Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
To the obstetrician-gynecologist, the ovarian examination is a fundamental part of the gynecologic evaluation and, depending on the age of the patient and other risk factors, ovarian enlargement triggers a series of investigative procedures. The surgical pathologist examines the ovarian specimen for several reasons, including to confirm or exclude pathology when the clinical impression is an ovarian abnormality or to examine the ovary for completeness when the uterus and adnexa are removed for other disease. Another possibility is prophylactic oophorectomy in women with a family history of ovarian cancer or inherited mutation in a BRCA-1 or BRCA-2 gene (see Chapter 24 ). To perform the examination under any of these circumstances, the pathologist must have a working understanding of the normal ovarian anatomy and the range of findings seen in the age group under study.
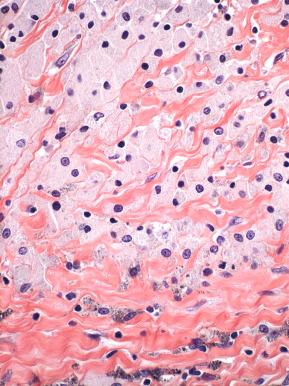
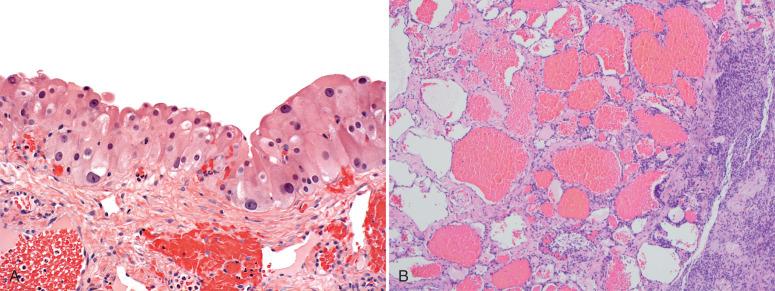
The adult ovary has three components: the cortex, the subcortical medulla, and the hilus. The cortex of the ovary is subdivided into the superficial epithelium and its underlying stroma ( Figs. 22.1 and 22.2 ). The ovarian surface epithelium (OSE) is composed of a simple lining of modified mesothelial cells, which are cuboidal to columnar cells with a low nuclear/cytoplasmic (N/C) ratio, inconspicuous nucleoli, and a moderate amount of pale cytoplasm ( Fig. 22.3 ). The cells lining the ovarian surface are ultrastructurally related to peritoneal mesothelial cells, including the presence of microvilli, although they tend to be cuboidal when compared with the flattened peritoneal mesothelium. The morphologic and immunophenotypic features of cellular proliferations seen on the ovarian surface are identical to those seen elsewhere (see Chapter 23 ). In brief, immunohistochemical studies have revealed this epithelium to be positive for cytokeratins, Ber-EP4, and hormone receptors (estrogen and progesterone). The OSE lies on a basement membrane that is normally inconspicuous. The OSE may even be absent and exhibit reactive atypia, with nuclear enlargement, hyperchromasia, and prominent nucleoli. The importance of the OSE lies in its controversial connection to ovarian carcinogenesis, via metaplastic transformation to an epithelial phenotype. This is discussed in greater detail in Chapter 24 . Otherwise, it is involved in the formation of adhesions and inclusion cysts.

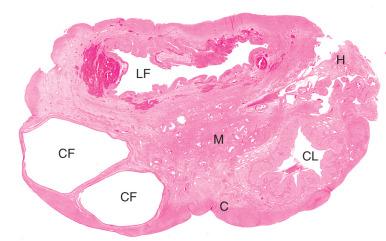
The underlying stroma is subdivided into the cortex and medulla. The cortex is composed of spindle-shaped cells, often arranged in parallel or alternating obliquely arranged bundles in a storiform pattern, with overlapping, tapered nuclei; inconspicuous nucleoli; and scant cytoplasm, with a variable amount of stromal collagen. Not surprisingly, these cells are positive for intermediate filament markers, such as vimentin and α-smooth muscle actin. The unique attribute of ovarian cortical stroma is the propensity to respond to pituitary or pregnancy hormones, as is discussed later. Oocytes, Graafian follicles, cystic and atretic follicles, corpora lutea, and corpora albicantia are commonly present in various stages of growth and involution in the cortex during reproductive life.
The medulla is composed principally of larger vessels and merges with the hilus. In the reproductive-age ovary, the distinction between cortex and medulla is subtle because of the abundance of cortical stroma. End-stage corpora lutea (alternatively, corpora albicantia) are often situated at the interface of the cortex/medulla. After menopause, when the cortex contracts, the medulla stands out sharply in relief by the presence of corpora albicantia that have not been resorbed.
The ovarian hilum is the anatomic site through which blood vessels (ovarian artery and vein) gain access to the ovary and site of attachment of the broad ligament. Embedded within its substance, which is composed of fibroconnective tissue, there are two basic structures: hilar cells and rete ovarii. The latter are mesonephric remnants and are described later.
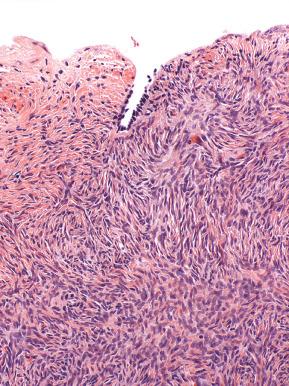
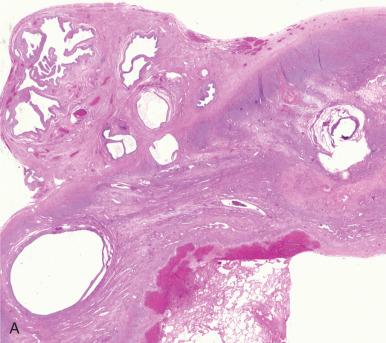
Periovarian adhesions are fibrous connections that form between the ovary and other organs or peritoneum ( Fig. 22.4 ). These fibrous bands form as a response to intrapelvic injuries, such as bleeding at a site of endometriosis, infection, and abdominal or pelvic surgery. The major consequence of adhesion formation is its association with chronic pelvic pain. The relationship of adhesions to pain continues to be controversial. Although studies have associated various forms of adhesions with different levels of pain, more recent studies have shown no relationship between pelvic pain and adhesions where adhesiolysis and diagnostic laparoscopy provide equivalent relief of pain. Histologically, adhesions are characteristically hypocellular bands of tissue with various amounts of collagen deposition on the surface of the ovarian cortex. Interestingly, histologic and immunohistochemical study of peritoneal adhesions has revealed the presence of both myelinated and nonmyelinated nerve fibers but was not related to the presence or absence of chronic pelvic pain.
The differential diagnosis of adhesions includes few entities other than cystic mesothelioma, which conceivably could mimic cystic adhesions. Cystic mesothelioma is a benign recurrent lesion that is characterized by a macroscopic multicystic mass in which the cystic spaces are usually lined by conspicuous mesothelial cells separated by a thick fibrous septae. In contrast, cystic adhesions are small and focal and are composed of delicate fibrous strands. Cystic mesothelioma is discussed in greater detail in Chapter 23 .
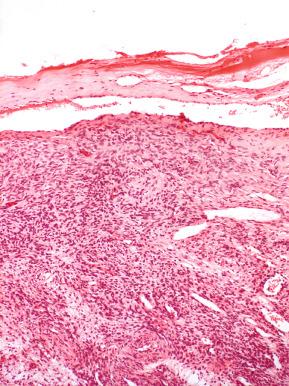
Mesothelial proliferations of the ovarian surface include the same spectrum of mesothelial changes seen in other mesothelial-lined surfaces, such as peritoneum, pleura, and pericardium, and usually occur in response to pelvic inflammation; local trauma, including torsion or infarction; endometriosis; and neoplasia. The reactive mesothelial response includes mesothelial hyperplasia, mesothelial-inclusion cysts, and infiltration by a variable number of macrophages, the latter most conspicuous in endometriosis (see Fig. 22.4 ). Another common, presumably reactive process is micropapillomatosis. Micropapillomatosis is incidental and self-limiting and consists of small finger-like excrescences composed of a central fibrous core and lined by OSE. Other than the papillary architecture, micropapillomatosis is easily distinguished from surface tumors of serous epithelial origin. The latter are composed of irregular papillae with epithelial differentiation, in contrast to the mesothelial lining of micropapillomatosis ( Fig. 22.5 ).
Rarer entities are benign papillary mesothelioma and malignant mesothelioma. These are discussed in Chapter 23 .
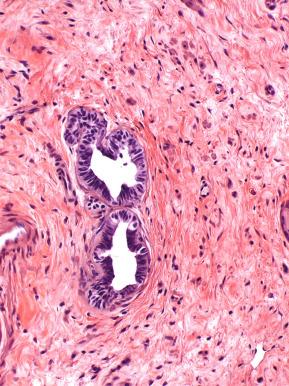
Endosalpingiosis of the ovary is defined by epithelial cysts or glandlike structures containing ciliated epithelium. The term endosalpingiosis in this site is best reserved for those epithelial structures that contain not only cilia but also a pseudostratified epithelium that closely resembles fallopian tube mucosa, with or without supporting stroma typical of that seen in tubal plica ( Fig. 22.6 ). However, if tubal stroma is not present, the term müllerian (cortical) inclusion cyst is preferred, inasmuch as they conceivably could originate from the endometrium or müllerian metaplasia of the mesothelium.
Cortical inclusion cysts (CICs) originate from the entrapment of epithelium within the cortex of the ovary. Traditionally this epithelium was presumed to be derived via müllerian metaplasia of the OSE, but currently a more popular explanation is that the epithelium develops via transporting of tubal or endometrial epithelium to the ovarian surface. The epithelium lining these CICs may be flat to cuboidal nonciliated epithelium like that seen on the surface of the ovary and more in keeping with mesothelium, or it may exhibit cilia similar to that seen in endosalpingiosis ( Fig. 22.7 ). The mechanisms by which CICs find their way into the ovarian cortex include entrapment within surface adhesions, infolding of surface epithelium into the cortex with CICs developing when the folds of the cortex fuse, and repair of ovulation sites with surface epithelium growing into atretic follicles.
Parenthetically, it is noteworthy that multiple CICs have been found in Birt-Hogg-Dubé syndrome. This is a rare autosomal dominant disorder characterized by a variety of tumors or lesions, including hamartomas, lung, and oncocytic cysts. The responsible gene (BHD) is highly expressed in the ovary. Although occasional cases with multiple CICs are highly unlikely to have this syndrome, such coincidences suggest that we still know very little about the mechanism for CIC development.
CICs are considered benign and are found in the majority of ovaries from postmenopausal women. The attention they receive results from their possible role in the pathogenesis of ovarian adenocarcinomas. This concept continues to evolve as the relative contributions of the fallopian tube (see Chapter 21 ), endometrium (see Chapter 19 ), and peritoneum (see Chapter 23 ), together with direct transformation of mesothelium to epithelium, continue to be resolved. CICs and related müllerian cysts in the paraovarian, paratubal, and hilar regions exhibit a wide range of epithelial metaplasias, including mucinous, endometrioid, and transitional (Walthard cell rests) type, corresponding to the malignant phenotypes seen in epithelial tumors. The role of CICs in ovarian carcinomas is discussed further in Chapters 24 and 25 .
Larger cysts of one or more centimeters in diameter may form on the surface of the ovary, within the cortex, or even hilus. The origin of these paraovarian, intracortical, or intrahilar cysts is presumably similar to that of CICs. The lining of these cysts ranges from flat to cuboidal to pseudostratified columnar. Cysts lined by flat or cuboidal epithelium are termed simple or mesothelial cysts ( Fig. 22.8 ). Those with a distinct epithelial lining are classified as müllerian cysts or, if accompanied by a dense fibrous wall, unilocular serous cystadenomas .
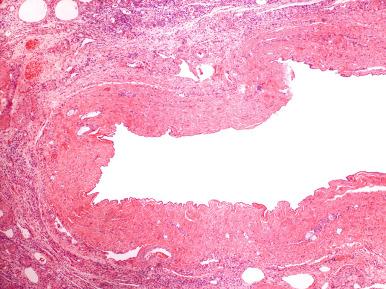
The differential diagnosis of simple cysts includes atretic follicles (residual theca lining cells), senescent endometriosis (hemosiderin or rare plasma cells), cystadenomas (dense fibrous capsule and pseudostratified ciliated [serous] epithelium), adhesed hydrosalpinx (smooth muscle wall), and paratubal cyst (continuity with the adnexa).
Follicle development is a dynamic process that goes on continuously, not only in the reproductive-age ovary but also to a lesser degree before menarche. Moreover, the preparation of follicles for eventual recruitment and selection and ovulation occurs over an extended period of time and is not confined within the time frame of a single cycle. Accordingly, follicles that are not selected may persist for a period of time prior to atresia. For this reason, the pathologist should expect to see a range of follicle development in otherwise normal ovaries removed incidentally for other reproductive tract abnormalities.
The development of germ cells of the ovary and their embryogenesis are discussed in Chapter 1 . In the adult ovary, follicles are embedded within the cortical stroma of the ovary, are classified according to their evolutionary stage, and include the following ( Fig. 22.9 ).
The primordial follicles are present at birth and composed of a primary oocyte and surrounded by a flattened layer of granulosa cells (see Fig. 22.9A ). Granulosa cell function is minimally dependent on gonadotropins at this stage and is primarily mediated by paracrine signaling within the oocyte.
As the oocyte matures, the granulosa cells increase in size, becoming mitotically active, and form the primary follicle (see Fig. 22.9A ). Fibroblast-like precursor cells are recruited from adjacent stroma and surround the developing follicle.
With subsequent stratification and expansion (2 to 5 mm thickness) of the granulosa cells layer, a secondary (preantral) follicle is formed (see Fig. 22.9B ). The recruited fibroblast-like precursor cells differentiate into theca cells. Granulosa cells acquire follicle-stimulating hormone (FSH) receptors.
The granulosa cells forming the secondary follicle produce large amounts of interstitial fluid, which accumulates and forms an antrum in which the enlarged, mature oocytes reside (Graafian follicle) (see Fig. 22.9C ).
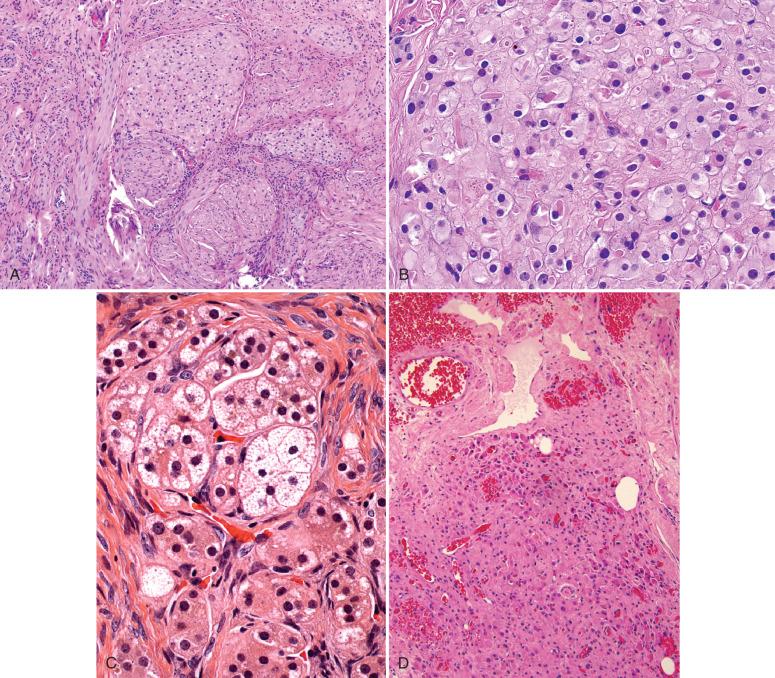
Surrounding the granulosa cell layer, theca cells differentiate into an inner (theca interna) and an outer (theca externa) layer. Cells of the theca interna are necessary for ovarian androgen production, whereas cells of the theca externa primarily provide structural support to the developing follicle and via smooth muscle-like function contribute to successful ovulation. This entire process is governed by FSH and luteinizing hormone (LH). Following ovulation, the antrum is filled with fibrin and debris, and it starts contracting to form the corpus luteum. Although a single Graafian follicle (usually) progresses to a corpus luteum, several other follicles may be present throughout the cycle, and the pathologist may encounter several follicles in various stages of development and atresia. Some may closely resemble preovulatory follicles, with expanded granulosa and theca cell layers; others will have lost most of their granulosa cells and be in a stage of involution (see Fig. 22.9D ). If ovulation does not take place, persistent follicle development can lead to an unopposed estrogen effect.
Cystic follicles are commonly encountered in the ovaries of reproductive-age women. They result from Graafian follicles that did not rupture and will eventually undergo reabsorption. Cystic follicles are usually asymptomatic or present with mild, vague pelvic pain. They can be solitary or multiple ( Fig. 22.10 ). Macroscopically, they appear as uniloculated cystic structures on the ovarian surface and cortex, with smooth walls and watery content. They are usually less than 10 mm in diameter.
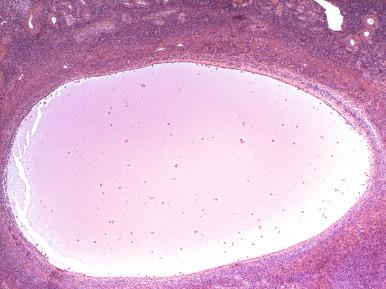
Cystic follicles vary in their appearance, presumably a function of their age. Some contain a thick layer of partially luteinized granulosa and theca cells and may be mistaken for corpora lutea (see Fig. 22.9D ). Most are composed of a theca layer that is variably luteinized with depleted granulosa cells. Still others are lined by a single layer of luteinized cells, the origin of which are presumably theca. When follicles exceed 3 cm in diameter, they are termed follicular cysts (discussed later).
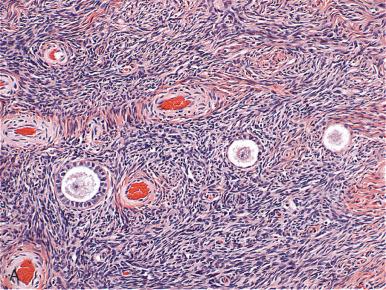
Atretic follicles are commonly present in the ovary and signify the end stage of follicle involution, cystic or otherwise. Early atretic follicles display a fibrotic rim beneath which the theca cells are slightly dispersed ( Fig. 22.11 ). As atresia progresses, the follicle space disappears, terminating in an indistinct oval to elliptical condensation of stroma with a central crease or slit-like remnant of the original lumen. Atretic follicles are particularly common in polycystic ovarian disease, a sign of increased follicle recruitment (discussed later).
The pathologist who routinely examines the ovary is unlikely to confuse follicles with neoplasia, or vice versa, but two pitfalls exist: one is common and one is rare:
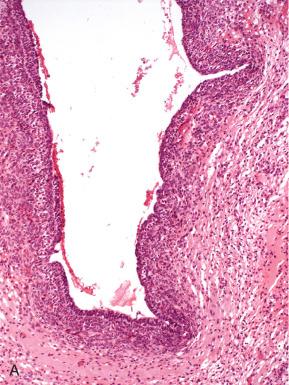
Tangentially sectioned theca externa may be misdiagnosed as a stromal neoplasm, particularly because the cells are plump in appearance and mitotically active. This pitfall is avoided by the pathologist familiar with this pattern, coupled with the absence of a discrete cortical mass ( Fig. 22.12A and B ).
Cystic follicles with lush lining may be confused with cystic granulosa cell tumors. The latter are usually multicystic and lined by irregularly arranged neoplastic granulosa cells (see Fig. 22.12C ).
Corpora lutea are normal ovarian structures that in the normal cycle are the consequence of ruptured follicles. Macroscopically, these structures are bright yellow masses (recent corpus luteum) or white masses (degenerating corpus luteum) with a small cystic center ( Fig. 22.13 ). A cystic or hemorrhagic appearance is common, leading to the common designation of cystic or hemorrhagic corpus luteum. These two characteristics typify most corpora lutea and are not necessary qualifiers; simply qualifying corpora lutea as recent or degenerating will suffice.

The histologic hallmark of a recent corpus luteum is prominent luteinization of the granulosa cell layers and is synonymous with a “granulosa-lutein cyst.” The plump granulosa cells are arranged in a cerebriform convoluted mass, with internal folds, the interstices of which contain smaller numbers of smaller luteinized theca cells ( Fig. 22.14 ). After ovulation, granulosa cells produce progesterone, and the theca cells continue to produce estrogen throughout the cycle. With the onset of menstruation, the granulosa and theca cells undergo apoptosis, with an abrupt drop in progesterone and estrogen production; and by the fifth day of the new cycle (late menstrual phase), they have lost their distinct architecture, because the cells become smaller and admixed with mononuclear cells. Within two cycles, the degenerated corpus luteum has contracted to a fraction of its size, the luteal cells are reduced to small rounded nuclei with scant cytoplasm, and the structure is recognized principally by its architectural similarity to the original corpus luteum ( Fig. 22.15 ).

Diagnostic pitfalls associated with corpora lutea include the following: (1) clinical interpretation as an adnexal mass; (2) rarely, misdiagnosis as an ovarian pregnancy during exploratory laparotomy for ectopic pregnancy; and (3) confusion with endometriosis, specifically when the latter consists of a pseudoxanthomatous pseudocyst. The diagnostic confusion stems from interpreting the foamy macrophages lining the pseudocyst as granulosa-lutein cells. The characteristic appearance of foamy histiocytes and the absence of a second theca cell layer characterize the xanthomatous pseudocyst (discussed later) ( Fig. 22.16 ).
The most common complication of corpus luteum is massive hemorrhage, the greatest risk factor being anticoagulant therapy or other coagulation disturbance. Some can be managed effectively by rapid reversal of the anticoagulation; however, if the hemorrhage is severe, laparotomy, coagulation, or suturing of the bleeding site may be necessary. Rarely, oophorectomy is required. In one study, approximately one-third had recurrent hemorrhage when anticoagulation was resumed.
Wolffian remnants are embryologic mesonephric residues usually found in the round ligament and vaginal wall, but they can be encountered anywhere in the female genital tract, including the ovaries (see Chapter 1 ). They are usually incidental microscopic findings. A single layer of cuboidal cells with round nuclei, inconspicuous nucleoli, and scant cytoplasm lines the glands and ducts of one to several glands. The glands are situated at oblique angles to one another and contain eosinophilic intraluminal secretions ( Fig. 22.17 ).
Recognition of Wolffian remnants is important; in certain settings, they may be misclassified as neoplastic. However, the nuclei are generally uniform in appearance and are oriented vertically (see Chapter 27 ). The major differential diagnosis is with metastatic carcinoma. Nuclear atypia and mitoses are usually absent and aid in the diagnosis.
Hilus cells are the ovarian counterparts of testicular Leydig cells (see Chapter 1 ). They are typically found singly or in nests within the hilum of the ovary, present in variable density in the connective tissue spaces between the vessels. In most instances, the cells are present in small groups and require a careful search. However, once found, the cells are distinct, with a moderate amount of cytoplasm, a polygonal shape, round central nuclei, small nucleoli, and abundant eosinophilic cytoplasm. Like Leydig cells, hilus cells often contain small round to oval intracytoplasmic droplets ( Fig. 22.18A and B ). Careful inspection will occasionally disclose crystalloids of Reinke (see Fig. 22.18C ). Hilus cell heterotopia has been reported in subcapsular ovarian cortex, as well as the fallopian tube.
Hilus cells are hormone responsive and become accentuated during pregnancy and at menopause, two conditions associated with increased gonadotropin secretion (discussed later). In some instances, they may appear hyperplastic (see Fig. 22.18D ), particularly when accompanied by stromal hyperthecosis. However, they are easily distinguished from mass-forming (Hilar cell tumor) lesions. Their importance lies in the latter, which arise from them, and their close resemblance to and occasional misclassification as lobular carcinoma of the breast.
The cells of the ovarian cortex and hilum are uniquely responsive to circulating gonadotropins and steroid hormones, which, apart from the corpus luteum, influence the submesothelial mesenchyme (deciduosis), stromal, follicular, and hilus cells. This process is characterized by continued follicle development and regression, upon which a prominent luteinized response in these gonadotropin-sensitive cells is superimposed. The result is general regression of the granulosa cells, expansion and luteinization of the theca interna and interfollicular stromal cells, and coincident hilus cell hyperplasia. The spectrum of pregnancy-related alterations can occasionally cause diagnostic confusion ( Table 22.1 ). The extent of the process varies widely and gives rise to a continuum of conditions discussed later.
| Finding | Misclassification |
|---|---|
| Luteoma | Metastatic carcinoma |
| Hyperreactio luteinalis (HRL) | Cystadenoma |
| Deciduosis | Mesenchymal tumor |
| Solitary cyst | Clear cell carcinoma |
| Decidualized endometrioma | Corpus luteum |
| Malignancy (on ultrasound) | |
| Malignancy (on frozen section) |
The corpus luteum of pregnancy is simply the persistence of the corpus luteum that accompanied conception. It is most prominent early in pregnancy and is critical to sustaining the gestation in the first 8 weeks, during which the maximum progesterone secretion occurs. As pregnancy evolves, the corpus luteum gradually regresses and plays a negligible role in the final two trimesters. Two histologic features characterize the corpus luteum of early pregnancy. The first is enlargement of the granulosa lutein cells. The second is the presence of cytoplasmic vacuoles and droplets of variable size, which persist throughout pregnancy ( Fig. 22.19 ).
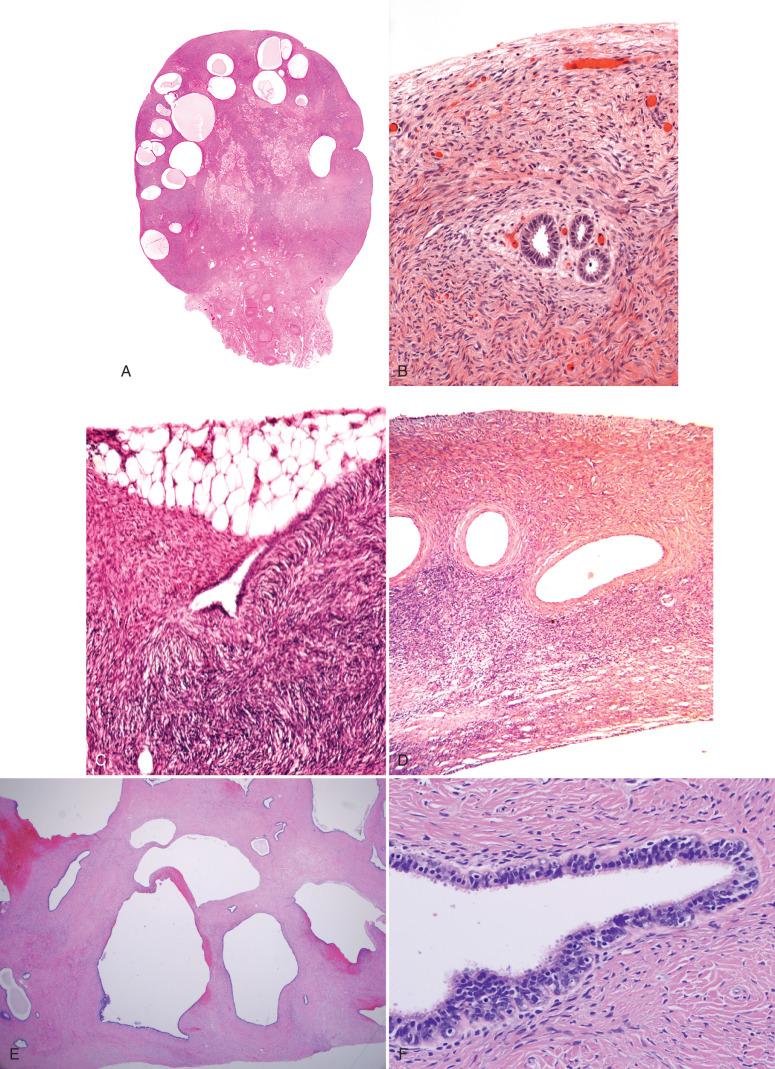
Ovaries removed incidentally at the time of delivery display one or more of the following, collectively defined as theca-lutein hyperplasia of pregnancy (TLHP). This consists of variable numbers of follicles containing an attenuated granulosa cell layer and an expanded luteinized theca ( Fig. 22.20 ). This expansion of the theca is often asymmetrical, producing elliptical aggregates of theca cells that merge with the ovarian stroma. The latter frequently contains scattered luteinized stromal cells singly or in clusters, cords, or loosely arranged groups. Coincident expansion of the hilus cells may also be seen. This collective accentuation of luteinized cell growth is not unlike that seen in hyperthecosis (discussed later), although the pathogenesis is related to the production of chorionic gonadotropins and their effects on the ovary.
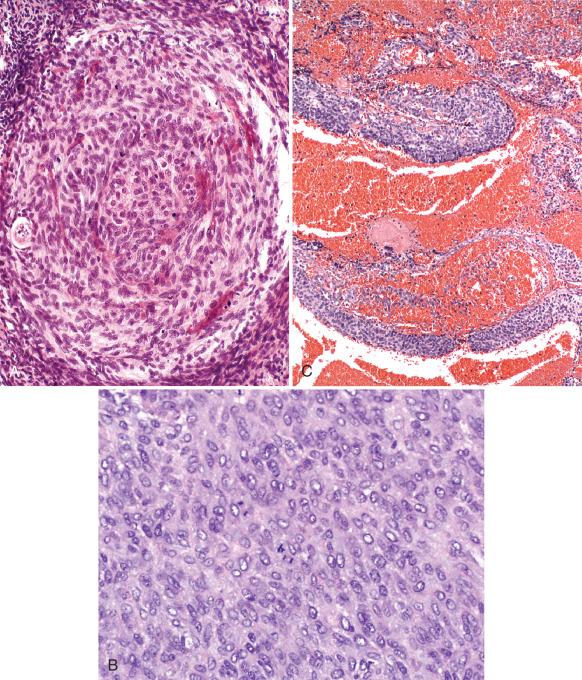
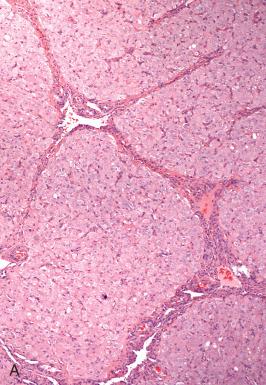
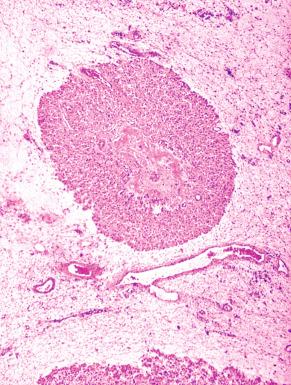
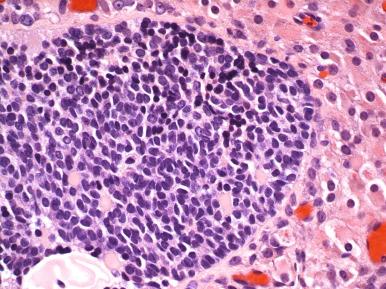
A more pronounced variation of theca-lutein hyperplasia is nodular theca-lutein hyperplasia of pregnancy (NTLHP) ( Fig. 22.21 ). NTLHP is characterized by conspicuous expansion of the follicular structures, which coalesce into confluent nodules. These nodules appear to be made up of theca interna, the follicle centers of which are often obliterated by the proliferation of the lining cells. The theca cells are cohesive but merge peripherally with luteinized cells that stream into the stroma. Whether the latter are derived from theca or stromal cells may be difficult to determine, but their more discohesive appearance and random distribution suggest a stromal origin.
The fate of the granulosa cells in these lesions varies. In most of the follicles undergoing replacement, the granulosa cells are inconspicuous. In others, the precise distinction between theca interna and granulosa cells may be difficult to ascertain. The pathologist may initially believe that he or she is witnessing a granulosa cell proliferation, only to realize that the expanding population of luteinized cells is the only layer present, in which case the logical conclusion is that the granulosa cells have involuted. In others, follicles with preserved, expanded, and partially luteinized granulosa cell hyperplasia are occasionally seen ( Fig. 22.22 ). More typically the granulosa cells are attenuated and inconspicuous; in some sites, they are incorporated into luminal fibrin. In the latter, the proliferating luteinized theca cells repopulate the follicle surface and residual granulosa cells are present in small linear groups or horizontally arranged tubular structures.
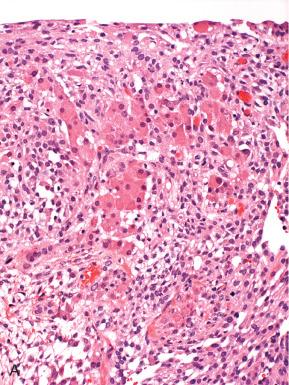
The more extreme form of NTLHP is pregnancy luteoma. As strictly defined, pregnancy luteomas are characterized by expansile solitary brown to yellow tumors that displace the ovarian parenchyma ( Fig. 22.23 ). These lesions differ from NTLHP by the greater extent of luteinized cell proliferation and plump, eosinophilic, and often vacuolated cells that resemble stromal luteomas or unclassified steroid cell tumors ( Fig. 22.24 ). Experts have traditionally argued that pregnancy luteoma is a more extreme variant of NTLHP and not a neoplasm, principally because of the tendency for these tumors to spontaneously regress following pregnancy. From a management perspective, this assumption is strongly encouraged, inasmuch as oophorectomy for such tumors should be avoided unless a period of postpartum observation has proven them to be persistent. However, because the hormonal environment that spawns these tumor-like lesions is similar to that seen at menopause (when other steroid-producing tumors develop), it is reasonable to assume that rare solitary luteomas of pregnancy are derived from a clonal population that has a growth advantage realized under the hormonal environment of pregnancy.

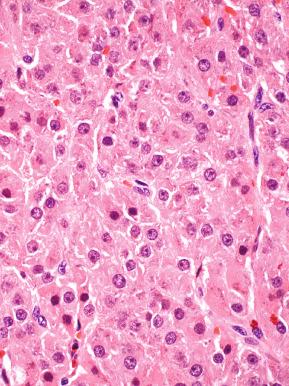
Most patients with pregnancy luteoma have a history of multiple pregnancies, and up to 80% of cases occur in black women. The vast majority of the cases are asymptomatic, although they can present with acute abdominal pain secondary to torsion, and the tumor-like mass is incidentally found during prenatal ultrasonographic examination, tubal ligation, or cesarean section. However, occasionally the mass may grow to a large size or is hormonally active, leading to virilization of the mother. Rarely, the elevated levels of testosterone may also affect female fetuses, which may also show signs of virilization at birth. Hormonal abnormalities in patients with “pregnancy luteoma” include elevated levels of testosterone, which is seen in most of the patients regardless of the symptomatology.
The differential diagnosis of NTLHP and pregnancy luteoma includes metastatic carcinoma, metastatic melanoma, and primary ovarian tumors (such as, luteinized thecoma), especially on gross examination of the resection specimen. Immunoperoxidase studies in association with a history of pregnancy are the most useful tools in making this differentiation. Carcinomas will be easily differentiated during microscopic examination. In addition, carcinomas will be positive for keratins and the pattern of staining for cytokeratins 7 and 20, in association with other markers (i.e., thyroid transcription factor-1 or CDX-2), can help in the localization of the primary tumor. Amelanotic malignant melanoma can be morphologically similar to luteoma of pregnancy. It is positive for S-100 protein and other melanocytic markers, such as HMB-45 and Melan-A. Luteoma of pregnancy may be positive for Melan-A and inhibin, but other epithelial and melanocytic markers are negative. As mentioned previously, the outcome of pregnancy luteoma is uneventful and the tumor-like mass typically regresses postpartum.
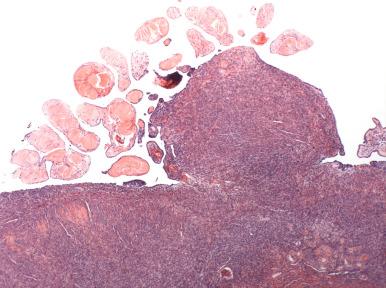
Hyperreactio luteinalis (HRL) is another pregnancy-related ovarian lesion in which numerous follicle cysts are the major manifestation rather than the luteinized thecal-stromal cell expansion of NTLHP ( Fig. 22.25 ). It is associated with physiologic and pathologic states of hyperstimulation of the ovaries, such as pregnancies (especially multiple pregnancies), gestational trophoblastic disease, and treatment for ovulation induction. In all of these conditions, ovarian exposure to high levels of endogenous or exogenous human chorionic gonadotropin (hCG) or increased sensitivity to hCG is present and is believed to be pivotal in the pathogenesis of this condition. In one series, most cases of HRL (approximately 70%) were identified in the third trimester or peripartum period. HRL may be associated with placental insufficiency based on the findings of one study.

Like other forms of TLHP, HRL may be clinically apparent as a palpable mass, encountered during cesarean section, or visualized during ultrasonography examination. Pelvic pain, torsion, or rupture of cysts with intrapelvic hhemorrhage can occur but are uncommon. In a smaller percentage of cases, virilization of the mother can be observed.
Grossly, the adnexa are characterized by bilateral cystic expansion of the ovaries by numerous small multiloculated thin-walled cysts (see Fig. 22.25 ). A layer of granulosa cells and a second layer of luteinized theca cells line the cystic cavities ( Fig. 22.26 ). Edema of the ovarian substance can be prominent. The principal exclusion is a cystic ovarian neoplasm. Microscopic examination allows immediate discrimination between these two conditions.

The natural history of this condition is postpartum regression of the cysts; however, this process of involution may take up to 6 months. When it is associated with hemorrhage or torsion, surgical removal may be necessary. However, the obstetrician should be aware of this benign condition, particularly in the settings of hydatidiform mole and twin pregnancy, and exercise discretion, particularly when faced with bilateral cystic ovaries.
Solitary luteinized follicle cyst is a benign condition that affects pregnant females or appears during puerperium, is self-limited in nature, and most often regresses spontaneously in the puerperium. In most cases, the cyst is an incidental finding during cesarean section or physical or ultrasonographic examination; however, its large dimension may cause an increase in the abdominal size. In the largest series, none of the patients showed hormonal deregulation.
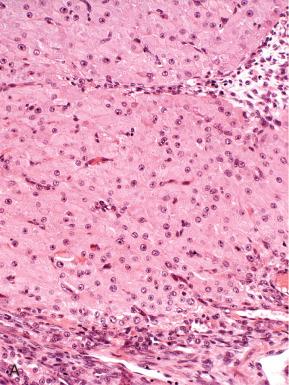
Solitary luteinized follicle cyst is a unilateral, uniloculated cystic mass filled with thin watery fluid. Its median size was 25 cm in one series. Microscopically, the cyst is lined by luteinized granulosa and theca cells, which show abundant eosinophilic, occasionally vacuolated, cytoplasm and large, hyperchromatic, focally pleomorphic nuclei ( Fig. 22.27A ). Mitoses are absent.
The differentiation between solitary luteinized follicle cyst and a cystic ovarian tumor can be difficult given the amount of nuclear atypia; however, the low N/C ratio, sporadic atypia, absence of mitotic activity, awareness of this entity, and clinical setting will minimize the risk of a misdiagnosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here