Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endocrine system diseases generally affect multiple organ systems, because hormones secreted into the general circulation act on multiple tissues that are distant from their sources of synthesis and secretion. Nearly all hormones and accompanying hormonal disorders may be associated with a pathophysiological disarrangement of some component of the cardiovascular system. This chapter focuses on the most common disorders and those with the most important deleterious consequences for cardiovascular function.
The seven peptide hormones secreted by the anterior pituitary gland and the two hormones secreted by the posterior pituitary gland all affect the cardiovascular system. Most of these hormones cause changes in salt or water metabolism that indirectly alter the system, but some directly affect vascular tone. The anterior pituitary hormones and their direct and indirect effects on cardiovascular function are listed in Table 66.1 . Three disorders can result in major changes in cardiovascular function: hypopituitarism, acromegaly, and antidiuretic hormone (ADH) secretion disorders.
| Hormone | Direct | Indirect |
|---|---|---|
| ACTH | Stimulates cortisol secretion Stimulates aldosterone |
Cortisol increases arteriolar tone. Aldosterone stimulates Na + retention and K + excretion. |
| TSH | Stimulates thyroxine and triiodothyronine synthesis | Thyroxine stimulates HR, pulse pressure, and LV contractility. |
| LH | Stimulates estrogen and testosterone synthesis | Estrogen acts as a vasodilator. |
| ADH | Stimulates water retention, increases plasma volume; acts through a central mechanism to increase vasoconstriction | |
| GH | Stimulates vasomotor force and LV function | Through IGF-1, it stimulates HR. |
Hypopituitarism in adults often results from mass lesions that arise in the hypothalamus or the pituitary fossa. Growth hormone (GH) deficiency and gonadotropin deficiencies are often present. If the lesion causing the deficit is extensive, thyroid-stimulating hormone (TSH) (thyrotropin) and adrenocorticotrophic hormone (ACTH) secretion may also be impaired. GH deficiency per se does not lead to cardiomyopathy or loss of vascular tone; however, patients with GH deficiency most commonly present with a lack of energy and stamina. Therefore, cardiac output (CO) may not be adequate to sustain peak exercise activity, and endurance may be moderately impaired. Treatment with GH replacement therapy for as long as 3 years improves treadmill performance, which suggests that GH deficiency leads to a decrease in exercise tolerance. However, whether this improvement is due solely to GH stimulation of myocardial function is unclear, because GH also increases red cell mass, which could alter exercise tolerance. TSH and ACTH deficiencies lead to changes in cardiovascular function, as discussed in the sections on hypothyroidism and hypoadrenalism. Loss of gonadotropin secretion, particularly in men, can lead to low testosterone concentrations. This can lead to impaired exercise performance, loss of skeletal muscle mass, and decreased stamina. Replacement with testosterone improves muscle function and exercise performance.
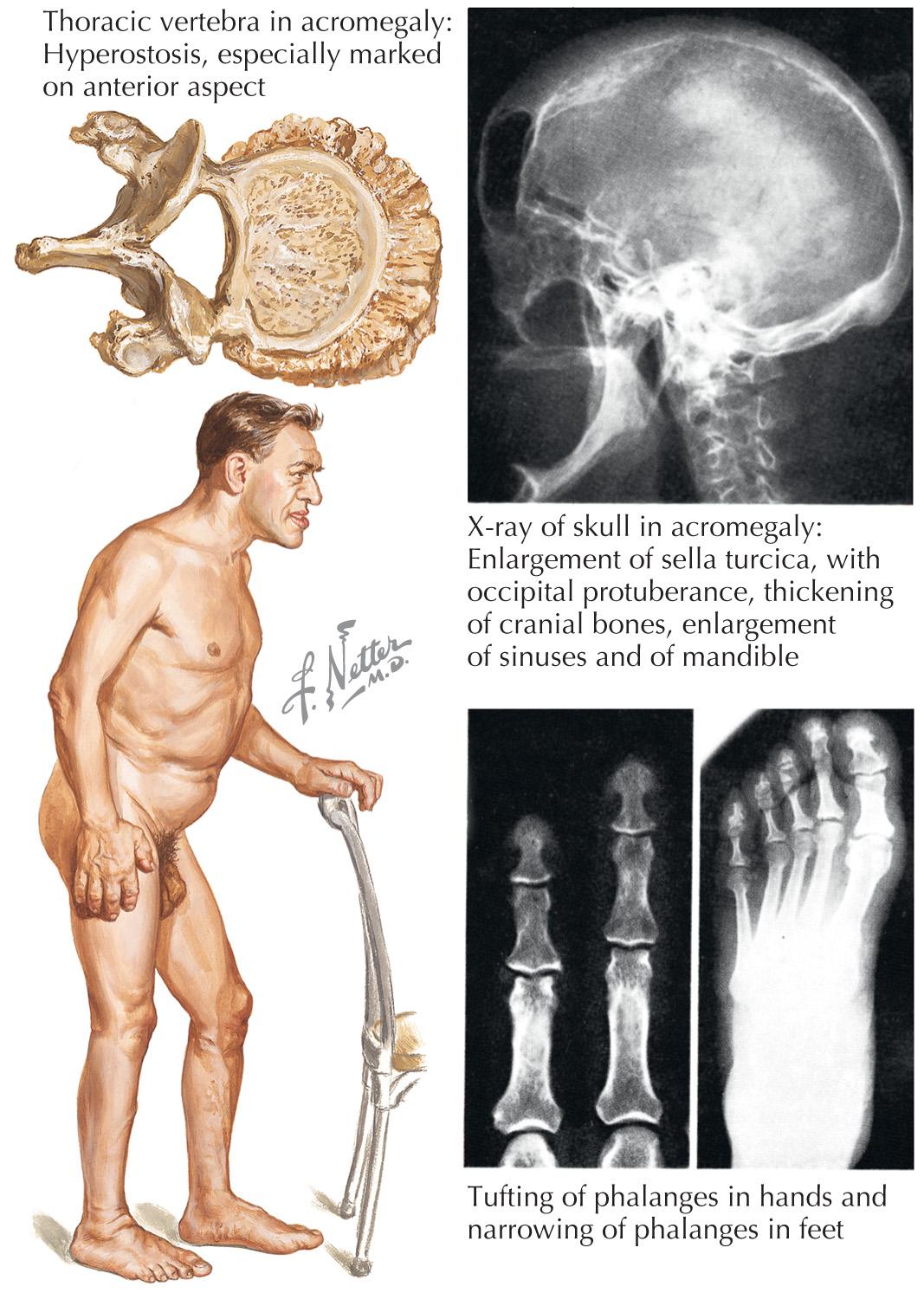
Sustained hypersecretion of GH by a pituitary tumor can lead to overgrowth of several tissues and to several cardiovascular changes ( Fig. 66.1 ). Cardiovascular function is an important determinant of morbidity and mortality in untreated acromegaly. The most common comorbid cardiovascular condition accompanying acromegaly is hypertension, which is present in 60% of inadequately treated patients. Hypertension in acromegaly is usually mild but can be difficult to manage conventionally. Left ventricular (LV) mass can be significantly increased compared with that of normotensive patients. Curing the acromegalic condition is the most effective way to lower blood pressure (BP). Some patients can develop a concentric ventricular hypertrophic cardiomyopathy unassociated with hypertension but which is associated with long-standing acromegaly, which can result in both diastolic and systolic dysfunction. Cardiomegaly can be disproportionate to the changes in size that occur in other organs in severe acromegaly. The severity of cardiomyopathy correlates with the duration of exposure to high levels of GH. Diastolic dysfunction and hypertrophy develop first and are common in untreated patients. These changes are reversible with adequate treatment of excessive GH. If left untreated, there is progression to systolic dysfunction, and heart failure and severe ventricular arrhythmias can occur. Histological evaluation of the myocardium in patients with long-standing acromegaly can show interstitial fibrosis, lymphocytic infiltration, and occasionally, necrosis.
Other changes in acromegaly can lead to secondary effects on the cardiovascular system. Some patients have sleep apnea that causes chronic recurrent hypoxemia, approximately 25% of patients have diabetes mellitus, and up to 40% of patients have hypertriglyceridemia. Premature mortality is increased in acromegaly, and cardiovascular diseases are the cause of death in 38% to 62% of patients. Normalizing GH and insulin-like growth factor 1 concentrations with conventional treatment restores normal life expectancy, preventing the premature death that results from cardiovascular disease.
Unlike diseases of the anterior pituitary gland, the etiology of ADH deficiency is often hypothalamic lesions (in ~60% of patients). Most cases of ADH deficiency are acquired, and many result from attempts to remove the pituitary tumor surgically, which can damage the pituitary stalk or the posterior pituitary. Severe ADH deficiency leads to polyuria, polydipsia, and, if untreated, vascular collapse. The most common hypothalamic causes are mass lesions, which are primarily tumors of the hypothalamus (e.g., craniopharyngioma and dysgerminoma).
ADH is a potent pressor agent that stimulates direct vasoconstriction of blood vessels. This action is conferred at the level of the regional arterioles, and physiological concentrations can induce this effect. Loss of ADH leads to a significant increase in serum osmolarity of >295 mOsm/L, with inappropriately dilute urine of <300 mOsm/L. The diagnosis is established by detecting abnormally high serum osmolarity with low plasma vasopressin and low urinary osmolarity.
Administering vasopressin quickly reverses the changes in these parameters. Vasopressin acts on the kidney to decrease free-water clearance. It also affects the brain to maintain central BP control; these brain actions are probably necessary for the maintenance of normal upright BP. The use of ADH antagonists illustrates the importance of endogenous arginine vasopressin for maintaining normal BP.
Several central nervous system and primary pulmonary diseases, as well as medications, can cause inappropriately high concentrations of ADH, leading to decreases in plasma osmolarity. In these syndromes, high levels of ADH secretion continue, despite low osmolarity. Arginine vasopressin concentrations can be increased up to 10 to 20 times greater than normal in this disorder. This does not lead to hypertension per se, but rather to water intoxication. Serum sodium continues to decrease because free-water clearance is consistently impaired, thus leading to severe hyponatremia, which sometimes manifest as seizures. Identification of the source of inappropriate ADH secretion or correction of the underlying lesion is needed for successful treatment. Empiric treatment severely restricts free-water intake. Recently, a new class of ADH receptor antagonists (vaptans) has been shown to improve hyponatremia associated with euvolemic inappropriate secretion of ADH. These drugs are approved for the in-hospital treatment of severe euvolemic hyponatremia.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here