Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although the aetiology of most liver diseases can be identified by currently available biological tests, and although the diagnosis of a liver mass can be approached by imaging techniques, histological evaluation continues to be integrated into the management of most hepatic diseases. Light microscopic examination of a liver sample, usually after a biopsy procedure, provides details that cannot be obtained by other means. Therefore liver biopsy remains central to the evaluation of liver diseases. Not only are cases of undefined liver disease subjected to histological analysis, but more importantly, the effects on the liver of noxious agents, whether of viral, chemical, autoimmune or metabolic origin, require accurate histological evaluation relevant to the prognosis of the patient and to indications for cost-intensive and potentially side effect-prone therapies. Management of liver transplant patients necessitates regular histological evaluation for identification of possible complications and adequate treatment in this delicate setting. , Liver biopsy may also provide important clues to the aetiology of unclear space-occupying lesions and suspected drug toxicity. Box 2.1 summarizes the most common reasons for practising liver biopsy.
Abnormal liver blood tests
Evaluation of diagnosis, grade and stage of chronic liver disease
Evaluation of therapeutic efficacy in chronic liver disease
Unexplained cholestatic liver disease
Unexplained portal hypertension
Suspected drug injury
Fever of unknown origin, systemic disease
Suspected hepatic neoplasm and classification
Post-liver transplantation: evaluation of rejection, recurrence of initial disease, any other complications
The quality and quantity of information provided by a liver biopsy are highly dependent on sampling and tissue-processing techniques. In addition to the identification of pathological features that rely on pattern recognition after standard histological staining, liver biopsy can provide a great deal of additional information through recently implemented cellular and molecular techniques. This chapter reviews in detail both the routine and the advanced cellular and molecular techniques that can be undertaken.
Liver biopsy is a time-honoured procedure; its history spans more than a century, after Ehrlich first proposed a liver puncture for assessing glycogen content in the liver of a diabetic patient. The technique was used a few years later by Lucatello to drain a tropical abscess of the liver. At that time, liver tissue was mainly obtained for biochemical rather than morphological studies. Its first application for the diagnosis of cirrhotic liver disease in humans and rats was published in a series by Schüpfer in France in 1907, and its diagnostic potential was expanded by Bingel in Germany in 1923. In 1938 the Vim–Silverman needle was introduced, but it was the introduction of the Menghini needle that boosted the development of liver biopsy for use in clinical hepatology, both because it was safer and because it provided tissue of sufficient quality to support light microscopic and ancillary studies. Since that time, the method of sampling has been diversified to encompass not only different needle types for cutting and aspiration but also different routes and combinations, through imaging modalities such as ultrasound (US), computed tomography (CT) and laparoscopy ( Box 2.2 ).
Percutaneous biopsy: diffuse liver disease
Transvenous biopsy: diffuse chronic or acute liver disease with coagulation disorders
Wedge/laparoscopic biopsy: focal lesion, subcapsular
Ultrasound-guided biopsy: focal lesion
Expanded use of liver biopsy by hepatologists and gastroenterologists greatly increased our understanding of the physiopathology of liver diseases; indeed, liver biopsy itself has contributed to major landmarks in hepatology. The development of techniques in molecular pathology and the implementation of novel optical approaches have further increased the quantity (and quality) of information provided by liver biopsy. However, it remains an invasive procedure with possible adverse events and limitations. Although liver biopsy still belongs to the armamentarium of hepatologists, the development of noninvasive diagnostic procedures, such as novel blood tests and new imaging procedures, has recently fuelled discussions concerning the respective roles of liver biopsy and noninvasive alternatives. ,
Furthermore, the development of new antiviral drugs that may definitively eradicate chronic viral hepatitis such as hepatitis C virus (HCV) or stop viral replication as with hepatitis B virus (HBV), yet have few or no side effects, strongly reduces the need for liver biopsy to assess liver damage.
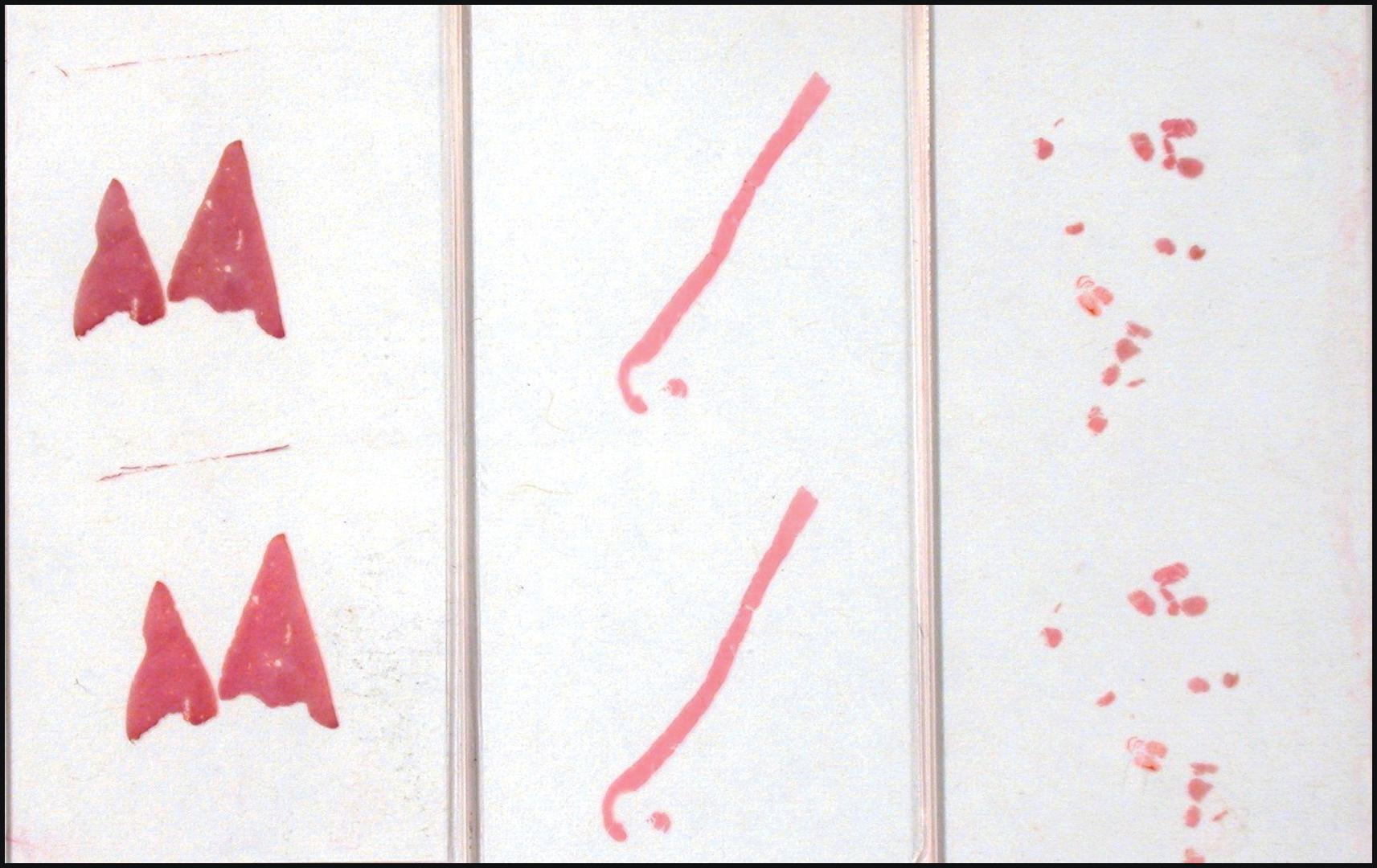
A liver sample can be obtained with a needle, either by cutting or by aspiration. The needle can proceed percutaneously, via an intercostal or subcostal route of penetration, or by using a transvenous approach, usually via the jugular vein, and then anatomically proceeding toward the hepatic veins. In the case of a focal lesion, US or CT guidance as well as visual guidance during laparoscopy are additional options. , Each of these methods has its advantages and disadvantages, providing samples of different shape and size ( Fig. 2.1 ). To avoid an unnecessary procedure, the goal of the biopsy should be determined before deciding on the method.
Percutaneous liver biopsy is performed with the patient in the supine position, the right hand behind the head. The extent of the liver is examined by percussion. It is customary to perform an abdominal US before percutaneous liver biopsy, which enables localization of the gallbladder and confirms the absence of dilated bile ducts, venous collaterals or anomalies in the chosen path of penetration. , After local anaesthesia, a skin incision is made. Using an aspiration device (Menghini needle), steady suction is applied to the syringe connected to the needle, and the patient is asked to exhale fully. The needle is then advanced into the liver and rapidly withdrawn. Using a cutting needle (Tru-Cut biopsy), the tissue is obtained by cutting a specimen lodged in a nichein the obturator needle by a second cylindrical needle sliding over it. The needle is advanced into the liver, the sliding mechanism is triggered manually or automatically (‘biopsy gun’), and the needle is then withdrawn from the liver. The cutting needle remains in the liver longer, but it has been shown to produce superior tissue specimens. The biopsy can be repeated by several passages through the same incision if the biopsy fragment is considered too small but increasing the number of passages is associated with an increased risk of complications if more than three passages are performed. ,
Percutaneous liver biopsy is an invasive procedure with a range of adverse events and limitations ( Box 2.3 ). Minor complications include transient and moderate pain, along with commonly reported anxiety and discomfort (5–20%), while vasovagal episodes are infrequent. Severe complications such as haemoperitoneum, biliary peritonitis and pneumothorax are rare (0.3–0.5%). , The risk of haemorrhage in percutaneous liver biopsy depends on several factors, including age and the presence of malignant tumours. , As with any invasive procedure, the risk of complications is influenced by the experience of the operator. In patients with coagulation disorders, an alternative procedure is recommended, and percutaneous liver biopsy coupled with embolization of the puncture canal (plugged biopsy) has been shown to be a safe procedure. Death after percutaneous biopsy is rare (between 0.1% and 0.01% according to the literature) but has been reported with biopsy in patients with advanced liver disease, haemorrhagic tumours and major comorbidities. , The type of needle used is also a factor in reported complications, with a higher incidence of haemorrhage, pneumothorax, biliary leakage and peritonitis using cutting needles, and puncturing of other internal organs and sepsis using Menghini needles. Whether the diameter of the needle is a factor predisposing to haemorrhage is controversial. When deciding whether to use Menghini or cutting needles, the clinician should remember that smaller needles and smaller specimens may increase the number of passages or necessitate repuncture, with an increased risk of bleeding, to obtain representative tissue. For diffuse liver disease, a 16-gauge needle (internal diameter of cylinder, 1.2 mm) is typically preferred.
Percutaneous liver biopsy is contraindicated in patients with severe coagulation disorders caused by hepatic or other diseases, since haemorrhage is the most dangerous complication. Because these patients are nevertheless frequent candidates for histological assessment, another approach, transvenous liver biopsy, was developed. Liver biopsy by this method is usually obtained via the transjugular route. Technically, the internal jugular vein is cannulated and a sheath inserted according to the technique of Seldinger. A catheter is then guided through the right atrium into the inferior vena cava. After loading it with the transvenous biopsy needle, the catheter is advanced into one of the hepatic veins, which is visualized by injection of contrast medium. The needle is rapidly advanced 1–2 cm beyond the tip of the venous catheter, and suction is applied during liver passage. Liver tissue can subsequently be recovered from the needle. , Transvenous liver biopsy is generally limited to patients with significant coagulation disorders, in whom liver histology is likely to alter therapeutic management.
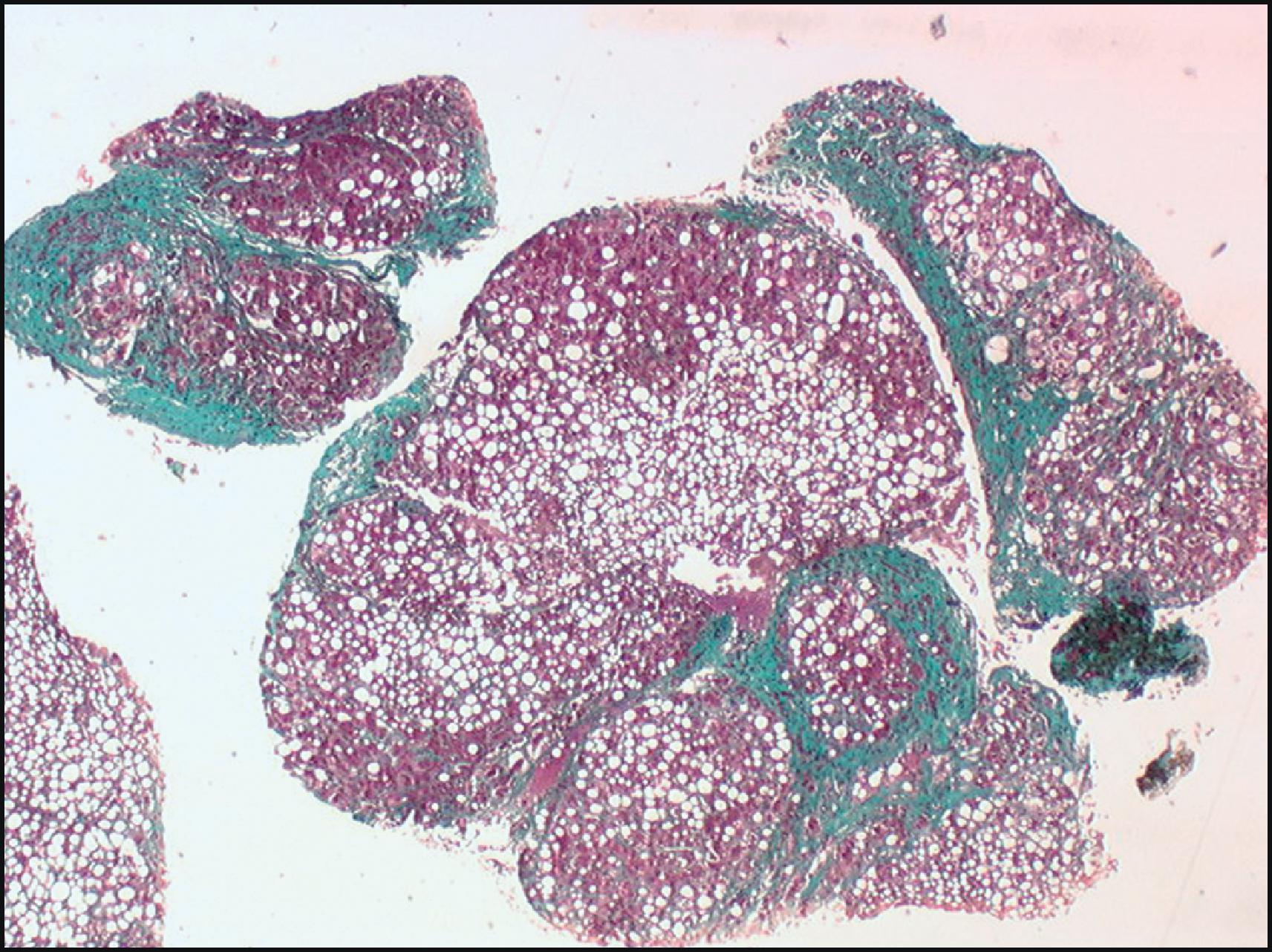
The primary disadvantages of transvenous liver biopsy are the considerable materials and experience required, with a complex setup and heavy workload generating a significant cost. There is a theoretical risk of arrhythmia and of contrast material-related reactions, in addition to the use of x-rays, although it is generally considered to be a safe procedure. In addition, the liver sample is usually smaller than transcutaneous liver biopsy and is fragmented, although a recent study showed that this approach provides samples adequate for accurate histological interpretation ( Fig. 2.2 ). A major advantage is that the transjugular route allows simultaneous measurement of blood pressure and assessment of the hepatic venous pressure gradient (HVPG) during the same procedure, which may be useful for predicting prognosis in cirrhosis, assessing the diagnosis of noncirrhotic portal hypertension and developing the management strategy.
Laparoscopic liver biopsy is an alternative route for obtaining a liver biopsy during visual assessment of the peritoneum and the abdominal organs. After a significant decline, laparoscopic liver biopsy has again attracted attention because of the development of minimally invasive minilaparoscopy. With this approach, visual inspection of the cranial and inferior liver surface is performed, and lesions of the left lobe, the dome of both lobes, the undersurface of the liver and the caudate and quadrate lobes can be biopsied by the aspiration or cutting technique. Several studies have suggested that laparoscopy is the gold standard for diagnosis of liver cirrhosis, since both the nodular pattern and the increased tissue hardness assessed by direct palpation led to an increase in sensitivity. However, the sample size as well as frequent crush artefacts can make interpretation difficult.
US-guided fine-needle aspiration (FNA) is extensively used to obtain histological and cytological information in focal hepatic lesions. It is a well-accepted, safe, easy and accurate diagnostic tool for the diagnosis of liver masses. Endoscopic US-guided FNA biopsies are also employed, particularly for lesions in the left lobe of the liver, with the needle easily traversing the stomach wall. , For US-guided FNA, the hepatic lesion is visualized by real-time US and a path for needle aspiration plotted. A US probe with an integrated needle guidance slot is usually employed. A fine needle with a diameter of <1 mm is advanced into the lesion while patients hold their breath, suction is applied with a syringe connected to the needle, and after three to five passages within the mass, the needle is withdrawn from the liver.
The reliability and efficiency of FNA also depend on management of the specimen. The aspirated material is expelled with the help of a syringe filled with air into appropriately labelled glasses. The material is spread over several glass slides. Smears should be air-dried and fixed immediately in an alcohol solution so that staining can be performed for rapid cytological examination ( Fig. 2.3 ). The presence of a technologist or cytopathologist in the radiology/procedure room or by other remote digital methods increases the overall accuracy of the procedure, enabling immediate verification of the adequacy of the material while final diagnosis is made after complete evaluation of smears, cell blocks and needle biopsy material. ,
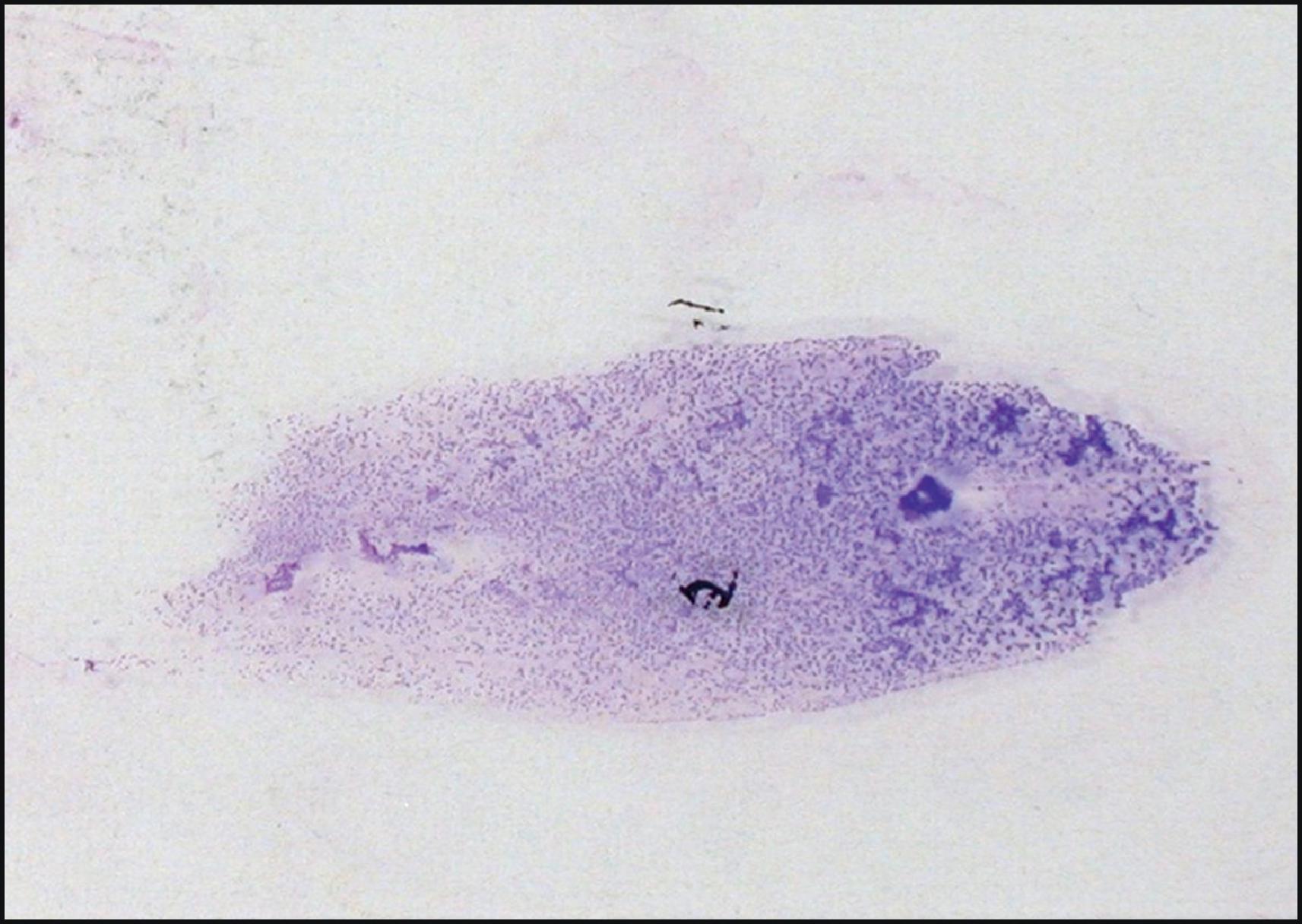
Small tissue fragments for cell blocks are best obtained by cytocentrifugation of the material obtained from an additional biopsy pass. This has been fully injected into a fixative (typically formalin) to provide adequate material to be handled as a routine microbiopsy sample using formalin fixation with paraffin embedding (FFPE) and sectioning. This material will enable evaluation of tissue architecture, special staining and use of additional techniques such as immunohistochemistry (IHC). US-guided biopsy can also be performed with larger needles, thereby obtaining a core specimen for standard histological evaluation.
Several studies have documented that the specificity of FNA cytology is excellent in the diagnosis of malignancy, with sensitivity as high as 93% and specificity approaching 100%. With respect to the biopsy approach, it was suggested that FNA and cutting-needle core biopsy each resulted in a diagnostic accuracy close to 80%, but when the two were combined, accuracy rose to 88%. , Based on these studies, FNA cytology was shown to be a safe and sensitive diagnostic procedure for liver masses.
As with any other type of biopsy, FNA has limitations and pitfalls. Sampling errors can occur, most often from inexact needle localization, targeting of small nodules <1 cm or the presence of areas of necrosis or fibrosis within the lesion. However, even in lesions with fibrosis, FNA samples can be more cellular and prove to be more diagnostic than small FFPE cores. Haemorrhage with FNA using needles <1 mm in diameter is rare. The mortality rate has been estimated at between 0.006% and 0.1%.
The potential seeding of cancer cells following FNA of a malignancy is a controversial issue. Seeding rates of biopsies obtained from abdominal organs have been estimated at <0.01%. However, in a retrospective study of hepatocellular carcinomas (HCCs), the rate was much higher, raising the question of the use of needle aspirations for this tumour. The use of a coaxial needle might significantly reduce the risk of seeding. Nevertheless, the issue of tumour cell seeding and its clinical relevance remains controversial and differs according to the lesion being biopsied.
In an intraoperative setting, wedge biopsy is generally useful for a previously unknown focal lesion that is identified at, or immediately below, the capsule. Interpretation of a wedge biopsy may be difficult when too small a biopsy is obtained, especially if the liver is sampled tangentially to the capsule surface.
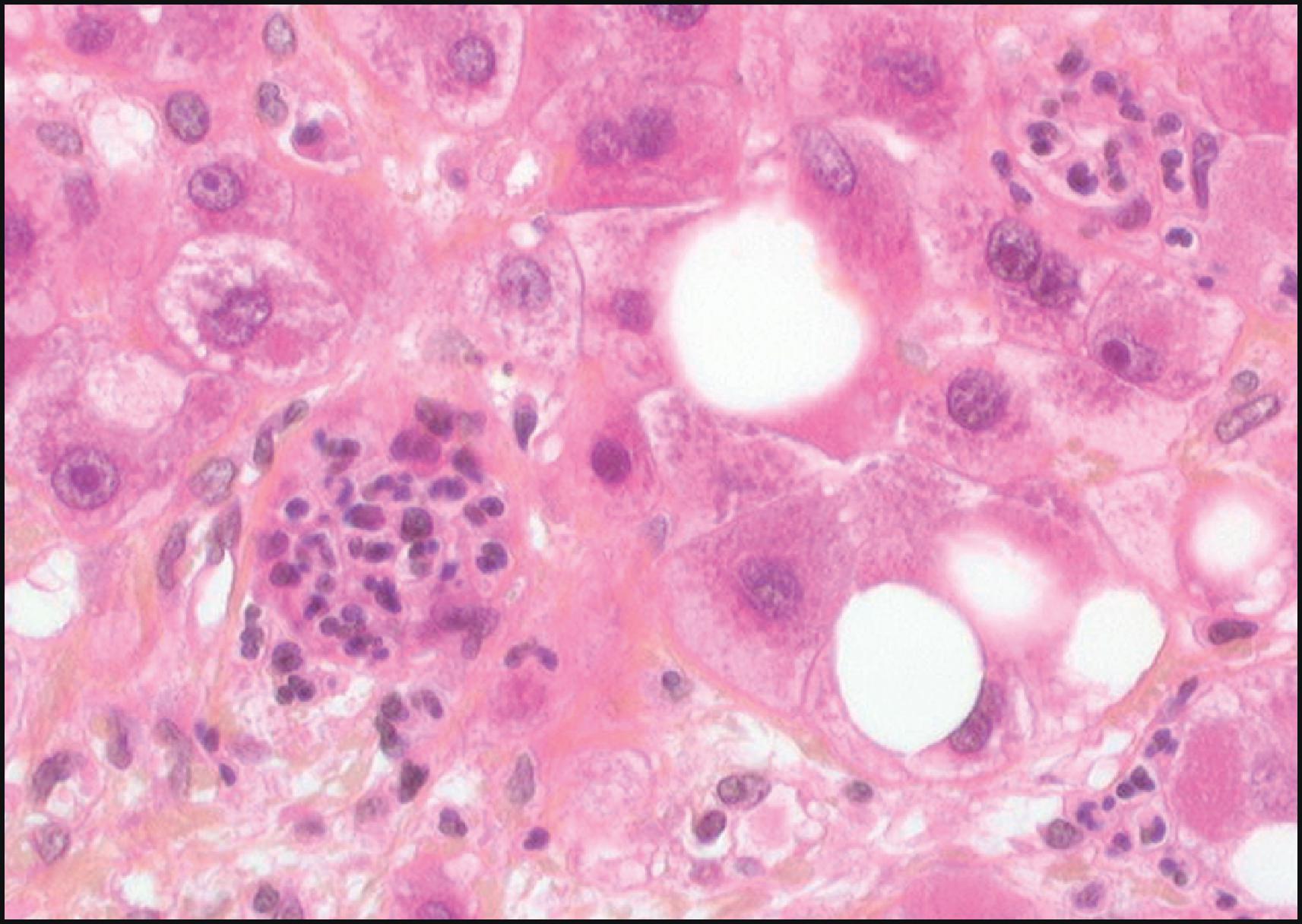
In the absence of a grossly recognizable lesion, biopsy obtained by the surgeon at the time of an operation is often disappointing; if a diffuse liver disease is suspected, needle biopsy rather than wedge biopsy should be performed to provide a more representative liver sample. Capsular and subcapsular fibrous tissue may be quite prominent in wedge biopsies of normal liver, and tissue coagulation artefacts can hamper biopsy interpretation. Clusters of acute inflammatory cells are often seen in the intraoperatively obtained liver biopsy as a nonspecific consequence of the surgical procedure itself—so-called surgical hepatitis ( Fig. 2.4 ).
The main drawbacks of liver biopsy as a diagnostic procedure are related to sampling and observation errors. As liver biopsy involves only a tiny part of the whole organ, there is a risk that the sample obtained will not be suitable for evaluating a lesion that is heterogeneously distributed throughout the entire liver, as in liver fibrosis. , Extensive reports have shown that, in the context of chronic liver diseases, increasing the size (length) of the biopsy can reduce the risk of sampling error. The length of the biopsy, rather than the number of portal tracts, appears to be a relevant criterion for assessing the adequacy of a liver biopsy, especially since counting portal tracts is difficult, if not impossible, in cases of chronic liver diseases with septal fibrosis or cirrhosis. Optimal dimensional (length and width) thresholds have been discussed by several authors and, except for cirrhosis—for which millimetre-sized fragments may be sufficient—a 25-mm biopsy is considered an optimal length for accurate evaluation, although 15 mm has also been considered sufficient in most studies. , In addition, the diameter of the core is important, and it has been demonstrated that samples obtained by fine-needle biopsy (using 20–22-gauge needles) are unsuitable for accurate staging and grading of chronic liver disease. Indeed, a biopsy obtained with a 16–18-gauge needle has proved to be much more useful for this purpose. These thresholds have been set up mainly in the context of chronic hepatitis but might vary slightly in other diseases where lesions are much more systematized in the lobule, such as steatosis in patients with nonalcoholic fatty liver disease (NAFLD).
Observer variation is another potential limitation related to discordance between pathologists in biopsy interpretation. Training and specialization of pathologists are of major importance for reducing interobserver variations, and problems can be alleviated if individuals have had subspecialty experience in liver pathology for several years and practice in an academic context. Observer variation is also related to histopathological features. In the case of chronic hepatitis, studies have shown that fibrosis pattern is more reproducible than features related to necroinflammation. In terms of fibrosis scores, concordance between pathologists has been judged satisfactory whatever the system used. , , Thus although liver biopsy has its limitations, adequate precautions can reduce the flaws inherent in this method.
As previously noted, semiquantitative scoring systems have been widely used for chronic liver diseases, including viral hepatitis, biliary diseases and NAFLD. , The systems are useful in defining homogeneous groups of patients as an aid in clinical trials for assessing eligibility or drug efficacy, as well as inthe follow-up when repeated biopsies are performed. Regardless of the disease, however, these scoring systems are not intended to replace the verbal description of the histological patterns and should be considered as only an aid for the clinician rather than a diagnostic procedure.
Both the recent development of noninvasive markers and the major progress in imaging procedures have fuelled discussions as to the usefulness of liver biopsy, given the risks and limitations involved in this invasive procedure. Clearly, a logical and valid goal in hepatology would be to develop noninvasive tests for all liver disorders, which would preclude the need for liver biopsy in many cases and thereby reduce the (very low) incidence of complications. Although this goal may be reached in the near future for some pathologies such as cirrhosis or advanced fibrosis, particularly in hepatitis C, liver biopsy will continue to be an indispensable technique in the armamentarium of the hepatologist.
Because the liver has an exceptionally abundant blood supply, it is anticipated that blood component analysis should provide valuable insight into liver disease evaluation. With more than 10,000 different proteins, a wide variety of carbohydrates, lipid particles and pathogens, peripheral blood might be a major source of information for both diagnosis and prognosis, provided the appropriate component is scrutinized.
Liver function tests (LFTs) have been routinely used for years as a first-line investigation to screen for liver diseases, but they can sometimes appear normal despite significant underlying liver disease. Furthermore, the relationship between severity of liver disease and changes in blood parameters is far from linear, with little predictive value or specificity. Commonly available tests include alanine transaminase (ALT) and aspartate transaminase (AST), alkaline liver phosphatase (ALP), γ-glutamyltransferase (GGT), serum bilirubin, prothrombin time (PT or international normalized ratio [INR]) and serum albumin. They reflect differing liver ‘functions’: excretion of anions (bilirubin), hepatocellular integrity (transaminases), formation and subsequent free flow of bile (bilirubin, ALP) and protein synthesis (albumin).
Bilirubin is formed through the turnover of red blood cells (RBCs, the ‘haem’ component). Unconjugated bilirubin is transported to the liver. It is water insoluble and therefore cannot be excreted. Within the liver, it is conjugated to bilirubin glucuronide and subsequently secreted into the bile and gut. Serum bilirubin is mainly present in an unconjugated form, reflecting a balance between production and hepatobiliary excretion. Unconjugated hyperbilirubinaemia (indirect bilirubin fraction >85% of total bilirubin) occurs with increased bilirubin production, as in haemolysis or ineffective erythropoiesis, or in defects in hepatic uptake or conjugation, which may be inherited (as in Gilbert syndrome) or acquired. Conjugated hyperbilirubinaemia characteristically occurs in parenchymal liver disease and biliary obstruction.
Transaminases (aminotransferases), including AST and ALT, are markers of hepatocellular injury. They participate in gluconeogenesis by catalysing the transfer of amino groups from amino acids to ketoglutaric acid. AST is present in the liver, cardiac muscle, skeletal muscle, kidneys, brain, pancreas, lungs, leukocytes and RBCs. AST is less sensitive and specific to the liver than ALT, a cytosolic enzyme found at its highest concentrations in the liver. Hepatocellular injury, but not necessarily cell death, triggers release of these enzymes into the circulation. An increase in liver transaminases is rather nonspecific, and common causes include acute hepatitis of any aetiology, NAFLD, alcoholic liver disease, chronic hepatitis B or C, autoimmune liver disease and drug injury.
ALP originates mainly from liver and bone. An elevation may be physiological, especially during pregnancy and during adolescent growth. Hepatic ALP is present on the canalicular and luminal domains of the bile duct epithelium. ALP rises as a result of increased synthesis and consequent release into the circulation. Common causes of a rise in ALP are extrahepatic biliary obstruction, small bile duct disease and drug-induced cholestasis.
GGT is an enzyme expressed in hepatocytes and biliary epithelial cells. Although GGT is a sensitive test of hepatobiliary disease, its usefulness is limited by lack of specificity, since high levels may be seen in pancreatic disease, myocardial infarction, renal failure, chronic obstructive pulmonary disease, diabetes and alcoholism. Along with other enzyme abnormalities, a rise in GGT supports a hepatobiliary source. A rise in GGT with high transaminase levels and an AST/ALT ratio of 2:1 or more suggests alcohol-related liver disease.
Albumin synthesis is an important function of the liver. With progressive liver disease, serum albumin levels fall, reflecting decreased synthesis. The albumin level depends on a number of other factors, such as nutritional status, catabolism, hormonal factors and urinary and gastrointestinal losses. The albumin concentration correlates with the prognosis in chronic liver disease. The synthesis of coagulation factors (except for factor VIII) is an important function of the liver. The PT measures the rate of conversion of prothrombin to thrombin (requiring factors II, V, VII and X) and thus reflects a vital synthetic function of the liver. PT may therefore be prolonged in liver disease and consumptive coagulopathy. The INR is often tested now along with or instead of PT (INR = Patient PT/Mean control PT.) This is helpful because INR avoids interlaboratory variability in PT; its interpretation is otherwise similar to PT.
The prognosis of liver diseases can be evaluated by blood sample analysis. Most useful are the Child–Pugh–Turcotte (CPT) classification for prediction of cirrhosis, the model for end-stage liver disease (MELD) for assessing the prognosis of patients with severely impaired liver function in the context of liver transplantation and the Maddrey discriminant function for predicting risk of mortality in alcoholic hepatitis. , Interestingly, these indices are often combined and include serum measurements and other clinical or pathological factors ( Table 2.1 ).
| Index | Indication | Description |
|---|---|---|
| Child–Pugh–Turcotte (CPT) classification | Cirrhosis mortality | Ascites (no = 0, medically controlled = 1, poorly controlled + 3) +Encephalopathy (no = 1, medically controlled = 2, poorly controlled = 3) +Total bilirubin (<34 µmol/L = 1, 34–50 µmol/L = 2, >50 µmol/L = 3) +Albumin (>35 g/L = 1, 28–35 g/L = 2, <28 g/L = 3) +INR (<1.7 = 1, 1.7–2.2 = 2, >2.2 = 3)Class A: score 5–6; Class B: score 7–9; Class C: score >10 |
| Model for end-stage liver disease (MELD) | End-stage liver disease | MELD score = (0.957 × ln (serum creatinine) + 0.378 × ln (serum bilirubin) + 1.120 × ln (INR) + 0.643) × 10 (if haemodialysis, value for creatinine is automatically set to 4.0) |
| Maddrey discriminant function | Alcoholic hepatitis | Discriminant function = 4.6 × (Patient PT − Control PT) + Total bilirubin |
Since fibrosis is the hallmark of all chronic liver diseases, and because fibrosis is the main determinant of clinical outcome, several groups are investigating whether serum might predict the stage of liver fibrosis and help to follow its progression. Algorithms have been developed combining different blood components and clinical parameters that correlate with fibrosis stage as evaluated on liver biopsy. Some of these combinations have been reported to predict the presence of bridging fibrosis or cirrhosis with considerable diagnostic accuracy. , However, they have only limited accuracy for predicting earlier hepatic fibrosis stages. Furthermore, the performance of fibrosis biomarkers at differentiating between adjacent scores of hepatic fibrosis is very limited. All such drawbacks limit their use for individual patients. The potential for more sophisticated extracellular matrix (ECM)-derived serum components has also been assessed. These include hyaluronic acid, products of collagen synthesis or degradation, enzymes involved in matrix biosynthesis or degradation, ECM glycoproteins and proteoglycans. However, the diagnostic accuracy of these ECM components in predicting liver fibrosis is limited. Furthermore, in order for these markers to reflect hepatic fibrogenesis or fibrosis accurately, they need to be organ specific, and the biological half-life should be independent of urinary and biliary excretion as well as sinusoidal endothelial uptake. Unfortunately, none of the available serum biomarkers fulfils all these criteria. Therefore biochemical blood tests have only limited value in predicting fibrosis stage; indeed, several studies have concordantly shown that their use may render liver biopsy unnecessary in only a minority of patients with chronic HCV.
The serum proteome describes the whole pool of proteins expressed in a biological milieu at a given time, and this overall evaluation is potentially relevant for disease diagnosis. In comparison to the previously described approach, mining of the proteome does not require an a priori hypothesis concerning the physiopathology of the liver disease. Therefore the challenge in clinical proteomic studies is to link global proteome profile variations to specific liver disease phenotypes and to elucidate relevant biomarkers in order to develop diagnostic or prognostic tools. Differences in protein patterns (profiling) between different conditions can then be detected. The possibility of rapidly obtaining and comparing profiles directly from the original source material and without laborious sample preparation makes this technique a promising possibility for clinical application. Using this technology, specific serum profiles have been delineated for the diagnosis of hepatic malignancy, liver fibrosis and nonalcoholic steatohepatitis (NASH), but none of these discoveries has yet been applied to clinical diagnosis. However, with the development of new technologies such as high-throughput robust proteomic methods, some progress might be expected in the near future.
Metabolomics uses a similar approach but targets smaller molecules, which are intermediate or end-products of a chemical process using various analytical technologies. This nontargeted approach is looking for chemical imprints of a pathophysiological process present in a biological milieu. In the field of chronic liver disease, metabolomics (and lipidomics) is actively investigated in the context of NAFLD. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here