Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Periprosthetic osteolysis is an adverse biologic reaction due to wear particles from joint replacements. Other contributory factors include increased intraarticular pressure and contamination of particles with bacterial or cellular by-products.
Excessive wear particle production stimulates a nonspecific chronic inflammatory reaction that results in increased bone degradation and decreased bone formation.
Interactions among many cell types are important to the development of osteolytic reactions. Macrophages are key cells. Recent research showed that macrophage phenotype is influenced by the local microenvironment.
Cytokines, chemokines, prostanoids, nitric oxide and superoxide metabolites, receptor activator of nuclear factor kappa B (NFκB; RANK), and other factors are the main biologic mediators of osteolysis.
Particle characteristics—including type of material, number (particle load), shape, surface area, surface energy, and other factors—determine the response of cells to particles. Individual patient characteristics may also modulate the extent of adverse response to wear particles.
Cross-linked polyethylene (XLPE) implants can mitigate particle-induced osteolysis. New technologies developing bioactive implants and other biologic interventions represent potential avenues to mitigate periprosthetic particle–associated osteolysis.
Wear—loss of material from the surfaces of the bearing couple—inevitably occurs with use of total joint replacements, leading to the production of particulate debris. According to McKellop, hundreds of thousands to millions of particles are produced from a metal-on-conventional-polyethylene total hip replacement (THR) with each step. The body normally distributes this debris locally and regionally via phagocytosis of particles by macrophages and other cells, leading to activation of cells to produce proinflammatory mediators. Despite the ongoing generation of small amounts of particulate debris, a state of homeostasis normally exists in the joint and surrounding tissues and the minor localized biologic reaction to wear debris has minimal consequences. However, when the host reaction to wear debris and associated by-products is excessive and persistent (state of decompensation), chronic inflammation can lead to periprosthetic bone loss by biologic processes that increase bone degradation and inhibit bone formation. This pathologic process is called particle-associated periprosthetic osteolysis or, among joint replacement surgeons and researchers, simply osteolysis . Although we normally think of osteolysis as a radiologic phenomenon (loss of bone on a radiograph of a joint replacement on follow-up), osteolysis is a complex pathophysiologic process with potentially major adverse clinical implications. This chapter will review the basic science underlying the biologic reactions to wear debris from polymeric, metallic, and ceramic implants.
Regardless of whether a hip prosthesis is cemented or cementless, or contains a bioactive surface coating, long-term implant stability within bone is a prerequisite for optimal pain-free function. During the surgical trauma of prosthesis implantation, an inflammatory response is initiated in which proinflammatory mediators are released locally. This begins a cascade of events resulting in the resorption of dead bone and marrow contents and the accretion of new bone immediately surrounding the implant. Over the ensuing weeks to months, the prosthesis becomes surrounded by a network of bony trabeculae, which undergo remodeling according to local biologic influences and mechanical loads. Thus, the bone–implant interface is a dynamic structure that matures and remodels over time, long after the prosthesis is implanted. Long-term prosthesis stabilization is possible whether the method of fixation is cemented or cementless. However, if the cement mantle fractures and degrades, or if excessive amounts of wear debris are produced from articulating or nonarticulating interfaces, an aggressive chronic inflammatory reaction can develop in response to foreign bodies, which may result in periprosthetic osteolysis ( Fig. 8.1 ).
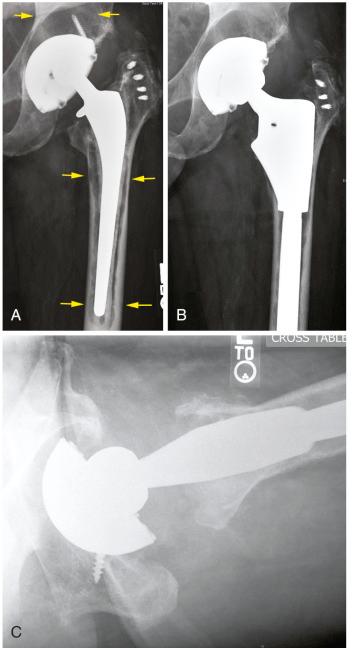
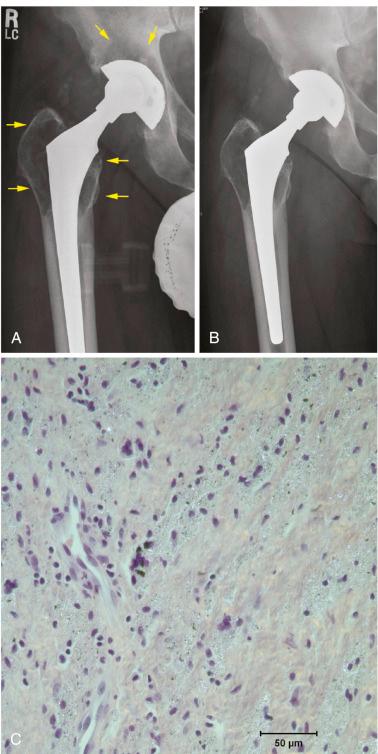
Examination of periprosthetic tissues retrieved at surgery has allowed identification of some of the key histologic characteristics and biologic mediators of bone destruction and remodeling. If the prosthesis is well fixed to bone, little intervening soft tissue is often found at the interface. This is true whether the prosthesis is cemented or cementless. The fibrohistiocytic tissues surrounding loose implants (with or without radiographic osteolysis) usually contain debris from various materials implanted in the operative site ( Fig. 8.2 ). These particles vary in size from the submicron (exceeding the visual capabilities of the light microscope) to larger shards of particles often several hundreds of microns in length. As we will see later, particles in the phagocytosable range, up to about 10 microns in size, and especially those around 1 micron or smaller, appear to be most stimulatory to cells.
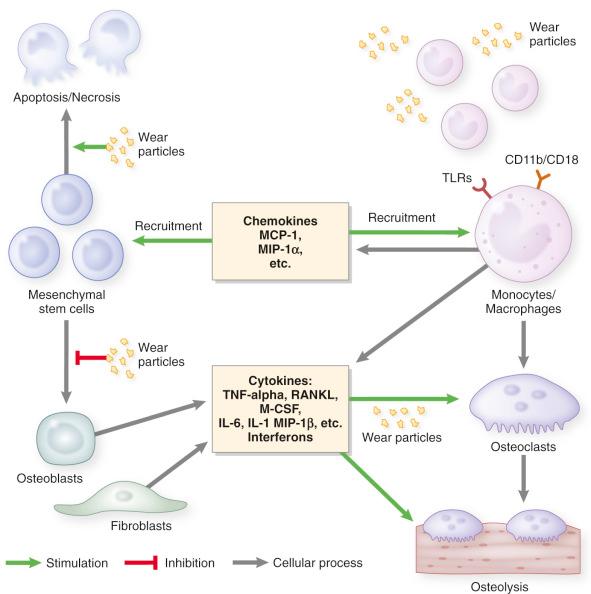
Polyethylene (PE) particles generated from metal-on-polyethylene (MOP) bearings interact with local cells and initiate a cascade of biologic events, which ultimately jeopardize implant longevity. The macrophage is the key cell in this nonspecific innate immunologic reaction. Macrophages are activated either by PE particle phagocytosis or by cell contact through membrane receptors (toll-like receptors [TLRs], CD11b, CD14, and others). TLR2 and TLR4 have been shown to be critical in the development of osteolysis. The inflammatory cascade is triggered and leads to the release of proinflammatory cytokines (interleukin-1 [IL-1], IL-6, TNF-α, and more), growth factors (such as macrophage colony-stimulating factor [M-CSF1]) and chemokines (including macrophage inflammatory protein-1 α [MIP-1α] and monocyte chemoattractant protein-1 [MCP-1]). The local microenvironment drives macrophages toward the M1 proinflammatory state. Macrophages can be broadly described as uncommitted M0, proinflammatory M1, and antiinflammatory M2. M1s produce proinflammatory mediators, including tumor necrosis factor- α (TNF-α), IL1, IL6, and express inducible nitric oxide synthase (iNOS), whereas M2s produce antiinflammatory factors—such as IL-4, IL-10, and IL-13—and express mammalian chitinase Ym1, arginase 1, CD163, and chitotriosidase. Retrieved tissues obtained from failed hip and knee replacement demonstrated an increased M1/M2 ratio compared to nonoperated osteoarthritic synovial tissues. Macrophage polarization is compromised with aging, which may mitigate the potential for tissue regeneration by M2 macrophages. Aging is associated with elevated proinflammatory factor levels, a phenomenon often referred to as “inflamm-aging.” A recent study showed significantly increased NF-κB activity at basal level in aged mesenchymal stem cells (MSCs) compared to young MSCs. Aged MSCs also had reduced osteogenic differentiation. Exposure to PE particles increased NF-κB in MSCs, which underscores the essential role of NF-κB activation during periprosthetic osteolysis.
Willert and Semlitsch first described the biology of prosthetic stabilization and recognized that continuous production of wear particles involved many cell types from hematopoietic and mesenchymal cell lineages. Normally, a state of prosthesis-tissue homeostasis exists, and the particle load that is generated is dealt with by normal clearance mechanisms without adverse consequences. However, if these mechanisms are overwhelmed (state of decompensation) as the result of excessive production of debris or other causes, osteolysis due to cellular activation and bone resorption will ensue. It is interesting to note that Willert described the pathophysiology of osteolysis-associated prosthetic loosening long before others postulated more widespread distribution of particles into an “effective joint space,” or that increased hydraulic pressure with loading of the limb resulted in fluid flow around the prosthesis, distributing inflammatory cells and factors more extensively. Charnley first believed that areas of osteolysis around hip replacements were the result of low-grade infection.
Cemented MOP hip implants that are still functioning well may already demonstrate histologic findings consistent with excessive wear particle production. In autopsy specimens, the density of macrophages and foreign-body giant cells in periprosthetic tissues was found to correlate with time after prosthetic implantation, membrane thickness, and polyethylene particle density. Wear particles in the joint gain access to the edges of the prosthesis interface and then migrate in centripetal fashion through the fibrous interface and the cancellous bone. Examination of tissues harvested from cemented implants has revealed that the most critical factor associated with radiologic osteolysis was the concentration of PE particles in the membranous tissue interface. In cementless implants, fibrous tissue present at the prosthetic interface functions as a conduit for migration of particles from the joint articulation into immediate periprosthetic tissues.
Goldring and colleagues were among the first to apply the techniques of cell biology to tissues retrieved from revised implants. Using histologic, cell, and organ culture methods, they showed that tissue around loose cemented prostheses contained a pseudosynovial layer adjacent to the cement. Particles of polymethylmethacrylate (PMMA) bone cement within the membrane were found to be surrounded and engulfed by mononucleated and multinucleated macrophages and foreign-body giant cells in a fibrovascular stroma. Lymphocytes were seen more rarely. Culture and analysis of the membrane showed that it had the capacity to produce large amounts of prostaglandin (PG) E 2 and collagenase and enhanced bone-resorbing activity. Since these seminal studies were conducted, numerous investigators have shown that osteolytic membranes from failed prostheses express numerous degradative enzymes, cytokines, chemokines, nitrogen oxide (NO) and superoxide metabolites, and other proinflammatory and antiinflammatory molecules ( Fig. 8.3 ).
In some cases, an aggressive granulomatous reaction develops, with localized, progressively expanding areas of bone lysis containing activated macrophages, fibroblasts, and other cells. It is postulated that these cases may be due to an uncoupling of events that normally lead to monocyte-macrophage clearance of wear particles via the nonspecific foreign-body reaction and fibroblast-mediated formation and remodeling of the extracellular tissue matrix. However, the periprosthetic tissues are heterogeneous; biopsies from different areas may yield different histologic and cytokine profiles. It is interesting to note that the bony interface surrounding loose hip and knee prostheses presents histologic evidence of both bone destruction and active bone formation, which implies that even during osteolysis, an active reparative process is ongoing. Thus, heightened alkaline phosphatase activity, a marker of bone formation, has been noted at the bony surface surrounding areas of osteolysis.
NFκB is a transcription factor that regulates numerous proinflammatory and antiinflammatory pathways. TNF-α and IL-1β are two proinflammatory cytokines that play an important role in particle-associated periprosthetic osteolysis; they are under the regulatory control of NFκB. RANK (receptor activator of NFκB), a membrane-bound receptor on the surface of osteoclasts, activates the transcription factor NFκB. Receptor activator of nuclear factor kappa-B ligand (RANKL), a member of the TNF superfamily, is a receptor ligand that is released from osteoblasts, stromal cells, and other activated cells in the inflammatory process. RANKL interacts with RANK, which, together with M-CSF, is essential for the differentiation and maturation of tissue monocytes/macrophages into bone-resorbing osteoclasts. RANKL is inhibited by the soluble decoy protein receptor antagonist osteoprotegerin (OPG). Studies have shown increased expression of RANKL and M-CSF and decreased OPG in the synovial fluid and periprosthetic tissues of revised prostheses exhibiting radiographic osteolysis.
The host reaction to MOP implants is generally thought to be both a nonspecific foreign body reaction and a chronic inflammatory reaction. Although attempts have been made to demonstrate an important role for T and B lymphocytes, it would appear that lymphocytes play an immunomodulatory rather than a primary role. Nevertheless, evidence of antigen presentation to lymphocytes has been reported in MOP joint replacements. These biologic pathways should be distinguished from the T cell–mediated, antigen-associated type IV allergic reactions seen in cases of metal-on-metal (MOM) implants.
Ceramic particles have a bimodal size distribution, either nanometric (range, 5–90 nm) or micrometric (as large as 3.2 µm). Current ceramic implants are made of alumina (AL 2 O 3 ) and zirconia (ZrO 2 ). Gutwein and Webster showed that nanophase particles (23 nm) were harmless to osteoblast viability compared to larger particles. Catelas et al. challenged J774 macrophages with ceramic particles of various sizes, compositions and concentrations in comparison to PE particles. Their analysis showed that macrophage cell death increased with concentration and sizes greater than 2 µm. TNF-α release was significantly higher with PE particles than with ceramic particles. Other studies have also reported limited inflammatory reaction and toxicity in the presence of ceramic particles.
Numerous in vivo animal models and in vitro studies have attempted to simulate the biologic processes associated with particle-induced osteolysis and to identify the critical variables and mechanisms underlying particulate disease. Animal models have included various small and large species, with and without weight-bearing implants, particles with different material properties and characteristics, and harvest periods that have varied from hours to many months. Many of these in vivo models have been summarized in recent review articles ( Table 8.1 ). It is often difficult to make definitive statements about particle-induced osteolysis on the basis of in vivo animal models because of the different variables used in each model and the relatively short duration of animal studies (weeks and months) compared with the period required for development of clinical and radiologic osteolysis in humans (years). However, experiments performed in animal models have provided some useful concepts that can be generalized to periprosthetic reactions in humans.
| Species | Type of Model | Key References |
|---|---|---|
| Mouse | Calvarial | |
| Mouse | Calvarial modified (paraclip) | |
| Mouse | Air pouch | |
| Mouse | Intramedullary implant with particles—femur | |
| Mouse | Intramedullary injection (no implant)—femur | |
| Mouse | Intramedullary implant with particles—tibia | |
| Rat | Intramedullary implant with particles—tibia | |
| Rat | Intraarticular or intramedullary—femur | |
| Rabbit | Intramedullary—femur | |
| Rabbit | Harvest chamber—tibia | |
| Dog | Pistoning implant—femoral condyle | |
| Dog | Intramedullary—hip replacement | |
| Sheep | Intraarticular injection—hip replacement |
The biologic pathways involved in foreign body and chronic inflammatory reactions are complex, redundant, and difficult to inhibit completely. As mentioned previously, numerous cellular constituents and inflammatory factors participate in this reaction. Furthermore, various characteristics—including the material, number, size, shape, surface area, topography, and surface chemistry of particulate debris—have been shown to influence the cellular and inflammatory profile. In general, bulk materials produce a more benign interface compared with the same volume of material in particulate form. Smaller particles that are phagocytosable, especially those around 1 micron or smaller, appear to be the most reactive. However, very small particles, less than about 0.3 microns, do not appear to activate cells, as they undergo pinocytosis rather than phagocytosis. Smaller particles may agglomerate together and, therefore, become much larger than the individual particles. This is especially true for polymers such as PE. Irregularly shaped particles are more activating than rounder particles. In general, excluding the type IV cell-mediated immune reactions that are sometimes seen with metals, particulate materials such as alumina ceramics evoke less of a foreign-body and chronic inflammatory reaction compared with metals (e.g., titanium alloy, cobalt chrome alloy, tantalum) at the same dose.
Particulate polymers, such as PE and PMMA, evoke the most exuberant reactions. In one study in which PE particles incited an inflammatory response, the same concentration of cobalt chrome alloy particles caused cell necrosis. These experiments are controversial, however, because of difficulties involved in obtaining and exposing cells to particles of similar doses, shapes, surface areas, surface chemistries, and so forth. For example, highly cross-linked PE (HXLPE) particles have been found to be more bioreactive (i.e., they produce more inflammatory cytokines) than similar particles of conventional PE in vitro. However, in vivo wear of HXLPE is far less than that of conventional PE, thereby presenting a much lower particle load to the body. It is clear that there is a need for standardized in vitro and in vivo models using standardized particles with known characteristics to more clearly delineate the biologic effects of particles. In light of the development of second-generation HXLPE, Jarret et al. investigated the biologic response of vitamin-E-doped PE (VE-HXLPE). The authors surgically placed VE-HXLPE plugs (1 cm × 3.75 cm) subcutaneously in rabbits and also performed THR in dogs. Their results showed no foreign-body reaction associated with the plug at 12 weeks. Tissue harvesting in dogs at 12 weeks showed a pseudocapsule rich in fibroblasts, small-caliber blood vessels, and extravasated red blood cells. The bone-implant composite sections showed no evidence of macrophage infiltration or active bone resorption. Similarly, Huang et al. used a calvarial model to analyze the effect of VE-HXLPE particles compared to HXLPE and conventional ultra-high-molecular-weight polyethylene (CPE). HXLPE induced the most vigorous osteolytic response, whereas VE-HXLPE and CPE showed no significant differences in inflammation and osteolysis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here