Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Assessment of erythrocyte, leukocyte, and platelet counts from manual and automated particle counters is central to the diagnosis and management of hematologic disease.
With few exceptions, manual methods have been replaced by automated hematology analyzers. The selection of analyzers is varied and voluminous enough to meet the needs of any hematology laboratory setting.
Hematology automation combined with sophisticated algorithms for data interpretation has led to dramatic improvement in the utility of automated analyzers in patient care. Newer instrumentation has progressed far beyond the screening tools of the past.
Examination of peripheral blood with bone marrow smear/biopsy represents the cornerstone of hematologic diagnosis. Bone marrow examination provides a semiquantitative and qualitative assessment of the state of hematopoiesis and aids in the diagnosis of several hereditary and acquired benign and malignant diseases.
Hematology includes the study of blood cells and coagulation. It encompasses analyses of the concentration, structure, and function of cells in blood; their precursors in the bone marrow; the chemical constituents of plasma or serum intimately linked with blood cell structure and function; and the function of platelets and proteins involved in blood coagulation. Advancement of molecular biological techniques and their increased use in hematology have led to the detection of several genetic mutations underlying the altered structure and function of cells and proteins that may result in hematologic disease.
Hemoglobin (Hb), the main component of the red blood cell (RBC), is a conjugated protein that serves as the vehicle for the transportation of oxygen (O 2 ) and carbon dioxide (CO 2 ). When fully saturated, each gram of Hb holds 1.34 mL of O 2 . The red cell mass of the adult contains approximately 600 g of Hb, capable of carrying 800 mL of O 2 . A molecule of Hb consists of two pairs of polypeptide chains (“globins”) and four prosthetic heme groups, each containing one atom of ferrous iron. Each heme group is precisely located in a pocket or fold of one of the polypeptide chains. Located near the surface of the molecule, the heme reversibly combines with one molecule of O 2 or CO 2 . The main function of Hb is to transport O 2 from the lungs, where O 2 tension is high, to the tissues, where it is low. At an O 2 tension of 100 mm Hg in the pulmonary capillaries, 95% to 98% of the Hb is combined with O 2 . In the tissues, where O 2 tension may be as low as 20 mm Hg, the O 2 readily dissociates from Hb; in this instance, less than 30% of the O 2 would remain combined with Hb.
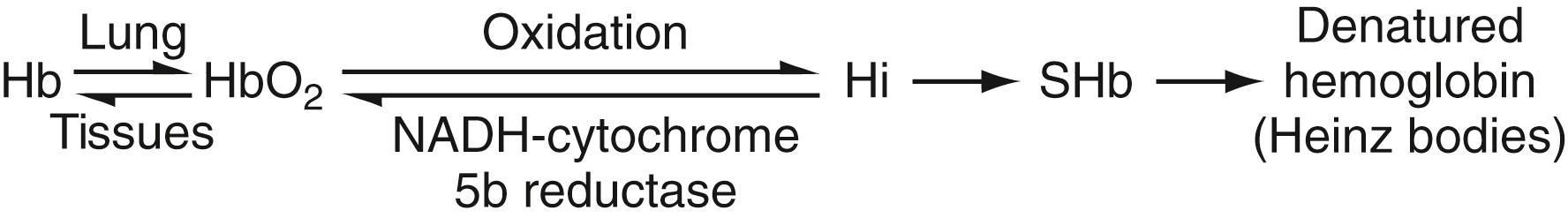
Reduced Hb is Hb with iron unassociated with O 2 . When each heme group is associated with one molecule of O 2 , the Hb is referred to as oxyhemoglobin (HbO 2 ). In both Hb and HbO 2 , iron remains in the ferrous state. When iron is oxidized to the ferric state, methemoglobin (hemiglobin [Hi]) is formed, and the molecule loses its capacity to carry O 2 or CO 2 .
Anemia is a decrease to below normal Hb concentration, erythrocyte count, or hematocrit (Hct). It is a very common condition and is frequently a complication of other diseases. Clinical diagnosis of anemia or of high Hb based on estimation of the color of the skin and of visible mucous membranes is highly unreliable. The correct estimation of Hb is important and is one of the routine tests performed on practically every patient.
Methemoglobin (Hi) is a derivative of Hb in which the ferrous iron is oxidized to the ferric state, resulting in the inability of Hi to combine reversibly with O 2 . The polypeptide chains are not altered. A normal individual has up to 1.5% methemoglobin. Methemoglobinemia will cause chocolate-brown discoloration of blood, cyanosis, and functional “anemia” if present in high enough concentrations. Cyanosis becomes obvious at a concentration of about 1.5 g Hi/dL (i.e., 10% of Hb). Comparable degrees of cyanosis will be caused by 5 g Hb/dL of blood, 1.5 g Hi/dL of blood, and 0.5 g sulfhemoglobin (SHb)/dL of blood. The degree of cyanosis, however, is not necessarily correlated with the concentration of Hi. A small amount of Hi is always being formed but is reduced by enzyme systems within the erythrocyte. The most important is the NADH (reducing agent derived from nicotinamide adenine dinucleotide)-dependent methemoglobin reductase system (NADH-cytochrome- b 5 reductase). Others, which may function mainly as reserve systems, are ascorbic acid, reduced glutathione, and reduced nicotinamide adenine dinucleotide phosphate (NADPH)–methemoglobin reductase. The latter requires a natural cofactor or an auto-oxidizable dye such as methylene blue for activity. NADPH is an essential cofactor for maintaining intracellular glutathione in the reduced state so that hemoglobin iron remains in the ferrous state.
Methemoglobinemia, an increased amount of Hi in the erythrocytes, may result from increased production of Hi or decreased NADH-cytochrome- b 5 reductase activity, and may be hereditary or acquired ( ). The hereditary form is divided into two major categories. In the first, methemoglobinemia is due to a decrease in the capacity of the erythrocyte to reduce the Hi that is constantly being formed back to Hb. This is most often due to NADH-cytochrome-b 5 reductase deficiency , which is inherited as an autosomal-recessive characteristic. The homozygote has methemoglobin levels of 10% to 50% and is cyanotic. Only occasionally is polycythemia present as a compensating mechanism. Hi concentrations of 10% to 25% may give no apparent symptoms; levels of 35% to 50% result in mild symptoms, such as exertional dyspnea and headaches; and levels exceeding 70% are probably lethal. Therapy with ascorbic acid or methylthioninium chloride (methylene blue) in this form of hereditary methemoglobinemia will reduce the level of Hi, the latter apparently by activation of the NADPH–methemoglobin reductase system. Heterozygotes have intermediate levels of NADH-cytochrome- b 5 reductase activity and normal blood levels of Hi. They may become cyanotic because of methemoglobinemia after exposure to oxidizing chemicals or drugs in amounts that will not affect normal individuals.
In the second major category of hereditary methemoglobinemia, the reducing systems within the erythrocyte are intact but the structure of the Hb molecule itself is abnormal. A genetically determined alteration in the amino acid composition of α- or β-globin chains may form a Hb molecule that has an enhanced tendency toward oxidation and a decreased propensity of the methemoglobin formed to be reduced back to Hb. Their principal consequence is asymptomatic cyanosis as a result of methemoglobinemia; they are designated as various forms of hemoglobin M (Hb M) . In six of the seven Hb M variants, tyrosine is substituted for histidine in the heme pocket of the proximal or distal globin chain. Nagai & Mawatari (1995) showed by spectroscopy that a considerable proportion of the mutant subunits of Hb M Saskatoon and Hb M Boston stay in the fully reduced form under circulation conditions. They are inherited as autosomal-dominant traits ( ). Methylthioninium chloride therapy in these individuals is without effect and treatment is not necessary.
Most cases of methemoglobinemia are classified as secondary or acquired, due mainly to exposure to drugs and chemicals that cause increased formation of Hi. Chemicals or drugs that directly oxidize HbO 2 to Hi include nitrites, nitrates, chlorates, and quinones. Other substances, which are aromatic amino and nitro compounds, probably act indirectly through a metabolite because they do not cause Hi formation in vitro. These include acetanilid, phenacetin, sulfonamides, and aniline dyes. Ferrous sulfate may produce methemoglobinemia after ingestion of very large doses. Levels of drugs or chemicals that would not cause significant methemoglobinemia in a normal individual may do so in someone with a mild reduction in NADH-cytochrome- b 5 reductase activity that, under ordinary circumstances, is not cyanotic. Such individuals are newborn infants and persons heterozygous for NADH-cytochrome- b 5 reductase deficiency ( ). Hi is reduced back to Hb by the erythrocyte enzyme systems. It can also be reduced (slowly) by the administration of reducing agents, such as ascorbic acid or sulfhydryl compounds (glutathione, cysteine); these, as well as methylthioninium chloride, are of value in cases of hereditary NADH-cytochrome- b 5 reductase deficiency. In cases of acquired or toxic methemoglobinemia, methylthioninium chloride is of great value; its rapid action is based not on its own reduction capacity but on its acceleration of the normally slow NADPH–methemoglobin reductase pathway. Hi can combine reversibly with various chemicals (e.g., cyanides, sulfides, peroxides, fluorides, azides). Because of the strong affinity of Hi for cyanide, the therapy of cyanide poisoning is to administer nitrites to form Hi, which then combines with the cyanide. Thus, the free cyanide (which is extremely poisonous to the cellular respiratory enzymes) becomes less toxic when changed to HiCN.
Hi is quantitated by spectrophotometry. If Hi is elevated, drugs or toxic substances must first be eliminated as a cause. Congenital methemoglobinemia due to NADH-cytochrome- b 5 reductase deficiency is determined by assay of the enzyme. An abnormal hemoglobin (Hb M) may also be responsible for methemoglobinemia noted at birth or in the first few months of life.
SHb is a mixture of oxidized, partially denatured forms of Hb that form during oxidative hemolysis ( ). During oxidation of Hb, sulfur (the source of which may vary) is incorporated into heme rings of Hb, resulting in a green hemochrome. Further oxidation usually results in the denaturation and precipitation of Hb as Heinz bodies ( Fig. 31.1 ). SHb cannot transport O 2 , but it can combine with carbon monoxide (CO) to form carboxysulfhemoglobin. Unlike methemoglobin, SHb cannot be reduced back to Hb, and it remains in the cells until they break down. The blood is mauve-lavender in sulfhemoglobinemia. SHb has been reported in patients receiving treatment with sulfonamides or aromatic amine drugs (phenacetin, acetanilid), as well as in patients with severe constipation, in cases of bacteremia due to Clostridium perfringens and in a condition known as enterogenous cyanosis . The concentration of SHb in vivo normally is less than 1%, and in these conditions it seldom exceeds 10% of the total Hb. It results in cyanosis and is usually asymptomatic. The reason why some patients develop methemoglobinemia, some sulfhemoglobinemia, and others Heinz bodies and hemolysis is not well understood. SHb is quantitated by spectrophotometry.
Endogenous CO produced in the degradation of heme to bilirubin normally accounts for about 0.5% of carboxyhemoglobin (HbCO) in the blood and is increased in hemolytic anemia. Hb has the capacity to combine with CO with an affinity 210 times greater than for O 2 . CO will bind with Hb even if its concentration in the air is extremely low (e.g., 0.02%–0.04%). In those cases, HbCO will build up until typical symptoms of poisoning appear. HbCO cannot bind and carry O 2 . Furthermore, increasing concentrations of HbCO shift the Hb-O 2 dissociation curve increasingly to the left, thus adding to the anoxia. If a patient poisoned with CO receives pure O 2 , the conversion of HbCO to HbO 2 is greatly enhanced. HbCO is light sensitive and has a typical brilliant cherry-red color.
Acute CO poisoning is well known. It produces tissue hypoxia as a result of decreased O 2 transport. Chronic poisoning, a result of prolonged exposure to small amounts of CO, is less well recognized but is of increasing importance. The chief sources of the gas are gasoline motors, illuminating gas, gas heaters, defective stoves, and the smoking of tobacco. Exposure to CO is thus one of the hazards of modern civilization. The gas has even been found in the air of busy streets of large cities in sufficient concentration to cause mild symptoms in persons such as traffic police officers, who are exposed to it over long periods of time. Chronic exposure through tobacco smoking may lead to chronic elevation of HbCO and an associated left shift in the Hb-O 2 dissociation curve; smokers tend to have higher Hcts than nonsmokers and may have polycythemia. Healthy persons exposed to various concentrations of the gas for 1 hour do not experience definite symptoms (headache, dizziness, muscular weakness, and nausea) unless the concentration of gas in the blood reaches 20% to 30% of saturation; however, it appears that in chronic poisoning, especially in children, serious symptoms may occur with lower concentrations. HbCO may be quantitated by differential spectrophotometry or by gas chromatography.
The cyanmethemoglobin (hemiglobincyanide; [HiCN]) method has the advantages of convenience and a readily available, stable standard solution.
Blood is diluted in a solution of potassium ferricyanide and potassium cyanide. The potassium ferricyanide oxidizes Hb to Hi (methemoglobin), and potassium cyanide provides cyanide ions (CN – ) to form HiCN, which has a broad absorption maximum at a wavelength of 540 nm ( Fig. 31.2 ; Table 31.1 ). The absorbance of the solution is measured in a spectrophotometer at 540 nm and is compared with that of a standard HiCN solution.
![Figure 31.2, Absorption spectra of oxyhemoglobin (HbO 2 ), deoxyhemoglobin (Hb), methemoglobin (hemiglobin [Hi]), and cyanmethemoglobin (hemiglobincyanide [HiCN]) Figure 31.2, Absorption spectra of oxyhemoglobin (HbO 2 ), deoxyhemoglobin (Hb), methemoglobin (hemiglobin [Hi]), and cyanmethemoglobin (hemiglobincyanide [HiCN])](https://storage.googleapis.com/dl.dentistrykey.com/clinical/BasicExaminationofBloodandBoneMarrow/1_3s20B9780323673204000316.jpg)
| Term | Symbol | ABSORPTION PEAK 1 | ABSORPTION PEAK 2 | ABSORPTION PEAK 3 | |||
|---|---|---|---|---|---|---|---|
| λ ∗ | ε | λ | ε | λ | ε | ||
| Hemoglobin | Hb | 431 | (140) | 555 | (13.04) | ||
| Oxyhemoglobin | HbO 2 | 415 | (131) | 542 | (14.37) | 577 | (15.37) |
| Carboxyhemoglobin | HbCO | 420 | (192) | 539 | (14.36) | 568.5 | (14.31) |
| Hemiglobin (methemoglobin) | Hi | 406 | (162) | 500 | (9.04) | 630 | (3.70) |
| Hemiglobincyanide (cyanmet Hb) | HiCN | 421 | (122.5) | 540 | (10.99) | ||
∗ These wavelengths are not shown in the absorption spectrum in Fig. 31.2. because the hemoglobins have much higher absorbances (i.e., the Soret band region).
The diluent is detergent-modified Drabkin reagent:
g Potassium ferricyanide (K 3 Fe[CN] 6 )
g Potassium cyanide (KCN)
g Dihydrogen potassium phosphate (anhydrous; KH 2 PO 4 )
Nonionic detergent, for example,
mL Sterox S.E. (Harleco) or
mL Triton X-100 (Rohm and Haas)
Distilled water to 1000 mL
The solution should be clear and pale yellow, have a pH of 7.0 to 7.4, and give a reading of zero when measured in the photometer at 540 nm against a water blank.
Substituting dihydrogen potassium phosphate (KH 2 PO 4 ) in this reagent for sodium bicarbonate (NaHCO 3 ) in the original Drabkin reagent shortens the time needed for complete conversion of Hb to HiCN from 10 minutes to 3 minutes. The detergent enhances lysis of erythrocytes and decreases turbidity from protein precipitation.
Care must be taken with KCN in the preparation of the Drabkin solution, as salts or solutions of cyanide are poisonous. The diluent itself contains only 50 mg KCN/L—less than the lethal dose for a 70-kg person. However, because hydrogen cyanide (HCN) is released by acidification, exposure of the diluent to acid must be avoided. Disposal of reagents and samples in running water in the sink is advised. The diluent keeps well in a dark bottle at room temperature but should be prepared fresh periodically.
To 5.0 mL of diluent, 20 μL of blood is added (1:251), mixed well, and allowed to stand at room temperature for at least 3 minutes ( ). The absorbance is measured against the reagent blank in the photoelectric colorimeter at 540 nm or with an appropriate filter. A vial of HiCN standard is then opened and the absorbance measured, at room temperature, in the same instrument in a similar fashion. The test sample must be analyzed within a few hours of dilution. The standard must be kept in the dark when not in use and discarded at the end of the day.
It is usually convenient to calibrate the photometer to be used for hemoglobinometry by preparing a standard curve or table that will relate absorbance to Hb concentration in grams per deciliter. The absorbance of fresh HiCN standard is measured against a reagent blank. Absorbance readings are made of fresh HiCN standard and of dilutions of this standard in the reagent (1 in 2, 1 in 3, and 1 in 4) against a reagent blank. Hb values in grams per deciliter are calculated for each solution as described previously. When the absorbance readings are plotted on linear graph paper as the ordinates against Hb concentration as the abscissa, the points should describe a straight line that passes through the origin. An advantage of the HiCN method is that most forms of hemoglobin (Hb, HbO 2 , Hi, and HbCO, but not SHb) are measured.
The test sample can be directly compared with the HiCN standard, and the readings can be made at the convenience of the operator because of the stability of the diluted samples. Increased absorbance not due to Hb may be caused by turbidity due to abnormal plasma proteins, hyperlipemia, large numbers of leukocytes (counts >30 × 10 9 /L), or fatty droplets, any of which may lead to increased light scattering and apparent absorbance.
Sources of error may be those of the sample, the method, the equipment, or the operator.
Improper venipuncture technique may introduce hemoconcentration, which will make Hb concentration and cell counts too high. Improper technique in fingerstick or capillary sampling can produce errors in either direction.
The HiCN method is the method of choice. Use of the HiCN standard for calibration of the instrument and for the test itself eliminates a major source of error. The broad absorption band of HiCN in the region of 540 nm makes it convenient to use both in filter-type photometers and in narrow-band spectrophotometers. With the exception of SHb, all other varieties of hemoglobin are converted to HiCN. Since the total non-sulfohemoglobin concentration is known and since the molar extinction coefficient for each type of hemoglobin is known at a number of different wavelengths, the concentration of sulfohemoglobin can be directly determined at any one of these wavelengths using Beer’s Law ( Chapter 4 ).
The accuracy of equipment is not uniform. A good grade of pipet with a guaranteed accuracy of greater than 99% is desirable. Calibration of pipets will lessen errors. Significant error can be introduced by the use of unmatched cuvets; therefore, flow-through cuvets are preferred. The wavelength settings, filters, and meter readings require checking. The photometer must be calibrated in the laboratory before its initial use and must be rechecked frequently to reduce the method’s error to 2% (±CV).
Automated equipment is now widely used and eliminates most errors associated with manual techniques of hemoglobinometry.
The various Hbs have characteristic absorption spectra, which can be determined easily with a spectrophotometer. Useful absorbance maxima are given in Table 31.1 . The maxima for Hi vary considerably with pH. The maxima given in the two right-hand columns are useful for distinguishing among these forms of Hb. Absorbance between 405 and 435 nm (the Soret band) is considerably greater and may be used when small concentrations of Hb are to be measured.
The Hct of a sample of blood is the ratio of the volume of erythrocytes to that of the whole blood. It may be expressed as a percentage (conventional) or as a decimal fraction (SI units). The units L/L are implied. Dried heparin and ethylenediaminetetraacetic acid (EDTA) are satisfactory anticoagulants. Before taking a sample from a tube of venous blood for a hematologic determination, it is important to mix the blood thoroughly. If the tube has been standing, this requires at least 60 inversions of the tube, or 2 minutes on a mechanical rotator; less than this leads to unacceptable deterioration in precision ( ). The number of inversions required to achieve homogeneity of a specimen depends on the dimensions of the container. Standard 10 to 14 × 75-mm tubes, containing 5 mL of blood and an air bubble that constitutes at least 20% of the tube volume, require at least eight inversions (National Committee for Clinical Laboratory Standards ). The venous Hct agrees closely with the Hct obtained from a skin puncture; both are greater than the total body Hct. The Hct may be measured directly by centrifugation with macromethods or micromethods, or indirectly as the product of the mean corpuscular volume (MCV) times RBC count in automated instruments. In blood kept at room temperature, swelling of erythrocytes between 6 and 24 hours raises Hct and MCV. Cell counts and indices are stable for 24 hours at 4°C ( ).
Hct determination is performed by centrifugation. Inspection of the specimen after spinning may furnish valuable information. The relative heights of the red cell column, buffy coat, and plasma column should be noted. The buffy coat is the red-gray layer between the red cells and the plasma; it includes platelets and leukocytes.
An orange or green color of the plasma suggests increased bilirubin; pink or red suggests hemoglobinemia. Poor technique in collecting the blood specimen is the most frequent cause of hemolysis. If specimens are not obtained within 1 or 2 hours after a fat-rich meal, cloudy plasma may point to nephrosis or certain abnormal hyperglobulinemias, especially cryoglobulinemia.
A capillary Hct tube about 7 cm long with a uniform bore of about 1 mm is used. For blood collection directly from a skin puncture, heparinized capillary tubes are available.
The microhematocrit tube is filled by capillary attraction from a free-flowing puncture wound or a well-mixed venous sample. The capillary tube should be filled to at least 5 cm. The empty end is sealed with modeling clay. The filled tube is placed in the radial grooves of the microhematocrit centrifuge head with the sealed end away from the center. Place the bottom of the tube against the rubber gasket to prevent breakage. Centrifugation for 5 minutes at 10,000 to 12,000 g is satisfactory unless the Hct exceeds 50%; in that case, an additional 5 minutes of centrifugation should be employed to ensure minimal plasma trapping. The capillary tubes are not graduated. The length of the blood column, including the plasma, and of the red cell column alone must be measured in each case with a millimeter rule and a magnifying lens, or with one of several commercially available measuring devices. The manufacturer’s instructions must be followed.
Typical reference values for adult males are 0.41 to 0.51, and for females, 0.36 to 0.45. A value below an individual’s normal value or below the reference interval for age and sex indicates anemia, and a higher value, polycythemia. The Hct reflects the concentration of red cells—not the total red cell mass. The Hct is low in hydremia of pregnancy, but the total number of circulating red cells is not reduced. The Hct may be normal or even high in shock accompanied by hemoconcentration, although the total red cell mass may be decreased considerably owing to blood loss. The Hct is unreliable as an estimate of anemia immediately after loss of blood or immediately following transfusions.
Adequate duration and speed of centrifugation are essential for a correct Hct. The red cells must be packed so that additional centrifugation does not further reduce the packed cell volume. In the course of centrifugation, small proportions of the leukocytes, platelets, and plasma are trapped between the red cells. The error resulting from the former is, as a rule, quite insignificant. The amount of trapped plasma is larger in high Hcts than in low Hcts. Trapped plasma accounts for about 1% to 3% of the red cell column in normal blood (about 0.014 in a Hct of 0.47) and slightly more in macrocytic anemia, spherocytosis, and hypochromic anemia ( ). Even greater amounts of trapped plasma are noted in the Hcts of patients with sickle cell anemia; these vary depending on the degree of sickling and consequent rigidity of the cells. In using the microhematocrit as a reference method for calibrating automated instruments, correction for trapped plasma is recommended (International Committee for Standardization in Hematology [ICSH], 1980).
Posture, muscular activity, and prolonged tourniquet-stasis can cause the same order of changes in Hct and cell concentrations as they do in nonfilterable soluble constituents. Unique to the Hct is error due to excess EDTA (inadequate blood for a fixed amount of EDTA): The Hct will be falsely low as a result of cell shrinkage, but the Hb and cell counts will not be affected. There is no uniformity as to which EDTA salt is used for anticoagulation ( ). The tripotassium (K 3 -EDTA) salt shrinks red cells about 2% and lowers packed cell volume compared with the dipotassium salt (K 2 -EDTA) ( ). Also, because K 3 -EDTA is a liquid, measured Hb and red and white cell counts are decreased by 1% to 2%. Although the ICSH and the Clinical Laboratory Standards Institute recommend the K 2 -EDTA salt (powder), the K 3 -EDTA is more often used, perhaps because of its increased miscibility and fewer instances of specimen clotting ( ).
Technical errors include failure to mix the blood adequately before sampling, improper reading of the levels of cells and plasma, and inclusion of the buffy coat as part of the erythrocyte volume. With good technique, the precision of the Hct, expressed as ±2 CV (coefficient of variation), is ±1%. With low Hct values, the CV is greater because of reading error.
Wintrobe introduced calculations for determining the size, content, and Hb concentration of red cells; these erythrocyte indices have been useful in the morphologic characterization of anemias. They may be calculated from the red cell count, Hb concentration, and Hct.
The MCV, the average volume of red cells, is calculated from the Hct and the red cell count. MCV = Hct × 1000/RBC (in millions per μL), expressed in femtoliters or cubic micrometers. If the Hct = 0.45 and the red cell count = 5 × 10 12 /L, 1 L will contain 5 × 10 12 red cells, which occupy a volume of 0.45 L.
The mean cell hemoglobin (MCH) is the content (weight) of Hb of the average red cell; it is calculated from the Hb concentration and the red cell count.
The value is expressed in picograms. If the Hb = 15 g/dL and the red cell count is 5 × 10 12 /L, 1 L contains 150 g of Hb distributed in 5 × 10 12 cells.
The mean cell (corpuscular) hemoglobin concentration (MCHC) is the average concentration of Hb in a given volume of packed red cells. It is calculated from the Hb concentration and the Hct.
If the Hb = 15 g/dL and the Hct = 0.45,
Indices are determined in the electrical impedance instruments somewhat differently. The MCV is derived from the mean height of the voltage pulses formed during the red cell count, and the Hb is measured by optical density of HiCN. The other three values are calculated as follows:
The reference values for the indices will depend on whether they are determined from the centrifuged Hct or the cell counters. The values in normal individuals will be similar if both are corrected for trapped plasma. However, because of increased trapped plasma in hypochromic anemias and sickle cell anemia, the MCHC calculated from the microhematocrit will be significantly lower than the MCHC derived from the electrical impedance counters.
The 95% reference intervals for normal adults are as follows: MCV = 80 to 96 fL; MCH = 27 to 33 pg; and MCHC = 33 to 36 g/dL ( ). In a healthy person, there is very little variation—no more than ±1 unit in any of the indices. Deviations from the reference value for an individual or outside the reference intervals for normal persons are useful, particularly in characterizing morphologic types of anemia.
In microcytic anemias , the indices may be as low as an MCV of 50 fL, an MCH of 15 pg, and an MCHC of 22 g/dL; rarely do any become lower.
In macrocytic anemias , the values may be as high as an MCV of 150 fL and an MCH of 50 pg, but the MCHC is normal or decreased ( ). The MCHC typically increases only in spherocytosis, and rarely is over 38 g/dL.
Except for some platelet counts and low leukocyte counts, the hemocytometer is no longer used for routine blood cell counting. However, it is still necessary for the technologist to be able to use this method effectively and to know its limitations. Any cell-counting procedure includes three steps: dilution of the blood, sampling of the diluted suspension into a measured volume, and counting of the cells in that volume. Counts of erythrocytes, leukocytes, and platelets are each expressed as concentrations, that is, cells per unit volume of blood. The unit of volume was expressed as cubic millimeters (mm 3 ) because of the linear dimensions of the hemocytometer (cell counting) chamber:
Although there is no consistency in the literature in the use of traditional/conventional units versus Système International d’Unites (SI) units, the ICSH recommends that the unit of volume be the liter (SI units), as on the right in the following examples:
Systems for manual dilutions combine a microcapillary tube with a plastic vial containing a premeasured volume of diluent. After the capillary tube is filled, it is pushed into the container and the sample is washed out by squeezing the soft plastic vial. This system is especially convenient for microsampling. Unopettes are available with diluents for counts of RBCs, white blood cells (WBCs), platelets, eosinophils, and reticulocytes.
Instruments are available for precise and convenient diluting that both aspirate the sample and wash it out with the diluent. The dilutor should perform a 1:250 or a 1:500 dilution with a coefficient of variation of less than 1%.
Reticulocytes are immature nonnucleated red cells that contain ribonucleic acid (RNA) and continue to synthesize Hb after loss of the nucleus. When blood is briefly incubated in a solution of new methylene blue or brilliant cresyl blue, the RNA is precipitated as a dye-ribonucleoprotein complex. Microscopically, the complex appears as a dark-blue network (reticulum or filamentous strand) or at least two dark-blue granules that allow reticulocytes to be identified and enumerated (ICSH, 1998). A proposed reference method for reticulocyte counting based on determination of the reticulocyte/red cell ratio has been published (ICSH, 1998) expanding on the 1994 ICSH red cell count reference method.
One percent new methylene blue in a diluent of citrate/saline (1 part 30 g/L sodium citrate plus 4 parts 9 g/L sodium chloride).
Although commercial controls are available, describe a method requiring about 2 hours that produces a multilevel control that is stable for several months. Hypotonic dialysis of RBCs in the presence of RNA followed by a short period of hypertonic dialysis to reseal the pores of the RBC membrane results in about 20% of the RBCs as “synthetic reticulocytes” with various amounts of encapsulated RNA.
Three drops each of reagent and blood are mixed in a test tube, incubated 15 minutes at room temperature, and remixed. Two wedge films are made on glass slides and air dried.
Viewed microscopically with an oil immersion lens, reticulocytes are pale blue and contain dark blue reticular or granular material, and red cells stain pale blue or blue-green. The percentage of reticulocytes is determined in at least 1000 red cells. A Miller disk inserted into the eyepiece allows rapid estimation of large numbers of red cells by imposing two squares (one square is nine times the area of the other) onto the field of view ( ). Reticulocytes are counted in the large square and red cells in the small square in successive microscopic fields until at least 300 red cells are counted. This provides an estimate of reticulocytes among at least 2700 red cells, as follows:
The absolute reticulocyte count is determined by multiplying the reticulocyte percentage by the red cell count.
Normal adults have a reticulocyte count of 0.5% to 1.5%, or 24 to 84 × 10 9 /L. In newborn infants, the percentage is 2.5% to 6.5%. This falls to the adult range by the end of the second week of life.
Because reticulocytes are immature red cells that lose their RNA a day or so after reaching the blood from the marrow, a reticulocyte count provides an estimate of the rate of red cell production. An absolute reticulocyte count or reticulocyte production index is more helpful than the percentage (see Chapter 33 ).
Because such a small number of actual reticulocytes are counted, the sampling error in the manual reticulocyte count is relatively large. The 95% confidence limits may be expressed as follows:
where R is the reticulocyte count in percent, and N is the number of erythrocytes examined. This means that if only 1000 erythrocytes are evaluated, the 95% confidence limits for a 1% count are 0.4% to 1.6%; for a 5% count, 3.6% to 6.4%; and for a 10% count, 8.1% to 11.9%.
Changes in red cell values are greatest during the first few weeks of life ( Fig. 31.3 ). At the time of birth, as much as 100 to 125 mL of placental blood may be added to the newborn if tying the cord is postponed until its pulsation ceases. In a study of newborns whose cords had been clamped late, average capillary red cell counts were 0.4 × 10 12 /L higher 1 hour after and 0.8 × 10 12 /L higher 24 hours after birth compared with newborns whose cords had been clamped early. Capillary blood (obtained by skin puncture) gives higher RBC and Hb values than venous blood (cord). The differences may amount to about 0.5 × 10 12 RBC/L and 3 g Hb/dL. Slowing of capillary circulation and the resulting loss of fluid may be the responsible factors. Examination of venous blood furnishes more consistent results than are obtained by examination of capillary blood.
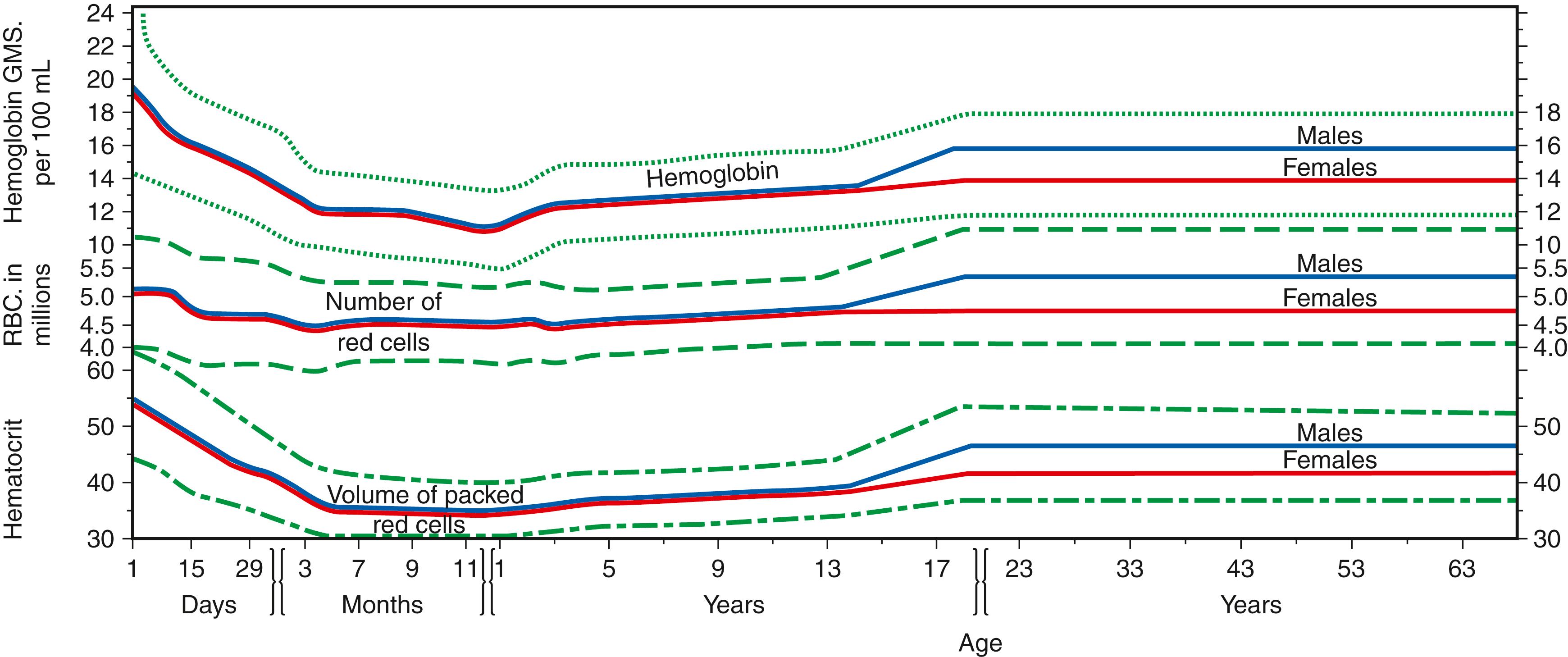
In the full-term infant, nucleated red cells average about 0.5 × 10 9 /L. The normoblast count declines to about 200/μL at 24 hours, 25/μL at 48 hours, and less than 5/μL at 72 hours. By 7 days, it is rare to find circulating normoblasts ( ).
The normal reticulocyte count at birth ranges from 3% to 7% during the first 48 hours, during which time it rises slightly. After the second day, it falls rather rapidly to 1% to 3% by the seventh day of life. Hb concentration in capillary blood during the first day of life averages 19.0 g/dL, with 95% of normal values falling to between 14.6 and 23.4 g/dL. In cord blood, the average is 16.8 g/dL, with 95% of normal between 13.5 and 20 g/dL. Frequently, an initial increase in the Hb level of venous blood is seen at the end of 24 hours compared with that of cord blood. At the end of the first week, the level is about the same as in cord blood, and it does not begin to fall until after the second week. During the first 2 weeks, the lower limit of normal is 14.5 g/dL for capillary blood and 13.0 g/dL for venous blood. The Hct in capillary blood on the first day of life averages 0.61, with 95% of normal values between 0.46 and 0.76. In cord blood, the average is 0.53. Changes during the first few weeks parallel the Hb concentration. The Hb and Hct are highest at birth but fall rather steeply in the first days and weeks of life to a minimum at 2 months of age, at which time the lower limit of the 95% reference values and the mean value for the Hb are 9.4 and 11.2 g/dL, and for the Hct are 0.28 and 0.35, respectively. After 4 months of age, the lower limit for the Hb is 11.2 g/dL and 0.32 for the Hct. These values rise gradually until about 5 years of age and somewhat more steeply in boys than in girls thereafter ( ). The normal MCV at birth ranges from 104 to 118 fL compared with the adult reference interval of 80 to 96 fL. Because the RBC count does not fall to the degree that the Hb and Hct counts fall, the MCV decreases abruptly, then gradually, during the first few months of life. The lowest value is reached at about 1 year. In studies in which iron deficiency and thalassemia are excluded, the lower reference limit (95% reference values) for the MCV gradually rises between 1 year and 15 years of age—from 70 to 76 fL in boys and from 70 to 78 fL in girls ( ). Reference intervals for RBC values in sexually mature adults are given in Table 31.2 . The indices are similar in males and females, but the Hb is 1 to 2 g/dL higher in males, with commensurate increments in Hct and RBCs (see Fig. 31.3 ). This is believed to be mainly the effect of androgen in stimulating erythropoietin production and its effect on the marrow. In older men, the Hb tends to fall; in older women, the Hb tends to fall to a lesser degree (in some studies) or even rise slightly (in other studies). In older individuals, therefore, the sex difference is less than 1 g Hb/dL ( ). Posture and muscular activity change the concentration of the formed elements. The Hb, Hct, and RBC counts increase by several percent in going from recumbency to standing, and strenuous muscular activity causes a further increase, presumably owing primarily to loss of plasma water. Diurnal variation that is not related to exercise or to analytic variation also occurs. The Hb is highest in the morning, falls during the day, and is lowest in the evening, with a mean difference of 8% to 9% ( ). In persons living at a higher altitude, the Hb, Hct, and RBC counts are elevated over what they would be at sea level. The difference is about 1 g Hb/dL at 2 km altitude and 2 g Hb/dL at 3 km. Increased erythropoiesis is secondary to anoxic stimulation of erythropoietin production. People who are smokers also tend to have a mild erythrocytosis.
| Men | Women | ||
|---|---|---|---|
| White cell count (×10 9 /L blood) | 7.8 (4.4–11.3) | ||
| Red cell count (×10 12 /L blood) | 5.21 (4.52–5.90) | 4.60 (4.10–5.10) | |
| Hemoglobin (g/dL blood) | 15.7 (14.0–17.5)1 | 13.8 (12.3–15.3) | |
| Hematocrit (%) | 46 (41.5–50.4) | 40.2 (35.9–44.6) | |
| Mean cell volume (fL/red cell) | 88.0 (80.0–96.1) | ||
| Mean cell hemoglobin (pg/red cell) | 30.4 (27.5–33.2) | ||
| Mean cell hemoglobin concentration (g/dL RBC) | 34.4 (33.4–35.5) | ||
| Red cell distribution width (CV, %) | 13.1 (11.6–14.6) | ||
| Platelet count (×10 9 /L blood) | 311 (172–450) |
EDTA should be used; heparin is unsatisfactory as an anticoagulant.
Although this method is used only occasionally in leukocyte counting, the technologist should be able to perform it in these circumstances:
As a check on the validity of electronic methods for calibration purposes
As a check on the validity of electronic counts in patients with profound leukopenia or thrombocytopenia
For blood specimens with platelet counting interference (i.e., very microcytic RBCs)
As a backup method
It is also commonly used as a method for counting cells in cerebrospinal fluid (CSF).
The hemocytometer is a thick glass slide with inscribed platforms of known area and precisely controlled depth under the coverslip. Counting chambers and cover glasses should be rinsed in lukewarm water immediately after use; wiped with a clean, lint-free cloth; and allowed to air dry. The surfaces must not be touched with gauze or linen because these materials may scratch the ruled areas.
The diluting fluid lyses the erythrocytes so that they will not obscure the leukocytes. The fluid must be refrigerated and filtered frequently to remove yeasts and molds.
Well-mixed blood is diluted 1:20 in diluting fluid and the vial rotated for about 5 minutes. The chamber is loaded with just enough fluid to fill the space beneath the cover glass.
The cells are permitted to settle for several minutes, and the chamber is surveyed with a low-power (10×) objective lens to verify uniform cell distribution.
Counting is performed. The condenser diaphragm of the microscope is partially closed to make the leukocytes stand out clearly under a low-power objective lens. The leukocytes are counted in each of the four large (1-mm 2 ) corner squares (A, B, C, and D in Fig. 31.4 ). A total of eight large corner squares from two sides of a chamber are counted.
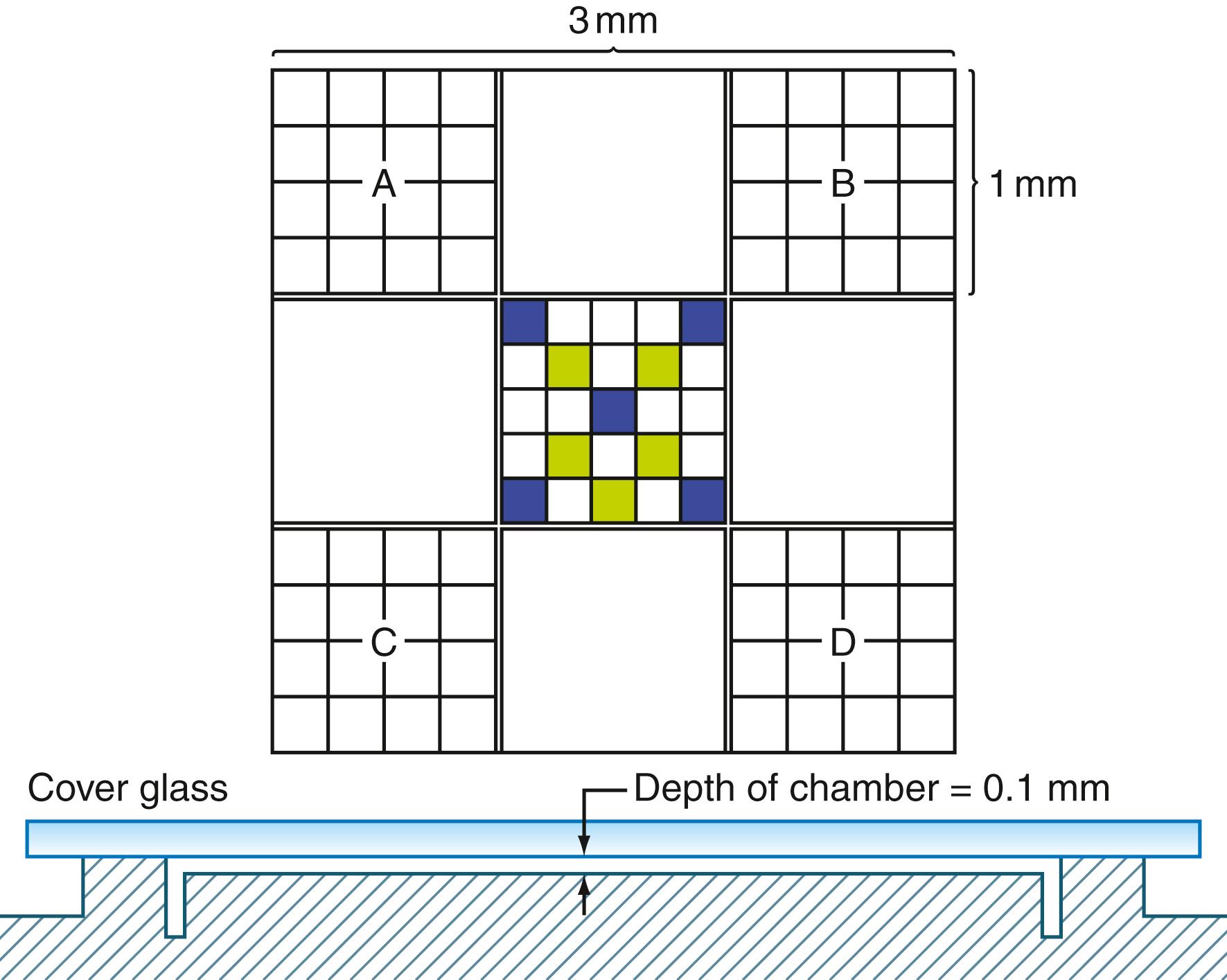
Each large square encloses a volume of 1/10 mm 3 , and the dilution is 1:20. A general formula is as follows:
where cc is the total number of cells counted, d is the dilution factor, 10 is the factor transforming value over one large square (1/10 mm 3 ) to the volume in mm 3 , and lsc is the number of large squares counted.
In leukopenia, with a total count below 2500, the blood is diluted 1:10. In leukocytosis, the dilution may be 1:100 or even 1:200.
Errors may be due to the nature of the sample, to the operator’s technique, and to inaccurate equipment. Errors that are inherent in the distribution of cells in the counting volume are called “field” errors and can be minimized only by counting more cells.
Hemocytometer leukocyte counts show a CV of about 6.5% for normal and increased counts and about 15% in leukopenic blood. Utilizing electronic counters, on the other hand, results in CVs of approximately 1% to 3%.
Partial coagulation of the venous blood causes changes in the distribution of the cells and/or decreases their number. Failure to mix the blood thoroughly and immediately before dilution introduces an error, which depends on the degree of sedimentation.
Errors caused by faulty technique may occur during dilution, when the chamber is loaded, and when the cells are counted.
Equipment errors can be diminished by using pipets and hemocytometers certified by the U.S. Bureau of Standards.
Even in a perfectly mixed sample, variation occurs in the number of suspended cells that are distributed in a given volume (i.e., come to rest over a given square). This “error of the field” is the minimal error. Another error is the “error of the chamber,” which includes variations in separate fillings of a given chamber and in sizes of different chambers. Still another is the “error of the pipet,” which includes variations in filling a given pipet and in the sizes of different pipets. In performing a WBC count, if 200 cells are counted using two chambers and one pipet, the CV = 9.1%, corresponding to 95% confidence limits of ±18.2% (twice the CV). Using four chambers and two pipets and counting twice as many cells reduces the 95% confidence limits to ±12.8%. This relatively large percentage error is of little practical consequence because of the physiologic variation of the leukocyte count.
Nucleated red blood cells (NRBCs) will be counted and cannot be distinguished from leukocytes with the magnification used. If their number is high, as seen on the stained smear, a correction should be made according to the following formula:
where the No. of NRBCs is the number of nucleated red cells that are counted during the enumeration of 100 leukocytes in the differential count.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here