Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Editor’s Note to Readers: For an excellent and more detailed discussion of the cardiovascular physical examination, read Physical Diagnosis Secrets, 2nd edition, by Salvatore Mangione.
A carotid arterial pulse that is reduced ( parvus ) and delayed ( tardus ) suggests the presence of aortic valvular stenosis . Occasionally, this also may be accompanied by a palpable thrill. If ventricular function is good, a slower upstroke correlates with a higher transvalvular gradient. In left ventricular failure, however, parvus and tardus may occur even with mild aortic stenosis (AS).
It depends on whether it is associated with normal or widened pulse pressure. If associated with the normal pulse pressure , a brisk carotid upstroke usually indicates two conditions:
Simultaneous emptying of the left ventricle into a high-pressure bed (the aorta) and a lower pressure bed : The latter can be the right ventricle (in patients with ventricular septal defect [VSD]) or the left atrium (in patients with mitral regurgitation [MR]). Both will allow a rapid left ventricular emptying, which in turn generates a brisk arterial upstroke. The pulse pressure, however, remains normal.
Hypertrophic cardiomyopathy (HCM) : Despite its association with left ventricular obstruction, this disease is characterized by a brisk and bifid pulse, due to the hypertrophic ventricle and its delayed obstruction. An example of the carotid pulsation in HCM and other conditions is given in Fig. 1.1 .
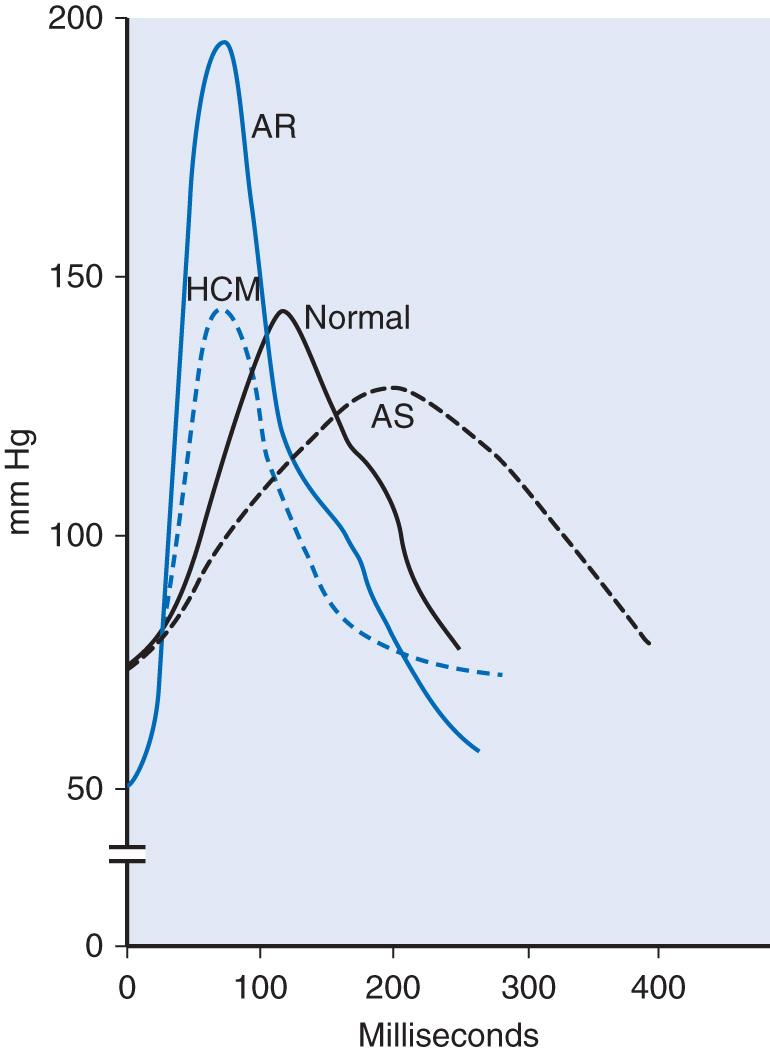
If associated with the widened pulse pressure, a brisk upstroke usually indicates aortic regurgitation (AR). In contrast to MR, VSD, or HCM, the AR pulse has rapid upstroke and collapse.
The most common are the hyperkinetic heart syndromes (high-output states). These include anemia, fever, exercise, thyrotoxicosis, pregnancy, cirrhosis, beriberi, Paget disease, arteriovenous fistulas, patent ductus arteriosus, AR, and anxiety—all typically associated with rapid ventricular contraction and low peripheral vascular resistance.
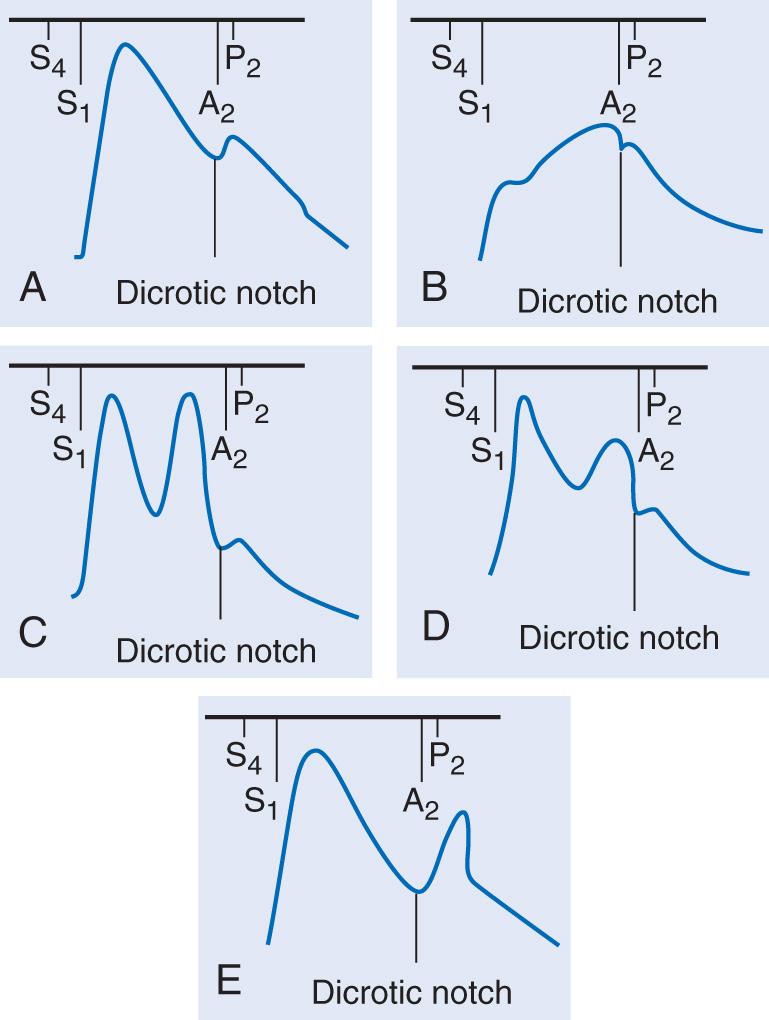
Examples of the carotid pulse waveform and its correlation to heart sounds are provided in Fig. 1.2 .
Pulsus paradoxus is an exaggerated fall in systolic blood pressure during quiet inspiration. In contrast to evaluation of arterial contour and amplitude, it is best detected in a peripheral vessel, such as the radial artery. Although palpable at times, optimal detection of the pulsus paradoxus typically requires a sphygmomanometer. Pulsus paradoxus can occur in cardiac tamponade and other conditions.
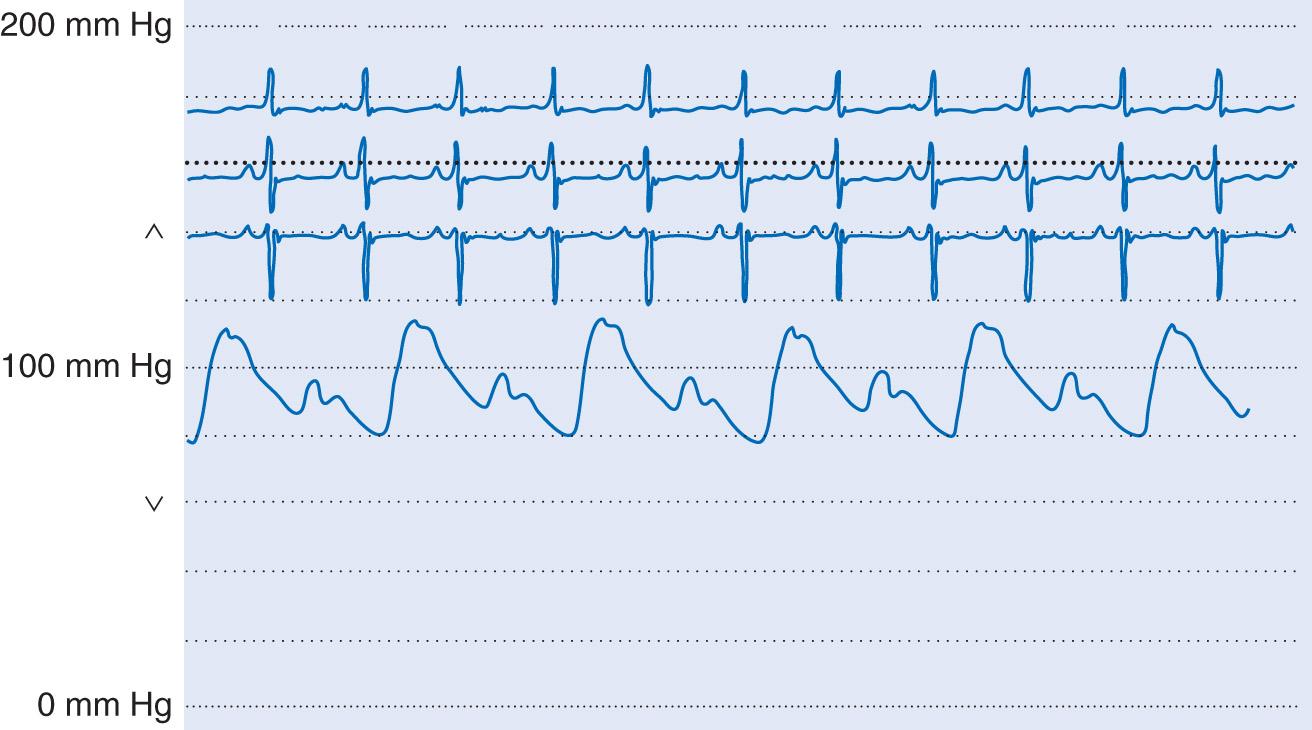
Pulsus alternans is the alternation of strong and weak arterial pulses despite regular rate and rhythm . First described by Ludwig Traube in 1872, pulsus alternans is often associated with alternation of strong and feeble heart sounds (auscultatory alternans). Both indicate severe left ventricular dysfunction (from ischemia, hypertension, or valvular cardiomyopathy), with worse ejection fraction and higher pulmonary capillary pressure. Hence, they are often associated with an S 3 gallop. A tracing indicating pulses alternans is given in Fig. 1.3 .
The Duroziez murmur is a to-and-fro double murmur over a large central artery—usually the femoral but also the brachial. It is elicited by applying gradual but firm compression with the stethoscope’s diaphragm. This produces not only a systolic murmur (which is normal) but also a diastolic one (which is pathologic and typical of AR). The Duroziez murmur has 58% to 100% sensitivity and specificity for AR.
Carotid shudder is a palpable thrill felt at the peak of the carotid pulse in patients with AS, AR, or both. It represents the transmission of the murmur to the artery and is a relatively specific but rather an insensitive sign of aortic valvular disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here