Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Cardiac disease has a significant association with neuromuscular diseases ( Table 3.1 ). In all cases, early recognition of the neuromuscular diagnosis can improve timely recognition of forthcoming cardiac disease. The extent and severity of cardiac disease can vary significantly within and between specific neuromuscular disorders. In some cases, cardiac disease is the presenting symptom, long before skeletal muscle symptoms develop. In other cases, where skeletal muscle weakness occurs first, the signs and symptoms of cardiac failure can be masked by limitations in the patient’s mobility and may not become apparent until cardiac failure is severe. Quality of life and longevity in some patients with muscular dystrophy are more dependent on disease of the cardiovascular system than on disease of the musculoskeletal system. Over the past 50 years, a more complete understanding of cardiac involvement in these patients has evolved. However, the specific etiologies and mechanisms of cardiac damage remain unclear. Although more data continue to emerge and improve the understanding of cardiac disease in these patients, there are still significant gaps in the etiology and best treatment practices. This chapter discusses the neuromuscular disorders most associated with cardiac disease and the current understanding of the proper diagnosis and treatment of these disorders.
| Diagnosis | Age of Onset of Cardiac Disease | Cardiac Symptoms | Electrocardiographic Findings | Echocardiographic Findings | Prognosis |
|---|---|---|---|---|---|
| DMD | Preclinical disease presents at 6–8 years Clinical disease pre-sents at 10–18 years |
AsymptomaticCHF with severe DCM | Common: Tall R waves in V1, V2, Q waves, BBB Arrhythmias more common with DCM progression |
Common: DCM |
Death of cardiac or respiratory complications at 20–30 years |
| BMD | Preclinical disease presents at 10–20 years Clinical disease rare in children, progresses with age, prevalent after 40 years |
AsymptomaticCHF with severe DCM | Common: Tall R waves, Q waves, BBB Arrhythmias more common with DCM progression |
Common: DCM |
Heart failure in the 40s Poor prognosis once heart failure is present Heart transplant eval |
| DMD/BMD carrier | Preclinical disease presents at 10–20 yearsClinical disease pre-sents at 30–50 years | AsymptomaticCHF with severe DCM | Common: Tall R waves |
Rare: DCM can develop in 30s |
Can have normal life expectancy Heart transplant eval in severe cases |
| XL-DCM | Clinical disease pre-sents at 20–50 years | AsymptomaticCHF with severe DCM | Common: Q waves, ST/T wave changes |
Common: DCM |
Poor survival after symptomatic Heart transplant eval |
| LGMD (types 1B, 2C, 2D, 2E, 2F, 2I) | Clinical disease varies with diagnosis | AsymptomaticCHF with severe DCM | Common: Types 1B, 2E Progressive 1°, 2°, 3° AVB Tall R waves, Q waves |
Common: DCM Rare : Type 2F |
Variable, depending on diagnosis Heart transplant eval |
| Myotonic dystrophy | Clinical disease pre-sents in adulthood | AsymptomaticSyncopeSudden death | Common: Type 1 1°, 2°, 3° AVB Afib/Aflutter, VT/VF |
Rare | Progressive cardiac involvement, death in 50s Sudden death |
| EDMD | Arrhythmias in 30–40 years; can be earlier in XL-EDMD | Presyncope/syncopeCHF (mostly AD-EDMD) | Common: Sinus bradycardia 1°, 2°, 3° AVB Afib/Aflutter, atrial standstill, VT/VF |
Rare: Risk for atrial thrombus due to arrhythmia |
Pacemaker placement at 30–40 years Heart transplant eval Sudden death |
| FSHMD | Arrhythmias in adulthood | Presyncope/syncope | Common: In adulthood 1°, 2°, 3° AVB SVT/VT |
Rare | Minimal cardiac involvement |
| Friedreich ataxia | Uncommon in children; increases with age | Asymptomatic | Common: LVH with repolarization abnormalities, arrhythmias |
Common: HCM ± LVOTO |
Death occurs 30–40 years |
| Barth syndrome | Clinical symptoms present at 3–6 months | CHF | Occasional: LVH with strain LAD Prolonged QTc Arrhythmias |
Common: DCM HCM LV noncompaction |
Improvement with cardiac medications Heart transplant eval |
| Pompe disease | Clinical symptoms have infantile onset | CHF | Common: Marked LVH Short PR interval |
Common: HCM |
Death can occur by 1 year without treatment |
| Mitochondrial disorders | Variable onset, depending on diagnosis | CHF syncope | Variable: ST/T wave abnormalities 1°, 2°, 3° AVB Arrhythmias |
Variable: DCM HCM |
Variable, depending on diagnosis |
| Congenital myopathies | Variable onset, depending on diagnosis | AsymptomaticCHF with severe DCM | Common: Tall R wave Q waves |
Occasional: DCM |
Usually more dependent on skeletal and respiratory function Heart transplant eval |
Cardiac involvement in Duchenne muscular dystrophy (DMD) occurs in all patients to varying degrees. Cardiac pathogenesis is similar to skeletal muscle where lack of dystrophin makes the myocyte plasma membrane susceptible to injury. Damage to the membrane leads to unregulated, calcium influxes into the cell causing inflammation, cell death, and fibrosis ( ). Further, loss of dystrophin affects the L-type calcium channels and mechanical stretch-activated receptors in myocytes, further exacerbating the influx of calcium ( ; ). The increased intracellular calcium leads to activation of proteases that begin a pathologic process of cell injury and death.
In a large study of 328 patients with DMD by , cardiac involvement was found in 26% of patients younger than 6 years old, 62% of patients 6 to 10 years old, 81% of patients 10 to 14 years old, 95% of patients 14 to 18 years old, and 100% of patients older than 18 years. Cardiac symptoms are unrelated to the severity of skeletal muscle disease, and one study showed that patients with stronger skeletal muscles were even more likely to die of cardiac disease than those with weaker muscles ( ). In a retrospective case-matched control study of 340 patients with DMD aged 2–28 years, 27% had cardiomyopathy among all age groups and mean age of onset of 16 years. The prevalence of cardiomyopathy correlated with increasing age, with 5% of 0–5 years old, 38% of 14–17 years old, and 61% of males >18 years old ( ). A more recent review of 408 males studied over a 10-year period until 2015 found 7% all-cause mortality. Thirty percent of those deaths were due to progressive heart failure or sudden cardiac death. Risk factors for death from any cause included young age at loss of ambulation, absence of glucocorticoid therapy, left ventricular (LV) dysfunction, and higher brain natriuretic peptide (BNP) levels. Lack of glucocorticoids was associated with cardiac cause of death ( ).
Despite frequent myocardial involvement, most patients are free of cardiovascular symptoms. Diagnosis of cardiac dysfunction is often difficult because patients are less active and do not have early clinical symptoms (i.e., exercise intolerance) ( ). As treatment of the skeletal and respiratory muscle systems improves, more patients with DMD are developing symptomatic heart disease. Approximately 72% of patients younger than 18 years were asymptomatic, but only 57% of patients older than 18 years old were symptomatic, even though all patients at this age were affected ( ). Gulati et al. studied 30 patients older than 6 years, and only 10% had symptoms or signs suggestive of heart failure. However, one third had cardiomegaly, 93% had electrocardiographic (ECG) abnormalities, and left ventricular ejection fraction (LVEF) was less than 55% in 64% of patients and less than 50% in 18% of patients (normal range is 55%–65%) ( ). Other studies found that only 15% to 22% of patients with DMD and cardiac disease reported symptoms ( ; ).
Recognition of cardiomyopathy in DMD requires active cardiac evaluation since signs and symptoms of cardiac dysfunction may be vague and nonspecific. Symptoms can include fatigue, weight loss, vomiting, sleep disturbance, inability to tolerate the daily regimen, and orthopnea. It is generally recommended that patients be referred to cardiology at diagnosis as asymptomatic children can have abnormal ejection fraction (EF) ( ; ). Duboc et al. found that 20% of asymptomatic children at age 10 years had abnormal EFs, further supporting early referral ( ).
In comparison to DMD, cardiac involvement in Becker muscular dystrophy (BMD) is frequently out of proportion to the skeletal muscle involvement and can be the main clinical problem ( ). Cardiomyopathy is rare before 16 years of age, but it increases progressively with age, eventually affecting more than 70% of patients older than 40 years ( ). There is significant variability, both within and between families, in the onset, severity, and progression of cardiac disease, as is true for skeletal muscle involvement ( ). One concern about the increased incidence of cardiac disease is the increased long-term workload on the heart because of slower progression of skeletal muscle weakness compared with DMD ( ). However, this may mostly be a reflection of the heterogeneity of disease progression seen in both BMD and DMD patients.
Dilated cardiomyopathy (DCM) can sometimes be the main pathologic finding in BMD. Despite the high proportion of DCM in BMD, only one third of patients are symptomatic. Patients with BMD and severe DCM can undergo cardiac transplantation with good results ( ). Hoogerwaard et al. studied 27 patients with a mean age of 37.5 years and a mean follow-up of 12.5 years. Only 5 of 27 patients (19%) had completely normal heart evaluations. ECG abnormalities increased from 44% to 71%, and 63% of the patients showed progression of cardiac abnormalities. The presence of DCM increased from 15% to 33% over the 12 years. Five of the patients died during the follow-up period, and four of these deaths were the result of congestive heart failure. Three of these patients were able to walk at the time of death. The mean age of death in these four patients was 42 years ( ).
Melacini et al. studied 28 patients with BMD ranging in age from 6 to 48 years with subclinical or benign skeletal muscle disease. Nineteen of these patients showed myocardial involvement, but only two were symptomatic ( ). Nigro et al. reviewed the clinical history of 68 patients and found preclinical cardiac involvement in 67% of patients younger than 16 years of age. Clinically evident cardiomyopathy was found in 15% of patients younger than 16 years, increasing to 73% in patients older than 40 years ( ). These studies show a high incidence of myocardial involvement among patients with mild or subclinical skeletal muscle symptoms that progresses with time.
A percentage of female carriers of DMD and BMD can develop DCM that can progress to heart failure and even lead to heart transplantation ( ; ). Politano et al. found preclinical or clinical evidence of myocardial involvement in 84% of DMD ( n = 152) and BMD ( n = 45) carriers. This increased with age, and 90% of carriers older than 16 years were affected. There were no statistically significant differences between DMD and BMD carriers. Only 11% of carriers were reported as having DCM, yet clinical symptoms were not reported ( ). studied 129 DMD and BMD carriers. ECG abnormalities were found in 47%, but DCM was found in seven DMD carriers (8%) and no BMD carriers. This agreed with the study of that found a 7% incidence of DCM in carriers. In a study of 20 carriers of DMD, evidence of cardiac fibrosis was detected in nine cases, which correlated with lower LVEF using cardiac magnetic resonance imaging (CMRI), higher creatine kinase (CK) levels, and shorter distances in 6-minute walk tests. Further, their pro-B-type natriuretic protein (BNP) levels were also elevated ( ). In these patients, DCM often occurs without any skeletal muscle symptoms.
X-linked DCM (XL-DCM) is a rare cardiomyopathy associated with increased serum CK levels, but an absence of significant skeletal muscle weakness. Berko and Swift first described a group of affected males and their mothers. The patients presented with DCM at 15 to 21 years and survived only 5 to 12 months after diagnosis. The mothers presented in their 40s with atypical chest pain and slowly progressing heart failure ( ). found mutations in the dystrophin gene of patients with XL-DCM who had normal dystrophin levels in skeletal muscle. These patients can have mild myopathic changes on skeletal muscle biopsy but have complete loss of dystrophin in cardiac muscle ( , ). Based on reviews, prevalence ranges from 3% to 7% in male patients with nonpaternally inherited XL-DCM who had no symptoms of muscular dystrophy ( ; ).
Limb-girdle muscular dystrophy (LGMD) is a heterogeneous group of diseases with variable cardiac involvement. Cardiac presentation can be similar to that of DMD because of the loss of dystrophin-associated glycoproteins that stabilize the dystrophin complex. Autosomal dominant (AD) LGMD 1 includes LGMD1 A–H and autosomal recessive LGMD 2 includes LGMD2 A–Y. AD forms include the genes for myotilin, lamin A/C, caveolin-3, Hsp40, desmin, transportin, and heterogeneous nuclear ribonucleoprotein D-like protein. Autosomal recessive forms include sarcoglycans, telethonin, fukutin related protein, titin, fukutin, and lamin alpha 2. LGMD1B (laminopathy) is associated with DCM, conduction defects, and high risk of sudden death ( ; ). Politano et al. studied patients with sarcoglycanopathies, and 11 of 20 patients had evidence of cardiac involvement. Patients with gamma and delta sarcoglycan deficiency had DCM, and patients with alpha and beta deficiency had preclinical involvement ( ). Melacini et al. studied patients with alpha, beta, and gamma sarcoglycan deficiency, and mild cardiac abnormalities were seen in 30% of patients who had severe skeletal muscle dystrophy. Four of 13 patients showed ECG abnormalities and two showed wall motion abnormalities on echocardiography. Patients were asymptomatic, and only one had a decreased LVEF of 43%. No correlation was found between the presence of cardiac abnormalities and the type of mutation or sarcoglycan gene involved ( ). Barresi et al. described two patients with beta sarcoglycan deficiency who had severe cardiomyopathy. One died at 18 years and the other died at 26 years of age ( ). Calvo et al. showed 10 patients with LGMD 2C who had ECG and echocardiographic abnormalities, especially of the right ventricle. Only one patient had decreased LV function ( ).
LGMD 1B (lamin A/C) is an AD disease associated with conduction defects. described a large French-Canadian family in which three of seven carriers of the gene had atrioventricular (AV) conduction blocks. Ben Yaou et al. described 13 patients with LGMD 1B who had conduction defects and arrhythmias. Seven of these patients needed a pacemaker or an implantable cardioverter defibrillator (ICD), and two underwent heart transplantation ( ). van der Kooi et al. studied 26 patients with LGMD 1B and 12 showed ECG abnormalities, including six cases of AV conduction block, four requiring pacemakers. Six patients also showed echocardiographic abnormalities including DCM ( ). Finally, van Rijsingen et al. studied a European cohort of 269 LMNA (lamin A/C) mutation carriers. A total of 48 people developed a malignant ventricular arrhythmia, of whom 11 received successful CPR and 12 died suddenly. Independent risk factors were nonsustained ventricular tachycardia (VT), LVEF <45% at first clinical contact, male sex, and non-missense mutations ( ).
LGMD type 2I is related to defects in fukutin-related protein and is significantly associated with cardiac disease. Wahbi et al. studied 23 patients with an average age of 32 years and found that 60% had decreased LVEF, 8% of which were severely decreased. None of the patients had significant arrhythmias, and no sudden death was recorded ( ). Poppe et al. studied 38 patients with LGMD 2I who were 10 to 61 years old. Overall, 55% of patients had cardiac involvement, which was defined as decreased shortening fraction, LV wall motion abnormalities, or ECG abnormalities. There was a tendency for cardiomyopathy to develop in patients with more severe skeletal muscle phenotypes, but 88% of patients with cardiac disease could still ambulate. Of 19 patients with a known clinical course, eight had symptomatic cardiac failure at 18 to 67 years of age ( ). An earlier study by the same group described 16 patients who were 11 to 53 years old. They found symptomatic cardiac failure in three patients at ages 28, 39, and 51 years and asymptomatic LV systolic dysfunction in three patients at 38, 57, and 58 years ( ). The possibility of severe cardiac disease was shown by D’Amico et al., who described the case of an 8-year-old boy who presented with LGMD 2I and severe cardiomyopathy. He required heart transplantation, with no clinical skeletal muscle weakness ( ). Murakami et al. identified six patients in four families with fukutin gene mutations who had DCM with no significant skeletal muscle involvement. One patient died of congestive heart failure at 12 years and one patient received a heart transplant at 18 years. The other patients had cardiomyopathy at 17, 27, 30, and 46 years ( ).
These studies show that cardiac disease is significantly involved in some forms of LGMD, and a specific muscle diagnosis is required to best anticipate cardiac complications.
Myotonic dystrophy (DM) is an AD disorder that presents in adulthood with myotonia and weakness of the skeletal muscles. There are two major subtypes: DM type I is caused by increased CTG repeats and DM type II is caused by increased CCTG repeats. The severity of cardiac disease in these patients is unrelated to the severity of skeletal muscle disease, but cardiac disease is causative in 30% of deaths in DM ( ; ; ). Fibrosis along the conduction system leading to myocyte hypertrophy and fatty infiltration makes arrhythmia the most common complication ( ; ; ).
Baseline ECGs frequently have QRS and PR prolongation with time. Groh et al. studied 406 patients with confirmed DM type I with abnormal CTG repeat sequences. Ninety-six of these patients had evidence of non-sinus rhythm, prolonged QRS duration (>120 milliseconds), or heart block. These patients were older, had more CTG repeats, and had more severe muscular disease. Twenty-nine of the patients with ECG abnormalities had atrial tachyarrhythmias, but only four had ventricular tachyarrhythmias, and of the patients with initially normal ECG findings ( n = 310), 69 patients developed severe abnormalities. During follow-up, 81 (20%) of the 406 patients died: 27 (33%) died suddenly, 32 (40%) died of respiratory failure, and 5 (6%) died of other cardiac causes. Analysis shows that rhythm other than sinus, PR >240 milliseconds, QRS >120 milliseconds, or second- or third-degree heart block all increased the risk of sudden death ( ). Ventricular tachyarrhythmias were commonly observed in patients who died suddenly. The presence of a severe ECG abnormality had a sensitivity of 74% for predicting sudden death ( ; ). Lund and colleagues reviewed 1146 patients, 485 of whom had positive genetic testing for DM type 1. The standard incidence rate for any cardiac disease was 3.41 and as high as 6.91 for cardiomyopathy, heart failure, arrhythmia, and device implantation. Any cardiac disease was present in 80% of DM patients and risk of disease increased with age ( ). Petri et al. retrospectively reviewed 1828 cases of DM type I and found first-degree AV block in 28%, QTc prolongation (>440 milliseconds) in 22%, and QRS prolongation in 20%. LV dysfunction was reported in only 7% of cases ( ).
In DM type II, patients can have DCM and arrhythmias. Schoser et al. described four patients with DM type II who had sudden death. Three of the patients were asymptomatic, and one had symptoms of heart failure. All of the patients had DCM, and fibrosis of the conduction system was found in two of them ( ). A case-control series of 38 DM type 2 patients showed that there were 15 patients with cardiac abnormalities, including 14 with conduction defects, six with systolic dysfunction, six with arrhythmias, and five patients with strokes. When compared to DM type 1 patients, there were fewer conduction defects, similar rates of arrhythmia, but more LV systolic dysfunction ( ). DCM is rare, but described as well ( ). In a series of 80 patients with DM and symptoms of dyspnea or exertional fatigue, 44% had functional or structural abnormalities. Abnormalities were more common in older men. LV systolic dysfunction was the most common finding, and LV dilatation, hypertrophy, and fibrosis were also commonly seen ( ).
Emery-Dreifuss muscular dystrophy (EDMD) is related to loss of the nuclear membrane proteins from XL ( STA , EMD , and FHL1 ) or autosomal recessive ( LMNA ) or AD loss of lamin A/C ( LMNA, SYNE1, SYNE2 , and TMEM43 ) mutations ( ). Almost half of patients with EDMD carry mutations in emerin, lamin A/C, nesprin1, and nesprin2. In XL-EDMD, muscle disease is milder and progresses more slowly than in AD-EDMD. In many patients, the severity of skeletal muscle disease is not significant, and the initial presentation is secondary to cardiac disease. Cardiac disease tends to start as sinus bradycardia and first-degree heart block and can evolve into third-degree (complete) heart block and atrial arrhythmias that lead to atrial paralysis. LV dysfunction can occur after the development of arrhythmias. The long-term prognosis of these patients depends significantly on the severity of cardiac involvement.
Boriani et al. studied 18 patients with EDMD as a result of both emerin and lamin deficiencies. Arrhythmias were found in 15 patients, including all of the patients with emerin deficiency. Only one patient had significant heart failure and presented with atrial flutter and AV block necessitating a pacemaker. This patient did not improve and eventually required heart transplantation. One patient had right-sided heart failure as a result of AV block that resolved with pacemaker implantation, and three other patients had mild to moderate LV dysfunction with limited or no impairment in daily activities ( ). It is generally thought that AV conduction defects and arrhythmias precede LV systolic dysfunction and pacemakers may prevent progression ( ; ).
Buckley et al. described three patients with XL-EDMD. The first presented at 19 years with atrial tachycardia and variable AV conduction. At 24 years of age, he was noted to have atrial standstill and junctional bradycardia of 37 beats per minute. A pacemaker was implanted at 29 years because of periods of atrial tachycardia and atrial arrest with junctional escape beats. The patient was then free of cardiac symptoms. His nephew was found to have junctional bradycardia at 17 years. No tachyarrhythmias were noted, and a pacemaker was implanted. He developed atrial fibrillation at 22 years, with a history of brief episodes of visual disturbances. Anticoagulants were administered and continued with intermittent atrial fibrillation. This patient’s brother had junctional bradycardia at 15 years and had a pacemaker implanted. He remained asymptomatic after the pacemaker was placed ( ). An additional case report of a patient with an FHL1 mutation with a hypertrophic cardiomyopathy phenotype is noted. The patient had LV hypertrophy (LVH) on ECG and asymmetric LVH without obstruction on echocardiogram and CMRI ( ). Finally, a large family with an inherited FHL1 mutation was described. There was 44% penetrance, 100% for males and 18% for females. Affected males had mild hypertrophy, systolic dysfunction, and abnormal diastolic function. Carriers had long QTc. One patient had a cardiac arrest and there were two cardiac transplants with arrhythmogenic cardiomyopathy suspected in the explanted hearts ( ).
Sanna et al. studied 10 patients with AD-EDMD. The average age at the first evidence of cardiac disease was 18.3 ± 9.7 years. ECG findings were abnormal in 8 of 10 patients, showing atrial fibrillation, atrial standstill, and AV conduction abnormalities. Holter recordings showed five patients with both atrial and ventricular arrhythmias, four associated with AV conduction abnormalities. Five patients had nonsustained VT. On echocardiography, only one patient had a mild reduction in LVEF. One patient showed mild LV dilation with normal function, and another patient showed right ventricular enlargement with a ventricular filling pattern consistent with a restrictive cardiomyopathy. Pacemakers were implanted in three patients. One patient who had a pacemaker because of atrial fibrillation with a slow ventricular response died suddenly at 48 years. Four patients had various degrees of LV dysfunction ( ).
Brodsky et al. described a single family found to have a lamin A/C mutation transmitted in an AD pattern in five of 14 members. The five affected family members had minimal skeletal muscle weakness, but two had severe cardiomyopathy, AV block, and VT. One of these patients received a heart transplant, and the second had sudden death ( ).
Fatkin et al. studied 85 members of five families with EDMD and found 44 with lamin A/C mutations and 39 with cardiovascular disease. The mean age of disease onset was 38 years (range, 19–53 years), and often the diagnosis was based on asymptomatic ECG changes. Progressive abnormalities developed with increasing age. In all, 34 of 39 had sinus node dysfunction or AV conduction disease and 23 affected members had atrial fibrillation or flutter. Twenty-one patients had pacemakers implanted, and 25 of 39 had DCM. Heart transplant was required in six members because of rapid progression of heart failure, and 11 of the 25 died suddenly between the ages of 30 and 59 years ( ). Atrial standstill has been described in a patient with a lamin A/C mutation ( ).
Facioscapulohumeral muscular dystrophy (FSHMD) does not appear to be a major cause of myocardial disease but is associated with conduction defects. Laforêt et al. studied 100 patients with FSHMD and found five with AV conduction defects or arrhythmias (supraventricular tachycardia, VT), but no structural or functional cardiac defects ( ). found no evidence of cardiac changes in 31 patients with FSHMD. Stevenson et al. studied 30 patients with well-documented FSHMD. ECG abnormalities were present in 60% of patients, and abnormal electrophysiologic (EP) findings were present in 27% of patients. Atrial flutter or fibrillation was induced in 10 of 12 patients during EP studies and sinus node function was abnormal in three patients ( ).
Friedreich ataxia is an autosomal recessive disorder caused by repeat mutations in the frataxin gene. Patients usually have ataxia with significant, but variable, progression over time. Patients have hypertrophic cardiomyopathy and show abnormal repolarization and arrhythmias on ECG findings. Tsou et al. studied 99 patients and found that the cardiac phenotype consists of LVH and fibrosis with scarring, arrhythmias, and progressive heart failure and is the most common cause of death. DCM was the most common cause of death with 59% ( ). Weidemann et al. reviewed 205 patients with multiple imaging modalities and stratified patients into four categories based on the LV septal measurement in diastole (IVSTd) and showed that 32% were normal and 40% had mild, 16% had moderate, and 12% had severe disease. Patients in the severe category had dilation of the LV, significant ECG abnormalities, and LVEF <50%. The group also found that younger patients had more advanced disease, likely signifying that more affected individuals present younger ( ). In a series of 32 patients with genetically proven Friedreich ataxia, Weidemann and colleagues found that almost all patients had some degree of cardiac involvement, with T wave inversion as the earliest sign. There was progression of the cardiomyopathy from mild to advanced stages, with an initial increase in wall thickness and then later decreased wall thickness and LV dilatation leading to end-stage cardiomyopathy ( ).
Barth syndrome is an XL disorder caused by mutations in the taffazin gene that result in abnormal mitochondria. Patients have a spectrum of symptoms, including skeletal muscle weakness, neutropenia, growth delay, and cardiomyopathy. Cardiac disease associated with Barth syndrome has a variable presentation unrelated to neurologic symptoms. In a study by Clarke et al., 151 reported cases of Barth syndrome was found in the literature. They note descriptions of several cardiac abnormalities ranging from dilated or hypertrophic cardiomyopathy to prolonged QTc and sudden death ( ). A registry study from Roberts et al. indicated that cardiac disease is the most common presenting symptom and is typically present before age 5 years and 70% within the first year of life. Multiple cardiomyopathies are described and 12% of patients required transplantation ( ).
Pompe disease is a rare autosomal recessive disorder caused by a deficiency in acid alpha-glucosidase, a lysosomal enzyme that degrades glycogen. Symptoms can begin at two months of age in the infantile-onset form, and approximately 88% of these patients have hypertrophic cardiomyopathy ( ). Death often occurs before 12 months, so long-term consequences are not known. ECGs can show large QRS complexes with short PR intervals. Nonspecific cardiac abnormalities are present in juvenile and late-onset Pompe disease but typically only present on CMRI ( ; ). Enzyme replacement therapy has significantly altered the disease course in treated infants.
Mitochondrial disorders, most often maternally inherited, are caused by specific defects in the mitochondrial respiratory transport chain or oxidative phosphorylation. Because of the high energy requirements of cardiac tissue, the heart is affected in these disorders. Cardiac manifestations include DCM and hypertrophic cardiomyopathy, AV conduction disturbances, and arrhythmias ( ).
Congenital muscular dystrophies constitute a heterogeneous group of disorders with varying degrees of cardiac involvement. Generally, a primary cardiomyopathy has not yet been seen in patients with ryanodine receptor 1 (RYR1) and myotubularin (MTM1) genes. Primary cardiomyopathy has been reported in patients with actin alpha 1, dynamin 2, and tropomyosin 2 mutations ( ). found decreased cardiac function in patients with merosin-positive congenital muscular dystrophy. showed increasing cardiac dysfunction as a function of age in Fukuyama-type congenital muscular dystrophy. published 143 cases of nemaline myopathy in which six infants had transient congestive heart failure and one had LV systolic dysfunction with congenital long QTc syndrome. Hypertrophic cardiomyopathy, DCM, and sudden cardiac death have also been reported ( ; ; ; ; ; ; ). In patients with titin mutations with multi-minicore-like disease, restrictive cardiomyopathy, hypertrophic cardiomyopathy, DCM, ventricular arrhythmias, and sudden cardiac death have been reported ( ; ; ; ; ; ; ; ; ). Heller et al. presented a series of three children with LMNA-related muscular dystrophy presenting in infancy. They described atrial level arrhythmias in all three and heart failure symptoms by the age of 5 years. Generally, children developed right heart failure symptoms including diarrhea and peripheral edema prior to a decrease in LVEF ( ). In these disorders, the prognosis is usually more dependent on skeletal and respiratory muscle weakness than on cardiac disease.
In summary, cardiac disease can be a significant comorbidity in neuromuscular disorders. The recognition and proper treatment of cardiac disease are important aspects of standard of care. While the commonly associated neuromuscular disorders were discussed previously, there are a significant number of neuromuscular diseases not commonly associated with cardiac disease. However, there are occasional case reports of cardiac disease in patients with these disorders, often related to stressful events ( ; ). Therefore, cardiac evaluations should be a consideration in any neuromuscular patient with concerning or uncommon symptoms.
It is of vital importance to obtain a complete history of the type of muscular dystrophy and current treatments. Special attention should be given to the family history, especially in cases of undiagnosed dystrophies. Two or more affected males in a single family should raise concern about a familial inheritance pattern, as is seen with XL-DCM, especially if there is no significant history of muscle weakness. Also, a family history of sudden death should raise suspicion for inherited cardiomyopathies.
Because these patients are inactive and often do not have significant exertional symptoms, it is important for the physician to ask specifically about changes in the activities of daily living. Is there increased fatigue? Does a child now use two pillows to sleep instead of one? Are there any changes in appetite or chronic nausea? Has there been weight loss? These are subtle changes that patients and caregivers may not recognize as concerning symptoms. Has the patient had any episodes of palpitations or dizziness? Arrhythmias can be symptomatic in young patients, but because of conduction abnormalities associated with some muscular dystrophies, they can occur with normal or even low ventricular rates, causing patients to remain asymptomatic ( ; ).
On physical examination, cardiac findings can be nonspecific but may provide initial clues to the presence and extent of cardiac disease. Vital signs can include tachycardia in patients with DMD and increased blood pressure as a result of steroid use. On examination of the neck, cannon A waves in the jugular venous pulse are suggestive of AV conduction disease, and loss of A waves can be related to atrial fibrillation or atrial standstill. Increased jugular venous distention can be present in heart failure. During palpation of the chest, displacement of the point of maximal impulse to the left and inferolaterally is caused by an enlarged left ventricle. The point of maximal impulse can also be displaced secondary to scoliosis. On auscultation, there is usually a regular rhythm, with normal S1 and S2. Irregular rhythms are associated with atrial fibrillation. A mid-systolic click secondary to mitral valve prolapse is sometimes appreciated in BMD. An S3 gallop can be heard during acute congestive heart failure and an S4 gallop can be heard secondary to LV dysfunction. Systolic ejection murmurs can be associated with DMD, and systolic regurgitant murmurs, often as a result of mitral regurgitation, can be heard in BMD ( ). found systolic ejection murmurs with grade I to II intensity in approximately 10% of patients with DMD. In Friedreich ataxia, systolic ejection murmurs can be present as a result of subaortic stenosis from LVH. Hepatomegaly can be found on abdominal examination but can be difficult to palpate because of positioning and scoliosis. Examination of the extremities often shows dependent edema when heart failure develops.
The ECG is an important tool for the diagnosis of arrhythmias, and muscular dystrophies can often have subtle early ECG changes. A 12-lead ECG examination provides noninvasive assessment of cardiac rhythm, ventricular axis, chamber enlargement, and conduction abnormalities or arrhythmias. The tracing speed can be increased (to 50 mm/second) to aid in the diagnosis of conduction abnormalities.
Sinus tachycardia is found in most (up to 75%) patients with DMD, even when these patients are nonambulatory ( ; ; ; ). This tachycardia occurs in childhood and persists into adulthood. In an early study of DMD, Gilroy et al. presented findings in 139 patients with DMD who were four to 35 years old. The most common clinical finding was sinus tachycardia, present in 124 cases (89%). The tachycardia was labile and appeared with minimal stimulation (e.g., raising the bed) ( ). In another study, sinus tachycardia was seen in 78% of patients with DMD ( ). The exact cause is unknown, but possible etiologies include compensatory tachycardia secondary to ventricular dysfunction, autonomic dysregulation, or fibrosis of the sinoatrial node and conduction system.
Another common ECG finding is tall R waves in both DMD and BMD ( Fig. 3.1 ). Abnormally tall R waves in leads V1 to V3 were found in a study of patients with DMD ( ). also showed prominent R waves in V1 in 88% of patients with DMD and 47% of patients with BMD. Other studies confirmed the prominent R waves in patients with DMD and BMD ( ; ; ). These forces represent a loss of posteriorly directed forces because of selective fibrosis of the posterobasal portion of the left ventricle that is common in dystrophic myocardium. This correlation was pathologically confirmed in a previous study ( ).
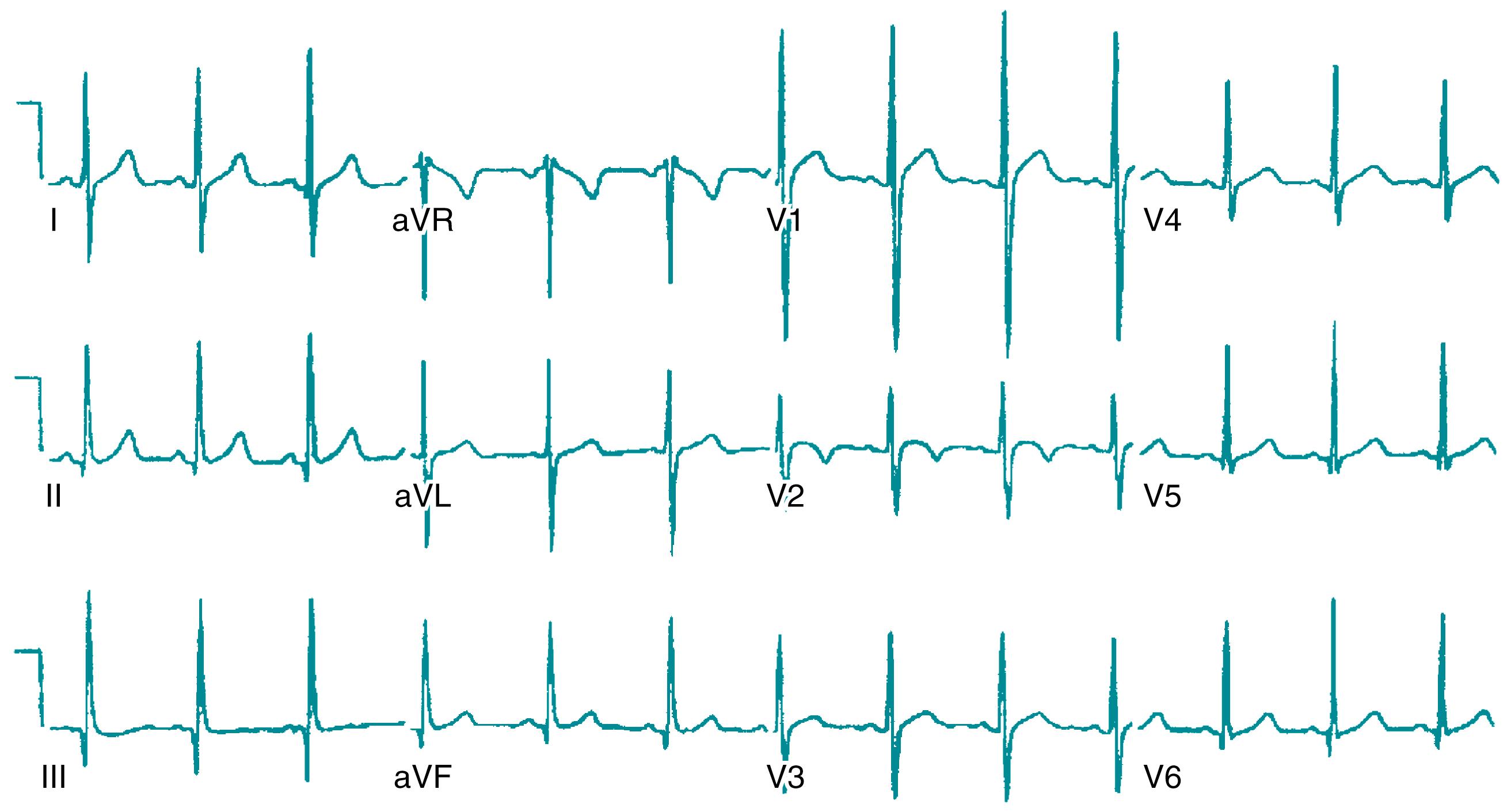
This myocardial fibrosis can also extend laterally and produce large Q waves on surface ECG findings (see Fig. 3.1 ). Q waves are most frequently seen in the lateral leads (I, aVL, V6) and less frequently in the inferior (II, III, aVF) or anterior (V1–V4) leads ( ; ; ). Lateral lead Q waves were seen in 73% of patients with DMD and 37% of those with BMD ( ). In DMD, lateral Q waves were present in 54% of patients compared with inferior Q waves in 30% of patients ( ). studied patients with BMD and found 33% with Q waves in the lateral leads and 11% with Q waves in the inferior leads. There is no correlation between baseline ECG findings and presence or absence of DCM; thus, ECG screening is insufficient and echocardiography or CMRI is required ( ). Acute presentation with chest pain can be associated with ECG ST segment elevation, especially in the inferior and lateral precordial leads, and is related to acute exacerbation with features consistent with myocarditis ( ).
Arrhythmias and conduction defects can also be present. Premature atrial contractions are common in DMD ( ). Other atrial arrhythmias, including flutter and fibrillation, and premature ventricular contractions are also seen in DMD ( Fig. 3.2 ) ( ). found ventricular arrhythmias in 32% of patients with DMD who were studied. Melacini et al. found arrhythmias on ECG tracings in patients with BMD, including benign, isolated, monomorphic, and polymorphic premature ventricular contractions. Ventricular arrhythmias were documented in one patient who died suddenly ( ). Conduction defects are also frequent. Many patients with DMD and BMD are found to have bundle branch block patterns, but heart block is rarely seen ( ; ; ).
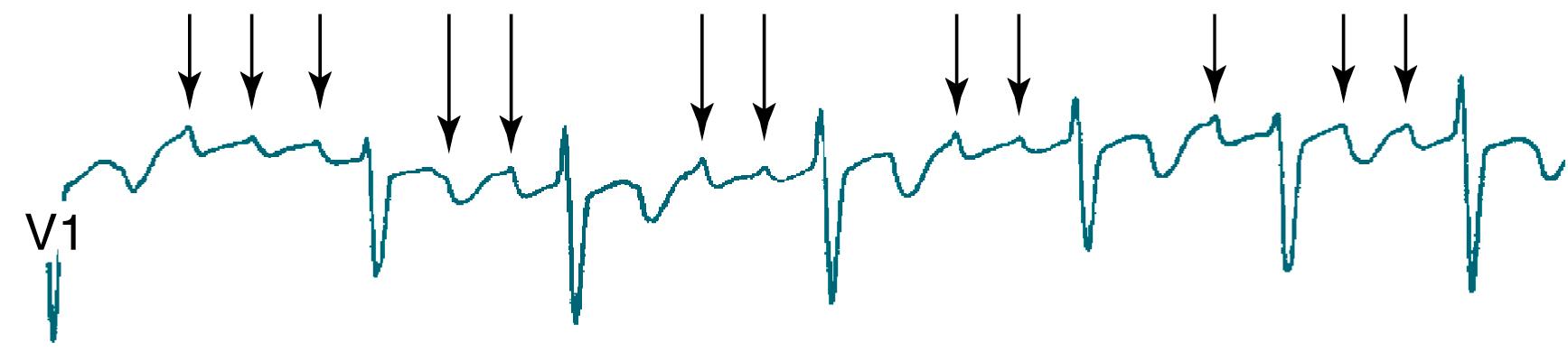
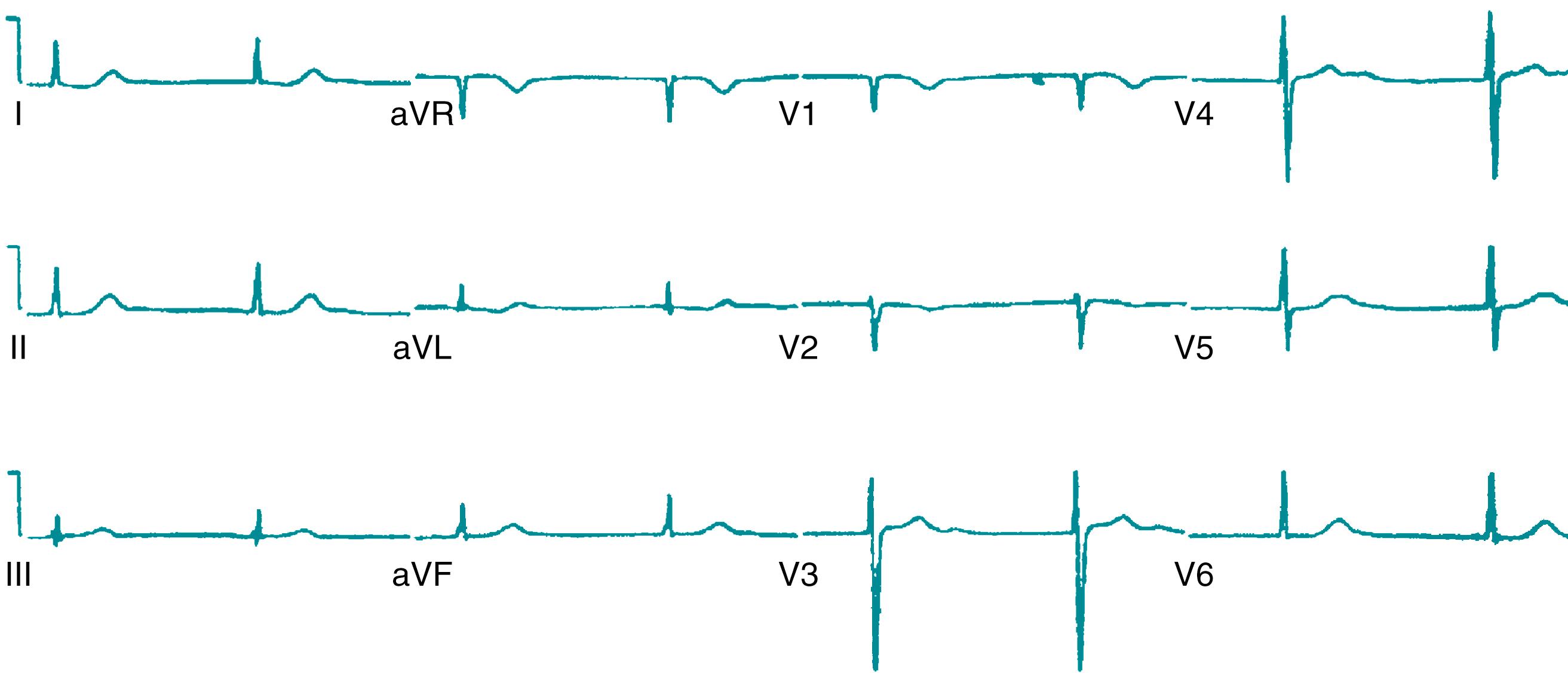
An ECG is most important in other muscular dystrophies where conduction defects are more prevalent. In LGMD 1B, AV conduction defects are primarily seen. These defects initially begin as a prolonged PR interval but become progressively more severe over time and can develop into complete heart block. Atrial fibrillation with a variable ventricular response is seen ( ; ; ). In LGMD 2C and 2I, along with AV conduction defects, abnormal findings include dysmorphic notched P waves, tall R waves, Q waves, inverted T waves, and ectopic beats ( ; , ). MD types I and II and EDMD, both XL and AD, are significantly associated with progressive AV conduction defects. Often these are the first and only presenting symptoms because muscular weakness has not developed. In a retrospective review of 1800 patients with DM type I, the most common finding was first-degree AV block in 28% of patients, with QTc >440 milliseconds in 22% of patients. In this series, atrial fibrillation and flutter were present in 5% of patients. Pacemakers were required in 4% of patients and 1% required an ICD ( ). Atrial fibrillation and flutter are present in approximately 25% of patients with DM type I ( ; ; ; ; , ; ; ). As a late consequence, atrial standstill can develop in patients with DM ( Fig. 3.3 ).
The ECG results can show many other pathologic changes that indicate myocardial damage. These include ST segment and T wave changes, shortened PQ interval, increased cardiomyopathy index (QT/PQ), prolonged QTc, and increased QT dispersion ( ; ; ; ; ). Repolarization abnormalities are common in Friedreich ataxia (FA). In a study by Child et al., 79% of patients showed ST/T wave abnormalities, and T wave inversion was an early sign of FA cardiomyopathy progression ( ; ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here