Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The significance and multiple functions of fat are not always fully appreciated. Fat serves not only as one of the principal and most readily available sources of energy in the body, but also functions as a barrier for the conservation of heat and as mechanical protection of the underlying tissues against physical injury. Two basic forms of adipose tissue can be distinguished: white fat and brown fat.
White fat makes its first appearance at a relatively late stage of development; it is rarely encountered before the third or fourth month of intrauterine life. In its earliest stages, after 10 to 14 weeks’ gestation, it consists of aggregates of mesenchymal cells that are condensed around proliferating primitive blood vessels. Following this stage, the stellate-shaped preadipocytes are organized into lobules that contain a rich network of proliferating capillaries. At later stages (14-24 weeks’ gestation), small lipid droplets appear in these cells, gradually converting them to rounded or spherical, multivacuolated lipoblasts. Intracellular glycogen is usually present at this stage of development. The multiple lipid droplets then fuse to form a single vacuole and displace the nucleus marginally, forming the mature fat cell, or lipocyte. Small aggregates of lipocytes form lobules that make their first appearance in the regions of the face, neck, breast, and abdominal wall, followed by the back and shoulders. The lobules multiply and enlarge, and by the end of the fifth month a continuous subcutaneous layer of fat is formed in the extremities.
Postnatally, white fat cells enlarge significantly during the first 6 months of life without a significant increase in cell number. This phase is followed by a progressive increase in adipocyte number, although the cell size remains fairly constant. At puberty, there is a marked increase in adipocyte size and number. After puberty, new adipocytes continue to form throughout adult life, although at a much slower rate.
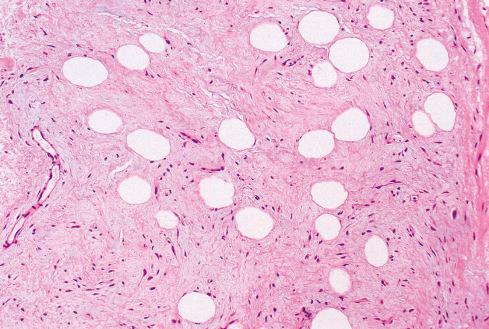
Histologically, differentiated white fat consists of spherical or polygonal cells in which most of the cytoplasm has been replaced by a single large lipid droplet, leaving only a narrow rim of cytoplasm at the periphery. The eccentrically placed nucleus is flattened and is crescent shaped on cross section, and it may contain one small lipid invagination (Lochkern). Like any metabolically active tissue, white fat is highly vascularized, a feature that is more evident in atrophic fat than in normal fat. In the subcutis and to a lesser extent in deeper tissues, the fat cells are arranged in distinct lobules separated by a thin membrane of fibrous connective tissue. The lobular architecture of white fat is most prominent in areas subjected to pressure, such as the foot, and probably has a cushioning effect.
Continued accumulation of cytoplasm and increasing amounts of intracellular lipid lead to more-rounded cells, which are characterized by a large, centrally located lipid droplet, a thin rim of cytoplasm, and a peripherally placed, flattened, or crescent-shaped nucleus. There is a membrane separating the central lipid inclusion from the surrounding cytoplasm. This signet-ring stage of cellular development represents the lipocyte of mature adipose tissue.
The precursors of brown fat are spindle-shaped cells that are closely related to a network of capillaries. Subsequently, there is a proliferation of capillaries and brown adipocytes, with organization into lobules by fibrous connective tissue septa. As the cells accumulate lipid, they are initially unilocular, but with further lipid accumulation, multiple cytoplasmic lipid vacuoles appear. Brown fat is found mainly in infants and children and gradually disappears from most sites with increasing age. In children, brown fat deposits are most conspicuous in the interscapular region, around the blood vessels and muscles of the neck, around the structures of the mediastinum, adjacent to the lung hila, on the anterior abdominal wall, and surrounding intraabdominal and retroperitoneal structures, including the kidneys, pancreas, and spleen. During adulthood, deposits of brown fat persist around the kidneys, adrenal glands, and aorta and within the mediastinum and neck.
The term brown fat refers to its gross appearance, which results from its abundant vascularity and numerous mitochondria. Compared to white fat, brown fat tends to have a more prominent lobulated growth pattern. Its cells are smaller (25-40 μm in diameter), are round or polygonal, and contain a large amount of deeply eosinophilic cytoplasm. The cells are mostly multivacuolated, with distinctly granular cytoplasm between the individual lipid droplets. Intermixed with these cells are nonvacuolated, purely granular cells and cells with a single large lipid vacuole, resembling lipocytes. The nuclei are rounded and situated in a central position, although the nucleus may be displaced to the periphery in cells with large lipid vacuoles, as in white fat. The cells are arranged in distinct lobular aggregates and are intimately associated with a prominent vascular network and numerous nerves.
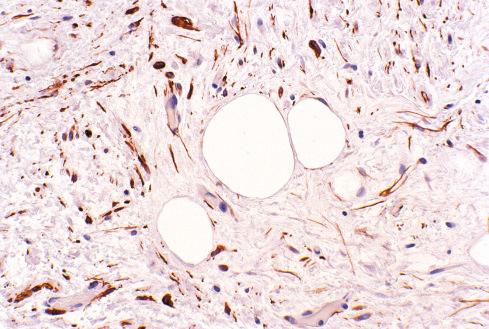
The DDIT3 gene (formerly known as CHOP ), located on the long arm of chromosome 12, appears to be involved in adipocytic differentiation. This gene encodes a member of the CCAAT/enhancer-binding protein (C/EBP) family, which may be an inhibitor of other C/EBP transcription factors known to be important in cell proliferation. Members of the C/EBP group are highly expressed in fat and are involved in the growth arrest of terminally differentiated adipocytes. Adipocytes and lipoblasts in benign and malignant fatty tumors stain positively for S-100 protein, although this marker is rarely used or needed in clinical practice.
It is widely assumed that benign lipomatous tumors represent a common group of neoplasms that cause few complaints or complications and present little diagnostic difficulty. This may be largely true for the ordinary subcutaneous lipoma, but it does not take into account the enormous variety of benign tumors and tumorlike lesions of adipose tissue that are well defined but often have received little attention in the medical literature. In fact, benign lipomatous tumors are among the most frequently received in a consultation practice.
The bulk of lipomatous tumors may be grouped into the following four categories:
Superficial lipoma , a tumor composed of mature fat and arising in the superficial (subcutaneous) soft tissues, represents by far the most common mesenchymal neoplasm.
Deep lipomas arise from or are intimately associated with tissues deep to the subcutis or arise in specific anatomic sites. The main subdivisions of this group are intramuscular and intermuscular lipoma, lipoma of the tendon sheath, neural fibrolipoma with and without macrodactyly (fibrolipomatous hamartoma), and lumbosacral lipoma.
Infiltrating or diffuse neoplastic or nonneoplastic proliferations of mature fat may cause compression of vital structures or may be confused with atypical lipomatous neoplasm/well-differentiated liposarcoma. This group is composed of six entities: diffuse lipomatosis, pelvic lipomatosis, symmetric lipomatosis (Madelung disease), adiposis dolorosa (Dercum disease), steroid lipomatosis, and nevus lipomatosus.
Variants of lipoma are much less common and differ from ordinary lipoma by a characteristic microscopic picture and specific clinical setting. These include angiolipoma, myolipoma, myelolipoma, chondroid lipoma, spindle cell/pleomorphic lipoma, hibernoma, and lipoblastoma/lipoblastomatosis.
When describing these entities, no attempt has been made to distinguish among true neoplasms, hamartomatous processes, and localized overgrowth of fat, because it would be largely speculative and of little practical consequence. In the past 25 years, cytogenetic data have contributed significantly to the understanding of the pathogenesis of both benign and malignant lipomatous tumors. Although cytogenetic analysis is of limited diagnostic utility in benign lipomatous tumors, the knowledge gained by such analyses has allowed a better understanding of how these lipomatous tumors are related to one another. Chapter 4 provides a summary of these alterations.
Solitary lipomas , consisting entirely of mature fat, have been largely ignored in the literature because they grow insidiously and cause few problems other than those of a localized mass. Many lipomas remain unrecorded or are brought to the attention of a physician only if they reach a large size or cause cosmetic problems or complications because of their anatomic site. As a consequence, the reported incidence of lipoma is certainly much lower than the actual incidence. Even if only the recorded data were considered, however, lipomas outnumber other benign or malignant soft tissue tumors by a considerable margin.
Lipoma is rare during the first two decades of life and usually makes its appearance when fat begins to accumulate in inactive individuals. Most become clinically apparent in patients 40 to 60 years of age. When not excised, the lipoma persists for the remainder of life, although they negligibly increase in size after the initial growth period. Statistics vary as to gender incidence, but most report a higher incidence in men. No difference regarding ethnicity is apparent.
Two types of solitary lipoma can be distinguished. Subcutaneous (superficial) lipomas are most common in the regions of the upper back and neck, shoulder, and abdomen, followed in frequency by the proximal portions of the extremities, chiefly the upper arms, buttocks, and upper thigh. They are seldom encountered in the face, hands, lower legs, or feet.
Deep lipomas are much rarer. They are often detected at a relatively late stage of development and consequently tend to be larger than superficial lipomas. They may also arise from juxtaarticular regions or the periosteum ( parosteal lipoma ), sometimes causing nerve compression, erosion of bone, or focal cortical hyperostosis. Deep lipomas in the region of the head occur chiefly in the forehead and scalp; those in the trunk are found principally in the thorax and mediastinum, chest wall and pleura, and pelvis and paratesticular region. Although uncommon, intramucosal lipomas of the colon should raise consideration of Cowden syndrome.
Deep or subfascial lipomas tend to be less well circumscribed than superficial ones, and their contours are usually determined by the space that they occupy. Intrathoracic lipomas, for instance, may extend from the upper mediastinum, neck, or subpleural region ( cervicomediastinal lipoma ) into the subcutis of the chest wall, sometimes assuming an hourglass configuration. Deep-seated lipomas of the hand or wrist form irregular masses with multiple processes underneath fascia or aponeuroses; they may attain a large size and, on rare occasions, extend from the palm to the dorsal surface of the hand. These tumors must be distinguished from lipomas growing in the tendon sheath ( endovaginal lipomas ) and those involving major nerves in the regions of the hand and wrist ( neural fibrolipomas or fibrolipomatous hamartomas ), which usually occur in young patients and may be associated with macrodactyly.
There are also rare lipoma-like fatty proliferations in the region of the umbilicus and inguinal ring ( hernial lipoma ) that may be associated with direct or indirect hernias or merely simulate a hernia clinically. A similar overgrowth of fat arising from surgical scars has been termed incisional lipoma .
The usual clinical history of lipoma is that of an asymptomatic, slowly growing, round or discoid mass with a soft consistency. Pain is rare with ordinary lipomas; when it occurs, it is a late symptom generally confined to angiolipomas or lipomas that compress peripheral nerves. Lipomas are more common in obese persons and often increase in size during a period of rapid weight gain. In contrast, severe weight loss in cachectic patients or during periods of prolonged starvation rarely affects the size of a lipoma, suggesting that the fatty tissue of lipomas (or liposarcomas) is largely unavailable for general metabolism.
Deep lipomas may cause a variety of symptoms, depending on their site and size. The symptoms range from a feeling of fullness and discomfort on motion and, rarely, restriction of movement with lipomas of the hand to dyspnea or palpitation with mediastinal tumors. Although some benign lipomatous tumors have been described in the retroperitoneum, most reported in the early literature probably represent well-differentiated liposarcomas rather than lipomas. However, retroperitoneal lipomas clearly exist but can only be diagnosed after extensive sampling and molecular analysis revealing an absence of MDM2 amplification. This topic is more thoroughly discussed in Chapter 14 .
Imaging studies are extremely helpful for diagnosis; lipomas present as globular radiolucent masses clearly outlined by the greater density of the surrounding tissue. CT scans reveal a mass having the appearance of subcutaneous fat and, like fat, having a much more uniform density than liposarcomas. On MRI, both benign and malignant lipomatous tumors exhibit a high signal intensity on T1-weighted images.
Subcutaneous lipoma usually manifests as a soft, well-circumscribed, thinly encapsulated, rounded mass varying in size from a few millimeters to 5 cm or more (median: 3 cm); lipomas larger than 10 cm are uncommon. On cross section, lipomas are pale yellow to orange and have a uniform greasy surface and an irregular lobular pattern ( Fig. 13.1A ). Lipomas of deeper structures vary much more in shape, but they also tend to be well delineated from the surrounding tissues by a thin capsule. Focal discoloration caused by hemorrhage or fat necrosis occurs, but it is much less common than in liposarcomas.
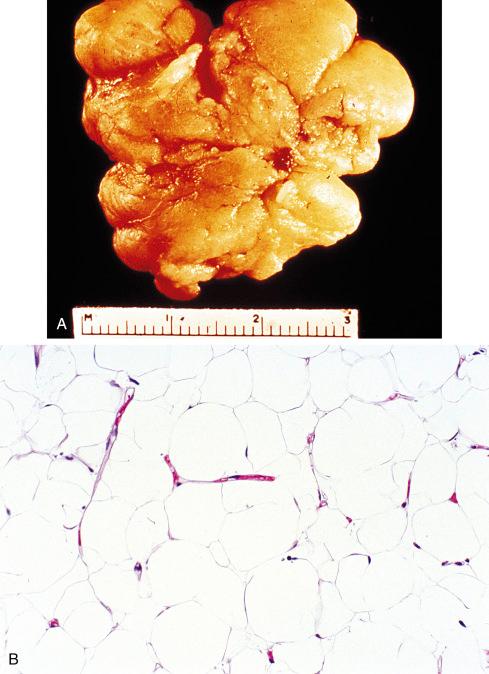
Lipomas differ little in microscopic appearance from the surrounding fat because they are composed of mature fat cells, but the cells vary slightly in size and shape and are somewhat larger ( Fig. 13.1B ). The nuclei are uniform, and importantly, there is an absence of nuclear hyperchromasia. Subcutaneous lipomas are usually thinly encapsulated and have a distinct lobular configuration. All are well vascularized, but under normal conditions the vascular network is compressed by the distended lipocytes and is not clearly discernible. The rich vascularity of these tumors becomes apparent in atrophic lipomas , where the greatly reduced volume of the lipocytes reveals the intricate vascular network in the interstitial space.
Lipomas are occasionally altered by an admixture of other mesenchymal elements that constitute an intrinsic part of the tumor. The most common of these elements is fibrous connective tissue, which is often hyalinized and may or may not be associated with the capsule or fibrous septa ( fibrolipomas ). Sclerotic lipomas have a predilection to occur on the scalp or hands of young men and are composed predominantly of sclerotic fibrous tissue with only focal lipocytic areas. Some lipomas show extensive myxoid change ( myxolipomas ); such cases may be difficult to distinguish from spindle cell lipomas ( Fig 13.2 ), and in fact many probably are hypocellular spindle cell lipomas with extensive myxoid change. Some of these lesions have an abundance of thin- and thick-walled blood vessels and have been termed vascular myxolipoma or angiomyxolipoma ; these are merely descriptive terms, however, and are not used as a distinctive diagnostic category of lipoma. Distinction of these tumors from myxomas and myxoid liposarcomas may occasionally be difficult. In general, however, the presence of transitional zones between fat and myxoid areas helps rule out myxoma, and the absence of lipoblasts and a diffuse plexiform capillary pattern militates against myxoid liposarcoma. Vacuolated cells containing mucoid material are occasionally seen in myxolipomas and angiomyxolipomas; but, unlike neoplastic lipoblasts, these cells lack hyperchromatic nuclei and distinctly outlined lipid droplets within the cytoplasm. In difficult cases, molecular analysis to show an absence of alterations of DDIT3 can be extremely helpful. Cartilaginous or osseous metaplasia ( chondrolipoma, osteolipoma ) is rare and is mainly encountered in lipomas of large size and long duration.
Lipomas with striking variation in adipocyte size, scattered cytologic atypia, and p53 overexpression (but not mutation) have been reported under the names anisometric cell lipoma and dysplastic lipoma. RB gene abnormalities have been detected in these tumors which may imply a relationship with spindle cell/pleomorphic lipomas.
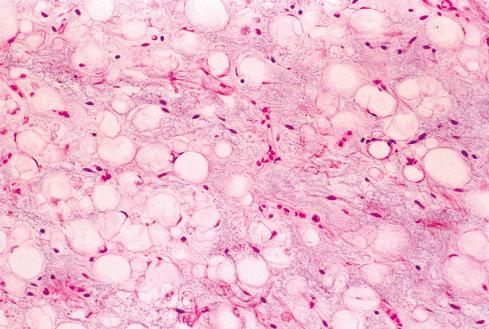
Secondary changes occasionally result from impaired blood supply or traumatic injury. Prolonged ischemia may lead to infarction, hemorrhage, and calcification and may result in impressive cystlike changes. Similarly, infection or trauma may cause fat necrosis and local liquefaction of fat, a process marked by phagocytic activity and formation of lipid cysts. Characteristically, nests of foamy macrophages are found in the intercellular spaces or around ruptured or traumatized lipocytes ( Fig. 13.3A and B ). This process is sometimes accompanied by multinucleated giant cells and scattered inflammatory elements, chiefly lymphocytes or plasma cells. In some cases, cystic spaces are lined by an eosinophilic, hyaline membrane with pseudopapillary luminal projections ( membranous fat necrosis ) ( Fig. 13.3C ) .
The majority of lipomas have chromosomal aberrations with an increase in prevalence with increasing patient age. There are essentially three major subgroups of cytogenetic aberrations. Approximately two-thirds of tumors with an abnormal karyotype have 12q13-15 aberrations. Although 12q13-15 can combine with many different bands in virtually all chromosomes, the most common is a t(3;12)(q27-28;q13-15), found in approximately 20% of cases with an aberration of 12q13-15. Less than 10% of cases with 12q13-15 aberrations involve 1p36, 1p32-34, 2p22-24, 2q35-37, 5q33, 11q13, and 12p11-12, among others.
Approximately one-third of lipomas with an abnormal karyotype do not harbor aberrations of 12q13-15. Of these, the most commonly involved loci include 6p21-23, 13q11-12, and 12q22-24. The only recurrent translocation involving 6p21-23 is a t(3;6)(q27-28;p21-23). Various combinations can occur in the same tumor, including simultaneous 13q11-12 and 6p21-23 rearrangements or 13q11-12 and 12q13-15 rearrangements, but aberrations of 6p and 12q rarely occur together.
At the molecular level, the HMGA2 gene, which encodes for a member of the high-mobility group of proteins and is located on 12q15, plays a central role in the pathogenesis of lipomas. The t(3;12) results in a fusion of HMGA2 on 12q15 with LPP on 3q27-28. Aberrations of 6p21-23 involve the HMGA1 gene. Monoclonal antibodies to HMGA2 and HMGA1 have been developed, and immunoreactivity with these antibodies was found to correlate very well with cytogenetic alterations.
Lipomas are completely benign, but they may recur locally (>5%). Previous reports of malignant change predate the MDM2 era and likely represent dedifferentiation of a well-differentiated liposarcoma, in which the diagnostic cells were not present. Deep lipomas have a greater tendency to recur, presumably because of the increased difficulty for complete surgical removal.
Aside from the relatively small number of patients in whom an increased familial incidence of lipomas can be demonstrated, little is known about the pathogenesis of these tumors. Certainly, lipomas are more common in obese than in slender persons and perhaps, as a consequence, are more frequently encountered in patients older than 45. An increased incidence of lipomas is also claimed for diabetic patients and those with elevated serum cholesterol. Perhaps due to a local effect on metabolism, lipomas have been reported at the site of insulin injections. Trauma or irradiation may lead to overgrowth of fat indistinguishable from a lipoma ( posttraumatic pseudolipoma ). In particular, such lesions, often exceeding 10 cm in diameter, have been observed to develop secondary to blunt, bruising injuries, often preceded by a large hematoma.
Approximately 5% of all patients with lipomas have multiple tumors that are grossly and microscopically indistinguishable from solitary lipomas. The term lipomatosis has been used to describe this scenario, but it is preferred that this term be used to describe a diffuse overgrowth of mature adipose tissue (described later in this chapter).
Multiple lipomas vary in number from a few to several hundred lesions, and they occur predominantly in the upper half of the body, with a predilection for the back, shoulder, and upper arms. In some cases the lipomas are arranged in a symmetric distribution, with a slight predilection for the extensor surfaces of the extremities. They are about three times as common in men than in women. Most have their onset during the fifth and sixth decades, although occasional lesions appear as early as puberty. There is a definite hereditary predisposition in about one-third of patients with this condition ( familial multiple lipomas ). Most cases seem to be inherited in an autosomal dominant manner.
The question of a relationship between multiple lipomas and neurofibromatosis has been raised repeatedly in the literature, but there is no convincing proof of this association. However, there are patients who have multiple lipomas and multiple café au lait macules without neurofibromas ( Legius syndrome ).
There are several syndromes with multiple lipomatous lesions. Bannayan-Zonana syndrome is characterized by the congenital association of multiple lipomas (including lipomatosis of the thoracic and abdominal cavity in some cases), hemangiomas, and macrocephaly. Cowden syndrome consists of multiple lipomas and hemangiomas associated with goiter and lichenoid, papular, and papillomatous lesions of the skin and mucosae. Mutations in the PTEN gene have been identified in both these inherited hamartoma syndromes. Fröhlich syndrome , also known as prune-belly syndrome , is defined by multiple lipomas, obesity, and sexual infantilism. Proteus syndrome is marked by multiple lipomatous lesions, including pelvic lipomatosis, fibroplasia of the feet and hands, skeletal hypertrophy, exostoses and scoliosis, and various pigmented lesions of the skin.
Angiolipoma occurs chiefly as a subcutaneous nodule in young adults, often making its first appearance when the patient is in the late teens or early 20s; it is rare in children and in patients older than 50 (unlike solitary or multiple subcutaneous lipomas). It also is more common in males, and about 5% of cases are familial. The forearm is by far the most common site; almost two-thirds of all angiolipomas are found in this location. Next in frequency are the trunk and upper arm. As with all lipomas, it seldom occurs in the face, scalp, hands, and feet. Spinal angiolipoma is a specific entity that should be distinguished from cutaneous angiolipoma . In addition, intramuscular hemangioma, sometimes referred to as infiltrating angiolipoma , is distinct from cutaneous angiolipoma. Interestingly, angiolipomas are detected more frequently in the vicinity of the breast, presumably as a result of the increased use of mammography.
Multiple angiolipomas are much more common than solitary ones and account for about two-thirds of all angiolipomas. Characteristically, angiolipomas are tender to painful (often on touch only or palpation), particularly during the initial growth period; frequently, pain becomes less severe or ceases entirely when the tumor reaches its final size, which is rarely more than 2 cm. There seems to be no correlation between the degree of vascularity and the occurrence or intensity of pain, and the pain is not intensified by heat, cold, or venous occlusion.
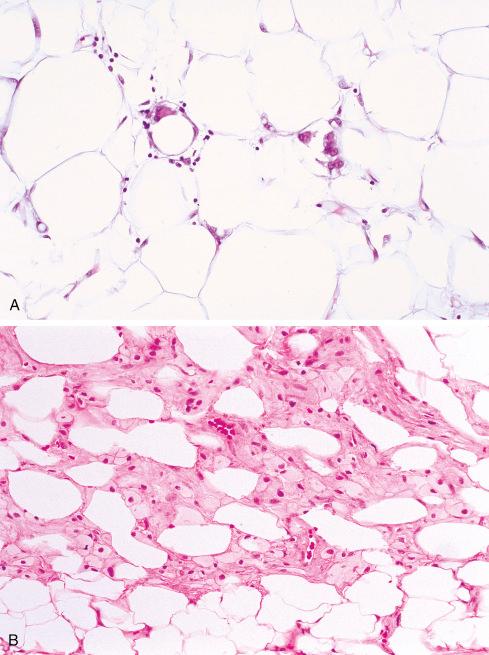
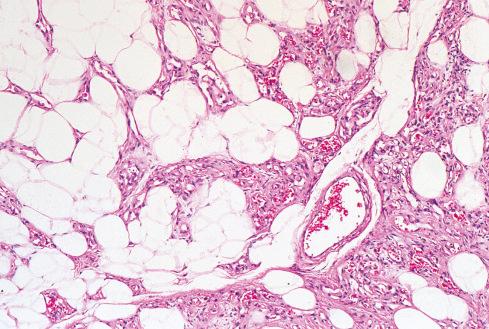
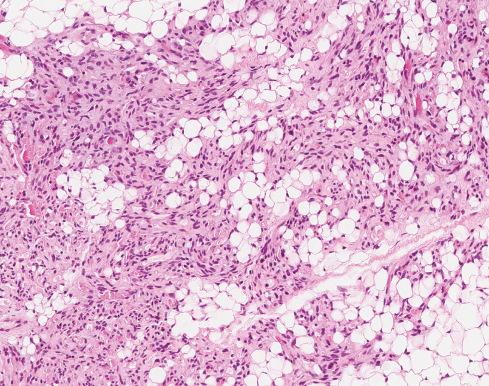
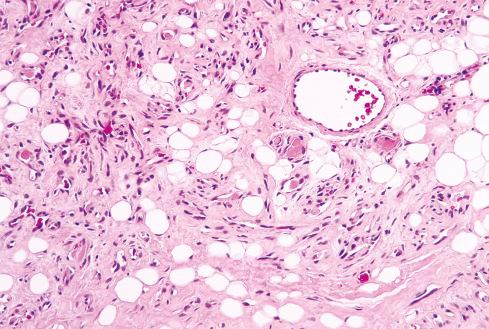
Angiolipomas are always located in the subcutis, where they present as encapsulated yellow nodules with a more or less pronounced reddish tinge. They consist of mature fat cells separated by a branching network of small vessels ( Fig. 13.4 ); the proportion of fatty tissue and vascular channels varies, but usually the vascularity is more prominent in the subcapsular areas ( Figs. 13.5 and 13.6 ). Late forms of this tumor frequently undergo perivascular and interstitial fibrosis. Characteristically, the vascular channels contain fibrin thrombi ( Fig. 13.7 ), a feature that is absent in ordinary lipomas. Mast cells are often conspicuous, another feature that distinguishes this tumor from the usual lipoma. Some examples are highly cellular and composed almost entirely of vascular channels ( cellular angiolipoma ), which can cause concern for a more ominous vascular lesion when they arise in the vicinity of the breast ( Fig. 13.8 ).
Unlike ordinary lipomas, which usually have karyotypic abnormalities involving 12q, 6p, and 13q (described previously), most angiolipomas show a normal karyotype. Hemangiomas also usually have a normal karyotype, which suggests that the vascular component is the primary proliferation. Using whole exome and ultradeep sequencing, Hofvander et al. recently showed that most angiolipomas contain mutations in the PRKD2 (protein kinase D2) gene. Expression of PRKD2 is important for angiogenesis, and altered expression of this gene in the adipocytes of angiolipoma is hypothesized to result in the characteristic vascular proliferation.
The differential diagnosis of this lesion in part depends on the density of vessels. The hypovascular lesions may be difficult to distinguish from ordinary lipomas , although the identification of microthrombi allows this distinction. Intramuscular hemangioma , at one time referred to as cellular or infiltrating angiolipoma , should not be difficult to distinguish from the more superficially located angiolipoma; despite similarities in name, the latter can be correctly diagnosed if attention is paid to the encapsulation of the lesion, the presence of microthrombi, and the small size, multiplicity, and subcutaneous location of the lesion. Cellular angiolipoma may be difficult to distinguish from Kaposi sarcoma (KS). Like cellular angiolipoma, KS can be found as multiple subcutaneous nodules in young men. However, KS has slitlike vascular spaces and periodic acid–Schiff (PAS)–positive globules in the cytoplasm of some cells, and it lacks microthrombi. Moreover, this lesion is characterized by immunoreactivity for human herpesvirus 8 (HHV8) LANA protein.
Angiolipomas are benign and virtually never recur. There is no evidence that these lesions ever undergo malignant transformation.
Myolipoma is a rare variant of lipoma marked by the proliferation of mature fat and mature smooth muscle tissue. The alternate term extrauterine lipoleiomyoma may also be used, but the preferred term is myolipoma because the former implies some relationship to uterine smooth muscle tumors. The tumor occurs in adults, most often during the fifth and sixth decades of life, with a striking predilection for women. In the large study by Fukushima et al., 32 of 34 patients were women. Myolipoma is most often found in the retroperitoneum, abdomen, pelvis, inguinal region, or abdominal wall. The extremities may also be involved, usually as a subcutaneous mass that can also involve the superficial muscular fascia. Most patients present with a painless mass, but in some cases the tumor is found incidentally because of its propensity to arise in deep locations. Deep-seated tumors are often quite large, obtaining an average size of 15 cm, whereas subcutaneous lesions tend to be much smaller.
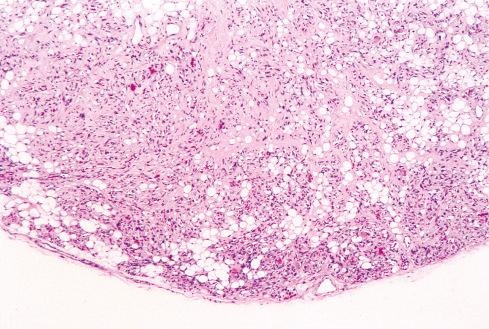
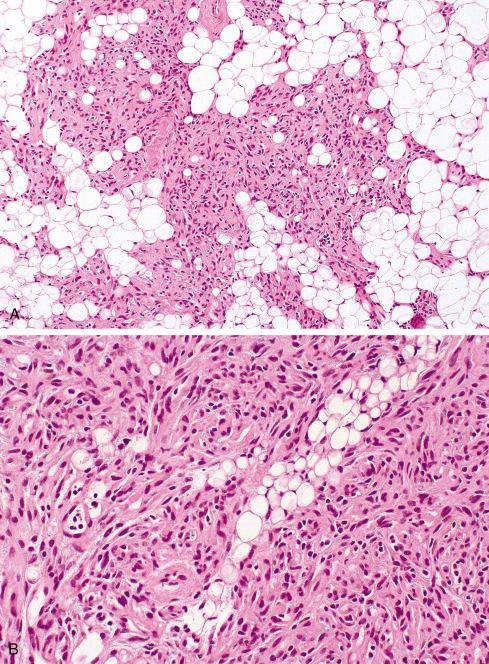
Grossly, the tumors are completely or partially encapsulated with a glistening, yellow-white cut surface; tumors with a prominent smooth muscle component have large areas of white or gray firm tissue with a whorled appearance. Histologically, myolipoma consists of a variable admixture of mature adipose tissue and bundles or sheets of well-differentiated smooth muscle, both of which lack nuclear atypia ( Fig. 13.9 ). Generally, the smooth muscle component is regularly interspersed with the adipose tissue, imparting a sievelike appearance at low magnification. The smooth muscle bundles are typically arranged in short interweaving fascicles and are characterized by cytologically bland oval nuclei with longitudinally oriented, deeply eosinophilic fibrillar cytoplasm. The adipose tissue component is entirely mature and lacks floretlike giant cells or lipoblasts. Some lesions have prominent stromal sclerosis and chronic inflammation; unusual features include round cell morphology, metaplastic bone or cartilage, and hemosiderin deposition.
The smooth muscle element stains strongly for smooth muscle actin (SMA) and desmin ( Fig. 13.10 ), and most show strong nuclear estrogen receptor positivity. In several cases studied cytogenetically, aberrations of the HMGA2 gene at 12q14-15 have been noted, which is not surprising since this gene is often rearranged in other lipomatous and smooth muscle tumors. In the Fukushima study, nuclear positivity for HMGA2 was noted in 15 of 25 cases (60%).
The differential diagnosis includes spindle cell lipoma, angiolipoma, angiomyolipoma, leiomyoma with fatty degeneration, and dedifferentiated liposarcoma. Spindle cell lipoma is composed of cytologically bland, spindle-shaped cells that express CD34 but not smooth muscle markers. Furthermore, spindle cell lipoma is exceedingly rare in the retroperitoneum, abdomen, and pelvis. Angiomyolipoma (a member of the PEComa family) often presents as a large retroperitoneal mass, as does myolipoma. It differs from myolipoma by the presence of medium-sized arteries with thick muscular walls, as well as epithelioid smooth muscle cells that are immunoreactive for melanocytic markers. Unlike angiomyolipoma, myolipoma is not associated with tuberous sclerosis. Leiomyoma with fatty degeneration lacks the regular distribution of fat that is present in myolipoma. Also, fatty degeneration of smooth muscle tumors of soft tissue is rare. Dedifferentiated liposarcoma can be distinguished from myolipoma by the presence of atypical hyperchromatic cells in the adipocytic component and cytologic atypia with mitotic activity in the dedifferentiated component. Rarely, well-differentiated liposarcoma can show heterologous myoid differentiation.
Myolipoma, despite its frequently large size and occurrence in deep soft tissue locations, is a benign neoplasm, with no reported recurrence or metastasis.
Chondroid lipoma is a rare, benign fatty tumor found in the subcutaneous tissue or deeper soft tissues, predominantly in the limbs and limb girdles of adult women. Although it is clinically benign, chondroid lipoma is another example of a pseudosarcoma in that it may be mistaken for a myxoid liposarcoma or chondrosarcoma. Although first recognized as a distinct entity in 1993 by Meis and Enzinger, it was probably first described by Chan et al., as an “extraskeletal chondroma with lipoblast-like cells.”
Although the age range is broad, most patients are in the third or fourth decade of life, and there is a striking predilection for women. In the largest series to date from the Armed Forces Institute of Pathology (AFIP) (20 cases), there were 16 females and 4 males ranging in age from 14 to 70 years (median: 35). Most patients present with a slowly growing painless mass that is often present for several years before excision. This lesion most frequently arises in the proximal extremity or limb girdle. Less common sites include the distal extremities, trunk, and head/neck region, especially the oral cavity. Radiologic studies show a heterogeneous soft tissue mass that has features different from typical lipoma, but not distinctive enough to be diagnostic. The diagnosis can be suggested by fine-needle aspiration in the hands of a skilled cytopathologist with some experience with this rare tumor.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here