Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Balloon sinus dilatation is a surgical technique that widens the natural sinus ostium using a balloon catheter.
Balloon sinus dilatation has been used to address the maxillary, sphenoid, and frontal sinuses. It can be performed as a balloon-only procedure unaccompanied by endoscopic sinus surgery (ESS) in which the sinus ostia are dilated without any removal of bone or redundant mucosa. It can also be combined with ESS, termed a hybrid procedure, in which ESS is performed with traditional techniques and balloon dilatation is used as a complementary procedure in various sinuses as needed.
The basic technique of balloon sinus dilatation involves advancing a balloon catheter over a guidewire through the natural opening of the sinus. The balloons are available in various lengths and widths that have been designed for specific sinus anatomy. A guide catheter is often used that helps direct the guidewire toward the sinus ostium. When positioned, the balloon is inflated with water under pressure. The balloon is then deflated and removed.
Currently, balloon sinus dilatation is not applied to the ethmoid sinuses. The ethmoid sinuses have multiple septations, with individual ostia that feed into a larger and variable outflow system. There is no one ethmoid sinus ostium that can be dilated with the balloon. Because of this, balloon dilatation is not a treatment modality that directly addresses ethmoid sinus disease.
Determining the applicability of balloon sinus dilatation in the setting of chronic inflammatory disease has been a source of significant contention within the rhinologic community. When balloon sinus dilatation is used in isolation, no bone is removed. Rather, the natural ostium is widened. Surgical objectives of ESS include the restoration of functional mucus flow and air exchange of the sinuses and facilitation of access for topical and irrigated medical treatments. A prevailing principle in ESS is that the bony septations of the sinuses are involved in the chronic inflammatory process and must be removed for the disease process to be adequately impacted. In ESS, the uncinate process is consistently resected, as are the bony septations of the ethmoid sinuses. Balloon sinus dilatation used without traditional ESS techniques does not directly address mucosal and bone inflammation, which is often thought to be a source of continued sinus inflammation.
For the foregoing reasons, consideration should be given to the severity of the disease present and the extent of surgery necessary to achieve clinical improvement. For balloon sinus dilatation to be performed, the natural ostium must be identified and cannulated. Significant mucosal inflammation may prevent introduction of the guidewire and may be more appropriately treated with a hybrid procedure or ESS without dilatation. Furthermore, bony obstructions and changes caused by osteitis may be present that inhibit the easy placement of the balloon system.
Patients with nasal polyposis are poor candidates for balloon sinus dilatation without traditional ESS. Nasal polyps may significantly obstruct the natural outflow tracts, and without débridement of the polyps, sinus dilatation is unlikely to adequately address the obstructive aspects of nasal polyps.
Various anatomic deformities may make balloon dilatation difficult. A deviated nasal septum may make it hard to maneuver the necessary instruments through the nose. Large inferior turbinates or a concha bullosa may also cause difficulty in passing the balloon. Furthermore, a tortuous or complex frontal sinus outflow tract may not allow for easy maneuverability of the guide catheter.
Identify the uncinate process and its relation to the orbit and skull base on CT scan. Examine the borders of the frontal outflow tract and, if possible, attempt to determine the location of the frontal recess in three dimensions. Identify significant variations in anatomy that may complicate the ability to pass the balloon, such as a deviated nasal septum, concha bullosa, large ethmoid bulla, agger nasi cell, suprabullar ethmoid cells, complex frontal sinus anatomy, severe inferior turbinate hypertrophy, and nasal polyposis.
Rule out variants of sinus anatomy that could predispose patients to complications from balloon dilatation. Examples are a dehiscent carotid artery and optic nerve within the sphenoid sinus, herniation of orbital fat into the maxillary sinus or ethmoid complex as a result of prior trauma, the presence of a supraorbital ethmoid cell, or any dehiscence of the skull base.
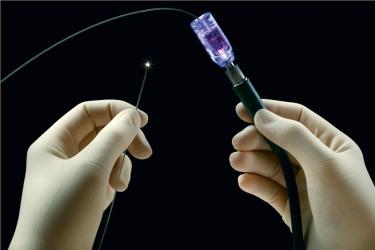
Guidewire: A flexible guidewire is used to determine the location of the sinus ostia. When the technology was originally introduced, fluoroscopy was necessary to confirm placement of the wire within the desired sinus. Now, both flexible and fixed angle guidewires are available with a fiberoptic core that allows the tip to be illuminated. This permits transillumination of the frontal or maxillary sinus to confirm guidewire placement ( Fig. 13.1 ).
Guide catheter: The guide catheter is a hollow-bore tube through which the balloon catheter and guidewire are passed. The tip of the catheter is configured at various angles depending on the sinus to be dilated. The purpose of the guide catheter is to make it easy to advance the balloon through the nasal cavity and direct the balloon into the sinus. Newer catheters have been developed that allow for suction to aid in visualization. Another recent innovation is image guidance localized balloons that allow for computed tomographic (CT) image guidance confirmation of sinus anatomy and balloon positioning ( Fig. 13.2 ).

Balloon: Balloons are available in various diameters and widths. Depending on the sinus to be dilated, a surgeon may choose a wider and longer, or narrower and shorter balloon. Balloons are passed over the flexible guidewire and through a catheter to be introduced into the sinus ( Fig. 13.3 ). Other devices have been designed that combine the balloon and guide catheter into one system ( Fig. 13.4 ).


Inflation device: An inflation device is attached to the balloon apparatus. The inflation device typically consists of a reservoir filled with water and a pressure gauge ( Fig. 13.5 ). Various configurations of this model exist depending on the manufacturer of the balloon system.

Irrigation catheters: Catheters have been designed that can be advanced over the guidewire for irrigation of sinuses.
Image guidance: Stereotactic image guidance systems can be utilized to track certain guide catheters to aid in localization of the sinus outflow tract for balloon placement.
The frontal anatomy in relation to the ethmoid anatomy should be determined before attempting to dilate the frontal sinus. Frontal recess cells can be mistaken for the true frontal recess.
Dilating the frontal recess at the beginning of surgery, before traditional ESS dissection, may be easier, because there will be no bleeding to obstruct the field of view. However, at times it can be difficult to introduce the guidewire into the frontal sinus with the uncinate process intact. Thus, dissection of the uncinate process before dilatation of the frontal sinus outflow tract is attempted may, in some cases, provide better access to the recess.
The risk of submucosal dissection by the guidewire is increased when the wire is placed after surgical dissection. Special care must be taken to appreciate the tactile feel of the wire during advancement to avoid this complication. Advancement with smooth, light pressure is appropriate, and resistance is an indication that the wire may not be in the correct space.
It is imperative to have a firm understanding of the patient’s ethmoid anatomy in relation to the frontal sinus anatomy. If well-pneumatized suprabullar ethmoid cells are present, it is easy to confuse these with the frontal sinus. For this reason, when an attempt is made to dilate the frontal sinus, the suprabullar ethmoid cell may actually be dilated. To prevent this error, it is critical to observe the intensity of the light on the forehead. When the guidewire is properly placed in the frontal sinus, the transillumination from the guidewire light will move as a well-defined spot along the inner surface with wire manipulation. When the wire is placed in the ethmoid or a suprabullar cell, the light will be more generally diffused without a focused, more intense spot that moves with the tip of the catheter.
A large ethmoid bulla can interfere with the movement of the guide catheter in the anterior to posterior dimension. At times, it may be necessary to dissect the anterior ethmoid cells so that proper positioning of the guide catheter is possible when the frontal sinus is to be dilated.
When the sphenoid sinus is to be dilated, there should be a firm understanding of the location of the carotid artery, optic nerve, and skull base in relation to the natural ostium. The guidewire is introduced blindly through the sphenoid ostium; if a dehiscent artery or nerve is present, these structures could be at risk. Likewise, the balloon should be subsequently introduced at the appropriate angle and depth. If there is any question as to the location of the guidewire, fluoroscopy can be used to confirm placement.
If a balloon-only procedure is used to dilate the maxillary sinus, careful attention should be paid to avoid causing mucosal injury to the uncinate process, which could result in adhesion formation and further obstruction.
When the guidewire is introduced into the maxillary sinus, it is of the utmost importance that the wire pass through the natural maxillary ostium. If the balloon is dilated in a location other than the natural ostium, an accessory ostium can be created or dilated, which may result in a recirculation phenomenon. If this occurs and is recognized at the time of surgery, the natural ostium should be identified and evaluated, and the surgeon should consider connecting the newly formed accessory ostium to the natural ostium.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here