Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Infants with special problems may require procedures, surgeries, or hospitalization to maintain and optimize their health or development. Breastfeeding and breast-milk feeding should be protected throughout these interruptions in an infant’s health routine because human milk may offer unique benefits to their health in this period.
Breastfeeding is the ideal and preferred feeding method for a newborn. Occasionally infant problems interfere with breastfeeding and require the attention of the infant's physician to diagnose and treat the infant’s problem and support breastfeeding (e.g., cystic fibrosis).
Guidelines for preprocedural or preoperative fasting recommend 6, 4, and 1 to 2 hours for solids (and nonhuman milk), breast milk, and clear liquids, respectively. Expressing and storing breast milk in this period of nothing by mouth for the infant will ensure the mother’s milk supply is maintained. After minor procedures or surgeries, an infant can return to breastfeeding as soon as the infant is able to feed by mouth.
Cow’s milk protein allergy can occur in exclusively breastfed infants but is less common than in the formula-fed infant. An oral food challenge is usually not necessary or indicated, but having the mother initiate an elimination diet while continuing to breastfeed is often the first intervention.
Metabolic disorders (galactosemia, phenylketonuria) can interfere with adequate infant feeding. Specialized formulas without the potentially dangerous substrate often supplant breastfeeding. In some instances, some breast milk can be fed in addition to the specialized formula.
Careful early breastfeeding instruction and hands-on guidance are important, along with ongoing support to assist mothers and parents in identifying the challenges or difficulties of breastfeeding related to infant illness, develop solutions, and optimize infant nutrition despite their illness. (Hypernatremic dehydration is just one example of infant illness that should be preventable by this approach; hyperbilirubinemia should be manageable with continued good breastfeeding, and ankyloglossia is an example of an infant condition that should be managed simultaneously as breastfeeding continues to be facilitated and supported.)
Breastfeeding has been discouraged in infants with congenital heart disease out of concern for destabilization of the cardiorespiratory system by the act of breastfeeding. Evidence disproves this concern, and breast milk benefits the infant in preventing necrotizing enterocolitis (NEC), improving weight gain, and optimizing long-term health benefits.
In this era of concern for bedsharing and sudden infant death syndrome (SIDS), bedsharing with breastfeeding (breastsleeping) with an emphasis on safer sleeping and risk minimization with bedsharing are recommended to optimize safe sleeping and successful breastfeeding.
Breastfeeding is a natural behavior for infants and provides the ideal nourishment, but some infants with complicating issues need special assistance or adjustments. 1 Infants with structural abnormalities, metabolic challenges, or neurologic difficulties; stressed infants; and twins and triplets will be discussed in this chapter. Prematurity is discussed in Chapter 14 . In this chapter we will briefly review the management of the specific medical conditions and discuss the management of breastfeeding in relation to the medical condition and optimal nutrition.
Infants with special problems may require procedures, surgeries, or hospitalization to maintain and optimize their health or development. Breastfeeding and breast-milk feeding should be protected throughout these interruptions in an infant’s routine and may be a solution to the unique problems faced during them.
A 2017 systemic review of procedural pain relief for neonates was reported by Benoit et al. 2 Fifteen studies reported on the use of breastfeeding or expressed breast milk in full-term infants, and six reported on preterm infants. Direct breastfeeding was more effective than maternal holding, maternal skin-to-skin contact, topical anesthetics, and music therapy and was as effective or more effective than sweet-tasting solutions in term infants. Expressed breast milk was not consistently found to reduce pain response in full-term or preterm infants. The studies generally had moderate to high risk of bias. The review concluded that there is sufficient evidence to recommend direct breastfeeding for procedural pain management in full-term infants but not expressed breast milk.
A Cochrane systemic review and meta-analysis of procedural pain relief for infants greater than 28 days was published in 2016. 3 Ten studies with a total of 1066 infants were included. All the studies were conducted during early childhood immunization, and all were rated as being at high risk of bias. Breastfeeding reduced behavioral pain responses (cry time and pain scores) during vaccination compared with no treatment, oral water, and other interventions such as cuddling, oral glucose, topical anesthetic, massage, and vapocoolant. Moderate-quality evidence from six studies ( N =547 infants) revealed that breastfeeding compared with water or no treatment resulted in a 38-second reduction in cry time (mean difference [MD]=–38, 95% confidence interval [CI] –50 to–26; p < 0.00001), and moderate-quality evidence from five studies ( N =310 infants) disclosed that breastfeeding was associated with a 1.7-point reduction in pain scores (standardized mean difference [SMD]=–1.7, 95% CI–2.2 to–1.3). 3
Various societies of anesthesia (American, European, and Scandinavian) have guidelines recommending preoperative fasting for intervals of 6, 4, and 2 hours for solids (and nonhuman milk), breast milk, and clear fluids, respectively. 4 , 5 , 6 The Academy of Breastfeeding Medicine (ABM) supports such recommendations in its Clinical Protocol 25: Recommendations for Preprocedural Fasting for the Breastfed Infant: “NPO” Guidelines. 7 Gastric emptying rates are the primary difference in determining the preprocedural fasting time. The use of clear liquids up to 2 hours, or even 1 hour, before the procedure and nonnutritive sucking on a pacifier or empty breast can be temporary comfort measures. 8 Expressing and storing breast milk during the period of “nothing by mouth” (NPO) is appropriate and will ensure that the mother’s milk supply is maintained. For minor procedures under anesthesia, a stable, otherwise-healthy child for which the surgical procedure does not prevent oral intake can resume breastfeeding as soon as the infant is awake.
Anesthesia is a main concern when any patient is scheduled for surgery. Traditionally, a patient has been ordered to have NPO status after midnight or 6 to 8 hours preoperatively. Young infants accustomed to feeding every 4 hours are often frantic when maintained without feeding before going to the operating room. The guidelines, as described previously, are appropriate.
One study reported postdischarge breastfeeding outcomes for a group of infants with complex anomalies that required surgery. 9 One hundred and sixty-five mother–infant pairs cared for in a tertiary care children’s hospital and who had surgery from 2009 to 2012 were included. Of these infants, 60.1% were still receiving human milk at 6 months of age, and 34.5% were still receiving human milk at 12 months of age. Exclusive human milk nutrition continued in 54.3% of infants at 3 months and 35.6% at 6 months. The average duration of ongoing use of human milk was 8 months. Consistent with the required surgery, 30.7% of the infants were still receiving gavage feeding postdischarge. This significant improvement in the level of ongoing use of human milk for infants undergoing surgery was accomplished with an organized lactation program, nursing staff with specific breastfeeding education, and a medical culture that strongly supports breastfeeding and the use of human milk. An infant who requires surgery or rehospitalization can and should be breastfed postoperatively in most cases. The gravity of the surgery and the length of the recovery phase will determine the time necessary for the mother to pump and manually express her milk to maintain her supply. The infant who is hospitalized is already traumatized by the separation, the strange surroundings and contact with multiple unknown persons, and the underlying discomfort of the disease process itself. If the infant is to be fed orally, feeding should be at the breast as often as possible. If the mother can room-in or the hospital has a care-by-parent ward, this works well. If obligations to other family members make it impossible for the mother to stay, she can pump her milk and bring it in fresh day by day or frozen if the time interval between visits is longer than a day. Freezing will destroy the cellular content, but this is not a major problem beyond the immediate neonatal period. The infant should not be subjected to the added trauma of being weaned from the breast when the infant needs the security and intimacy of nursing most, unless weaning is absolutely unavoidable.
The medical professional needs to be aware of these infants and mothers and their special needs for support. An opportunity to discuss the breastfeeding aspect of the infant's management should be offered by the physician. The pediatrician should assume the advocacy role. The parents should not have to fight for the right to maintain breastfeeding. Plans for pumping and saving milk should be discussed and provided. If the infant is recovering in an open ward or a room with other infants and their parents without adequate privacy, a separate room should be provided for the mother to nurse or pump her milk. This room should be clean, neat, adequately illuminated, and equipped with a sink for washing hands. Storerooms, broom closets, bathrooms, and staff dressing rooms are inappropriate. If a mechanical pump is to be used, it should be kept clean and operable with individual tubing and attachments that come in contact with the milk or the breast. If a breast pump is not provided in the pediatric department, it should be available from the newborn unit or neonatal intensive care unit (NICU).
Arrangements for providing sterile containers for collecting milk and storing it are discussed in Chapter 22 . Occasionally, a mother may become so concerned about the adequacy of her milk for her infant that she may nurse much too frequently. Her child may need more nonnutritive sucking and holding than usual. A physician should reassure the mother when pointing this out. The father or other parent should also be encouraged to understand all the tubes, bandages, and appliances the infant may have attached. They are important members of the parenting team and should provide some of the soothing and especially the nonnutritive cuddling.
Postmature infants are full-grown, mature infants who have stayed in utero beyond the full vigor of the placenta and have begun to lose weight in utero. 10 They are usually “older-looking” and have a wide-eyed countenance. Their skin is dry and peeling, and subcutaneous tissue is diminished; thus the skin appears too large. These infants have lost subcutaneous fat and lack glycogen stores. Initially, they may be hypoglycemic and require early feedings to maintain adequate blood glucose levels. If breastfed, the infants should go to the breast early, taking special care to maintain body temperature, which is labile in postmature infants who lack the insulating fat layer. Blood sugar levels should be followed with a frequency and duration commensurate with the specific risk factors of the individual infant, and monitoring should continue until normal, prefeed blood sugar levels are consistently, successively obtained. 11 Initially, these infants may feed poorly and require considerable prodding to suckle. In extreme cases of hypoglycemia, an intravenous (IV) infusion may be necessary, and management should follow guidelines for any infant who has hypoglycemia that is resistant to routine early feedings. Because the infants lack glycogen stores, hypoglycemia may persist, and glucagon is contraindicated because no glycogen stores are present to be stimulated. Calcium problems, on the other hand, although common in these infants, generally are rare if the infant is adequately breastfed early because of the physiologic calcium–phosphorus ratio in breast milk. After postmature infants begin to feed well, they tend to catch up quickly and adapt well. Problems with hyperbilirubinemia seldom occur because their livers are mature. Postmature infants gain well at the breast once they stabilize.
Infants who have been compromised in utero or during delivery because of insufficient placental reserve, cord accidents, or other causes of intrauterine hypoxia have very low Apgar scores at birth and need special treatment. 12 Neonatal asphyxia is a major cause of neonatal mortality worldwide, with an incidence of approximately 0.7 to 1.2 million annually. 13 The incidence of hypoxic-ischemic encephalopathy is 2.5 per 1000 live births, and the proportion of cerebral palsy associated with intrapartum hypoxia-ischemia is 14.5%. Multiple other organs are often involved, including renal (40%), pulmonary (25%), cardiac (30%), and/or gastrointestinal (GI; 30%), and decreases in gastrointestinal blood flow often occur. 14 , 15 A recent retrospective review of NEC revealed asphyxia to be a major predisposing factor to this disease process in both term and preterm infants. 16 Therapeutic hypothermia reduces mortality and improves survival with normal neurologic outcome and is now standard treatment. 17 A recent study revealed that celiac and mesenteric artery flow remained low during hypothermia but rose significantly after rewarming (peak systolic velocity in the celiac artery [CA]=0.63 m/s to 0.77 m/s, p =0.004, and superior mesenteric artery [SMA]=0.43 m/s to 0.55 m/s, p =0.001). 18 The authors hypothesized that the low GI perfusion during hypothermia may indicate a favorable effect of cooling against reperfusion injury of the GI tract. Enteral feedings are usually withheld during hypothermia, even for mild neonatal encephalopathy. 19
Colostrum should be expressed and often becomes the first oral feedings, drop by drop. Mothers will need help initiating lactation and understanding the pathophysiology of the infants' disease. These infants often have a poor suck that does not coordinate with the swallow, making nursing at the breast and bottle equally difficult. The mother may need to hold her breast in place and hold the infant's chin as well. These infants are especially susceptible to “nipple confusion” or “nipple preference.” That is, the infant seems to prefer feeding via a bottle versus the breast. In the case of a sick infant, this is not likely to be “confusion”; rather, the infant seems to feed “better” via a bottle per the nursing staff or family. In hopes of the infant developing the feeding skills for effectively breastfeeding, a means of sustaining nourishment other than via a bottle should be sought. Cup feeding has been well tolerated using a soft plastic 1-ounce medicine cup. Even infants who will not be breastfed but feed poorly from a bottle for neurologic reasons will do better with a cup. 20 , 21 , 22 Weaning slowly from the IV hyperalimentation fluids while introducing breastfeeding is helpful. Using a dropper and employing the nursing supplementer (feeding tube delivering supplemental feeds directly to the mother’s nipple) are options if milk supply from the breasts is low. These infants may continue to feed poorly for neurologic reasons. If the mother is taught to cope with the problem, using specific positions, holds, and supports for the infant, nursing should progress satisfactorily.
Infants can be held in positions that may help an individual baby adapt better. The “football hold” is a popular but poorly named position in which an infant is held close to the mother's body with the feet to her side. The head and face are squarely in front of the breast and steadied by the mother's arm and hand on that side. Cupping the breast and the jaw in one hand facilitates the infant's seal around the breast with the mouth ( Fig. 13.1 ). This position has been called the dancer hold . 23 One of the most valuable suggestions is the use of a sling or pleat-seat to hold an infant's body in a flexed position, thus giving the mother both hands free to hold the head and the breast in position for feeding ( Fig. 13.2 ).


Pacing the feedings and pumping after feedings will establish, maintain, or increase a mother's milk supply when the infant is unable to suck vigorously enough. Giving the pumped milk by lactation supplementer, small cup, or dropper ensures proper weight gain in the early weeks. 23 Holding an infant in a flexed position that mimics the fetal position relaxes an infant who is hypertonic or arching away from the breast.
In a study of the energetics and mechanics of nutritive sucking in preterm and term neonates, Jain et al. 24 compared 38-gestational-week infants with 35-gestational-week infants and noted that preterm infants used less energy to suck the same volume of milk. The preterm infants took up to 0.5 mL per suck but generated lower pressures and a lower suck frequency.
Exploring the hypothesis that milk flow achieved during feeding contributes to ventilatory depression during rubber-nipple feeding, Mathew 25 compared nipples with different flow rates. Decreases in minute ventilation and breathing frequency were significantly greater with high-flow nipples, thus confirming that milk flow influences breathing in premature infants who are unable to self-regulate the flow.
Tracings were made from the first oral feeding to time of discharge in term and premature infants. Serial oxygen pressure values showed small undulations across baseline (above and below) while breastfeeding. Substantial dips while bottle-feeding were shown with recovery but not above baseline. The quality and quantity of variation were different in the two modes of sucking (i.e., breast or bottle), with large drops in oxygen saturation occurring during actual sucking of the bottle but only during burping or repositioning while breastfeeding. Meier concludes that the findings do not support the widely held view that breastfeeding is more stressful. 26 , 27 The comparative data suggest that both the use of a pacifier and bottle-feeding are more stressful than suckling at the breast. For further discussion of the stress of breastfeeding versus bottle-feeding, see Chapter 14 on feeding the 28- to 32-week premature infant. If an infant has significant motor tone disabilities or lacks the usual oral reflexes in response to stimulation of the rooting and sucking reflexes, a neonatal neurologist should assess the infant before any routine exercises are initiated.
It has been suggested that perioral stimulation enhances an immature or neurologically impaired infant's ability to suck and to coordinate suck and swallow. 28 Perioral stimulation, consisting of stimulating the skin overlying the masseter and buccinator muscles by manually applying a quick-touch pressure stimulus lasting 1 second, was studied. This is accomplished by simultaneously squeezing the buccal fat of both cheeks. Suck-monitoring equipment revealed that perioral stimulation increased the sucking rate, suggesting that this may facilitate sucking. 28 Exercising the mouths of infants who already have excessive mouth stimulation may not be appropriate. Many infants in an NICU are being suctioned, tube fed, and orally stimulated for other reasons, which may lead to oral aversion.
Kangaroo care is recommended for full-term infants who are neurologically or metabolically impaired. It involves holding the infant skin to skin inside the parent's shirt. It can stabilize temperature, respirations, and heart rate and be neurologically calming. For a mother who is to breastfeed, it facilitates milk production and helps a mother learn to handle her infant. 29 Kangaroo care is further discussed in Chapter 14 .
Domperidone and metoclopramide are the most commonly used pharmaceutical galactagogues. Both are dopamine antagonists that increase prolactin secretion. A recent meta-analysis reported a significant improvement with the use of domperidone in mothers experiencing insufficient human milk production. 30 Five studies ( N =239) showed an increase in the MD of expressed human milk volume in mothers given domperidone of 94 mL/day (95% CI 71.12 to 116.83 mL]; random effect, T 2 0.00, I 2 0%). The use of domperidone in lactation has been the subject of controversy because of the increased risk of ventricular arrhythmia and sudden cardiac death of approximately 4 per 1000 person-years observed among nonlactating adults, including males and females. Numerous studies provide reassuring evidence as to the safety of domperidone use in lactating women. For example, a Canadian population-based cohort study of 320,351 women, of which 45,163 were prescribed domperidone within 6 months postpartum, revealed that no cases of ventricular arrhythmia were identified among those women with no prior history of arrhythmia. 31
The evidence for metoclopramide is less clear. Brodribb and the ABM protocol team reviewed the use galactagogues for initiating or augmenting maternal milk production in 2018. 32 Although some older trials and observational studies reported increased milk production with metoclopramide, there is concern about the potential for bias in those studies. Five randomized, placebo-controlled blinded trials from 1980 to 2001 did not demonstrate an increase in milk production or duration of breastfeeding with the use of metoclopramide in women diagnosed with poor milk production.
The ABM protocol recommended identifying and correcting any potential cause of low milk production but did not recommend the use of any specific pharmacologic galactagogue for low milk production. Despite the high-quality studies that found domperidone to be useful, they were concerned about rare but significant adverse effects. Since the publication of the ABM protocol, Thomas Hale reported an online survey of self-reported side effects of 1990 mothers, representing 25 countries, who took metoclopramide, domperidone, or both medications to enhance milk production. 33 They found that side effects affected only a small percentage of women who took either medication and that there were fewer side effects with domperidone than metoclopramide. There was no significant difference in cardiac arrhythmias between the two groups. However, there was significantly more depression and tardive dyskinesia symptoms in the metoclopramide group. Of concern, the risk of depression increased by seven times when women took metoclopramide. The authors concluded that recommendations regarding the relative safety of both metoclopramide and domperidone should be reexamined in light of these findings.
Although growth hormone has been observed to enhance milk supply, no recommended protocol exists for its clinical use. 34 In one study, 20 healthy mothers with insufficient milk who delivered between 26 and 34 weeks were given growth hormone, 0.2 international units/kg per day subcutaneously for 7 days. A group of 10 mothers received a placebo. Milk volume increased in the treated mothers. No change was noted in plasma growth hormone levels, but an increase was seen in insulin-like growth factor. No other changes were noted during this short-term therapy. 34
Other galactagogues are discussed in Chapter 11 .
The medical literature on nursing twins or triplets or multiples in general is limited. Despite this, it is well established that mothers can make enough milk for multiple infants. Many case reports support that a mother can exclusively breastfeed twins and triplets. It has been documented for centuries that an individual mother can provide adequate nourishment for more than one infant. In 17th-century France, wet nurses were allowed to nurse up to six infants at one time. Foundling homes provided wet nurses for every three to six infants.
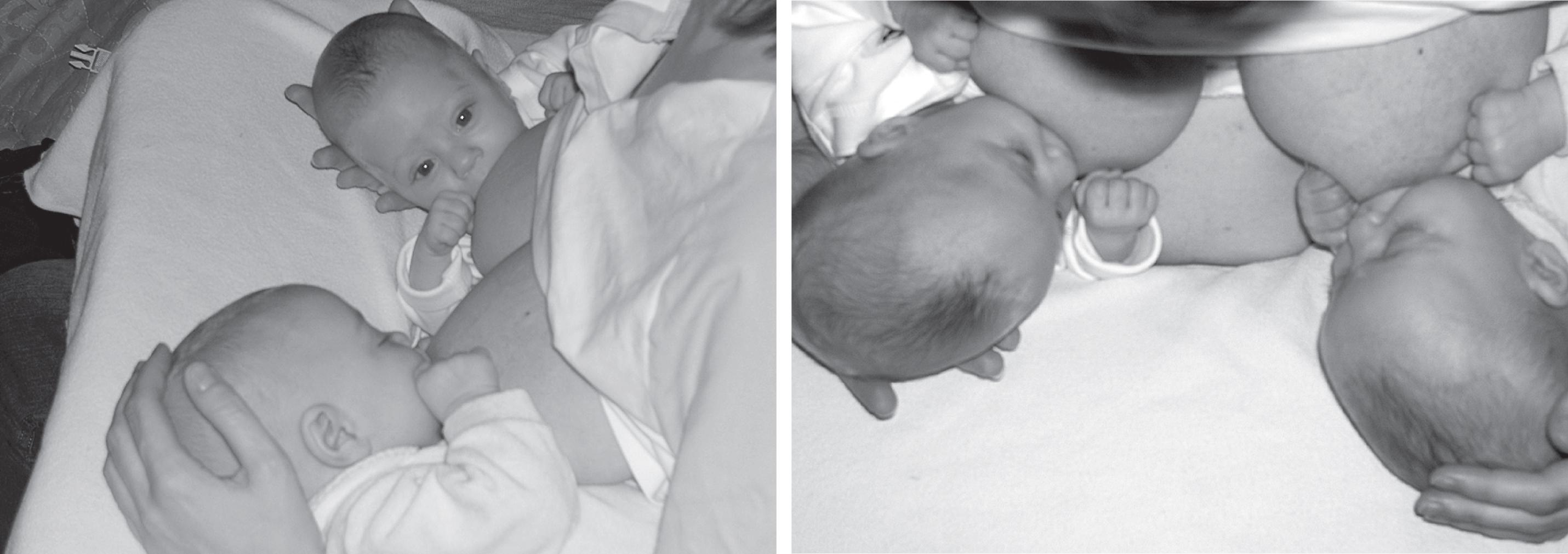
The key deterrent to nursing twins is not usually the milk supply but time. If a mother can nurse both infants simultaneously, the time factor is reduced ( Fig. 13.3 ). Many strategies have been suggested to achieve this. As the infants become larger and more active, it may be difficult to keep them simultaneously nursing with only two hands to manage infant behavior. However, twins trained from birth to nurse simultaneously will often continue to nurse in a position that allows both to nurse when they are older, even if the other is not nursing at the moment. The first year of life for a parent of a set of twins is an extremely busy one and really requires additional help, particularly if the mother is going to breastfeed. She will need time for adequate rest and nourishment. She often benefits from suggestions from other mothers of twins. The incidence of prematurity with twins is 3 in 10 pregnancies; with triplets, 9 of 10; and with singletons, just 1 in 10. Therefore the challenge of breastfeeding multiples may include some of the challenges of feeding premature infants.
The challenge of breastfeeding twins was investigated through a questionnaire of mothers who were members of the Mothers of Twins Clubs of Southern California, a national organization that offered help and advice to mothers of twins in 1975. 35 No other socioeconomic information was available. Of the respondents, 41 mothers (23.7%) breastfed from birth, although 30% of the infants were premature. Of those who did not breastfeed, 9% were told not to do so by their physician, 11% did not think it was possible, and 11% did not think they would have enough milk for two. Of multiparas who had breastfed their first child, an equal number breastfed and bottle-fed. Of the mothers who breastfed, 39 breastfed for more than 1 month, and 12 breastfed for more than 6 months.
In another study from 1986, highlighting the breastfeeding potential of multiples, eight healthy women who were breastfeeding twins and one breastfeeding triplets participated in a study by Saint et al. 36 to determine the yield and nutrient content of their milk at 2, 3, 6, 9, and 12 months postpartum. At 6 months, they fed an average 15 feeds per day. Fully breastfeeding women produced 0.84 to 2.16 kg of milk in 24 hours. Those partially breastfeeding produced 0.420 to 1.392 kg in 24 hours. The mother feeding triplets at 2½ months produced 3.08 kg/day, and the three infants were fed a total of 27 times per day. At 6 months the twins received 64% to 100% of total energy from breastfeeding, and at 12 months, they received 6% to 13%. This further demonstrates that breasts are capable of responding to nutritional demands.
Guidelines for success in breastfeeding twins recommended in 1999 by Hattori and Hattori 37 admit that many obstacles exist but suggest that health care professionals should provide extended support to mothers of multiples to promote successful breastfeeding. The initiation and duration of breast-milk feedings by mothers of multiples compared with mothers of singletons were studied by a mailed questionnaire to 555 women. 38 The 358 mothers who gave birth to twins and multiples in Ohio in 1999 and who answered the questionnaire were older, had higher incomes, were married, and were less likely to return to work by 6 months postpartum. Initiation of breastfeeding was comparable between mothers of multiples and singletons, but mothers of multiples provided milk for a shorter period of time, and mothers of preterm multiples breastfed the shortest period of time. Among mothers who initiated breast-milk feeding, the geometric mean duration of at least some breast-milk feeding was significantly shorter for preterm multiples than for all other groups: term singletons =23 weeks, preterm singletons =19 weeks, term multiples =24 weeks, and preterm multiples =12 weeks ( p =0.002). At 6 months of age, 31% of preterm singletons were breastfed compared with 16% of preterm multiples. 38 A report in the Cochrane Database in 2017 confirmed the limited published data on breastfeeding for twins and multiples. Of the 10 trials (23 reports), the quality of evidence was mixed, and the risk of bias was high. The authors concluded there was insufficient data to make any reasonable conclusions on specific breastfeeding interventions for twins or multiples. 39 A 2018 study revealed that the main reasons for weaning in the first 6 months cited by mothers of twins were insufficient human milk supply, infants’ behavior, and returning to work. 40 On the other hand, books, pamphlets, and websites supply personal stories and advice for mothers, fathers, and families. La Leche League International, Mothers of Twins, pregnancytoday.com, parentingweb.com, multiplebirthsfamilies.com, and others have copious commentaries for mothers. Coping strategies can be helpful. Wisdom from Gromada is shared with mothers in her book Mothering Multiples, Breastfeeding and Caring for Twins or More . 41 A case of a mother successfully nursing quadruplets is reported by Berlin. 42 One helpful device is frequently recommended, the “breastfeeding pillow,” which is a pillow that wraps around the mother as she sits to nurse. Two infants can be supported by the pillow.
Infants who have self-limited acute illnesses, such as fever, upper respiratory infection, colds, diarrhea, or contagious diseases such as chickenpox, do best if breastfeeding is maintained. Because of breast milk's low solute load, an infant can be kept well hydrated despite fever or other increased fluid losses. If respiratory symptoms are significant, an infant seems to nurse well at the breast and poorly with a bottle. This observation has been documented many times when nursing mothers have roomed-in with their sick infants in the hospital. The studies of Johnson and Salisbury on the synchrony of respirations in breastfeeding in contrast to the periodic breathing or gasping apnea pattern of the normal bottle-fed infant may well provide the underlying explanation for the phenomenon of an acutely ill infant continuing to nurse at the breast. 43
In addition to the appropriateness of human milk for a sick infant, nursing and closeness with the mother provide comfort. If an infant is suddenly weaned, psychologic trauma is added to the stress of the illness. 44
It may be difficult to distinguish the effect of trauma of acute weaning from the symptoms of the primary illness, such as poor feeding or lethargy, if the acutely weaned infant fails to respond to adequate treatment. In this case, returning to breastfeeding may be the treatment because the stress of acute weaning will be removed.
It is not appropriate to give a mother medicine intended to treat the infant, especially antibiotics. This has been tried to the detriment of the child because variable amounts of the drug reach the infant depending on the dose, dosage schedule, and amount of milk consumed. Maternal drugs can produce symptoms in an infant in some cases, and thus maternal history is important in assessing symptoms in a breastfed infant (see Chapter 11 ). 45
Guidelines for buccal smear collection in breastfed infants should be followed when genetic review is indicated. A buccal smear is a noninvasive, fast, and relatively inexpensive diagnostic method for collecting genetic material. It is used for sex determination as well as aneusomy, microdeletion syndromes, and a variety of polymerase chain reaction–based molecular genetic tests. Maternal cells can contaminate smears taken from breastfed infants. The recommendation is to wait at least 1 hour after a feeding. Buccal mucosa should be cleansed thoroughly with a cotton swab applicator. These procedures apply to both neonates and older nursing children. 46
Bouts of diarrhea and intestinal tract disease are less common in breastfed infants than in bottle-fed infants, but when they occur, the infant should be maintained on the breast if possible. 47 , 48 Human milk is a physiologic solution that normally causes neither dehydration nor hypernatremia. Occasionally, an infant will have diarrhea or an intestinal upset because of something in the mother's diet. It is usually self-limited, and the best treatment is to continue to nurse at the breast. If a mother has been taking a laxative that is absorbed or has been eating laxative foods, such as fruits, in excess, she should adjust her diet. Intractable diarrhea should be evaluated as it would be in any infant. Allergy to mother's milk is extremely rare and would require substantial evidence to support the diagnosis. Allergy to a foreign protein passed into the milk, such as bovine β-globulin, as in cow milk, however, can cause severe allergic symptoms in an infant (see following discussion).
Suckling milk is the defining characteristic of mammals. Lactose, the major carbohydrate in milk, is hydrolyzed by lactase-phlorizin hydrolase, an enzyme of the small intestine. Lactase plays a critical role in the nutrition of mammalian neonates. Congenital lactase deficiency, present from birth, is extremely rare and is inherited as an autosomal-recessive gene. 49 Most humans (except Northern Europeans) and other adult mammals do not drink milk beyond infancy; it causes indigestion and mild to severe GI symptoms because of an adult's inability to digest lactose. Low lactase levels result from injury or limited genetic expression of lactase. The enzyme hydrolyzes lactose, phlorizin, and glycosyl ceramides. A decline in lactase-specific activity occurs at the time of weaning in most mammalian species. In humans it may occur as early as 3 to 5 years of age; in other species, the elevated juvenile levels of lactase-specific activity persist. The developmental patterns of lactase expression are regulated at the level of gene transcription. 49
Premature infants and those recovering from severe diarrhea have transient lactose intolerance. The only treatment is a temporary lactose-free diet. Reports of lactose-hydrolyzed human milk suggest that banked human milk can be treated with lactase, which will hydrolyze the lactose (900 enzyme activity units to 200 mL breast milk degraded 82% of the lactose). 50 In one case, the reason for using human milk was that the infant became infection prone when he was weaned from the breast at the time the initial diagnosis was made. That infant showed marked improvement with lactase-treated human milk. In a breastfed infant, lactase deficiency may be manifest by chronic diarrhea and marked failure to thrive.
Cow’s milk protein allergy (CMPA) may be seen in exclusively breastfed infants. Symptoms suggestive of this disorder may be seen in up to 15% of all infants, although the actual incidence is likely closer to 2% to 7.5% in the first year of life. Breastfeeding reduces this incidence to 0.5% to 1.0%. 51 Exclusive breastfeeding may also prevent sensitization to cow’s milk protein. 52 CMPA often confused with lactase deficiency (lactose intolerance or cow’s milk intolerance) by parents, although it is etiologically distinct and lactose intolerance rarely occurs in infants. CMPA in breastfed infants is generally found to be caused by the passage of bovine β-lactoglobulin. In one study, when mothers ingested cow’s milk then breastfed, infants with diagnosed CMPA reacted, but only 63% of their mothers had detectable levels of bovine β-lactoglobulin in their milk. 53 The authors concluded that other proteins may also be responsible for symptoms.
CMPA is currently thought to have two etiologic frameworks: one is immunoglobulin E (IgE) mediated, and the other is non-IgE mediated. IgE-mediated reactions tend to occur within a few hours of ingestion as a type 1 hypersensitivity reaction and include respiratory (wheezing, stridor), dermatologic (hives, atopic dermatitis), allergic (running eyes or nose), and GI symptoms (vomiting and diarrhea). This diagnosis can be made by history, specific IgE blood levels, or skin-prick testing. If the history is clear or symptoms are severe, an oral challenge should be avoided because of the risk. 54
Non-IgE related reactions are type 4 mediated and generally include reflux, malabsorption, atopic dermatitis, and allergic proctocolitis. This latter results in the characteristic microscopic hematochezia. Symptoms generally present in the first few months of life. 51 Because of the etiology, allergy testing is likely to be inconclusive. Rather, diagnosis is made based on history and elimination diets. A controlled oral food challenge (OFC) with direct medical supervision can help in some situations to confirm or exclude the diagnosis of CMPA.
For exclusively breastfed infants with clinical evidence of allergic colitis, mothers should eliminate all forms of cow’s milk protein, including milk products, casein, and whey. The difficulty for mothers in maintaining this diet financially, nutritionally, and psychosocially must be weighed against the potential benefits. 55 Elimination diets with appropriate supplementation of missing nutrients have not been shown to negatively affect infant growth. 56 The ABM has outlined a clinical protocol for a maternal elimination diet in the case of allergic proctocolitis in the exclusively breastfed infant. 57 For supplemented infants, extensively hydrolyzed formula (eHF) or amino acid–based formulas (AAFs) may be used. Some debate exists over whether soy formula should be attempted first, because of its lower cost, increased infant enjoyment, and larger evidence base for growth. However, infants may have cross-reactivity with soy products. Goat, sheep, and other mammal’s milk also cross-reacts with CMPA. Studies have shown no increased risk of poor growth from hydrolyzed formulas, and they may result in more rapid resolution of symptoms, particularly if these symptoms are severe. 58 Although allergens likely clear from breast milk within 2 to 7 days, it may take 2 to 4 weeks for inflammation to subside and symptoms to fully resolve. 59 If there is no improvement in symptoms, mothers may consider eliminating other allergens (soy, egg, wheat), seek testing if testing has not yet been done, and reintroduce milk products. An AAF may also be attempted. Very rarely for extremely sick infants, it may be necessary to pause breastfeeding while attempting an AFF, encouraging the mother to pump and store her milk to maintain her supply.
If infants improve with an elimination diet, reintroduction of cow’s milk products may be attempted in maternal diets around 9 to 12 months of age, then again periodically if this fails. Most children have outgrown CMPA by school age. If the reaction is IgE mediated or severe, reintroduction should take place under the care of an allergist, or, when unavailable, at the physician’s office.
There have been anecdotal reports that severe cases of allergic colitis and also severe GI colic can be alleviated by treating the mother with pancreatic enzymes. These reports noted it was safe for the mother and often showed dramatic improvement for the infant. This treatment is appropriate when eliminating cow protein has not solved the problem.
A formal study of this therapy was reported by Repucci, who described four term infants who were exclusively breastfeeding between 1 and 3 months of age who had a positive family history for atopy. 60 Elimination of bovine protein had not relieved the blood in the stools. Mothers were prescribed pancreatic enzymes (Pancrease MT4 USP units: 4000 units of lipase, 12,000 of amylase, and 12,000 units of protease per capsule), two capsules with each meal and one capsule for snacks. Blood cleared within 2 days. One mother had to increase the dose to three capsules per meal and two with snacks. Mothers experienced no side effects from this therapy.
In severe cases of CMPA, food protein–induced enterocolitis syndrome (FPIES) should be ruled out. 61 This disorder presents somewhat later, between 2 and 7 months of age, and is generally triggered by milk, soy, or grain intolerance. 62 It is characterized by recurrent vomiting, diarrhea, and episodes of pallor and lethargy after ingestion. Acute FPIES may present with hypovolemic shock, hypotension, and hypothermia, whereas chronic FPIES symptoms may be intermittent and cause failure to thrive. Diagnostic criteria are based on history and the outcome of an elimination diet or OFC. Exclusively breastfeeding mothers need extensive dietary counseling for food elimination and milk supply because weaning to solid foods can be very difficult, and even AAFs may not be tolerated by their infants. Time to resolution varies significantly. Close physician counseling and follow-up are recommended. The pathophysiology of FPIES continues to be elusive, with evidence for the stimulation of different components of the immune system. Management involves the treatment of symptoms after an exposure, elimination of suspected food triggers, and ongoing assessment and evaluation using OFCs to identify the resolution of the problem. 61
Chronic, protracted diarrhea (or enteropathy) includes a variety of abnormalities of the small intestinal mucosa. GI infections are the most common cause of enteropathy. They alter mucosal permeability, antigen penetration in the mucosa, local inflammation, and T-cell activation. Coexisting malnutrition exacerbates the local immune response, alters repair of damaged mucosa, and limits systemic nutritional recovery. Celiac disease and CMPA are other causes of chronic diarrhea. Human milk banks have reported the use of donor human milk in the management of protracted diarrhea. Eleven of 24 children managed by MacFarlane and Miller in a hyperalimentation referral unit recovered when fed banked human milk orally without protracted IV therapy. 63 All the infants had been tried on the available special formulas first. A study of oral rehydration in 26 children younger than the age of 2 years showed that the children who continued to breastfeed while receiving rehydration fluid had fewer stools and recovered more rapidly than those receiving only rehydration fluid. 64 The Pima Infant Feeding Study clearly showed that in less developed and more disadvantaged communities in the United States, exclusive breastfeeding protected against severe diarrhea and other GI disorders. 65
Some chronic diseases are better controlled by keeping an infant on breast milk because symptoms usually become more severe with weaning. If an infant is weaned and does poorly on formula, relactation of the mother should be considered. With the availability of the nursing supplementer, this possibility is no longer remote (see Chapter 19 ).
Celiac disease or permanent gluten-sensitive enteropathy is an immunologic disease dependent on the exposure to wheat gluten or related proteins in rye and barley. 66
A case-control study was done on the effect of infant feeding on the development of celiac disease to investigate the association between duration of breastfeeding and age at first gluten introduction into the infant diet and the incidence and age of onset of celiac disease. 67 A significant protective effect on the incidence of celiac disease was related to the duration of breastfeeding after 2 months. It was not related to the age of first gluten in the diet, although the age of first exposure did affect the age of onset of symptoms. 67 The risk for celiac disease was reduced in children younger than 2 years old in a study of 2000 Swedish children if they were still being breastfed when dietary gluten was introduced. The effect was more pronounced if breastfeeding continued after gluten was introduced. The authors conclude that gradual introduction of gluten-containing foods into the diet while breastfeeding reduces the risk for ever getting celiac disease. 66 The declining incidence of celiac disease and transient gluten intolerance has been associated with changing feeding practices, which include later introduction of dietary gluten, the use of gluten-free foods for weaning (rice), and the increased initiation and duration of breastfeeding. 68 The recent US Department of Agriculture (USDA) and US Department of Health and Human Services Pregnancy and Birth to 24 Months Project reviewed nine articles published from January 1980 to March 2016. They concluded, based on limited case-control evidence, that never versus ever being fed human milk is associated with a higher risk of celiac disease. However, concerns about reverse causality precluded a conclusion about the relationship of shorter versus longer duration of any human milk feeding with celiac disease. 69
A window of opportunity has been suggested to reduce the risk of celiac disease by introducing gluten at specific ages. Two large studies dealt with that hypothesis. The first study, conducted at 20 centers throughout Italy, compared a delayed strategy of the introduction of gluten at 12 months of age to the standard strategy of 6 months of age. 70 The 553 children in this trial were at increased risk for developing celiac disease, with a compatible human leukocyte antigen (HLA) haplotype and a first-degree relative with celiac disease. The cumulative prevalence of celiac disease at age 10 years was 16.8%. This study revealed that although the later introduction of gluten delayed the onset of celiac disease in early childhood, there was no difference between the two groups by the age of 5 or 10 years, suggesting that the age of introduction of gluten had very little impact on the ultimate risk for celiac disease later in childhood.
The second study was a double-blind trial conducted in eight countries on 944 infants with an at-risk HLA haplotype and a first-degree relative with celiac disease who were randomly assigned either 200 mg of vital wheat gluten or placebo at 4 months of age, and then dietary gluten was introduced to both groups at age 6 months. 71 At 5 years, the cumulative prevalence of celiac disease was 12.1%, and there was no significant difference in the risk of celiac disease when comparing the intervention to the placebo group.
In children at high risk for celiac disease, neither delaying the timing of the introduction of gluten to 12 months or introducing gluten between 4 and 6 months decreased the overall risk of celiac disease, although it may change the timing of onset of the disease. 70 , 72
Crohn disease and ulcerative colitis constitute the two major groups of inflammatory bowel disease. Environmental factors, genetic factors, and immune responses are important in the etiology of inflammatory bowel diseases, with resultant excessive and destructive inflammatory reactions of the gut wall. In addition, it is thought that downregulation of the immune responses may allow the damaged mucosa to heal and reset the physiologic functions of the gut back to normal. Because it has been suggested that breast milk is essential for the development of the normal immunologic competence of the intestinal mucosa, investigators have studied the association between breastfeeding and later Crohn disease.
A recent meta-analysis and systemic review have evaluated the risk of inflammatory bowel disease and breastfeeding. A meta-analysis evaluated 35 studies that ran through November 2016 comprising 7536 individuals with Crohn disease, 7353 with ulcerative colitis, and 330,222 controls. They reported that ever breastfeeding was associated with a 29% reduced risk of Crohn disease (odds ratio [OR] 0.71, 95% CI 0.59 to 0.85) and a 22% reduced risk of ulcerative disease (OR 0.78, 95% CI 0.67 to 0.91). 73 Although this inverse association was observed in all ethnicity groups, the magnitude of protection was significantly greater among Asians (OR 0.31, 95% CI 0.20 to 0.48) compared with Caucasians (OR 0.78, 95% CI 0.66 to 0.93; p =.0001) in Crohn disease. Breastfeeding duration showed a dose-dependent association, with the strongest decrease in risk when breastfed for at least 12 months for Crohn disease (OR 0.20, 95% CI 0.08 to 0.50) and ulcerative colitis (OR 0.21, 95% CI 0.10 to 0.43) as compared with 3 or 6 months. 73
The recent USDA systemic review evaluated 17 articles published from January 1980 to March 2016. It concluded, based on limited but consistent case-control evidence, that longer durations of breastfeeding were associated with lower rates of inflammatory bowel disease. 69
Infants who develop respiratory illnesses should be maintained at the breast as tolerated. The added advantages of antibodies and other antiinfective properties in human milk are valuable to infants over and above the importance of nutritional support during infection. 74 , 75 The comfort of having the mother nearby is important whenever the infant has a crisis; weaning during illness may be difficult for both the infant and mother.
Wheezing and lower respiratory tract disease and other respiratory illnesses are lower in frequency and duration when the infant is breastfed. The risk of hospitalization for respiratory disease in infants is decreased for breastfed infants. 75 Recovery is accelerated if breastfeeding is maintained. The Millennium Cohort Study, a nationally representative longitudinal study of 18,818 infants in the United Kingdom, revealed that exclusive breastfeeding for 6 months was associated with a decreased risk of lower respiratory tract infections compared with infants who exclusively breastfed for <4 months, stressing the importance of recommending 6 months exclusive breastfeeding. 48 The Environmental Determinants of Diabetes in the Young (TEDDY), a prospective longitudinal study from six centers in the United States and Europe, followed 6861 children between the ages of 3 and 18 months and 5666 children up to the age of 4 years. Breastfeeding was found to be inversely associated with the odds of respiratory infections with fever at 3 to 6 months (any breastfeeding: OR 0.82, 95% CI 0.70 to 0.95, exclusive breastfeeding: OR 0.72, 95% CI 0.60 to 0.8) and with laryngitis and tracheitis at 6 to 18 months (OR 0.79, 95% CI 0.63 to 0.97, p = 0.03). 76 The Agency for Health Care Research and Quality (AHRQ) reported a 72% reduction in the risk of hospitalization for respiratory infections in children under a year of age who were exclusively breastfed for at least 4 months. 77
A meta-analysis of 20 studies on lower respiratory tract infection from respiratory syncytial virus (RSV) revealed that not breastfeeding doubled the incidence (OR 2.24, 95% CI 1.56 to 3.20). 78 It has been estimated that if 90% of US infants were exclusively breastfed for 6 months, this could prevent almost 21,000 hospitalizations and 40 deaths for lower respiratory tract infections in the first year of life. 79 The American Academy of Pediatrics (AAP) Committee on Nutrition and Section of Allergy and Immunology recently concluded that any duration of breastfeeding ≥3 to 4 months is protective against wheezing in the first 2 years of life and that longer breastfeeding, as opposed to less breastfeeding, protects against asthma even after 5 years of age. 80 In addition, the USDA Pregnancy and Birth to 24 Months Project recent systematic review concluded, based on moderate, mostly observational evidence, that any breastfeeding is associated with a lower risk of childhood asthma and that longer durations provide more protection. 81
Young infants who have older siblings may well be exposed to some virulent viruses and bacteria. Developing croup, for instance, may make an infant seriously ill. Hydration can be maintained by frequent, short breastfeeding periods. Studies have shown that respirations are maintained more easily when feeding on human milk than on cow’s milk, even from a bottle. Nursing at the breast permits regular respirations, whereas bottle-feeding is associated with a more gasping pattern. 82 Thus breastfed infants should continue to nurse when they are ill. If an infant is hospitalized, every effort should be made to maintain breastfeeding or to provide expressed breast milk if the infant can be fed at all. Staff should provide rooming-in for the mother if a care-by-parent ward is not available.
Colostrum and milk contain large amounts of immunoglobulin A (IgA) antibody, some of which is RSV specific. Breastfed but not bottle-fed infants have IgA in their nasal secretions. Neutralizing inhibitors to RSV have been demonstrated in the whey of most samples of human milk tested. 83 IgG anti-RSV antibodies are present in milk and in reactive T lymphocytes. Breastfeeding-induced resistance to RSV was associated with the presence of interferon and virus-specific lymphocyte transformation activity, suggesting that breastfeeding has unique mechanisms for modulating the immune response of infants to RSV infection. 84 Clinical studies indicating a relative protection from RSV in breastfed infants were clouded by other factors. 85 The populations were unequal because of socioeconomic factors and smoking (i.e., bottle-feeding mothers were in lower socioeconomic groups and smoked more). In general, if breastfed infants become ill, they have less severe illness. 83 , 85 Although breastfeeding protects, parental smoking and daycare are important negative factors in the incidence of respiratory infection. Respiratory illness in either infant or mother should be treated symptomatically, and breastfeeding should be continued. If the infant has nasal congestion, nasal aspiration and saline nose drops just before a feed are helpful.
Acute otitis media is a common affliction among young children, with estimates as high as 60% of children experiencing at least 1 episode of acute otitis media (AOM) before 1 year of age and more than 80% by 3 years of age. 86 Beyond the acute illness, AOM can lead to a variety of sequelae, including persistent middle ear effusion, short-term hearing loss, perforation of the eardrum, chronic suppurative otitis media, persistent hearing impairment, and less commonly, mastoiditis, brain abscess, and meningitis. 87 The global incidence of AOM has been estimated at 11% per year, with a peak incidence in the 1- to 4-year age group. 88 There is wide variation in incidence by region and by country. The World Health Organization (WHO) has published data on the occurrence of AOM by region, with sub-Saharan Africa being the highest, followed by southern Asia, South East Asia and the Pacific Islands, and Central America and the Caribbean. 88 Numerous risk factors have been associated with the risk of AOM, including allergy/atopy, upper respiratory tract infection (URTI), snoring, gender (male), attending daycare, multiple children in a household, family history of AOM, patient’s previous history of AOM, passive smoking, socioeconomic status, pacifier (or dummy) use, exposure to air pollutants, immunizations (influenza, Haemophilus influenzae B, pneumococcal vaccines), obesity, and breastfeeding. 89 , 90 In different populations and studies, each of these risk factors appeared to be a contributor to the occurrence of otitis media. There is mixed data concerning the contribution or relative effect of these different risk factors, except for passive smoking and breastfeeding.
Otitis media in infants occurs less frequently in breastfed infants because of the infection protection properties of human milk and the protective effect of suckling at the breast. In a prospective birth cohort study, the West Australian Pregnancy Cohort (Raine) Study recruited 2900 mothers through antenatal clinics at the major tertiary obstetric hospital in Perth, Western Australia. A total of 2237 children participated in a 6-year cohort follow-up, and a subset of 1344 children were given ear and hearing assessments. There was a significant, independent association between predominant breastfeeding (OR 1.33, 95% CI 1.04 to 1.69, p =0.02) and otitis media, and breastfeeding duration (OR 1.35, 95% CI 1.08 to 1.68, p =0.01) with otitis media at 3 years of age. 91 The TEDDY Study described earlier reported that breastfeeding was inversely associated with the odds of otitis media at 3 to 6 months (any breastfeeding: OR 0.76, 95% CI 0.62 to 0.94, exclusive breastfeeding: OR 0.64, 95% CI 0.49 to 0.84) and at 6 to 18 months (OR 0.89, 95% CI 0.82 to 0.97, p =0.008). The duration of exclusive breastfeeding was inversely associated with the odds of otitis media up to 48 months of age (OR 0.97, 95% CI 0.95 to 0.99), long after breastfeeding had stopped. 76
The AHRQ reported that exclusive breastfeeding for 3 to 6 months provided a 50% reduction in otitis media compared with formula-feeding even when controlling for socioeconomic status, parental smoking, and the presence of siblings. 77 A meta-analysis of 24 studies, all from the United States or Europe, revealed that breastfeeding protects against otitis media in the first 2 years of life. 86 Exclusive breastfeeding for the first 6 months was associated with the greatest protection, a 43% reduction in ever having AOM in the first 2 years of life (OR 0.57, 95% CI 0.44 to 0.75), followed by “more versus less” breastfeeding (OR 0.67, 95% CI 0.59 0.76) and “ever versus never” breastfeeding (OR 0.67, 95% CI 0.56 to 0.80), again stressing the importance of recommending 6 months exclusive breastfeeding. The researchers did not report on data showing that breastfeeding offers any protection against AOM beyond 2 years of age. 86 The Italian Society of Pediatrics presents updated guidelines for the management of AOM in children. 90 In those guidelines, the review of the type of feeding as a preventive measure against AOM concludes that breastfeeding is clearly protective. The guidelines state that the heterogeneity of the numerous studies in the review prevents exact statements regarding exclusivity and duration of breastfeeding for protection against AOM. There is biologic plausibility for the protective effect of breastfeeding against AOM based on the multiple immunologic factors in breast milk that can affect mucosal barrier protection, colonization with nonpathogens, and local and systemic immune protection. There is a large amount of clinical and research data demonstrating the protective effect of breastfeeding against AOM. The most benefit from breastfeeding is gained with exclusive breastfeeding and longer duration (at least 6 months in the case of AOM). Discussing and addressing other potential risk factors for AOM is appropriate if there is parental concern or a family history of frequent otitis media.
Galactosemia, caused by a deficiency of galactose-1-phosphate uridylyltransferase (GALT), is a rare circumstance in which an infant is unable to metabolize galactose and must be placed on a galactose-free diet. The disease can be rapidly fatal in the severe form. The infant may have severe and persistent jaundice, vomiting, diarrhea, electrolyte imbalances, cerebral signs, and weight loss. This is a medical emergency. This does necessitate weaning from the breast to a special formula because human milk, as with all mammalian milks, contains high levels of lactose, which is a disaccharide that splits into glucose and galactose. Until the subtype is discovered, the mother may be encouraged to continue to pump and store milk in case the infant may be partially breastfed. The condition is suspected when reducing substances are found in the urine in the newborn, and the diagnosis is confirmed by measuring the enzyme uridylyltransferase in the red and white blood cells. The several forms can be distinguished by genetic testing. Except for the mild form, the infant must be weaned to a lactose-free diet. An infection with Escherichia coli in the newborn period may be the trigger that precipitates serious symptoms associated with this or other metabolic disorders. Galactosemia is screened for in most states in the United States, along with phenylketonuria (PKU) and other metabolic disorders.
When the diagnosis is made, genetic testing should be done. In the more common and milder form of the disease, the Duarte variant (DG), some enzyme is available. A recent study demonstrated that DG, diagnosed on newborn metabolic tests, is not associated with an increased risk of developmental abnormalities and does not benefit from dietary restrictions of galactose. In one study, 350 children between the ages of 6 and 12 in 13 US states were studied, including 206 who had DG and 144 unaffected siblings who served as controls. 92 The children were found to be at no greater risk of long-term developmental abnormalities than their unaffected siblings, regardless of their exposure to milk as infants. Breastfeeding, therefore, should be encouraged with DG.
Although newborns are screened for galactosemia in all 50 US states, screening protocols vary from state to state; some only test for the extreme deficiencies of classic galactosemia, whereas others are designed to detect DG as well. Newborn screening tests for galactosemia look at blood levels of GALT, which helps convert galactose into glucose. Children with GALT enzyme levels of 1% or less are considered to have classic galactosemia, which affects about one out of every 50,000 babies born in the United States. Most babies with DG, which is 10 times more common, have about 25% of the normal level of GALT activity. 93 At present, in most places, the diagnostic evaluation of an abnormal newborn screen for galactosemia can take more than a week for results. The risk of sepsis, hepatic injury, kernicterus, and even death in infants with classic galactosemia leads most providers to respond to an abnormal newborn screening (NBS) result by stopping breastfeeding to use a galactose-free formula. The solution may be to change the NBS by adjusting the cutoff values such that the identification of DG and other benign variants of galactosemia is kept to a minimum. Other solutions would be to change the NBS by adding a screen for the Duarte allele and/or including the several most common classic galactosemia mutations to reduce the number of infants unnecessarily treated. Although the presence of the Duarte allele does not completely eliminate the risk of severe mutations, it would provide reassurance, allowing health care providers to better assess the need to stop breastfeeding without excessive risk to the infant. 94
With other forms of galactosemia, such as galactokinase (GALK) deficiency or galactose epimerase (GALE) deficiency, the standard treatment is to wean to a lactose-free diet to eliminate complications. Some infants can only be partially breastfed, with some lactose-free formula in addition for necessary calories. 95 A recent review included two infants with GALE who were exclusively breastfed for a mean of 2.5 months. At 7 years of age, their neurologic development was normal, and body length was above the 3rd percentile. 96 An endocrinologist should make the decision for the exact balance of milks. In classic GALT deficiency, breastfeeding is contraindicated.
Other metabolic deficiency syndromes may be apparent only as mild failure-to-thrive syndrome until the infant is weaned from the breast and the symptoms become severe. This particularly applies to inborn errors of metabolism caused by an inability to handle one or more of the essential amino acids that are in higher concentration in cow’s milk than human milk. Infection is often a complication early in the lives of these infants with inborn errors, most commonly as a result of E. coli bacteria. While the acute infection is being treated, the infant may be weaned from the breast, and the metabolic disorder would then become apparent precipitously.
Certain amino acids, including phenylalanine, methionine, leucine, isoleucine, and others associated with metabolic disorders, have significantly lower levels in human milk than in cow’s milk. Management of an amino acid metabolic disorder while breastfeeding depends on careful monitoring of blood and urine levels of the specific amino acids involved. Because these are essential amino acids, a certain amount is necessary in the diet of all infants, including those with disease. An appropriate combination of breastfeeding and milk free of the offending amino acid should be developed. The care of such infants should be provided in consultation with a pediatric endocrinologist.
Screening programs that test all newborns have identified many victims early. Almost all NBS programs test for PKU, galactosemia, and hypothyroidism, and increasingly, maple syrup urine disease, homocystinuria, biotinidase deficiency, tyrosinemia, and now cystic fibrosis are included. Most cases can be managed with continued breastfeeding and diet modification. Congenital adrenal hyperplasia requires corticosteroids, but the feeding can be breast milk. If it is the salt-wasting variety, an infant must have added salt.
The most common of the amino acid metabolic disorders is PKU, in which the amino acid phenylalanine (Phe) accumulates as a result of mutations in the liver enzyme phenylalanine hydroxylase. The dietary treatment of PKU is based on the restriction of Phe intake to maintain blood Phe concentrations within the recommended range. Unless the affected child is maintained on a strict low-Phe diet, PKU leads to mental retardation, seizures, behavioral problems, and other neurologic symptoms. In contrast, when identified via newborn screening and if treatment is initiated before 1 month of age, cognitive–neurologic development is preserved. 97 The treatment of PKU involves a lifelong diet low in Phe; frequent monitoring of blood Phe values; and regular consultation with the pediatric metabolic team of physicians, nurses, and dieticians. Normal cognitive development is expected when Phe blood levels are managed and remain within acceptable levels (120 to 360 μmol/L). 98
Unfortunately, exclusive breastfeeding for the first 6 months of life affects the neurologic development of patients with PKU. Although human milk has less phenylalanine than formula, it still exceeds the tolerance of most infants with PKU. Because breast milk and regular infant formula contain Phe, babies with PKU need to consume a phenylalanine-free infant formula. The standard of care for infants with PKU was immediate discontinuation of breastfeeding with the combination of a standard infant formula and a phenylalanine-free formula. At the time, this was believed to be the only effective way to monitor the infant's intake and allow for precise titration and measurement of Phe to protect the neurologic and cognitive development of the infant. Mothers of infants with PKU titrated Phe-free formula with a standard commercial formula based on Phe levels obtained from infant heel sticks. Breastfeeding is sometimes continued until the diagnosis is confirmed and Phe-free formula is begun. There are reports concerning breastfeeding and PKU that discuss the challenges of doing this and the difficulty of monitoring Phe levels and titrating the amount of Phe-free formula. 99 , 100
As soon as the diagnosis is made, an infant should be placed on a low-Phe formula to reduce the levels in the plasma promptly. The mother should pump her breasts to maintain her milk supply. The breastfed infant is offered a small volume of special formula (10 to 30 mL) first and then completes the feeding at the breast. As long as the blood Phe levels can be maintained between 120 and 360 mmol/L, the exact intake need not be measured. Initially, weight checks to ensure adequate growth are essential because poor intake leading to a catabolic state will interfere with control. Because human milk is low in Phe, the offending amino acid, more than half of the diet can be breast milk.
Another protocol for breastfeeding an infant with PKU was studied by van Rijn et al. 101 The feeding schedule was based on alternating breastfeeding and phenylalanine-free formula by bottle. Each child had a separate schedule convenient for the mother–baby dyad, depending on tolerance and age. At the beginning of treatment, the mother breastfed once daily, allowing the infant to feed until satiated, and the mother pumped the rest of the day. Breastfeedings were increased while monitoring phenylalanine plasma levels. Ultimately, breastfeeding and bottle-feeding were alternated and equal. At all feedings, the infant drank until satisfied. The breastfed infants did well on this protocol, and plasma levels were stable. The mean Phe concentration was 170 μmol/L (range 137 to 243 μmol/L) for the breastfed infants and 181 μmol/L (range 114 to 257 μmol/L) for the formula-fed infants; all of the values in each group of infants were within the recommended range. An essential member of the management team is a board-certified licensed lactation consultant to assist the mother in managing her milk supply. It is not known if the type of feeding strategy will affect the duration of breastfeeding in PKU.
A 2018 recent study reviewed 41 infants with PKU, 40 (98%) of whom were breastfed following delivery. 102 After the diagnosis, breastfeeding was continued in 25 (61%) infants. The mean duration of breastfeeding was 7.4±4.0 (1 to 15) months. The serum Phe concentration of breastfed infants (280±163 μmol/L) was significantly lower than that of nonbreastfed infants (490±199 μmol/L, p < 0.001), most likely reflecting the lower level of Phe in human milk compared with regular infant formula. Mean monthly weight gain in the first year of life was significantly higher in breastfed patients (493±159 g/month) compared with nonbreastfed patients (399±116 g/month, p =0.046).
Another recent study reviewed early feeding practices in infants with PKU across Europe. 103 Only 42% of centers were likely to have 76% or more of their infants on breastfeeds at the time of diagnosis, and only 26% of centers maintained 76% or more of their infants on breastfeeds after diagnosis. Overall, breastfeeding duration was short, with a mean of 4 weeks in 9%, 5 to 17 weeks in 26%, 18 to 26 weeks in 34%, 27 to 52 weeks in 24%, and >1 year in 6% of centers. For breastfeeding infants, 53% of centers gave premeasured Phe-free infant formula before each breastfeed to satiety, 23% alternated breastfeeds with Phe-free infant formula, 11% gave a premeasured Phe-free infant formula before time-limited breastfeeds, and 6% gave expressed breast-milk feeds followed by Phe-free formula. The authors concluded that controlled prospective studies are needed to assess how different feeding practices influence breastfeeding outcomes to define the optimal infant feeding practices in PKU.
The weaning of this special infant should be similar to that of other infants. Adding solid foods can be initiated at 6 months. 104 The liquid part of the diet continues as before, that is, two feeding components of low-Phe formula and breastfeeding plus solids with little or no Phe (fruits, vegetables, low-protein foods). Rice and wheat contain too much Phe. When the decision is made to wean from the breast, solid foods can be used to replace the Phe in the breast milk as needed. Growth should be followed closely. When weaning is complete, the infant should be given other, less bulky sources of protein free of Phe. This stage will be carefully orchestrated by the endocrinologist and nutritionist. There is one case-control study examining feeding development and progress onto solid foods during weaning for 20 PKU-positive infants and 20 non-PKU infants. 105 The infants were monitored monthly until 12 months and then again at 15 and 18 months of age. Children with PKU had comparable weaning progression to non-PKU infants, including texture acceptance, infant formula volume, and self-feeding skills. The children with PKU had a longer period of Phe-free infant formula bottle-feeding and parental spoon-feeding than controls. The children with PKU also had fewer meals/snacks per day; more flatulence ( p =0.0005), burping ( p =0.001), and retching ( p =0.03); and less regurgitation ( p =0.003). There were negative behaviors associated with Phe-free infant protein-substitute (PS) at ages 10 to 18 months, which overlapped the age of teething. The use of semisolid PS in PKU supported normal weaning development/progression. The authors observed that the parents required additional support to manage the complexity of feeding and to normalize the social interactions in the child's family food environment. 105
Because infants with PKU are more prone to thrush infection, the mother should be alerted to watch for symptoms in the infant and the onset of sore nipples that could be caused by Candida albicans . Treatment is nystatin for both the mother and baby initially. (See discussion in Chapter 15, Chapter 16 .)
The other benefits of human milk make the effort to breastfeed valuable for the infant and for the mother, who usually wants to continue to contribute to her infant's nurturing and nourishment. The prognosis for intellectual development is excellent if treatment of PKU is initiated early and the blood levels are maintained at less than 10 mg/dL phenylalanine (120 to 360 mmol/L).
A retrospective study of 26 school-age children who had been breastfed or formula-fed for 20 to 40 days before dietary intervention was conducted by Riva et al. 106 The children who had been breastfed had a 14-point IQ advantage, which persisted at 12.9 points when corrected for maternal social and educational status. The age of treatment onset for PKU was not related to IQ scores. This study strongly supports the belief that breastfeeding in the prediagnostic stage has a positive impact on the long-range neurodevelopmental performance of patients with PKU ( Fig. 13.4 ).

Phe levels in human milk are relatively constant regardless of the mother’s diet. Dietary precautions for the mother of a breastfeeding child with PKU are to avoid the artificial sweetener aspartame (NutraSweet), which metabolizes to aspartate and Phe.
Pompe disease (acid maltase deficiency or glycogen storage disease type II) is an inborn error of metabolism caused by a complete or partial deficiency of the enzyme acid α-glucosidase that normally breaks down lysosomal glycogen into glucose. Glycogen accumulates in the tissues, especially muscles. The disease takes various forms. The most severe form, classic infantile-onset Pompe disease (IOPD), typically features dramatic hypertrophic cardiomyopathy at birth, whereas atypical (nonclassical) IOPD can present cardiomyopathy several months later. High-dose (40 mg/kg) enzyme-replacement therapy with recombinant human alglucosidase alpha (GAA; Myozyme) started immediately at newborn screening gives the best outcome. 107 It is safe and reverses cardiomyopathy; improves gross motor outcomes, lingual strength, pulmonary function measures, and biochemical markers; and improves overall survival. 108 Because of the frequency of respiratory infection and difficulty feeding, breastfeeding should be encouraged.
Ornithine transcarbamylase deficiency is a rare, life-threatening genetic disorder. It is one of six urea-cycle disorders named for the specific enzyme deficiency present. Ornithine transcarbamylase deficiency (OTC) is the most common of the urea-cycle disorders. Urea-cycle disorders occur in 1 of 8200 US live births, making these disorders more common in the United States than globally. OTC deficiency occurs more commonly in neonates and early childhood than in adulthood. Males more commonly experience severe symptoms as neonates because the mutation is on the X chromosome. Approximately 10% of female carriers become symptomatic. 109 A lack of enzyme results in excessive and symptomatic accumulation of ammonia in the blood (hyperammonemia). Symptoms vary but can occur within 72 hours of birth and include poor suck, irritability, vomiting, and progressive lethargy followed, if untreated, by hypotonia, seizures, respiratory distress, and coma. Infant-onset disease is more common in males. Treatment includes hydration, arginine, and hemodialysis. Arginine supplementation bypasses the OTC enzyme in the urea cycle, allowing for urea creation and ammonia elimination. Using a combination of sodium benzoate and sodium phenylbutyrate reduces ammonia by using alternative pathways for nitrogen elimination. If ammonia rises above 500 μm/L, the patient should receive urgent hemodialysis. Ammonia levels above 800 μm/L are associated with severe neuralgic damage, limiting treatment options. Once OTC deficiency is suspected, genetic counseling can be helpful for patients and their families. To prevent their condition from deteriorating, patients should limit their protein intake. OTC causes high mortality and morbidity. Fifty percent of infants perish. Even if infants survive a hyperammonemic coma, they will probably face intellectual disabilities if they were in the coma for over 24 hours. 109 Patients diagnosed early and treated emergently have an improved prognosis, as do patients who adhere to low-protein diets and take medications that bypass the OTC enzyme in the urea cycle. Infants can be breastfed and receive nonprotein caloric supplement. The advantage of human milk is not only dietary but the infection protection and immune-protective qualities. A recent review found that these infants breastfed well. 96 Clinical and biochemical monitoring was performed in at 2- to 4-week intervals, including ammonia and analysis of plasma amino acids. Feeding breast milk was generally uncomplicated in all the patients, without any case of metabolic crisis. An essential amino acid formula is available for those not breastfeeding.
Transient neonatal tyrosinemia , which has been reported to occur in a high percentage (up to 80%) of neonates fed cow’s milk, is associated with blood tyrosine levels 10 times those of adults. Wong et al. 110 have associated severe cases with learning disabilities in later years. Tyrosine appears in human milk at low levels. Tyrosinemia type I is an inherited autosomal-recessive trait. Symptoms are caused by the accumulation of tyrosine and its metabolites in the liver. It is treated by dietary control consisting of low protein with limited Phe and tyrosine. Some breastfeeding is possible, combined with protein-free supplements. 2-(2-Nitro-4-trifluoromethylbenzyl)-1-3-cyclohexanedione reduces the production of toxic metabolites. Liver failure is common. Dietary restrictions are lifelong.
Nutrition management of infants with organic acidemias involves limiting the intake of the offending amino acid(s) to the minimum necessary for normal growth and development and suppressing amino acid degradation during catabolic periods by providing alternative fuels, such as glucose. In some disorders, including isovaleric acidemia, specific treatment is included to increase the excretion of toxic metabolites by enhancing the body's capacity to make isovalerylglycine, an acylcarnitine translocase. As more specific amino acid-free formulas are made available, a recipe for combining breastfeeding with the special formula can be engineered to specific infants’ needs. The endocrinologist and the nutritionist can provide such a recipe.
A recent study reviewed eight infants with organic acidemias (propionic acidemia [PA; N =3], methylmalonic acidemia [MMA; N =2], malonic acidemia [MA; N =1], and glutaric acidemia type I [GI; N =2]) who breastfed for a mean of 8 months. 96 Five of the eight patients (PA, N =3; GI, N =2; MMA, N =1) received specific amino acid–free formula after the diagnosis was established. In all the patients, the special formula was given mixed with a small amount of expressed breast milk via a standard bottle immediately before breastfeeding. Clinical and biochemical monitoring of the infants was done closely at 2- to 4-week intervals and included ammonia and analysis of urine organic acids and/or plasma amino acids as the metabolic disorders required. Body length was above the 3rd percentile in all the patients except one (G1). Neurologic development was normal in one patient (MA). Five patients had mild to moderate mental retardation (PA, N =3; MMA, N =2), which is consistent with the natural course of the disease. 96
There are many other variations of these enzyme deficiency diseases. Without treatment, these amino acid enzyme deficiencies lead to deterioration, mental retardation, and often organ failure, especially liver failure. The National Organization for Rare Disorders Inc. (NORD) provides information for professionals, the lay public, and support groups regarding more than 1000 rare diseases. It lobbies for the development of specific treatments (orphan drugs). (Specific treatment information is available at the NORD website, http://www.rarediseases.org .)
Cystic fibrosis (CF) is an autosomal-recessive disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. The CFTR protein is in the epithelia of tissues, including the lungs, sweat glands, pancreas, and GI tract.
Screening tests for CF have been initiated in state-mandated metabolic screening programs for newborns, so a greater number will be identified early. Meconium plugs, especially large plugs and full-blown meconium ileus, have a high correlation with pancreatic enzyme deficiency and CF. As clinicians are alerted to meconium plugs, early tests for CF can be carried out and management adjusted. Breastfeeding is optimal not only for the nutrition but for the presence of enzymes to facilitate digestion and absorption of nutrients. Because infection is a significant morbidity in these children, the infection-protection properties of human milk make a critical impact. A study of infants exclusively breastfed or formula-fed showed that breastfeeding does not compromise growth and is associated with fewer infections and respiratory problems in infants with CF. 111
The first symptom in infants with CF is often failure to thrive. If an infant is breastfed, the mother may be forced to wean, yet the infant feeds even less well and has no weight gain on formula. Infants do better if placed back on the breast. Pumping to increase the mother's milk supply will help satiate the child's hunger. The use of pancreatic enzymes may be a way to improve tolerance and weight gain in these special breastfed infants rather than weaning to formula. 112 Prescribing pancreatic enzymes for a mother while breastfeeding, as described earlier, is also a consideration. 113
Breastfeeding is protective for infants with CF. In one study, 146 children (73 males and 73 females) were studied at age 5 to 18 years (mean 10.5±3.9 years). 114 Breastfed compared with formula-fed infants with CF had improved lung function (higher FEV-1, p =0.001) and a reduced incidence of infections in the first 3 years of life ( p =0.098) after multivariate analysis. A study of 99 infants with CF revealed that breastfeeding for at least 3 months delayed the first acquisition of Pseudomonas aeruginosa to beyond 12 months (4/16, 25% vs. 7/11, 64%, p =0.06). 115 A review of 85 infants with CF and meconium ileus revealed that 31 (37%) had a negative outcome at 12 months, 22 with stunted growth and 9 with chronic Pseudomonas infection. 116 Logistic regression showed that the probability of having a negative outcome was decreased if the infant did not have cholestasis (OR 0.125) or did not need intensive care unit (ICU) care (OR 0.141) and increased by not having been breastfed (OR 2.921). The European Society for Clinical Nutrition and Metabolism (ESPEN); the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN); and the European Society for Cystic Fibrosis (ECFS) have recommended exclusive breastfeeding for infants with CF. 117
A recent study evaluated a quality improvement project to improve breastfeeding in CF by incorporating international board-certified lactation consultants (IBCLCs) into the initial CF diagnosis visit to support mothers who were breastfeeding at diagnosis. 118 In the preintervention group, only 8/14 (57%) continued to provide breast milk after the first visit, whereas postintervention, 16/17 (94%) mothers continued to do so ( p =0.03). The duration of breastfeeding increased to an average of 7.7 months from an average of 6.4 months preintervention ( p =0.45). The authors concluded that lactation support to mothers can prolong the duration of breastfeeding in infants with CF.
Alpha 1 -antitrypsin is a serum protease inhibitor that inactivates a number of proteases. More than 24 genetic variants of this disease are designated B through Z, with the M variant being most common. Children with α 1 -antitrypsin deficiency are at increased risk for liver disease, which occurs most often during infancy and often progresses to cirrhosis and death. Udall et al. investigated the relationship between early feedings and the onset of liver disease. Severe liver disease was present in eight (40%) of the formula-fed and one (8%) of the breastfed infants (breastfed for only 5 weeks). 119 Of the 32 infants, 24 were still alive at the end of the study; 12 had been breastfed and 12 formula-fed during their first month of life. All eight of the deceased children had been formula-fed; small-for-gestational-age (SGA) and preterm infants had been excluded from the study so that all infants were equally stable at birth and capable of breastfeeding. A formula-fed infant was seven times more likely to develop liver disease.
With the increasing early diagnosis of α 1 -antitrypsin deficiency, encouraging a mother to breastfeed if her infant is affected would appear to have a significant impact on reducing the chance of long-range liver disease in her infant.
Acrodermatitis enteropathica is a rare and unique disease in which feeding an infant with human milk may be lifesaving. Its onset is as early as 3 weeks. 120 It is inherited as an autosomal-recessive trait and is characterized by a symmetric rash around the mouth, genitalia, and periphery of the extremities. The rash is an acute vesicobullous and eczematous eruption, often secondarily infected with C. albicans . It may be seen by the third week of life or not until late in infancy and has been associated with weaning from the breast. Failure to thrive; hair loss; irritability, and chronic, severe, intractable diarrhea are often life threatening. The disease has been associated with extremely low plasma zinc levels. Oral zinc sulfate has produced remission of the syndrome. Zinc deficiency was seen frequently in premature infants on peripheral alimentation until zinc was added to the solution.
Human milk contains less zinc than does bovine milk, with zinc concentrations of both decreasing throughout lactation. Eckert et al. studied the zinc binding in human and cow’s milk and noted that the low-molecular-weight binding ligand isolated from human milk may enhance absorption of zinc in these patients. 121 Gel chromatography indicated that most of the zinc in cow’s milk was associated with high-molecular-weight fractions, whereas zinc in human milk was associated with low-molecular-weight fractions. The copper–zinc ratio may also be of significance because the ratio is lower in cow’s milk. Pabon and Lonnerdal demonstrated in vivo zinc absorption in suckling rat pups dosed with 65Zn-labeled infant diets; the rats were killed, and individual tissues were gamma counted. 122 Lower zinc bioavailability was evident for bovine milk at pH=4.0 (%65Zn in liver =18.7±1.4) when compared with whey-predominant infant formula (WPF; 22.8±1.6) or human milk (26.9±0.8). Lowering the pH further decreased zinc bioavailability from human milk, but not from cow's milk or WPF.
The zinc-binding ligand from human milk was further identified as prostaglandin E by chromatography, ultrafiltration, and infrared spectroscopy by Evans and Johnson. 123 Patients also have low arachidonic acid levels. Arachidonic acid is a precursor of prostaglandin. The efficacy of human milk in the treatment of acrodermatitis enteropathica results from the presence of the zinc–prostaglandin complex. The primary deficiency in an infant is an inability to absorb zinc except in this complex form.
The clinical significance of the relationship of human milk to the onset of the disease and its treatment is in successfully developing lactation in the mother of such an infant, rare as the disease may be. Delayed lactation or relactation is possible and should be offered as an option to the mother of such an infant (see Chapter 19 ).
Several reports of isolated cases of zinc deficiency during breastfeeding have appeared in the literature. 124 , 125 More recent cases have described zinc deficiency in infants as a result of low concentrations in human milk. 126 In some cases, zinc levels in the milk were low; in others, they were not measured. 127 There are genetic mutations identified as causing an insufficiency of zinc transporter proteins, leading to a deficiency of zinc in human milk. 128 Other authors have described the regulation of iron, zinc, and copper in breast milk and the transport of these minerals across the mammary gland epithelium as poorly understood. Milk values at 9 months postpartum were not associated with maternal mineral status. 129 This suggested an active transport mechanism, according to these investigators. 129 One child had a classic “zinc-deficient” rash that responded to oral zinc therapy. In summary, the three most likely issues related to zinc deficiency in infants are insufficient zinc in their diet, malabsorption of zinc from the GI tract, or defective zinc transportation into milk. In the majority of cases, supplementing the infant with zinc should overcome the deficiency.
The treatment of choice is oral administration of zinc at a dose of 3 mg/kg of elemental zinc. 130 It is usually well tolerated, safe, inexpensive, effective, and expedient. When zinc deficiency occurs in a breastfed infant, the possibility of zinc deficiency in the milk, although a rare disorder, should be considered. 120 Treating the mother would be the appropriate therapy in such a case.
Premature infants have a negative zinc balance associated with inadequate mineral stores and high requirements associated with rapid growth. 131 Transient zinc deficiency in breastfed infants has been described as manifest by the classic zinc-deficiency rash and was treated by oral zinc to the infant because milk levels are normal in the mother.
In addition to infants who have been neurologically impaired by perinatal hypoxia or asphyxia as demonstrated by low Apgar scores, a rare infant may have an inherited neurologic problem as in a trisomy or a congenital abnormality, such as spina bifida. These infants can be breastfed in most situations, but it requires patience and perseverance. Holding the infant in a flexed position is an essential element of breastfeeding. A sling can work well if muscle tone and posture are part of an infant’s difficulties.
Down syndrome is one of the more common syndromes, occurring in 1 of 800 to 1000 births. Children with Down syndrome have characteristic phenotypic features and increased risk of congenital diseases and malformations, which may interfere with breastfeeding. These include hypotonia, suction-swallowing disorders, congenital heart disease, macroglossia, gastrointestinal malformations, hypothyroidism, and intrauterine growth restriction or low birth weight. Neonatal illness is common among newborns with Down syndrome, leading to hospital admissions, medical interventions, mother–infant separation, and formula supplementation, all of which limit breastfeeding success. In addition, maternal feelings at the birth of a disabled child, such as stress, frustration, and depression, may also have a negative influence on breastfeeding. However, breastfeeding is important for these infants because of their increased risk of morbidities associated with artificial feeding, such as ear, respiratory, and other infections; malocclusion; and developmental delay.
More than 90% of infants with Down syndrome have hypotonia. Hypotonia is a major feature that, along with a small mouth and a large tongue, makes breastfeeding a challenge. Breastfeeding is challenging, but many can successfully breastfeed at the breast. Sucking behavior with trisomy 21 is less efficient than in normal term infants, with multiple parameters affected, including the pressure, frequency, and duration of sucking and smooth peristaltic tongue movement. Mizuno and Ueda from Japan studied the sucking behavior of 14 infants with Down syndrome at 1, 4, 8, and 12 months of age. 132 Sucking pressure increased significantly from 1 to 4 months and again at 8 and 12 months. Sucking frequency increased from 1 to 4 months; however, sucking duration showed no improvement over time. Sucking efficiency demonstrated a significant stepwise increment throughout the first year. Ultrasound analysis revealed abnormal peristaltic tongue movements at 1 month. Normally, the tongue initially sticks to the palate, shortly after which the posterior portion of the tongue moves downward, releasing the palate. In infants with Down syndrome, the tongue often remains stuck to the palate more than once during the suck cycle. Of note, the mothers reported that feeding difficulties had decreased after 3 or 4 months of age, which is the time when the sucking pressure and frequency had significantly improved. Understanding this time frame allows health professionals to support breastfeeding and assist in maintaining a sufficient milk supply, despite significant difficulties at the beginning.
Breastfeeding is challenging, but many can successfully breastfeed at the breast. There is no evidence that infants with trisomy 21 or other hypotonic infants feed better with the bottle than at the breast and no evidence that these children need to feed from a bottle before attempting to breastfeed. A team of professionals with expertise in assisting infants with special needs to breastfeed should work together to help the mother–infant dyad. The importance of health professionals is highlighted in studies that found that mothers of these children felt they were not given appropriate support for breastfeeding. Instead, they expressed that “health professionals did not encourage breastfeeding and did not pass accurate information, confusing mothers about practices they should have, leaving doubts, discomfort, and a demotivating environment.” 133
In a study of 59 breastfed infants with Down syndrome, Aumonier and Cunningham reported that 31 had no sucking difficulty, 12 were successfully nursing within a week, and 16 required tube feeding initially, which was associated with other medical problems, including low birth weight (LBW), cardiac lesions, and jaundice. 134 Hyperbilirubinemia is common in trisomy and was seen in 49% of the infants in this study. Eighteen babies had multiple medical conditions, and 11 of them sucked poorly. The authors point out that the initial sucking ability of the infants did not appear to be a major cause for nonmaintenance of breastfeeding; 10 of the 13 mothers who discontinued breastfeeding cited insufficient milk as a contributing cause, which might have been prevented by early pumping of the breasts between feedings. 134
Another review of 73 cases of Down syndrome in Chile revealed that 47% (34/73) of the mothers exclusively breastfed for 6 months, despite the fact that 67% (49/73) of the infants had a disease or malformation that interfered with breastfeeding. 135 Seventy of 73 infants (96%) breastfed (exclusively or not) for at least 1 month, and 71% (52) breastfed for 6 months or more. Among the 39 mothers who did not exclusively breastfeed for 6 months, 25 (64.1%) reported child factors, most commonly poor weight gain and suck-swallow disorder, as reasons for discontinuing. Multivariate analysis revealed that hospitalization during the first 6 months was the most significant factor affecting the cessation of breastfeeding (OR 6.13, 95% CI 1.48 to 25.40). However, other studies show much lower breastfeeding rates, such as a 68% rate of any breastfeeding at birth (compared with a 95% rate in the general population) in a study in Croatia. 136
To breastfeed successfully, families need to understand that breastfeeding can occur even if the child presents difficulties and has some limitations. Had these mothers received adequate breastfeeding support, they would likely have felt empowered rather than frustrated.
At first, the infant may quickly drift off to sleep at the breast, and weight gain is slow. The mother learns to hold her breast in place because the infant's grasp is not strong enough to overcome gravity. A sling or pillow works to support the infant and free up the mother’s hands for additional support. The mother can hold the infant in place and free both the mother's hands to hold both the breast and infant’s jaw. This position is referred to as the Dancer hand position or Dancer hold specifically because of the position of the hand which can be helpful for the hypotonic infant in that it supports both the breast and the infant's chin and jaw while the infant is breastfeeding. (For a picture of the Dancer hold, see Fig. 13.1 .) The mother supports her breast with the thumb on top and three fingers underneath, while the index finger and thumb form a “U,” with the baby’s chin resting on the bottom of the “U.” This keeps the weight of the breast off the baby’s chin and helps him hold his head steady while nursing. Some mothers facilitate milk transfer by using hand compression in conjunction with breastfeeding, and more time may be necessary in the early weeks to complete a feeding. When the suckling is weak initially, the mother should pump between feedings to stimulate the production of milk. If supplements are required, it is best to provide them with a cup or supplemental nursing system. However, the use of a nursing supplementation aid alone may not be as helpful because it works best with an infant who has an effective latch.
Infants with Down syndrome or other genetic trisomies may be difficult to feed because of a variety of contributing factors, such as hypotonia and difficulty with position and/or latch, inadequate sucking force, difficulty with coordinating suck/swallow/breathe, the infant becoming easily fatigued and not completing a feeding session, and so forth. Careful early instruction and hands-on guidance are important, along with ongoing support and instruction to identify challenges or difficulties (see Figs. 13.1 and 13.2 ).
The initial goals for the mother–infant pair are developing confidence in handling the infant, adjusting to the infant's problem, and dealing with the parental grief and sense of loss—loss of the normal infant who was expected. If the mother has breastfed other children, the emphasis on breastfeeding modifications is more successful, and milk supply usually responds to manual expression and pumping. Initiating sufficient stimulus to the breast to increase milk production is critical in the first few days to induce good prolactin response, especially in primiparas. Renting a hospital-grade breast pump is a good investment, justifiable for reimbursement from health insurance by physician prescription.
With prenatal ultrasound, amniocentesis, and genetic testing or screening in older mothers, the diagnosis is often known before birth so that the family can be prepared. In developing a discharge plan for an infant with Down syndrome, a pediatrician will need to coordinate a team to avoid the fragmented care that develops with a multiple-problem situation, which may require the consultation of a geneticist, genetic counselor, cardiologist, and other medical experts to deal with the infant’s problems. Ideally, a pediatrician, family practitioner, or nurse practitioner can provide the additional support and counsel necessary.
The birth of an infant with a major genetic abnormality is a shock, even to the strongest parents. If the mother wants to breastfeed, she should be offered all the encouragement and support necessary. Usually she needs to talk with someone to express her anguish about the infant, not the feeding per se. A sympathetic nurse practitioner or lactation consultant in the pediatric office can be invaluable in providing support and expertise to help with the various management problems. If the mother chooses not to breastfeed, appropriate support can also be provided without disrupting treatment continuity.
It is especially important that these infants be breastfed if possible because they are particularly prone to infection, especially otitis media. Before the advent of antibiotics, they often died of overwhelming infection and rarely survived past 20 years of age. These infants and most other infants with developmental disorders do better with stimulation and affection, so the body contact and communication while at the breast are especially important. Those who have associated cardiac lesions not only can suckle, swallow, and breathe with less effort at the breast but also can receive a fluid more physiologic for their needs. Breastfed or bottle-fed, these infants gain poorly; thus switching to a bottle does not solve the problem. The recommendation that children with Down syndrome receive extra vitamins was tested in a controlled study in children 5 to 13 years of age, and no sustained improvement in the children's appearance, growth, behavior, or development was seen with added vitamins. 137
Growth charts from birth to 18 years illustrate the deficient growth through the growing periods. In infancy they fall behind, so this observation should not be used to discontinue breastfeeding. Breastfed infants remain healthier. Revised growth charts for infants and children with Down syndrome have been published because these children grow differently, but their growth has improved compared with previous studies. 138 Of note, the growth charts reflect the characteristic short stature, small head circumference, and normal to high relative weight measures (weight for length and body mass index [BMI]) associated with this genetic syndrome. The charts are also published on the Centers for Disease Control and Prevention (CDC) website. 139
Down syndrome is a lifelong condition. Having a support system is important for a family. Support groups of other families in the community serve as vital peer support.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here