Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The heart, shown in Figure 9-1 , is actually two separate pumps, a right heart that pumps blood through the lungs and a left heart that pumps blood through the systemic circulation that provides blood flow to the other organs and tissues of the body. Each of these is a pulsatile, two-chamber pump composed of an atrium and a ventricle. Each atrium is a weak primer pump for the ventricle, helping to move blood into the ventricle. The ventricles then supply the main pumping force that propels the blood either (1) through the pulmonary circulation by the right ventricle or (2) through the systemic circulation by the left ventricle. The heart is surrounded by a two-layer sac called the pericardium, which protects the heart and holds it in place.
Special mechanisms in the heart cause a continuing succession of contractions called cardiac rhythmicity, transmitting action potentials throughout the cardiac muscle to cause the heart’s rhythmical beat. This rhythmical control system is discussed in Chapter 10 . In this chapter, we explain how the heart operates as a pump, beginning with the special features of cardiac muscle ( ).
The heart is composed of three major types of cardiac muscle— atrial muscle, ventricular muscle, and specialized excitatory and conductive muscle fibers. The atrial and ventricular types of muscle contract in much the same way as skeletal muscle, except that the duration of contraction is much longer. The specialized excitatory and conductive fibers of the heart, however, contract feebly because they contain few contractile fibrils; instead, they exhibit automatic rhythmical electrical discharge in the form of action potentials or conduction of the action potentials through the heart, providing an excitatory system that controls the rhythmical beating of the heart.
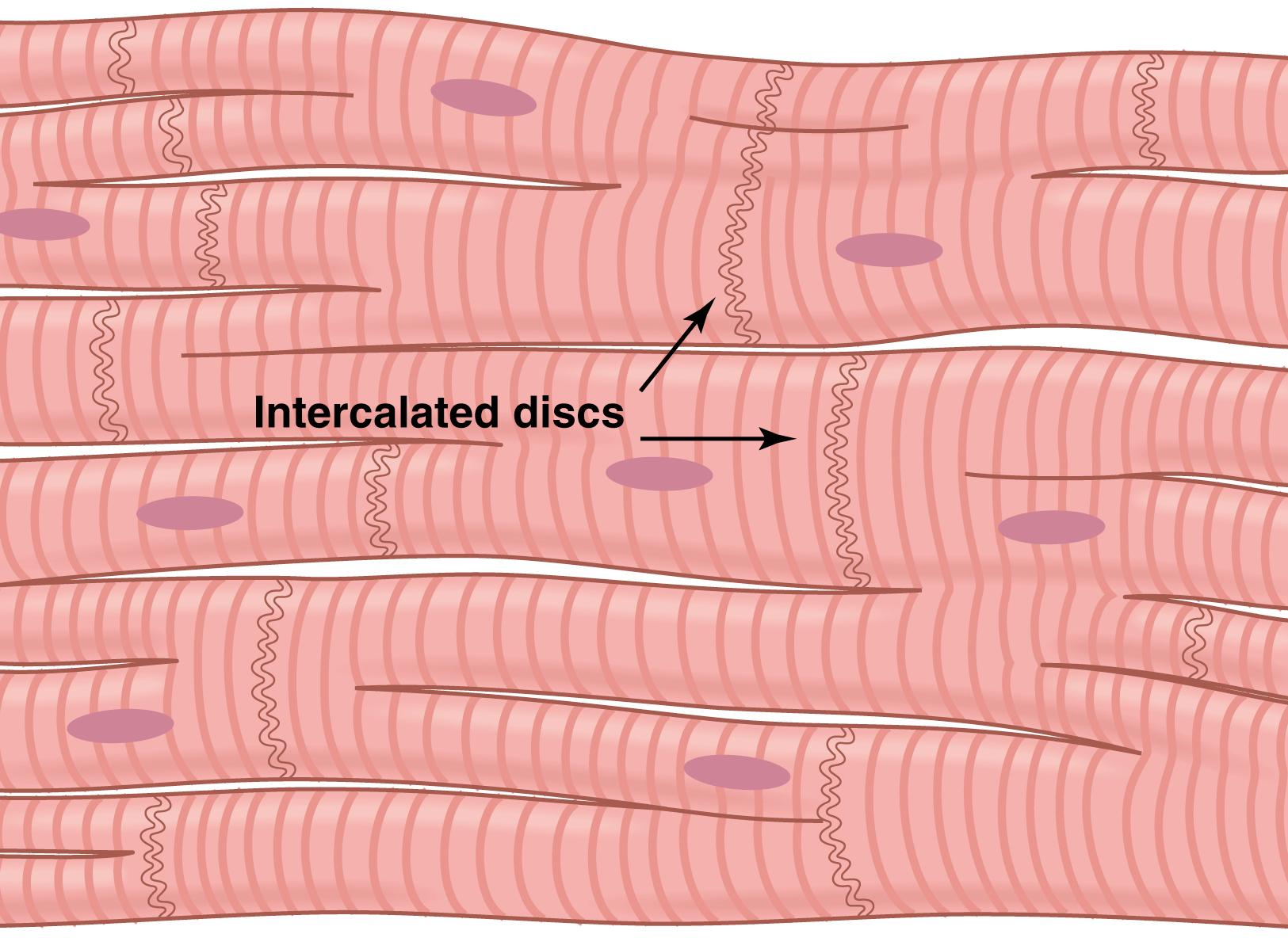
Figure 9-2 shows the cardiac muscle histology, demonstrating cardiac muscle fibers arranged in a latticework, with the fibers dividing, recombining, and then spreading again. Note that cardiac muscle is striated in the same manner as in skeletal muscle. Furthermore, cardiac muscle has typical myofibrils that contain actin and myosin filaments almost identical to those found in skeletal muscle; these filaments lie side by side and slide during contraction in the same manner as occurs in skeletal muscle (see Chapter 6 ). In other ways, however, cardiac muscle is quite different from skeletal muscle, as we shall see.
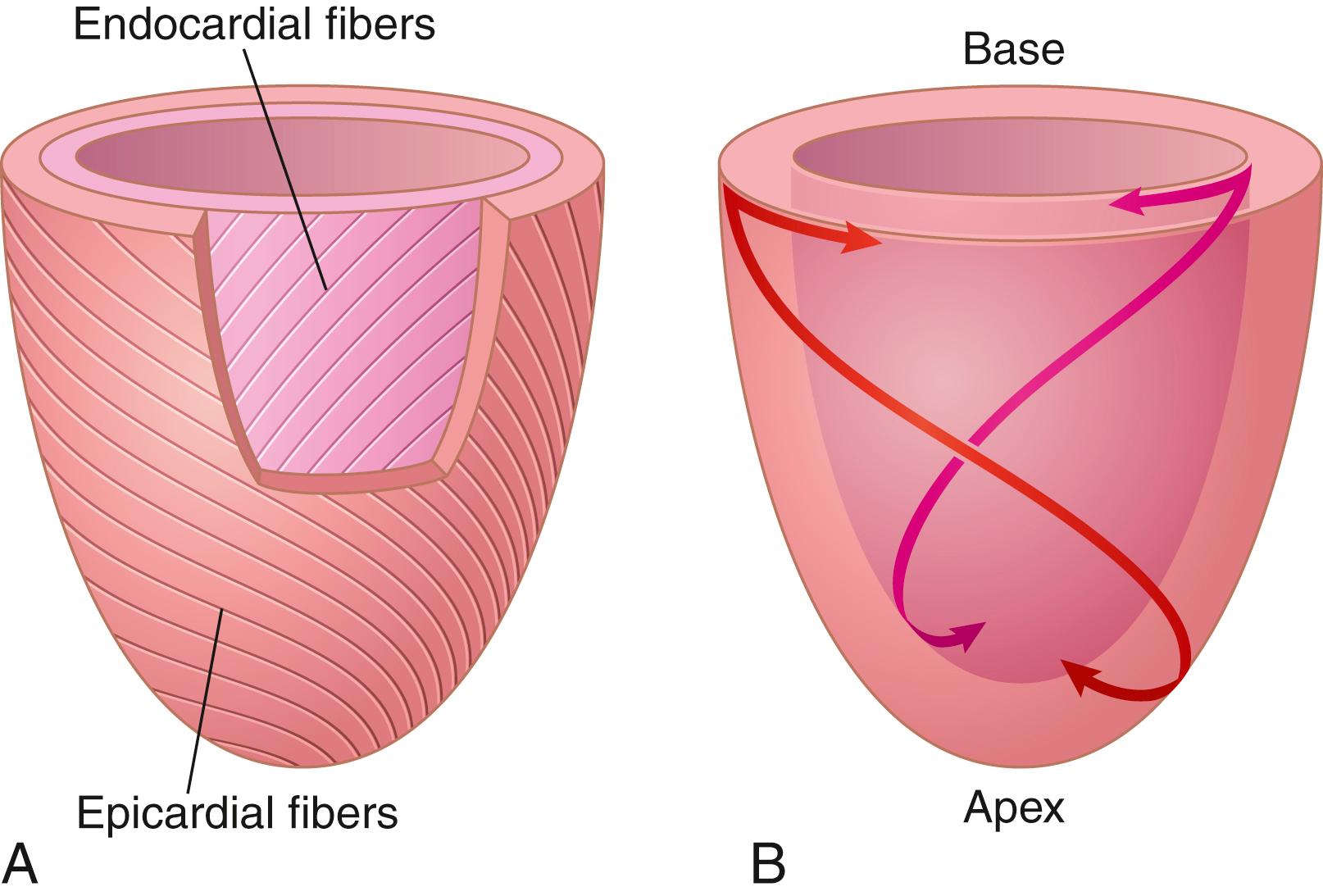
The left ventricle is organized into complex muscle fiber layers that run in different directions and allow the heart to contract in a twisting motion during systole. The subepicardial (outer) layer spirals in a leftward direction, and the subendocardial (inner) layer spirals in the opposite direction (rightward), causing counterclockwise rotation of the apex of the heart and clockwise rotation of the base of the left ventricle during the ejection phase ( Figure 9-3 ). This causes a wringing motion of the left ventricle, pulling the base downward toward the apex during systole (contraction). At the end of systole, the left ventricle is similar to a loaded spring and recoils or untwists during diastole (relaxation) to allow blood to enter the pumping chambers rapidly.
The dark areas crossing the cardiac muscle fibers in Figure 9-2 are called intercalated discs; they are actually cell membranes that separate individual cardiac muscle cells from one another. That is, cardiac muscle fibers are made up of many individual cells connected in series and in parallel with one another.
At each intercalated disc, the cell membranes fuse with one another to form permeable communicating junctions (gap junctions) that allow rapid diffusion of ions. Therefore, from a functional point of view, ions move with ease in the intracellular fluid along the longitudinal axes of the cardiac muscle fibers so that action potentials travel easily from one cardiac muscle cell to the next, past the intercalated discs. Thus, cardiac muscle is a syncytium of many heart muscle cells in which the cardiac cells are so interconnected that when one cell becomes excited, the action potential rapidly spreads to all of them.
The heart actually is composed of two syncytia; the atrial syncytium, which constitutes the walls of the two atria; and the ventricular syncytium, which constitutes the walls of the two ventricles. The atria are separated from the ventricles by fibrous tissue that surrounds the atrioventricular (A-V) valvular openings between the atria and ventricles. Normally, potentials are not conducted from the atrial syncytium into the ventricular syncytium directly through this fibrous tissue. Instead, they are only conducted by way of a specialized conductive system called the A-V bundle , a bundle of conductive fibers several millimeters in diameter that is discussed in Chapter 10 .
This division of the muscle of the heart into two functional syncytia allows the atria to contract a short time ahead of ventricular contraction, which is important for the effectiveness of heart pumping.
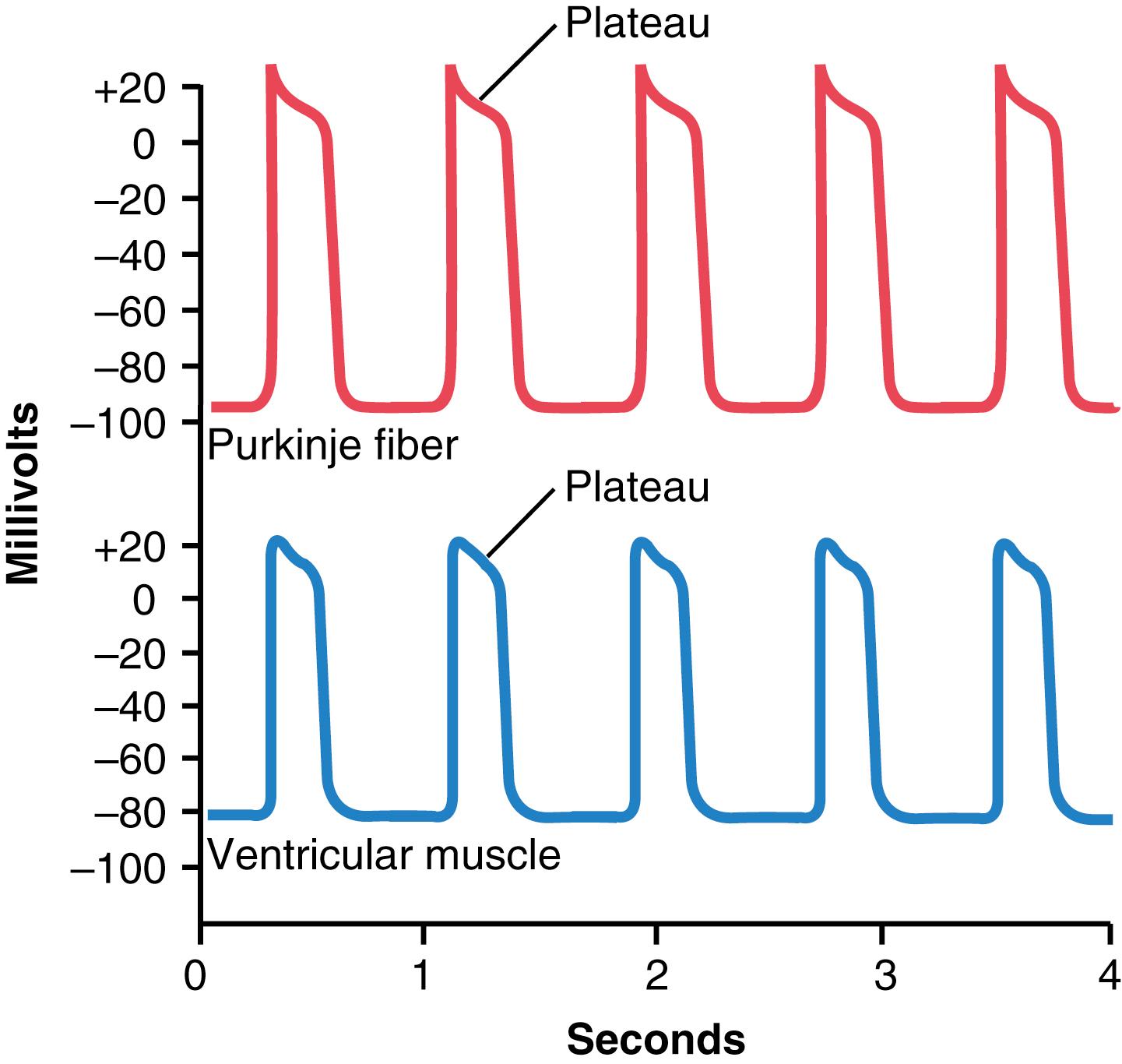
The action potential recorded in a ventricular muscle fiber, shown in Figure 9-4 , averages about 105 millivolts, which means that the intracellular potential rises from a very negative value between beats, about −85 millivolts, to a slightly positive value, about +20 millivolts, during each beat. After the initial spike , the membrane remains depolarized for about 0.2 second, exhibiting a plateau , followed at the end of the plateau by abrupt repolarization. The presence of this plateau in the action potential causes ventricular contraction to last as much as 15 times longer in cardiac muscle than in skeletal muscle.
At least two major differences between the membrane properties of cardiac and skeletal muscle account for the prolonged action potential and the plateau in cardiac muscle. First, the action potential of skeletal muscle is caused almost entirely by the sudden opening of large numbers of fast sodium channels that allow tremendous numbers of sodium ions to enter the skeletal muscle fiber from the extracellular fluid. These channels are called fast channels because they remain open for only a few thousandths of a second and then abruptly close. At the end of this closure, repolarization occurs, and the action potential is over within about another thousandth of a second.
In cardiac muscle, the action potential is caused by opening of two types of channels: (1) the same voltage-activated fast sodium channels as those in skeletal muscle; and (2) another entirely different population of L-type calcium channels (slow calcium channels), which are also called calcium-sodium channels. This second population of channels differs from the fast sodium channels in that they are slower to open and, even more importantly, remain open for several tenths of a second. During this time, a large quantity of both calcium and sodium ions flows through these channels to the interior of the cardiac muscle fiber, and this activity maintains a prolonged period of depolarization, causing the plateau in the action potential. Furthermore, the calcium ions that enter during this plateau phase activate the muscle contractile process, whereas the calcium ions that cause skeletal muscle contraction are derived from the intracellular sarcoplasmic reticulum.
The second major functional difference between cardiac muscle and skeletal muscle that helps account for both the prolonged action potential and its plateau is that immediately after the onset of the action potential, the permeability of the cardiac muscle membrane for potassium ions decreases about fivefold, an effect that does not occur in skeletal muscle. This decreased potassium permeability may result from the excess calcium influx through the calcium channels just noted. Regardless of the cause, the decreased potassium permeability greatly decreases the efflux of positively charged potassium ions during the action potential plateau and thereby prevents early return of the action potential voltage to its resting level. When the slow calcium-sodium channels do close at the end of 0.2 to 0.3 second, and the influx of calcium and sodium ions ceases, the membrane permeability for potassium ions also increases rapidly. This rapid loss of potassium from the fiber immediately returns the membrane potential to its resting level, thus ending the action potential.
Figure 9-5 summarizes the phases of the action potential in cardiac muscle and the ion flows that occur during each phase.
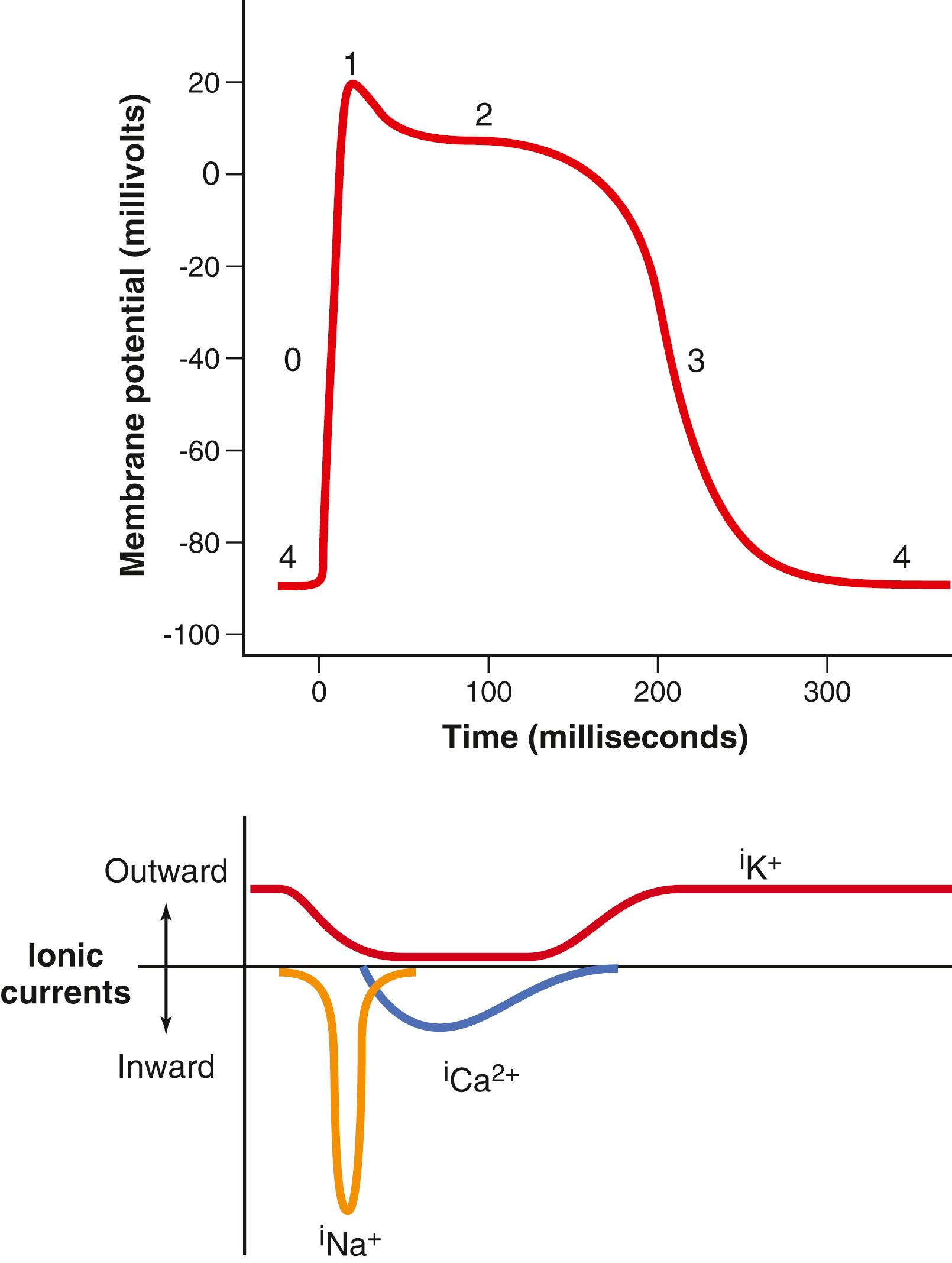
When the cardiac cell is stimulated and depolarizes, the membrane potential becomes more positive. Voltage-gated sodium channels (fast sodium channels) open and permit sodium to rapidly flow into the cell and depolarize it. The membrane potential reaches about +20 millivolts before the sodium channels close.
The sodium channels close, the cell begins to repolarize, and potassium ions leave the cell through open potassium channels.
A brief initial repolarization occurs and the action potential then plateaus as a result of increased calcium ion permeability and decreased potassium ion permeability. The voltage-gated calcium ion channels open slowly during phases 1 and 0, and calcium enters the cell. Potassium channels then close, and the combination of decreased potassium ion efflux and increased calcium ion influx causes the action potential to plateau.
The closure of calcium ion channels and increased potassium ion permeability, permitting potassium ions to exit the cell rapidly, ends the plateau and returns the cell membrane potential to its resting level.
This averages about−80 to −90 millivolts.
The velocity of conduction of the excitatory action potential signal along both atrial and ventricular muscle fibers is about 0.3 to 0.5 m/sec, or about 1/250 the velocity in very large nerve fibers and about 1/10 the velocity in skeletal muscle fibers. The velocity of conduction in the specialized heart conductive system—in the Purkinje fibers —is as high as 4 m/sec in most parts of the system, allowing rapid conduction of the excitatory signal to the different parts of the heart, as explained in Chapter 10 .
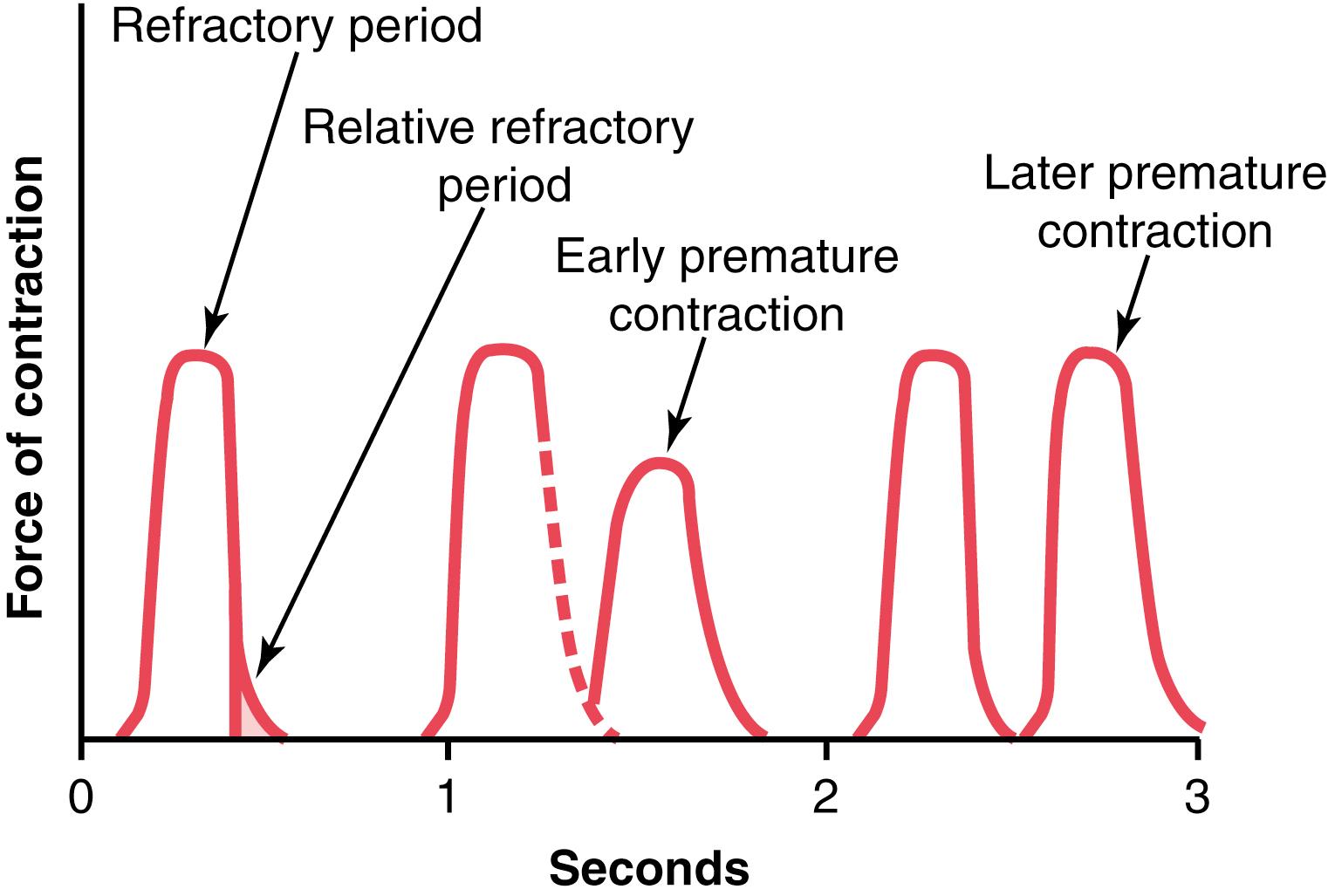
Cardiac muscle, like all excitable tissue, is refractory to restimulation during the action potential. Therefore, the refractory period of the heart is the interval of time, as shown to the left in Figure 9-6 , during which a normal cardiac impulse cannot re-excite an already excited area of cardiac muscle. The normal refractory period of the ventricle is 0.25 to 0.30 second, which is about the duration of the prolonged plateau action potential. There is an additional relative refractory period of about 0.05 second during which the muscle is more difficult to excite than normal but can be excited by a very strong excitatory signal, as demonstrated by the early premature contraction in the second example of Figure 9-6 . The refractory period of atrial muscle is much shorter than that for the ventricles (about 0.15 second for the atria compared with 0.25 to 0.30 second for the ventricles).
The term excitation-contraction coupling refers to the mechanism whereby the action potential causes the myofibrils of muscle to contract. This mechanism was discussed for skeletal muscle in Chapter 7 . Again, there are differences in this mechanism in cardiac muscle that have important effects on the characteristics of heart muscle contraction.
As is true for skeletal muscle, when an action potential passes over the cardiac muscle membrane, the action potential spreads to the interior of the cardiac muscle fiber along the membranes of the transverse (T) tubules . The T tubule action potentials then act on the membranes of the longitudinal sarcoplasmic tubules to cause release of calcium ions into the muscle sarcoplasm from the sarcoplasmic reticulum. In another few thousandths of a second, these calcium ions diffuse into the myofibrils and catalyze the chemical reactions that promote sliding of the actin and myosin filaments along one another, which produces the muscle contraction.
Thus far, this mechanism of excitation-contraction coupling is the same as that for skeletal muscle, but there is a second effect that is quite different. In addition to the calcium ions that are released into the sarcoplasm from the cisternae of the sarcoplasmic reticulum, calcium ions also diffuse into the sarcoplasm from the T tubules at the time of the action potential, which opens voltage-dependent calcium channels in the membrane of the T tubule ( Figure 9-7 ). Calcium entering the cell then activates calcium release channels, also called ryanodine receptor channels, in the sarcoplasmic reticulum membrane, triggering the release of calcium into the sarcoplasm. Calcium ions in the sarcoplasm then interact with troponin to initiate cross-bridge formation and contraction by the same basic mechanism as that described for skeletal muscle in Chapter 6 .
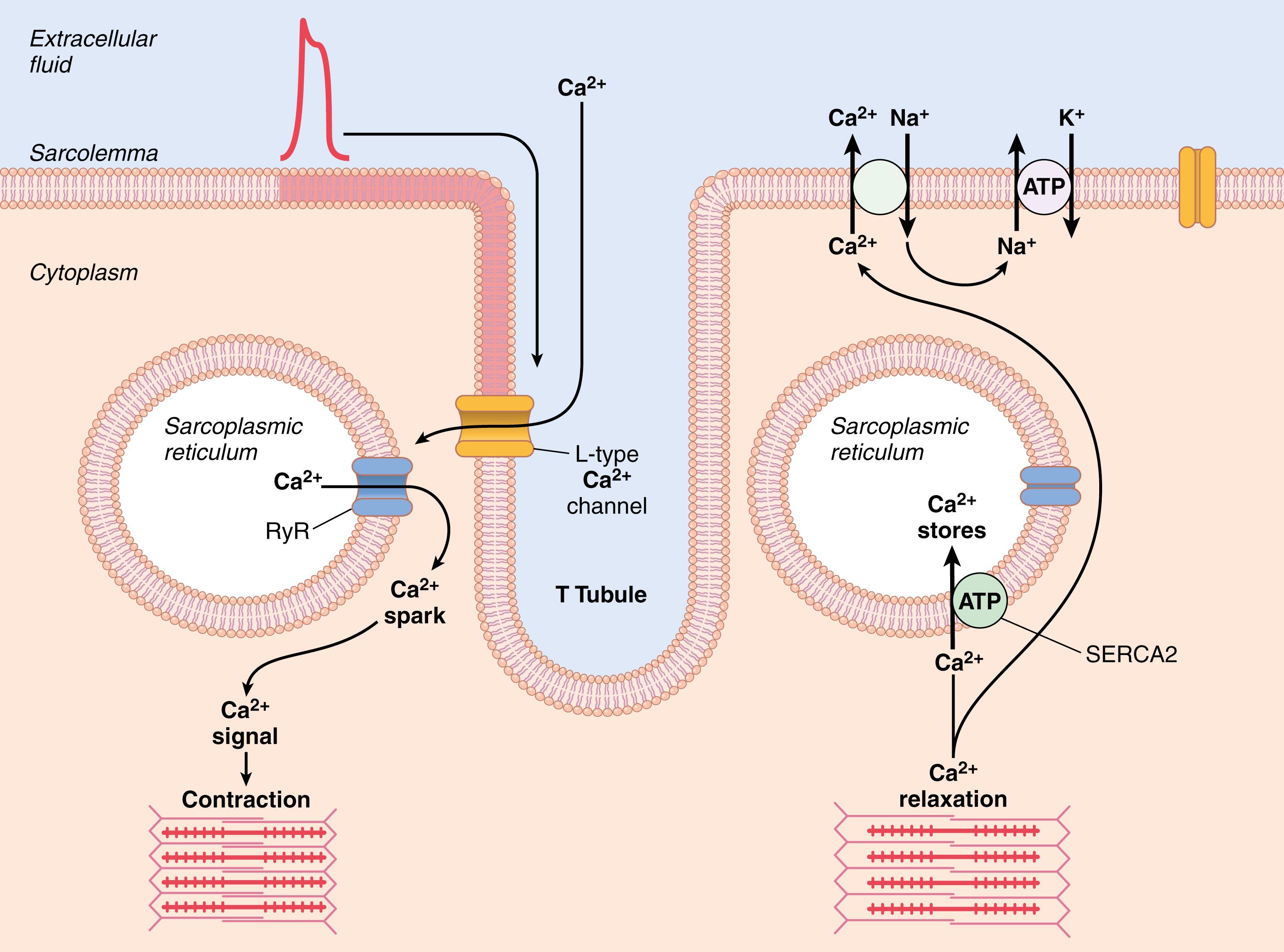
Without the calcium from the T tubules, the strength of cardiac muscle contraction would be reduced considerably because the sarcoplasmic reticulum of cardiac muscle is less well developed than that of skeletal muscle and does not store enough calcium to provide full contraction. The T tubules of cardiac muscle, however, have a diameter five times as great as that of the skeletal muscle tubules, which means a volume 25 times as great. Also, inside the T tubules is a large quantity of mucopolysaccharides that are electronegatively charged and bind an abundant store of calcium ions, keeping them available for diffusion to the interior of the cardiac muscle fiber when a T tubule action potential appears.
The strength of contraction of cardiac muscle depends to a great extent on the concentration of calcium ions in the extracellular fluids. In fact, a heart placed in a calcium-free solution will quickly stop beating. The reason for this response is that the openings of the T tubules pass directly through the cardiac muscle cell membrane into the extracellular spaces surrounding the cells, allowing the same extracellular fluid that is in the cardiac muscle interstitium to percolate through the T tubules. Consequently, the quantity of calcium ions in the T tubule system (i.e., the availability of calcium ions to cause cardiac muscle contraction) depends to a great extent on the extracellular fluid calcium ion concentration.
In contrast, the strength of skeletal muscle contraction is hardly affected by moderate changes in extracellular fluid calcium concentration. This is because skeletal muscle contraction is caused almost entirely by calcium ions released from the sarcoplasmic reticulum inside the skeletal muscle fiber.
At the end of the plateau of the cardiac action potential, the influx of calcium ions to the interior of the muscle fiber is suddenly cut off, and calcium ions in the sarcoplasm are rapidly pumped back out of the muscle fibers into the sarcoplasmic reticulum and T tubule–extracellular fluid space. Transport of calcium back into the sarcoplasmic reticulum is achieved with the help of a calcium–adenosine triphosphatase (ATPase) pump (the sarcoplasmic endoplasmic reticulum calcium ATPase, SERCA2; see Figure 9-7 ). Calcium ions are also removed from the cell by a sodium-calcium exchanger. The sodium that enters the cell during this exchange is then transported out of the cell by the sodium-potassium ATPase pump. As a result, the contraction ceases until a new action potential comes along.
Cardiac muscle begins to contract a few milliseconds after the action potential begins and continues to contract until a few milliseconds after the action potential ends. Therefore, the duration of contraction of cardiac muscle is mainly a function of the duration of the action potential, including the plateau —about 0.2 second in atrial muscle and 0.3 second in ventricular muscle.
The cardiac events that occur from the beginning of one heartbeat to the beginning of the next are called the cardiac cycle . Each cycle is initiated by the spontaneous generation of an action potential in the sinus node , as explained in Chapter 10 . This node is located in the superior lateral wall of the right atrium near the opening of the superior vena cava, and the action potential travels from here rapidly through both atria and then through the A-V bundle into the ventricles. Because of this special arrangement of the conducting system from the atria into the ventricles, there is a delay of more than 0.1 second during passage of the cardiac impulse from the atria into the ventricles. This delay allows the atria to contract ahead of ventricular contraction, thereby pumping blood into the ventricles before the strong ventricular contraction begins. Thus, the atria act as primer pumps for the ventricles, and the ventricles in turn provide the major source of power for moving blood through the body’s vascular system.
The total duration of the cardiac cycle, including systole and diastole, is the reciprocal of the heart rate. For example, if the heart rate is 72 beats/min, the duration of the cardiac cycle is 1/72 min/beat—about 0.0139 min/beat, or 0.833 sec/beat.
Figure 9-8 shows the different events during the cardiac cycle for the left side of the heart. The top three curves show the pressure changes in the aorta, left ventricle, and left atrium, respectively. The fourth curve depicts the changes in left ventricular volume, the fifth depicts the electrocardiogram , and the sixth depicts a phonocardiogram , which is a recording of the sounds produced by the heart—mainly by the heart valves—as it pumps. It is especially important that the reader study this figure in detail and understand the causes of all the events shown.
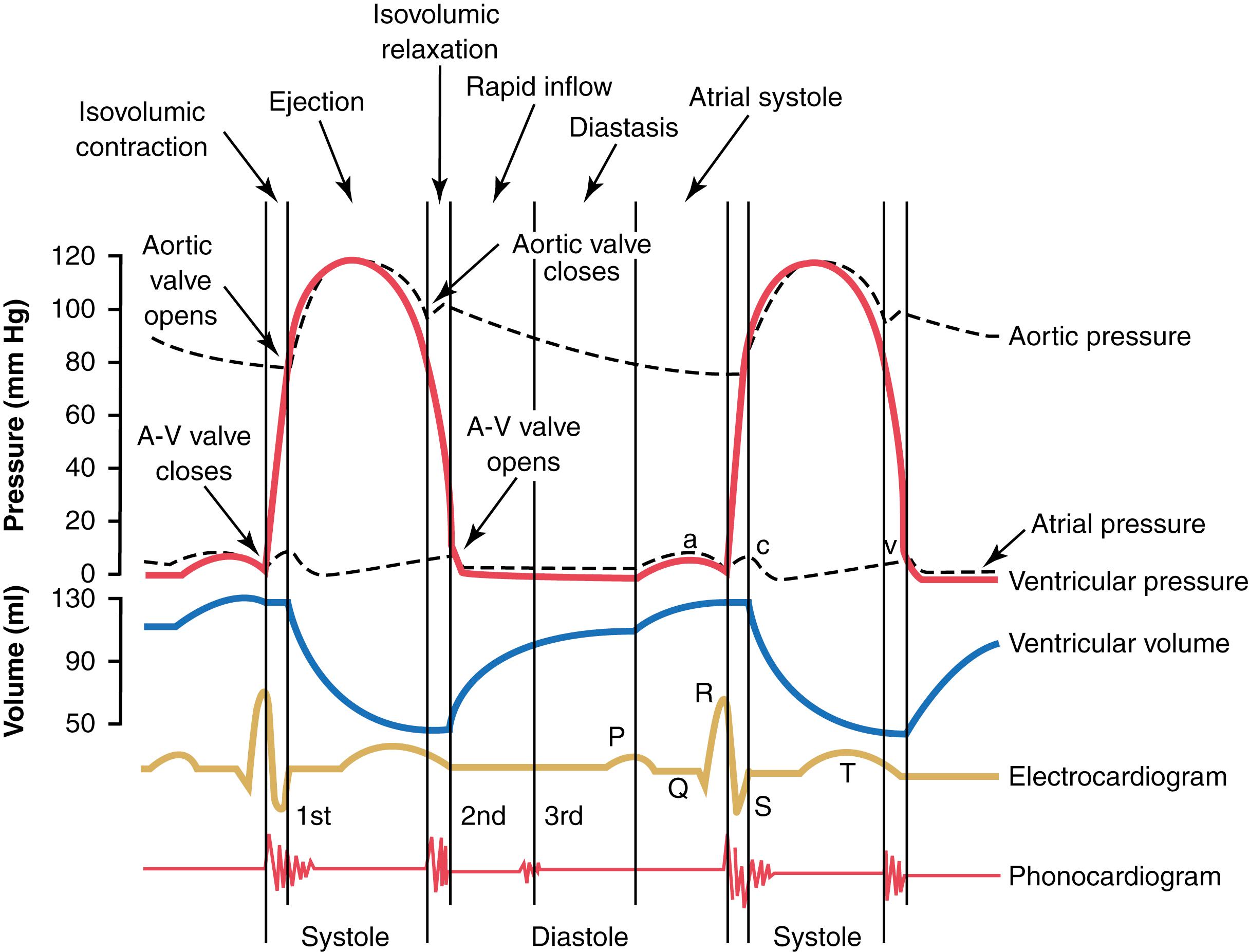
When heart rate increases, the duration of each cardiac cycle decreases, including the contraction and relaxation phases. The duration of the action potential and systole also decrease, but not by as great a percentage as diastole. At a normal heart rate of 72 beats/min, systole comprises about 0.4 of the entire cardiac cycle. At three times the normal heart rate, systole is about 0.65 of the entire cardiac cycle. This means that the heart beating very rapidly does not remain relaxed long enough to allow complete filling of the cardiac chambers before the next contraction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here