Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The original design of the bilobe flap is attributed to Esser, who described its use in 1918 for reconstruction of nasal tip defects. Ziminy and others expanded the use of the flap to reconstruct defects on the trunk and soles. Nevertheless, most authors now share the opinion that this flap is most useful for facial reconstruction, particularly of the nose.
Esser’s original design required that the angle of tissue transfer be 90° between each lobe of the flap, for a total pivotal movement of over 180°. An example of this design for repair of a nasal tip defect would be the first lobe of the flap harvested from the nasal sidewall and the second lobe from the glabella. This design maximizes the distance that skin can be moved, but the wide angles between the two lobes (90°) also maximize the standing cutaneous deformities (SCDs) and the likelihood of creating trap-door deformities of both the first and second lobes. These were common problems with the original flap design and limited the use of the bilobe flap for facial reconstruction.
Bilobe flaps are double transposition flaps that share a single base. Similar to single transposition flaps, bilobe flaps move around pivotal points located at their base and develop SCDs as they pivot. Because each flap or lobe moves around an independent pivotal point, each lobe develops an individual SCD. The greater the arc of movement about their pivotal points, the larger the SCDs.
In general, bilobe flaps are designed in such a way that the first lobe is immediately adjacent to the defect and has a surface area that is less than the surface area of the defect. Thus part of the closure of the defect is achieved by secondary movement of surrounding skin through direct advancement. The relationship between the surface area of the first lobe and the size of the skin defect depends on the location of the defect on the face and the elasticity of skin surrounding the defect. On the caudal nose for instance, the first lobe must nearly approximate the size of the defect because of the inelasticity of nasal tip skin. On the cheek, however, the first lobe may be designed considerably smaller than the size of the defect (up to 25% less in surface area) because of the general elasticity and redundancy of the skin surrounding cheek defects. The second lobe of a bilobe flap is usually designed so that its surface area is less than the surface area of the defect left by harvesting the first lobe. Again, advancement of adjacent skin assists the second lobe in repair of the donor site of the first lobe. The defect left by the second lobe is closed primarily by direct advancement of surrounding skin. Thus, for the bilobe flap to work, there must be considerable skin laxity in the vicinity of the first and second lobes to achieve wound repair without excessive wound closure tension.
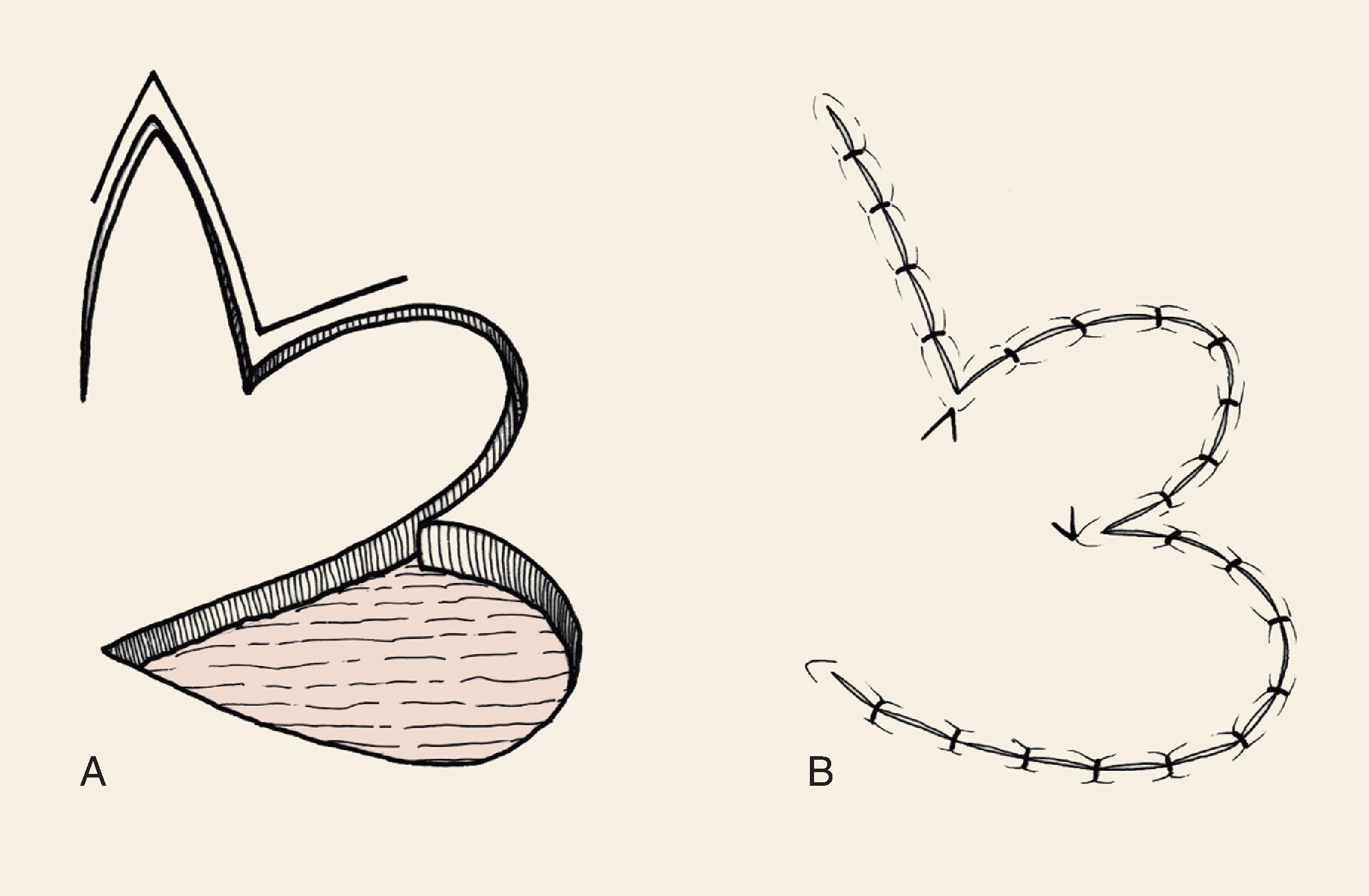
The bilobe flap would appear to be a modified rotation flap with some component of transposition. During transfer of the flap, however, there is noticeably less restriction of tissue movement than would be present with a pure rotation flap. This ease of tissue movement of the first lobe is the result, in part, of transposing the triangular-shaped peninsula of skin located between the defect and the first lobe of the flap. The transposition of this skin peninsula adjacent to the distal portion of the first lobe of the flap in essence represents a modified Z-plasty ( Fig. 10.1 ). Likewise, there is a triangular-shaped peninsula of skin that forms between the first and second lobes, which is also transposed during closure of the donor site of the second lobe. Thus the bilobe flap in some ways represents a modified double Z-plasty. This results in repositioning of the skin adjacent to the defect and the two lobes of the flap. This in turn results in an overall reduction in wound closure tension compared with using a single transposition or rotation flap.
Bilobe flaps expand the use of transposition flaps. The major advantage of bilobe flaps is the ability to recruit skin for construction of a flap from areas of skin redundancy that are not adjacent to the defect. On the cheek, this skin redundancy may be located at some distance from the defect and may be difficult to transfer to the recipient site by other surgical approaches. Defects that cannot be easily repaired with a single transposition flap without excessive wound closure tension causing distortion of facial structures may often be reconstructed with a bilobe flap. This is because the second lobe of the transposition flap reduces overall wound closure tension and provides additional skin to the proximity of the reconstruction. Furthermore, bilobe flaps transfer the tension of wound closure through a 90° arc, which is more than the usual 45° to 60° arc of transfer of a single lobe transposition flap. This greater distribution of wound closure tension helps contribute to minimizing the distortion of structures surrounding the primary defect.
McGregor and Soutar altered the design of bilobe flaps and noted that the degree of pivotal movement could be varied greatly from the original 90° between each lobe. In 1989, Zitelli published his experience using the bilobe flap for nasal reconstruction. He emphasized the use of narrow angles of transfer, 45° between each lobe, so that the total pivotal movement of tissue occurs over no more than 90° to 100°. This eliminated the need to excise SCDs and trap-door deformities were frequently avoided. Burget confirmed the excellent results using this design for reconstruction of the nose. Other surgeons also advocated a similar design for repair of skin defects of the cheek, chin, and lips. , They used narrow angles between the lobes of the flap and achieved better results than when using traditionally designed bilobe flaps that are transposed through an arc of 180°.
Limiting the angle between the axis of the first and second lobes of the bilobe flap is more important on the nose than on the cheek. When bilobe flaps are used on the cheek, the primary determinants of the position of the first and second lobes of the flap are the location of the defect and the availability of donor skin for construction of the two lobes. In such instances, the first and second lobes are designed in areas of greatest skin laxity or in areas where scar camouflage will be maximized. This may on occasion necessitate design of the second lobe along an axis that is 180° to the axis of the defect.
Variations of the bilobe flap are useful. On the nose, the flap may be based medially, although it works best and is most often designed with a lateral base ( Fig. 10.2 ). The lobes of the flap may be designed with rhombic shapes for smaller defects. Bilobe flaps may be used to repair large defects located on the cheek in lieu of larger cervical facial rotation advancement flaps. They may also be used to transfer skin from the postauricular area to cover helical rim defects that might otherwise require skin grafting.
![FIG. 10.2, Variations of bilobe flap used to repair caudal nasal cutaneous defects. (From Zitelli JA, Baker SR: Bilobe flaps. In Baker SR, Swanson NA [eds]: Local Flaps in Facial Reconstruction. Mosby, 1995, pp 170-174, Figs. 5B, 7B, 9B with permission.) FIG. 10.2, Variations of bilobe flap used to repair caudal nasal cutaneous defects. (From Zitelli JA, Baker SR: Bilobe flaps. In Baker SR, Swanson NA [eds]: Local Flaps in Facial Reconstruction. Mosby, 1995, pp 170-174, Figs. 5B, 7B, 9B with permission.)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/BILOBEFLAPS/1_3s20B9780323683906000104.jpg)
The bilobe flap is best suited for reconstruction of circular defects on the caudal one-third of the nose. In this location, reconstruction with other types of nasal cutaneous flaps is difficult. The bilobe nasal flap enables the surgeon to repair defects using adjacent skin without causing nasal distortion. The aesthetic result is usually excellent and often surpasses those resulting from use of full-thickness skin grafts. This is especially true for deep nasal cutaneous defects. As a consequence, the bilobe flap is a preferred flap for reconstruction of the nose in the area of the tip, caudal dorsum, and caudal nasal sidewall when skin defects are 1 to 2 cm in size.
The primary disadvantage of the bilobe flap is that most of the incisions necessary to create the flap produce scars that do not parallel relaxed skin tension lines (RSTLs). On the nose, incisions for the flap do not lie within boundary lines separating nasal aesthetic units. The resulting scar is also lengthy because of the need to elevate two lobes. Because bilobe flaps have curvilinear incisions, they are prone to develop a trap-door deformity. This is especially true when used on the nose in patients with thick skin or with sebaceous gland hyperplasia. On the nose, trap-door deformity may be minimized by extensive peripheral undermining of the nasal skin as far laterally as the cheek. Designing the lobes of the flap with angles such as with rectangular or rhombic-shaped lobes may also reduce the incidence of trap-door deformity. Adjusting the thickness of the first lobe so that it matches the depth of the recipient site is accomplished by thinning the flap if necessary and may be helpful in preventing the deformity.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here