might not manifest treatment-related neurocognitive deficits until they reach a time when school work, employment responsibilities, or social interactions require more complex cognitive function. The clinical manifestations of a single treatment exposure can change over time and are influenced by the physical, emotional, and social needs of the individual survivor.
Duration of follow-up also influences the potential for late effects. Some irradiation-associated late effects, especially secondary malignancies, have long latency periods, with increases in cumulative incidence over time. In contrast, other treatment-related toxicities can be acute and resolve (bone marrow suppression) or occur late and be progressive (pulmonary fibrosis). The leukemogenic potentials of specific forms of chemotherapy appear to be associated with fairly discrete time frames after exposures: topoisomerase inhibiters are associated with occurrence of secondary leukemias within months of exposure and rarely beyond 5 years, whereas alkylating agents are associated with a later onset and a later, but still predictable plateau in cumulative incidence at 10 years after exposure. In addition, acute chemotherapy organ toxicity can predict late toxicity. For example, chemotherapy-associated renal toxicity diagnosed during therapy can persist as a chronic condition or resolve and be diagnosed again as chronic renal disease decades after treatment. Although treatment exposures are the largest determinants of future late effects, a survivor's age or developmental stage during cancer treatment and his or her sex, family history, existing comorbidities, and health behaviors can all modulate risk for the development of late effects. In general, younger age at treatment is associated with a higher risk and/or greater severity for late effects. Children treated with cranial irradiation during the critical period of rapid brain development (<2 years old) are at greater risk for neurocognitive late effects than children treated when they are older. In addition, female survivors are at greater risk than males for some late effects, including chemotherapy-associated cardiomyopathy, neurocognitive impairment, and second cancers, although the explanation for this gender difference is not clear.
Underlying genetic predisposition for cancer (contributing etiologically to the primary cancer occurrence) will influence the risk for secondary cancers, as has been observed in hereditary retinoblastoma and nevoid basal cell carcinoma syndrome. In some patients, the only marker of this predisposition will be family history or a feature of the primary tumor itself (young age at occurrence, occurrence in paired organs). Predisposition to late effects based on genetic background is an area of great interest in survivorship research. Those survivors with a genetic predisposition to chronic medical conditions, such as heart disease, may be at greater risk for treatment-associated chronic conditions, such as radiation-associated coronary artery disease. Recent genome-wide association studies have identified risk-specific polymorphisms that may become clinically relevant for predicting the risk for late effects and allow for potential tailoring of primary cancer therapy or follow-up. Most associations that have been described—for example, for ototoxicity after cisplatin exposure or second cancer after irradiation —await further validation. In addition, common medical comorbidities associated with aging, such as hypertension or hypercholesterolemia, may contribute to a survivor's risk for a variety of medical late effects, including chronic renal disease, heart disease, and cerebrovascular disease. Modifiable health behaviors such as diet, exercise, smoking, and sun exposure may also modulate a survivor's risk for late effects.
High rates of chronic health conditions have been described in adult survivors of childhood cancer. In the CCSS cohort, the relative risk for a severe or life-threatening chronic condition in survivors when compared with siblings was 8.2 (95% confidence interval [CI], 6.9 to 9.7). In the St. Jude Lifetime Cohort Study, the cumulative prevalence of a chronic condition was 95.5% (9%% CI, 94.8% to 98.6%) by age 45 years and 80.5% (95% CI, 73.0% to 86.6) for a severe or life-threatening or disabling condition. The following section provides an overview of late effects experienced by survivors of childhood cancer. A summary of selected treatment-associated late effects is presented in Table 72-1 .
| Treatment | Late Effect | Comments | Reference |
|---|---|---|---|
| Alkylating agents (busulfan, carmustine, lomustine, mechlorethamine, procarbazine, cyclophosphamide, ifosfamide, dacarbazine, melphalan) | Secondary leukemia/ myelodysplasia | Melphalan and mechlorethamine more leukemogenic than cyclophosphamide Median latency 4-6 years Dose-response relationship |
|
| Premature menopause | Risk factors: increasing cumulative total dose, concurrent pelvic radiation, increasing age, older age at treatment Myeloablative doses are associated with ovarian failure. Cryopreservation of oocytes or embryos are interventions to preserve fertility. |
||
| Male infertility | Risk of azoospermia increases with increasing cumulative dose; spermatogenesis may recover over time. Highest dose is associated with impaired testosterone production. Pretreatment semen cryopreservation and testicular sperm extraction are interventions to preserve fertility. |
||
| Anthracyclines (daunorubicin, doxorubicin, mitoxantrone, idarubicin) | Clinical heart failure | Risk factors: female gender, age <5 yr, cumulative doxorubicin equivalent dose >250-300 mg/m 2 , concurrent radiation | |
| Bleomycin, carmustine, busulfan (pulmonary toxic chemotherapies) | Pulmonary fibrosis | No plateau in incidence observed Radiation exposure an additional risk factor |
|
| Platinum compounds (cisplatin, carboplatin) | High-frequency hearing loss | Cumulative dose cisplatin >450 mg/m 2 Risk factors: dose, age <5 yr Carboplatin ototoxic at myeloablative dose |
|
| Speech frequency hearing loss | Cumulative dose cisplatin >720 mg/m 2 Rarely observed cumulative dose cisplatin <360 mg/m 2 Risk factors: dose, age <5 yr Carboplatin ototoxic at myeloablative dose |
||
| Topoisomerase II inhibitors (epipodophyllotoxins and anthracyclines) | Secondary leukemia | Median latency 1-3 yr Frequent administration increases risk (weekly/twice weekly). |
|
| Any irradiation | Secondary sarcoma | Risk factors: increasing radiation dose, concurrent alkylating agent or anthracycline chemotherapy, young age at diagnosis, primary diagnosis of sarcoma or retinoblastoma, family history of sarcoma | |
| Nonmelanomatous skin cancer | Fifty percent of survivors will have multiple lesions. Basal cell carcinoma—linear dose-response |
||
| Melanoma | Risk factors: radiation dose >15 Gy, prior history melanoma, retinoblastoma, familial melanoma | ||
| Cranial and head/neck irradiation (including TBI) | Growth hormone deficiency | High prevalence (85%-100%) with median dose 45-55 Gy Observed at 18-24 Gy, with lower prevalence and longer latency |
|
| Obesity | Risk factors: ≥20 Gy cranial radiation, female gender | ||
| Hypothyroidism | Primary—direct neck radiation ≥10 Gy Central hypothyroidism—cranial dose >35 Gy Dose-response relationship with no plateau in incidence observed after neck radiation |
||
| Thyroid cancer | Risk factors: radiation dose 15-30 Gy, young age at treatment, female gender | ||
| Brain tumors | The most common pathologic processes are meningioma and glioma. Risk increases with increasing dose. |
||
| Head and neck carcinoma | Parotid gland carcinoma most common; secondary head and neck carcinoma Risk of salivary gland carcinoma increases linearly with dose. |
||
| Stroke | Mean cranial radiation dose ≥30 Gy increased risk for both leukemia and brain tumor survivors. Highest risk after cranial dose ≥50 Gy |
||
| Dental abnormalities | Risk factors: age at diagnosis <5 yr, higher-dose radiation | ||
| Chest irradiation (chest, mantle, lung, mediastinal, TBI) | Coronary artery disease | Increased risk with high-dose exposure | |
| Cardiac valve disease | Increased risk with high-dose exposure | ||
| Breast cancer | Risk factors: increasing radiation dose, age 10-30 years at diagnosis Latency: 10-15 years Ovarian failure reduces risk. |
||
| Lung fibrosis | Pulmonary—toxic chemotherapy an additional risk factor | ||
| Lung cancer | Greatest risk in Hodgkin lymphoma survivors Increased risk in smokers |
||
| Thyroid cancer | Risk factors: radiation dose 15-30 Gy, young age at treatment, female gender | ||
| Hypothyroidism | Risk factors: increasing radiation dose, older age at diagnosis, female gender No plateau in incidence observed over time |
||
| Abdominal irradiation (abdominal, periaortic, flank) | Gastrointestinal cancer | Risk factors: dose >30 Gy; concurrent treatment with alkylating agents; increasing radiation dose and increasing radiation volume | |
| Pelvic irradiation (pelvic, inverted “Y,” TBI) | Genitourinary cancer | Modestly increased risk overall; greatest risk for cancers of the female genital tract, bladder cancer, and renal cell carcinoma Risk factors: renal cell carcinoma renal irradiation, platinum-based chemotherapy, primary diagnosis of neuroblastoma |
|
| Premature menopause | Risk factors: dose (≥1 to ≤20 Gy) and concurrent alkylating agent chemotherapy Pelvic radiation >10 Gy associated with ovarian failure Cryopreservation of oocytes or embryos is intervention to preserve fertility. |
||
| Male hypogonadism | Risk of irreversible azoospermia >2 Gy Higher dose associated with impaired testosterone production, >20 Gy Pretreatment semen cryopreservation and testicular sperm extraction are interventions to preserve fertility. |
Second cancers are the leading cause of treatment-related mortality in 5-year survivors. In the CCSS cohort, second cancers accounted for 13% of deaths overall and for 60% of deaths defined as treatment related. Most often, a new cancer diagnosed in a survivor can be associated with a prior treatment exposure, such as radiation therapy or alkylating agent chemotherapy. Genetic cancer predisposition may also contribute to a survivor's risk for subsequent cancers. In addition, survivors, like all aging individuals, develop cancers that are not related to prior treatment or known genetic predisposition and these cancers will become more prevalent as the childhood cancer survivor population ages. To date, there are no data that address the comparative morbidity and mortality from these adult-onset cancers and whether survivors will be compromised in their ability to receive or respond to known effective therapies.
Overall, the likelihood of a childhood cancer survivor being diagnosed with a second primary cancer is three to six times greater than the risk in the aged-matched general population. At 20 years after diagnosis, the cumulative incidence of second cancers in childhood cancer survivors is estimated at 3.2% to 4.2%. In the British Survivorship Cohort, 5% of survivors had developed a secondary cancer by 38 years of age; this cumulative incidence of cancer would be expected at age 54 in a comparable, nonsurvivor population. Clinical and demographic factors that increase the risk for second cancers include primary diagnosis, exposure to radiation, attained age, and chemotherapy with alkylating agents or epipodophyllotoxins. Diagnoses that confer the greatest risk for subsequent cancers include Hodgkin lymphoma (standardized incidence ratio [SIR], 8.7), Ewing sarcoma (SIR, 8.5), and retinoblastoma (relative rate [RR], 15).
Genetic predisposition for second cancers results from an inherited or spontaneous germline mutation in a known or presumed cancer susceptibility gene. Characteristic findings in family cancer predisposition syndromes are younger age at cancer diagnosis, cancer in two or more generations, two or more cancers in an individual, and rare forms of cancer in combination. An example of a rare cancer predisposition syndrome that is associated with pediatric malignancies is Li-Fraumeni syndrome, which is associated with germline mutations in the tumor suppressor gene TP53. It is inherited as an autosomal dominant trait and has a high penetrance with cancer risk of 50% by age 40 years. The cancers most commonly observed in Li-Fraumeni syndrome are soft tissue sarcomas, breast cancer, leukemia, osteosarcoma, adrenocortical cancer, and brain tumors.
Survivors with an underlying genetic predisposition for cancer are more susceptible to treatment-associated secondary malignancies. This is demonstrated in survivors of retinoblastoma who carry a mutation in the RB1 gene. Those with hereditary retinoblastoma treated with irradiation for their primary cancer have a cumulative risk for second cancers of 58% at 50 years, compared with 26% if not treated with irradiation. There are other rare genetic syndromes that are associated with an increased susceptibility to pediatric cancers and subsequent adult-onset secondary cancers, and increasing evidence suggests that a substantial percentage of children with cancer may have an underlying cancer predisposition syndrome that might inform risk for subsequent cancers. Genome-wide association studies of patients with and without secondary cancers may reveal polymorphisms associated with increased risk; for example, a study of Hodgkin lymphoma survivors who received irradiation identified two variants at genetic locus 6q21 that are associated with increased risk for a subsequent cancer. Further work in this field may determine which survivors should undergo more intensive surveillance or prophylaxis for secondary cancer. All survivors of childhood cancer should be assessed for risk for secondary cancer based on a possible cancer predisposition, with attention to the family history as it evolves, development of benign disorders (e.g., polyps or hamartomatous lesions), as well as assessment of the pediatric history, including the primary diagnosis and age at diagnosis. Referral for genetic counseling for survivors of childhood cancer is increasingly important, because recent studies suggest that early genetic diagnosis and subsequent tumor surveillance may result in early diagnosis of secondary cancers in patients with known cancer predisposition syndromes ( Box 72-2 ).
Cancer in first-degree relatives
Relatives with cancer at early age
Cancer in two or more generations
Individual with two or more cancers
Rare cancers in combination
Cancer in paired organs
Adrenal cortical carcinoma
Choroid plexus carcinoma
Melanoma
Pleuropulmonary blastoma
Renal cell carcinoma
Retinoblastoma
Rhabdoid tumor
Sarcoma
X-linked lymphoproliferative syndrome
Wiskott-Aldrich syndrome
Beckwith-Weidemann syndrome
WAGR/Denys-Drash syndrome
Hereditary leiomyomatosis and renal cell carcinoma
Familial adenomatous polyposis
Juvenile polyposis syndrome
Peutz-Jeghers syndrome
Cowden syndrome
Bannayan-Riley-Ruvalcaba syndrome
Von Hippel-Lindau disease
Hereditary paraganglioma–pheochromocytoma
Nevoid basal cell carcinoma
Noonan syndrome
Blooms syndrome
Diamond-Blackfan anemia
Fanconi anemia
Ataxia-telangiectasia
Neurofibromatosis
Tuberous sclerosis
Carney complex
Xeroderma pigmentosum
Turcot syndrome
Rubenstein-Taybi syndrome
Simpson-Golabi-Behmel syndrome
Costello syndrome
ATM
TP53
APC
RB1
WT1
PTCH
MLH1, MLH2
BRCA1, BRCA2
NF1, NF2
MEN1, MEN2
DICER-1
PTEN
VHL
Dysmorphic features
Skin lesions
Hemihypertrophy
Cancer that develops in a prior radiation field is the most common type of second cancer observed in survivors. Risk estimates for second cancers have been reported from populations of survivors treated with irradiation during historic treatment eras when the modes of radiation therapy routinely used in clinical practice were different than current practices. In current oncology practice, orthovoltage radiation has been eliminated, thus reducing radiation doses to nontumor tissues such as skin, bones, and soft tissue. Large-dose extended-field radiation therapy is increasingly being replaced by involved-field lower-dose radiation therapy or conformal radiation therapy, often in combination with chemotherapy. It is assumed that this change in clinical practice aimed at reducing exposure to radiation will result in a lower incidence of radiogenic cancer; however, no “safe” dose of therapeutic radiation has been established and irradiation-associated cancers have been observed at what would be considered the lowest treatment doses. In general, risk factors for irradiation-associated second cancers include treatment with radiation doses greater than 30 Gy, radiation in combination with alkylating agent chemotherapy, young age at exposure, more than 10 years beyond treatment, and the presence of a cancer predisposition syndrome. Of particular concern is the observation that the cumulative incidence of irradiation-associated cancers does not plateau in groups of survivors followed for up to 50 years after their therapy for childhood cancer. Second cancer risk is modulated by lifestyle choices; for example, adult survivors of Hodgkin lymphoma who smoke after exposure to chest irradiation have a 20-fold greater risk for secondary lung cancer compared with survivors who are nonsmokers.
All tissues and organs are vulnerable to cancer induction by exposure to radiation. However, some tissues, such as thyroid and breast tissue, have greater sensitivity to radiation. Excluding low-grade nonmelanomatous skin cancer and (benign) meningiomas, the most frequently reported irradiation-associated second cancers in 5-year survivors of childhood cancer followed in the CCSS are, in order, breast cancer, thyroid cancer, CNS cancers, soft tissue sarcomas, and bone sarcomas. Additional irradiation-associated second cancers reported in survivors, especially with longer follow-up intervals, include carcinomas of the head and neck (primarily parotid gland), colon cancer and other gastrointestinal cancers, lung cancer, and carcinomas of the genitourinary tract. The most common second cancers observed in childhood cancer survivors are described next.
Breast cancer is one of the most frequently diagnosed irradiation-associated second cancers in childhood cancer survivors. Women treated with mantle, mediastinal, chest, spinal, whole-lung, and total-body irradiation during childhood or adolescents are at risk for secondary breast cancer. Large cohort studies of childhood Hodgkin lymphoma survivors report a fifteen- to thirtyfold increased risk for irradiation-associated secondary breast cancer compared with the age-matched general population. Risk estimates vary by characteristics of the cohort, including radiation dose, age at therapy, and duration of follow-up. The cumulative incidence of secondary breast cancer is as high as 12% to 35% at 20 years after therapy for Hodgkin lymphoma, and the incidence does not plateau with longer duration of follow-up.
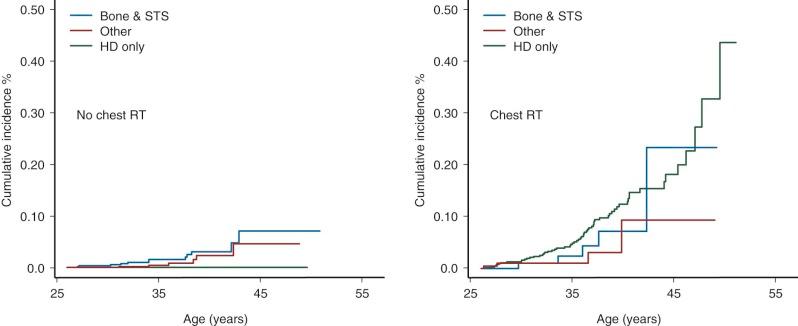
Female survivors at greatest risk for secondary breast cancer are those treated between the age of 10 and 30 years with chest radiation doses greater than 20 Gy. Studies have demonstrated a linear dose-response relationship between radiation dose and risk for secondary breast cancer. The typical latency of irradiation-associated breast cancer is 10 to 15 years after therapy; however, secondary breast cancer has been reported in women as young as 20 years of age and as soon as 4 years after primary diagnosis. Secondary breast cancer is most often associated with chest irradiation for Hodgkin lymphoma; however, it is important to recognize that women treated with chest irradiation for any childhood cancer diagnosis have increased risk for subsequent breast cancer, as illustrated in Figure 72-4 . Survivors of primary sarcomas not treated with chest irradiation also have an increased risk for secondary breast cancer (RR, 7). Interestingly, survivors with therapy-induced ovarian dysfunction have a relative decreased risk for irradiation-associated breast cancers compared with survivors with normal ovarian function. Although very rare, sporadic cases of male breast cancer have been reported in men treated with whole-lung irradiation as children.
The most common type of breast cancer diagnosed in survivors is invasive ductal carcinoma; adverse biologic features (e.g., hormone-receptor negativity) may be more common in these childhood cancer survivors than in the general population. Similar to findings in the general population, secondary breast cancer is detectable by radiographic imaging and has an excellent prognosis when treated in the earliest stages. Breast cancer treatment options for survivors, however, can be limited by the therapy received for their childhood cancer. Specifically, prior anthracycline exposure and concern for potential cardiotoxicity may limit the use of adjuvant systemic chemotherapy with doxorubicin and the concern for tissue necrosis with repeated exposure to chest irradiation limits the option of breast-conserving surgery for some women.
Current screening recommendations for childhood cancer survivors treated with chest radiation published by the Children's Oncology Group include monthly self-breast examination, annual clinical breast examination, and annual breast magnetic resonance imaging (MRI) and mammography starting 8 years after treatment or age 25 whichever comes last. Guidelines published by the American Cancer Society also advocate mammography and annual breast MRI, but suggest MRI only for women treated with chest irradiation between the ages of 10 and 30 years. The addition of MRI to mammography has been reported to increase the sensitivity of breast cancer screening, although an impact on breast cancer outcomes has not been described ( Table 72-2 ).
| Treatment Risk Factors | Clinical Evaluation | Special Considerations | |
|---|---|---|---|
| Breast Cancer | Any chest irradiation Spinal irradiation TBI |
Monthly breast self-examination Biannual clinical breast examination Breast MRI Mammogram |
Current recommendations are to begin annual radiologic screening 8 years after irradiation or age 25 years, whichever occurs last. |
| CNS Tumor | Cranial irradiation Head /neck irradiation TBI |
Annual neurologic examination Head MRI |
Imaging studies are indicated for new or persistent neurologic symptoms. |
| Colorectal Cancer | Any abdominal irradiation Pelvic irradiation Spinal irradiation TBI |
Colonoscopy Computed tomographic colonoscopy (CTC) |
Current recommendations are to begin colonoscopy 10 years after radiation or age 35, whichever occurs last. CTC is not universally recommended as an alternative to colonoscopy in high-risk populations. |
| Thyroid Cancer | Neck irradiation Chest irradiation TBI MIBG |
Annual clinical thyroid examination Thyroid ultrasound evaluation |
Routine ultrasound screening is not currently recommended but should be considered for survivors with difficult clinical examination. |
| Skin Cancer | Any irradiation | Annual skin cancer screening Monthly skin self-examination |
Practicing skin cancer prevention has potential to reduce risk. |
Irradiation of the head and neck and upper thorax, total-body irradiation, and treatment with radioactive iodine (e.g., with 131 I-labeled-metaiodobenzylguanidine [MIBG]) place childhood cancer survivors at risk for subsequent thyroid cancers. Large cohort studies of childhood cancer survivors estimate relative risks for secondary thyroid cancer of between 4 and 36, with a cumulative incidence of 1.3% at 30 years reported for female survivors and 4.4% in Hodgkin disease survivors. Well-differentiated papillary carcinoma is the most common pathologic process (63% to 80%); however, follicular carcinomas are also observed. The minimum observed latency period for secondary thyroid carcinoma is 5 years, although cases have been reported closer to the time of original diagnosis. At 20 years of follow-up, the relative risk for thyroid carcinoma remains increased and a plateau in incidence has not been observed beyond 40 years of follow-up. The risk for thyroid cancer is related to radiation dose; but unlike most other radiation-induced second cancers, the risk for thyroid cancer is greatest at lower doses of 15 to 30 Gy and beyond 30 Gy there is a decline in risk. This finding demonstrates that thyroid tissue has enhanced sensitivity to radiation toxicity and supports the “cell kill” hypothesis that suggests higher doses of radiation cause cell death, which reduces the initiation of carcinogenesis observed at lower doses. Although there is conflicting evidence, chemotherapy does appear to modify risk for irradiation-associated secondary thyroid cancer when the radiation dose is less than 20 Gy. Female gender and young age at treatment are independent risk factors for secondary thyroid cancer. Survivors of neuroblastoma treated with 131 I-MIBG are also at risk for subsequent thyroid cancer. In a single-institution case series of 16 neuroblastoma survivors treated with 131 I-MIBG and no external-beam irradiation, followed for a median of 15 years, 9 of 16 had nonpalpable thyroid nodules detected on thyroid ultrasonography, 6 of the 9 went on to biopsy, and 2 of those 6 were diagnosed with papillary thyroid carcinoma.
Radiation-induced thyroid cancer in young survivors has an excellent prognosis; therefore many experts have recommended clinical screening. Appropriate screening schedules for secondary thyroid cancers and recommended modality for screening are controversial. At a minimum, annual palpation of the thyroid for nodules by an experienced examiner is recommended. Routine screening to detect subclinical thyroid nodules with high-resolution ultrasonography has been recommended by some investigators but remains controversial. Ultrasound screening has the benefit of detecting smaller nonpalpable nodules but has the consequence of false-positive findings and potential for unnecessary biopsies. Thyroid nodules do have ultrasound characteristics that are of concern for malignancy (hypoechogenicity, irregular margins, microcalcification). However, these findings are not diagnostic and fine-needle aspiration of nodules larger than 1.0 cm or with suspicious features is usually necessary to evaluate for malignancy. Serial ultrasonography is then recommended to monitor thyroid nodules that are small or benign on biopsy. Although clinical practice is moving toward using ultrasound to screen asymptomatic high-risk survivors for thyroid cancer, screening should be considered only after a discussion of the potential risks and benefits (see Table 72-2 ).
In general, irradiation-associated thyroid cancer is treated the same as other thyroid cancers and has an excellent prognosis. Thyroid surgery is indicated for nodules that are enlarging, are of indeterminate pathology on fine-needle aspiration, or are positive on fine-needle aspiration for malignancy. Total thyroidectomy is often recommended to survivors because irradiation-associated thyroid cancers can be multicentric and because benign nodules can accompany clinically undetectable malignant lesions. Finally, there is indirect evidence to support that exogenous thyroid hormone use reduces the risk for secondary thyroid cancer by suppressing thyroid stimulating hormone (TSH)-induced proliferation of thyroid nodules. Although not proven to reduce risk for thyroid cancer, the use of exogenous thyroid hormone to suppress thyroid proliferation is supported by data that show a decrease in incidence of new thyroid nodules in patients treated with exogenous thyroid hormone after partial thyroidectomy (34% vs. 14%).
Survivors treated with radiation are at increased risk for secondary cancer of the bone and soft tissue in the radiation field. Although secondary sarcomas are most often associated with irradiation, survivors of primary sarcoma and hereditary retinoblastoma who have not had prior radiation therapy also have an increased risk, suggesting a genetic predisposition. Risk estimates for secondary sarcoma vary by type of sarcoma and composition of the study cohort. The CCSS cohort, which did not include survivors of retinoblastoma, reports an overall ninefold increased risk for secondary sarcomas and an absolute excess risk of 32.5 per 100,000 person-years. Secondary sarcomas occurring after childhood cancer include multiple histologic subtypes such as osteosarcoma, nonrhabdomyosarcoma soft tissue sarcomas, primitive neuroectodermal tumors (Ewing sarcoma), and malignant peripheral nerve sheath tumors, as well as rarer sarcoma subtypes. The median latency for secondary sarcomas is 11 years, with increased risk persisting beyond 20 years. Reported risk factors for subsequent sarcomas include higher doses of radiation, primary diagnosis of sarcoma or hereditary retinoblastoma, younger age at diagnosis, alkylating agent exposure, anthracycline exposure, and family history of sarcoma. A nested case-control study of secondary sarcomas in the CCSS cohort identified a dose-response relationship between radiation dose and risk for secondary sarcomas, with elevations in risk ratios with higher radiation doses: 10 to 29.9 Gy (odds ratio [OR], 15.6; 95% CI, 4.5 to 53.9), 30 to 49.9 Gy (OR, 16.0; 95% CI, 3.8 to 67.8), and more than 50 Gy (OR, 114.1; 95% CI, 13.5 to 964.8). Risk factors other than irradiation associated with increases in risk for secondary sarcoma in this study included primary cancer diagnosis of sarcoma or Hodgkin lymphoma and anthracycline exposure.
For survivors of hereditary retinoblastoma treated with irradiation, the risk for subsequent bone sarcomas is as high as 400-fold with a cumulative incidence at 20 years of 14.1% and the relative risk for soft tissue sarcomas is 140 with 50-year cumulative incidence of 13%. Radiation exposure and underlying genetic predisposition both contribute to risk for secondary sarcomas in retinoblastoma survivors.
Routine radiographic screening for secondary sarcomas is currently not recommended. Survivors at risk for secondary sarcomas should be counseled to report new pain, lesions, or masses in the radiation field and should be promptly evaluated for any signs or symptoms suggestive of a secondary sarcoma. As survivors enter follow-up care, providers should consider obtaining baseline imaging of any previously irradiated site, so these studies are then available for comparison should symptoms suggestive of a new malignancy develop. There is no established role for secondary sarcoma surveillance for survivors of hereditary sarcoma predisposition syndromes (Li-Fraumeni syndrome, hereditary retinoblastoma), although the role of whole-body MRI is currently under investigation.
Melanoma and nonmelanomatous skin cancers are reported with increased incidence in survivors. The relative risk for melanoma is 2.5 to 9.0 in childhood cancer survivors, with a median latency of 15 to 18 years. Survivors of hereditary retinoblastoma, familial melanoma syndromes, and those with a prior history of melanoma all have an increased risk for subsequent melanoma independent of irradiation. Although the association between therapeutic radiation and melanoma is not firmly established, a case-control study of 16 survivors with secondary melanoma in a European cohort of 4000 childhood cancer survivors found an association between secondary melanoma and exposure to more than 15 Gy of radiation. In contrast, basal cell carcinomas and squamous cell carcinomas are known to be more common in radiation-exposed survivors (RR, 6.3), with 90% of all nonmelanomatous skin cancers diagnosed in previously irradiated fields. A linear dose-response relationship is described for basal cell carcinomas, with an excess odds ratio of 1.09 per Gy of radiation. Also of note, these low-grade skin cancers can be recurrent, and almost half of survivors diagnosed will have multiple lesions. The prognosis for secondary skin cancers is excellent with early diagnosis; therefore routine screening with skin examinations is recommended. Because ultraviolet radiation from the sun is known to contribute to skin cancer risk; patients should be routinely educated about preventive strategies such as aggressive sun exposure protection (see Table 72-2 ).
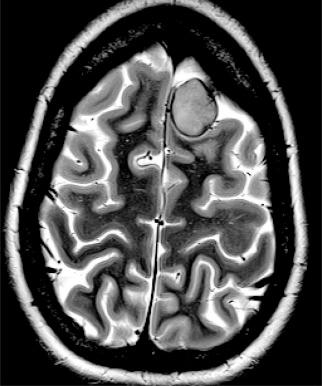
Past exposure to cranial irradiation is considered the most important risk factor for the development of subsequent CNS tumors in survivors of childhood cancer. The most common pathologic processes include meningioma ( Fig. 72-5 ) and glioma; however, other tumors such as primitive neuroectodermal tumor or medulloblastoma have been reported. In a report from the British Childhood Cancer Survivor Study, the standardized incidence ratio for development of a subsequent glioma was 10.8 (95% CI, 8.5 to 13.6), and in the CCSS cohort it was 8.7 (95% CI, 6.2 to 11.6). Higher standardized incidence ratios have been reported for meningioma, and meningioma is the most common subsequent CNS tumor 10 years or more after a childhood cancer diagnosis. There is an established dose-response relationship between cranial radiation dose and incidence of secondary CNS tumors. In the CCSS cohort, Neglia and colleagues reported an excess relative risk of 1.06 per Gy of cranial irradiation for meningiomas and 0.3 per Gy for gliomas. In the British Childhood Cancer Survivor Study cohort, Taylor and colleagues reported that the risk for glioma and for meningioma each increased linearly with increasing radiation dose. Several studies have suggested that the increased risk for development of meningioma does not appear to plateau. In a report from the CCSS, among survivors with no previous diagnosis of meningioma at 25 years after a primary CNS tumor, the cumulative incidence of meningioma at 30 years was 3.5% (95% CI, 0.9% to 6.1%). The contribution of chemotherapy to the risk for CNS malignancies is controversial. Laboratory investigations have suggested an association between radiation-induced brain tumors and thiopurine-based chemotherapy related to a deficiency in the enzyme thiopurine methyltransferase (TPMT). In the British Childhood Cancer Survivor Study cohort, a higher cumulative dose of intrathecal methotrexate was associated with the development of meningioma. In the CCSS cohort, after adjusting for radiation dose, chemotherapy exposure did not alter the survivor's secondary brain tumor risk.
The role of routine surveillance for secondary CNS tumors with neuroimaging in asymptomatic childhood cancer survivors requires further investigation. Single-institution series of neuroimaging screening have reported high rates of meningioma. For example, in a prospective study of 76 survivors of acute lymphoblastic leukemia that was treated with cranial irradiation and who were screened with MRI every 3 to 6 years for 20 years, Goshen and colleagues detected 16 meningiomas (15 asymptomatic) and one glioma. Cumulative incidence in this screened population was 14.8% at 20 years. Surgical resection of these secondary CNS tumors was recommended for 12 of the 16 survivors, with one surgical complication reported. Whether early detection of meningiomas in asymptomatic survivors might reduce morbidity and minimize neurologic complications by facilitating surgical intervention remains to be determined. Survivors with a prior history of cranial irradiation should be educated about the potential for late-occurring CNS tumors and instructed to report new or persistent neurologic signs or symptoms (see Table 72-2 ).
Secondary carcinomas of the gastrointestinal tract, genitourinary organs, lung, and head and neck region are observed in survivors of childhood cancer and are associated with radiation exposure and longer follow-up times. In general, irradiation-associated carcinomas (like colon cancers) occur at an earlier age than is seen in the general population, thereby supporting recommendations for early initiation of cancer screening and aggressive evaluation of symptoms suggestive of possible secondary malignancy.
Large cohorts of childhood cancer survivors report relative risks for gastrointestinal cancers between 4.6 and 7.0. A European cooperative cohort study found the risk for secondary gastrointestinal malignancies greatest after abdominal radiation dose greater than 30 Gy (SIR, 9.7); however, lower-dose radiation was also associated with increased risk (10 to 29 Gy, SIR 5.2). Alkylating agent chemotherapy is consistently found to be independently associated with an increased risk for gastrointestinal cancer. The most common irradiation-associated secondary gastrointestinal malignancy is colorectal cancer, with a standardized incidence ratio of 3.6 to 13 and as high as 63.4 (95% CI, 15.7 to 71.8) reported in a cohort of Hodgkin lymphoma survivors. In a British cohort of 18,000 childhood cancer survivors, the 50-year cumulative incidence of colorectal cancer for those treated with direct abdominal radiation was 1.4% (95% CI, 0.7 to 2.6). The St. Jude Children's Research Hospital cohort of over 13,000 childhood cancer survivors found a 40-year cumulative incidence of secondary colorectal cancer of 1.4% ± 0.53%). In this study, the risk for colorectal cancer increased by 70% with each 10-Gy increase in radiation dose and increasing radiation volume also significantly increased risk. Current recommendations for screening of survivors treated with abdominal radiation therapy are to begin colon cancer screening earlier than what is recommended for the general population (10 years after completing radiation therapy or age 35 years, whichever comes last), although the benefit of early surveillance has not be established in this high-risk population (see Table 72-2 ).
Of note, gastric cancers and esophageal cancers are also observed in greater numbers than expected for age in survivors of pediatric Hodgkin lymphoma. Common symptoms such as dysphagia and dyspepsia should be evaluated aggressively, with a low threshold for utilizing endoscopy or imaging to rule out malignant or premalignant conditions in exposed survivors.
Overall, the relative risk for genitourinary cancer is modestly elevated (SIR, 1.9; 95% CI, 1.6 to 2.4), with elevated relative risks for secondary malignancies of the female genital tract (SIR, 2.1; 95% CI, 1.4 to 3.2), secondary renal cell carcinoma (SIR, 8.0; 95% CI, 5.2 to 11.7), and secondary bladder cancer (SIR, 5.1; 95% CI, 2.1 to 12.4). Data from the CCSS show the risks for secondary renal carcinoma are primary diagnosis of neuroblastoma (SIR, 85.8; 95% CI, 38.4% to 175.2%), renal-directed radiation therapy of 5 Gy or greater (RR, 3.8; 95% CI, 1.6 to 9.3), and platinum-based chemotherapy (RR, 3.5; 95% CI, 1.0 to 11.2). Secondary urinary bladder cancer is associated with both radiation therapy and cyclophosphamide chemotherapy, with the risk dependent on dose and duration of therapy. An adult series of more than 6000 non-Hodgkin lymphoma survivors treated with cyclophosphamide reported 31 cases of bladder cancer (RR, 4), and no significantly increased risk was observed at doses less than 20 g/m 2 . In a British cohort of 18,000 childhood cancer survivors, 17 were diagnosed with bladder cancer (RR, 4); risk factors were diagnosis of hereditary retinoblastoma, treatment with chemotherapy, male gender, and longer follow-up. In another series of adults treated with prolonged cyclophosphamide for nonmalignant disease, 5% developed secondary bladder cancer at a median of 8.5 years and all diagnoses were preceded by symptoms of microscopic hematuria. Although the absolute excess risk for bladder cancer in childhood cancer survivors is low, routine monitoring with urinalysis of survivors exposed to pelvic radiation, large cumulative dose of cyclophosphamide, and those with hereditary retinoblastoma should be considered.
Cancer of lung and bronchus is diagnosed more commonly in childhood cancer survivors than the general population (SIR, 3.4; 95% CI, 1.9 to 6.1), with greater risk observed in cohorts of pediatric Hodgkin lymphoma survivors (SIR, 5.1 to 27.2). In a meta-analysis of secondary lung cancer in Hodgkin lymphoma survivors, the largest risk for secondary lung cancer was observed among patients diagnosed age 15 to 24 years (RR, 8.76; 95% CI, 4.55 to 16.89). Treatment with alkylating agents and irradiation are both associated with increased lung cancer risk. In addition, studies of adult survivors of Hodgkin lymphoma have shown that smoking increased lung cancer risk more than twentyfold. Aggressive smoking cessation interventions and routine surveillance with radiographic imaging have been suggested for this high-risk population of survivors, although the use of spiral computed tomography has not been studied in the survivors who had chest irradiation.
Survivors are also at increased risk for secondary head and neck carcinomas (SIR, 10.8 to 14.1), with mucoepidermoid carcinoma of the parotid gland the most frequently observed diagnosis. In a CCSS analysis of secondary salivary gland carcinomas, the incidence was thirty-ninefold higher in survivors compared with the general population (95% CI, 25.4 to 57.8). The analysis also demonstrated that risk increased linearly with radiation dose (excess RR, 0.36/Gy; 95% CI, 0.06 to 2.5). Interestingly, modifiable health behaviors including cigarette smoking and alcohol intake were not associated with increased risk for head and neck cancers in childhood cancer survivors.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here