Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The major androgen produced by the ovaries is testosterone and that of the adrenal glands is dehydroepiandrosterone sulfate; many potent 11-oxo androgens produced by the adrenal glands determine androgen action but are not currently measured.
Androgen action is determined by the “free” or non–SHBG-bound component of testosterone and other androgens, but is poorly measured; and by dihydrotestosterone produced peripherally, in skin, by increased 5α-reductase activity.
Symptoms of androgen excess in women are hirsutism, acne, and scalp hair loss (alopecia). The most common cause of androgen excess is polycystic ovary syndrome (PCOS), occurring approximately 70% of the time. There are three criteria to diagnose PCOS; the diagnosis is based on clinical criteria, not laboratory values.
Because androgen excess is best explained as being a peripheral or skin disorder related to enhancement of androgen action, antiandrogens are a mainstay of treatment. Hirsutism is best treated with an oral contraceptive and an antiandrogen, with spironolactone being the preferred agent. Response rates are approximately 70%.
Excessive hair removal should be carried out once excessive androgen action has been suppressed. Laser treatment is more effective than electrolysis, although the latter is preferred for light-colored hair.
Androgen excess in women usually presents with elevated androgen levels in blood as well as skin manifestations ( acne, hirsutism, and scalp hair loss or alopecia ), but many women exhibit only skin manifestations without demonstrable findings in blood, perhaps in part because of the lack of sensitivity of current clinical laboratory assays.
The clinical signs associated with excessive androgen production in women are related to findings in skin and include acne, hirsutism, alopecia, and, rarely, virilization. It is these complaints that warrant an evaluation and possible treatment. Merely having elevated androgens in blood (hyperandrogenemia), per se, should not be the target of any treatment.
These skin disorders may be understood by understanding the pilosebaceous unit (PSU). The PSU is composed of a sebaceous component and pilary component from which the hair shaft arises. Abnormalities of the sebaceous component lead to acne, and abnormalities of the pilary unit lead to excessive growth (hirsutism) or excessive shedding (alopecia). There are two types of hair; vellus hair is soft, fine, and unpigmented, whereas terminal hair is coarse, thick, pigmented, and undergoes cyclic changes. Anagen is the growth phase of hair. It is followed by the transitional catagen phase, and, finally, by a resting, or telogen, phase, after which the hair sheds ( ). Androgen is necessary to produce development of terminal hair, and the duration of the anagen phase is directly related to the levels of circulating androgen. The duration of anagen also determines the length of hair , which varies in different parts of the body. For facial hair it is approximately 4 months, which has implications for the treatment of facial hirsutism, described later.
There are several steroidogenic enzymes in the hair follicle, but the activity level of the enzyme 5-alpha-reductase (5 α -reductase) most directly influences the degree of androgenic effect on hair growth. With elevated levels of circulating androgen or increased activity of 5 α -reductase, terminal hair appears where normally only vellus hair is present. With these alterations, the length of the anagen phase is prolonged and the hair becomes thicker. Excessive 5α-reductase activity also may lead to acne and scalp hair loss (alopecia) .
The amount and location of hair growth found in women with hirsutism varies. In the milder forms, hair is found only on the upper lip and chin, whereas with increasing severity it appears on the cheeks, chest (intermammary), abdomen (superior to the umbilicus), inner aspects of the thighs, lower back, and intergluteal areas. The severity of the hirsutism can be roughly quantified by a modified scoring system of Ferriman and Gallwey ( ; ) ( Fig. 38.1 , Table 38.1 ). Examples of this scoring system may be found in Fig. 38.2 . Although a score greater than 7 or 8 has generally been considered to be consistent with hirsutism, this only pertains to the Caucasian or African American population. In Asian women the threshold for an abnormal score is much lower at greater than 3 ( ). Increased hair growth only on the extremities or in isolated areas is called hypertrichosis and should not be confused with hirsutism.
| Site | Grade | Definition |
|---|---|---|
| Upper lip | 1 2 3 4 |
Few hairs at outer margin Small mustache at outer margin Mustache extending halfway from outer margin Mustache extending to midline |
| Chin | 1 2 3, 4 |
Few scattered hairs Scattered hairs with small concentrations Complete cover, light and heavy |
| Chest | 1 2 3 4 |
Circumareolar hairs With midline hair in addition Fusion of these areas, with 75% cover Complete cover |
| Upper back | 1 2 3, 4 |
Few scattered hairs Rather more, still scattered Complete cover, light and heavy |
| Lower back | 1 2 3 4 |
Sacral tuft of hair With some lateral extension 75% cover Complete cover |
| Upper abdomen | 1 2 3, 4 |
Few midline hairs Rather more, still midline Half- and full cover |
| Lower abdomen | 1 2 3 4 |
Few midline hairs Midline streak of hair Midline band of hair Inverted V-shaped growth |
| Arm | 1 2 3, 4 |
Sparse growth affecting not more than 25% of limb surface More than this; cover still incomplete Complete cover, light and heavy |
| Forearm | 1-4 | Complete cover of dorsal surface; two grades of light and two of heavy growth |
| Thigh | 1-4 | As for arm |
| Leg | 1-4 | As for arm |
Virilization is a relatively uncommon clinical finding and its presence is usually associated with markedly elevated levels of circulating testosterone (≥2 ng/mL). In contrast to the gradual development of hirsutism, signs of virilization usually occur over a relatively short period. These signs are caused by the masculinizing and defeminizing (antiestrogenic) actions of testosterone and include temporal balding, clitoral hypertrophy, decreased breast size, dryness of the vagina, and increased muscle mass. Women with virilization are almost always amenorrheic. The presence of androgen-secreting neoplasms should always be suspected in any woman who develops signs of virilization, particularly if the onset is rapid.
Androgen production in women is best understood by the concept of production from glandular tissues, namely the ovaries and adrenals, and from nonglandular (peripheral) tissues. This third compartment of production and modification of androgens includes many peripheral tissues and, for our discussion of hyperandrogenism, principally means the PSU itself, which not only responds to androgen but can modify it by enzymatic modifications. From a quantitative perspective, the major androgen produced by the ovaries is testosterone and that of the adrenal glands is dehydroepiandrosterone sulfate (DHEAS) . Measurement of the amount of these two steroids in the circulation provides clinically relevant information regarding the presence and source of increased androgen production. In addition to glandular production of androgens, conversion of androstenedione and dehydroepiandrosterone (DHEA) to testosterone occurs in peripheral tissues.
The ovaries secrete only approximately 0.1 mg of testosterone/day, mainly from the thecal and stroma cells. Other androgens secreted by the ovary are androstenedione (1 to 2 mg/day) and DHEA (<1 mg/day). The adrenal glands, in addition to secreting large quantities of DHEAS (6 to 24 mg/day), secrete approximately the same daily amount of androstenedione (1 mg/day) as the ovaries and less than 1 mg of DHEA/day. The normal adrenal gland secretes little testosterone, although some adrenal tumors have the ability to produce testosterone directly.
Androstenedione and DHEA do not have strong androgenic activity but are peripherally converted at a slow rate to the biologically active androgen, testosterone. Because the ovaries and adrenal gland secrete approximately equal amounts of androstenedione and DHEA, approximately two-thirds (0.22 mg) of the daily testosterone produced in a woman originates from the ovaries. Thus increased circulating levels of testosterone usually indicate abnormal ovarian androgen production. Clinical measurements of testosterone have not been sufficiently sensitive to differentiate normal from slightly elevated values; however, more laboratories are now moving toward using mass spectrometry and related methods, which are far more sensitive.
For practical purposes, circulatory levels of DHEAS reflect an adrenal source of production , and in women more than 95% is adrenal derived. Occasionally, in women who have increased production of ovarian DHEA, such as some with polycystic ovary syndrome (PCOS), the elevated levels of DHEAS might have an ovarian component because DHEA may be converted to DHEAS in the circulation. Another specific marker of adrenal androgen production, used for research purposes, is 11 β -hydroxyandrostenedione, because the adrenal primarily has the ability to 11-hydroxylate androstenedione, whereas the ovary has a limited ability to do so.
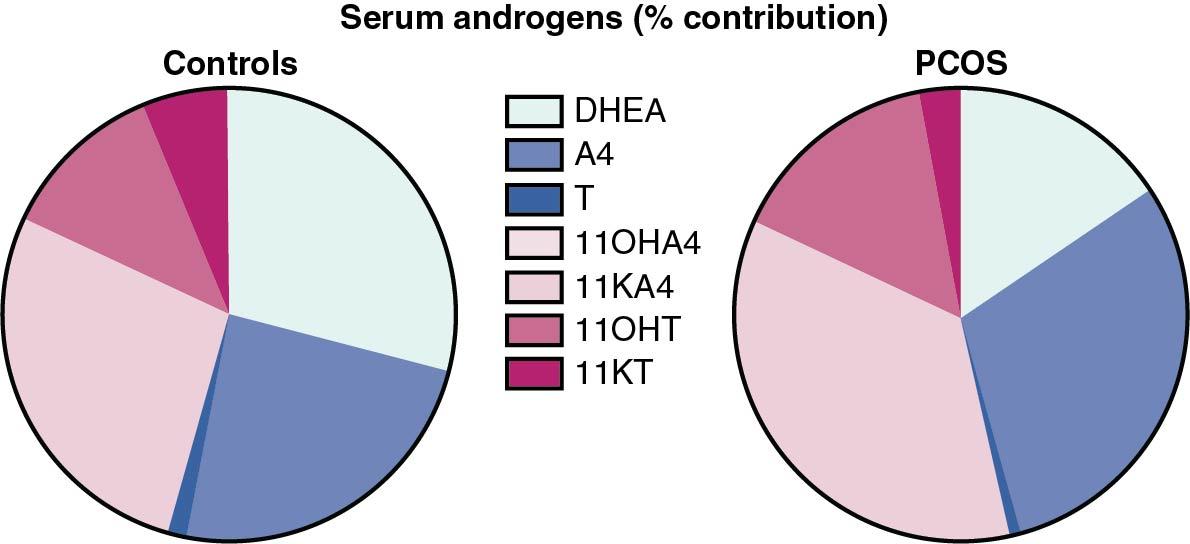
Just in the last few years it has been realized using mass spectroscopy techniques that 11-oxygenated androgens produced by the adrenal circulate in blood in large quantities. It has been suggested that these androgens are the predominant circulating androgens in women with PCOS ( ) Fig. 38.3 . Some of these steroids such as 11-keto dihydrotestosterone are extremely potent and likely enhance androgen action. In the future it is likely that some of these androgens will be measured more routinely to have a better understanding of abnormal secretion and how they may be affected by treatment.
Although DHEAS serves as a good marker of adrenal hyperandrogenism, several guidelines for the evaluation of androgen excess in women omit this measurement, because DHEAS itself is a “weak” androgen and may not contribute much to the overall androgenicity. Nevertheless it is our perspective that the measurement of DHEAS gives a more complete picture of androgen production.
Most testosterone in the circulation (≈85%) is tightly bound to sex hormone–binding globulin (SHBG) and is believed to be biologically inactive. An additional 10% to 15% is loosely bound to albumin, with only approximately 1% to 2% not bound to any protein ( free testosterone ). Both the free and albumin-bound fractions (often called unbound biologically active) are . Serum testosterone can be measured as the total amount, the amount that is believed to be biologically active (unbound, or non-SHBG bound), and as the free form. As discussed later, because commercial laboratory measurements of “free” testosterone are not accurate, it may be useful to measure the ratio of testosterone and SHBG.
To exert a biologic effect, testosterone is metabolized peripherally in target tissues to the more potent androgen 5 α -dihydrotestosterone (DHT) by the enzyme 5 α -reductase . 5 α -reductase activity is important for testosterone action peripherally (as in the PSU) as well as in the genitalia ( ). It is not necessary for testosterone action in other areas such as in muscle or bone. After further 3-keto reduction, DHT is converted to another metabolite, 5 α -androstane-3 α ,17 β -diol (3 α -diol). 3 α -Diol is conjugated to the sulfate or glucuronide. The glucuronide, 5 α -androstane-3 α ,17 β -diol glucuronide (3 α -diol-G) , is a stable, irreversible product of intracellular 5 α -reductase activity and reflects this activity in blood ( Fig. 38.4 ).
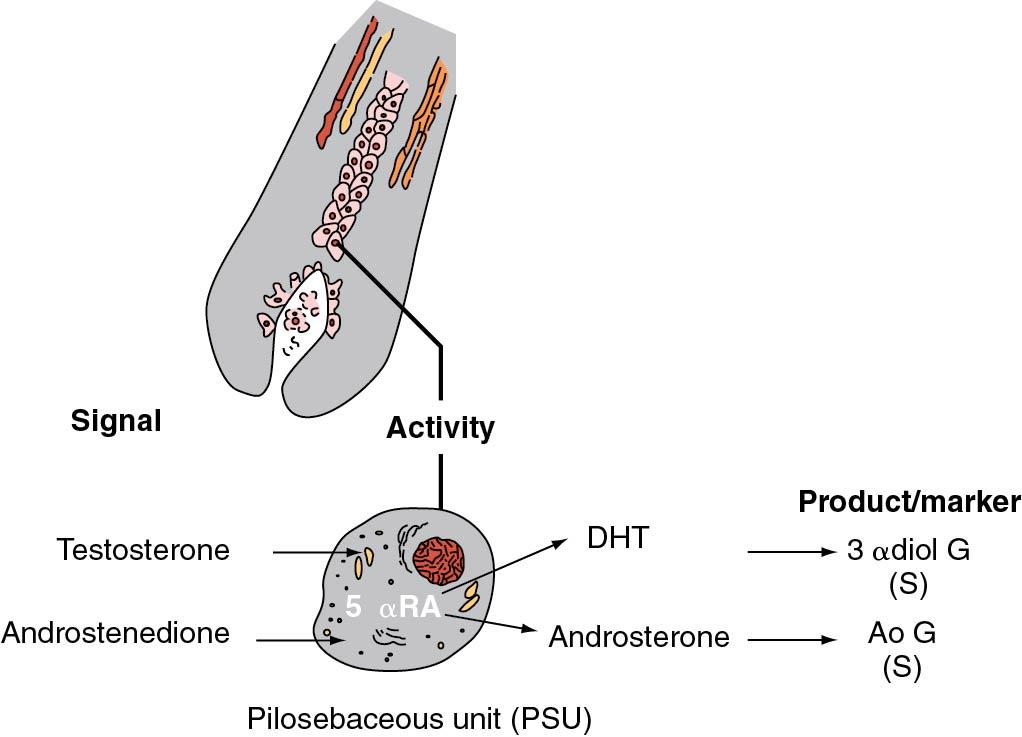
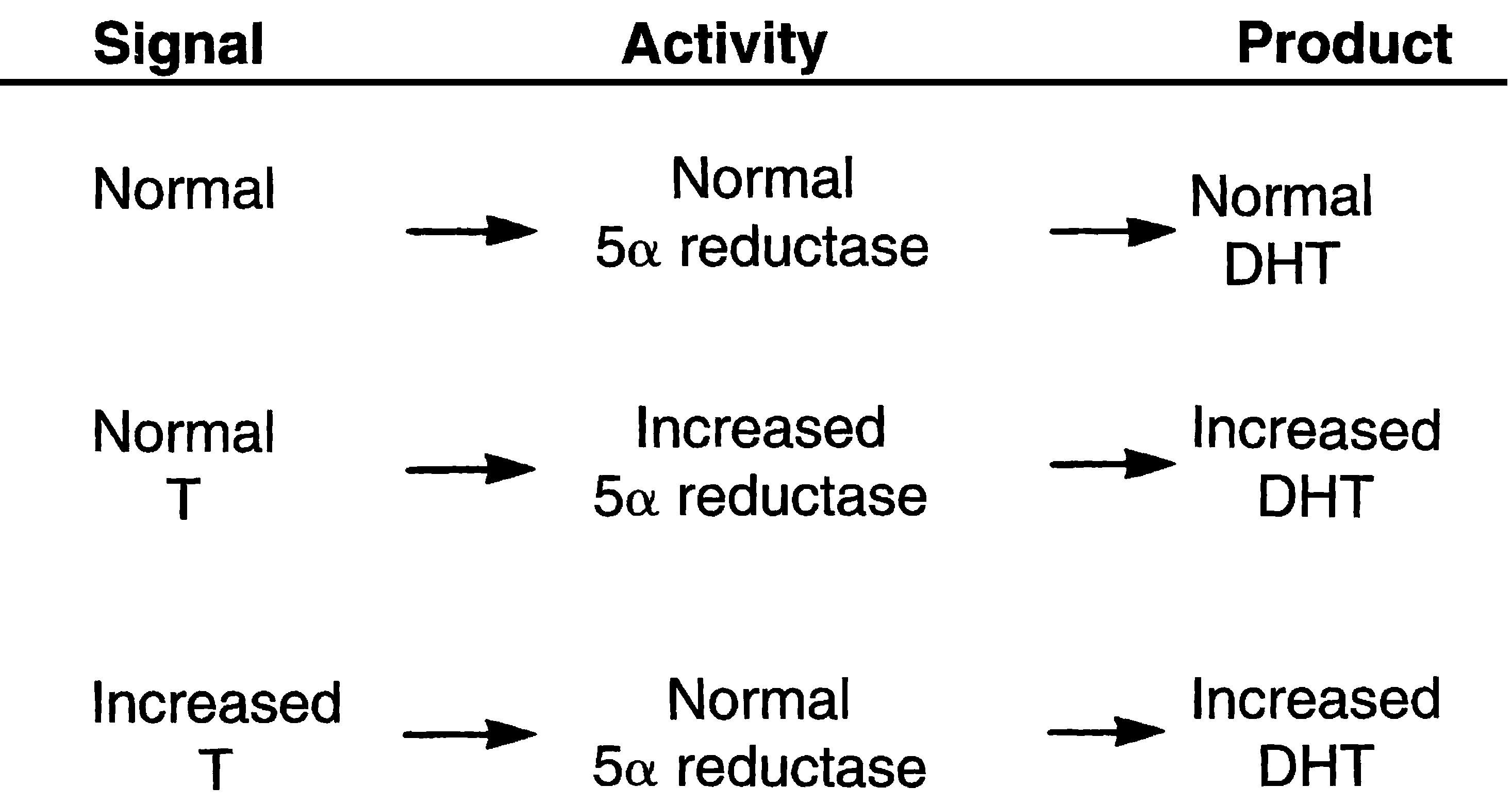
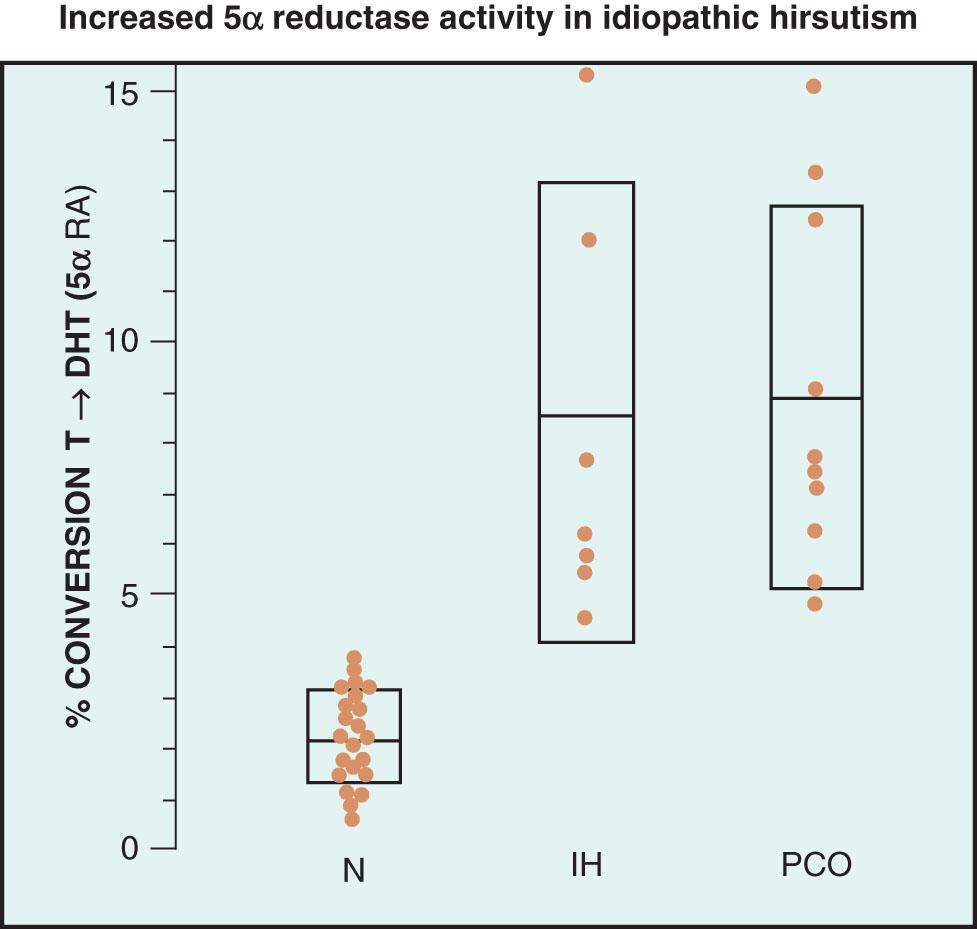
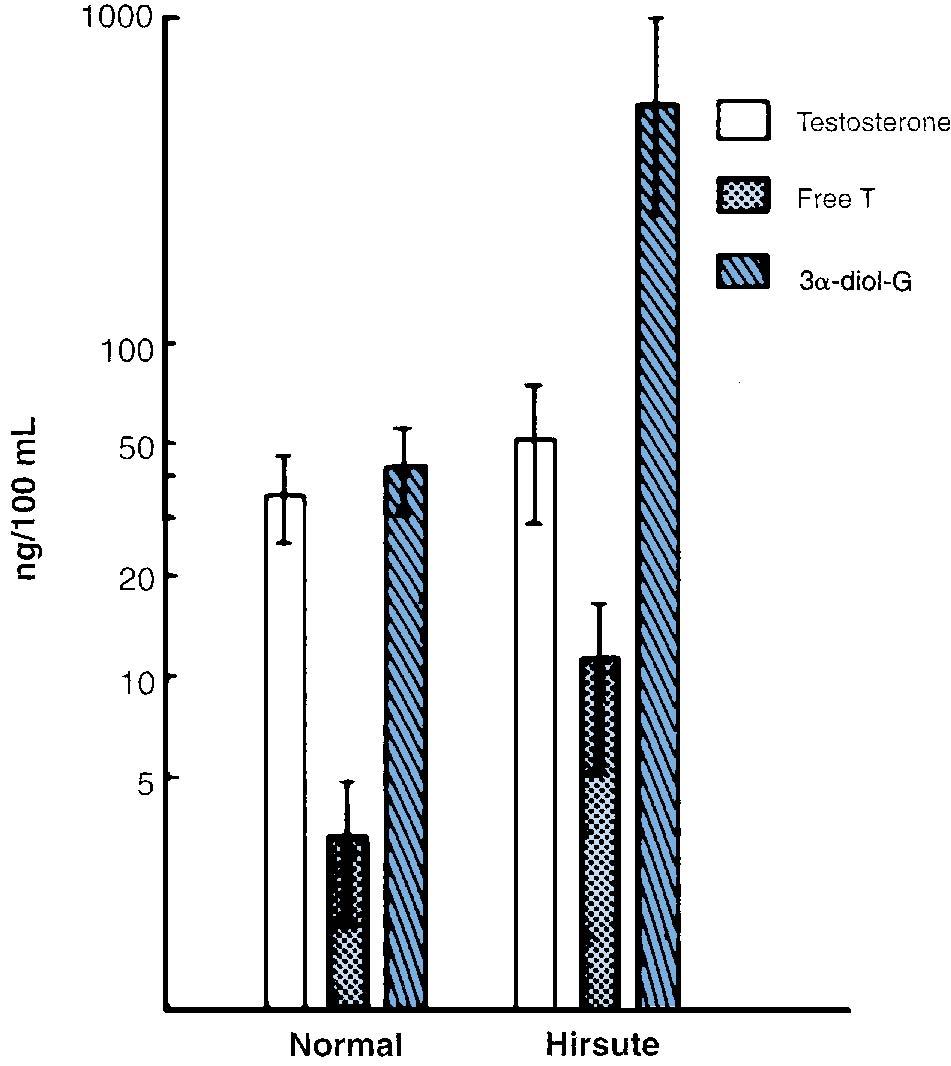
Even with normal circulatory levels of androgen, increased 5 α -reductase activity in the PSU results in increased androgenic activity, producing hirsutism ( ; ) ( Fig. 38.5 ). Measurements of 5 α -reductase activity in skin biopsies have found that the level of activity correlated well with the degree of hirsutism present ( ). The activity level is elevated in “idiopathic” hirsutism, where circulating levels of androgens are thought to be normal ( Fig. 38.6 ). The degree of 5 α -reductase activity can be measured in skin biopsy specimens by a variety of methods. This technique is only used for investigational purposes; if necessary for diagnostic reasons, 3 α -diol-G levels can be directly measured in serum. We have found that the measurement of this metabolite is the most accurate indicator of the degree of peripheral androgen metabolism in women, as long as the level of glandular production (testosterone) is appreciated. Although serum levels of total testosterone are similar in normal and hirsute women, there are significant differences in 3 α -diol-G ( ) ( Fig. 38.7 ). In general, whereas non–SHBG-bound testosterone has been found to be elevated in approximately 60% to 70% of hirsute women, levels of 3 α -diol-G have been found to be elevated in more than 80% of women in this setting.
In summary, there are three markers of androgen production in serum, one for each compartment in which androgens are produced ( Table 38.2 ). These measurements best reflect the area of interest, although it is clear that each compartment also produces other hormones. Interpretation of levels of 3 α -diol-G is controversial because these levels are highly dependent on circulating levels of precursor androgens, such as testosterone and also androstenedione. A reasonable argument may be that if testosterone and DHEAS are normal but there is significant hirsutism, then measuring 3 α -diol-G may not be necessary and one may merely assume a peripheral source of androgen excess. As suggested earlier, it is envisioned that in the future the measurement of 11-oxygenated androgens will be part of our armamentarium.
| Source | Marker |
| Ovary | Testosterone |
| Adrenal gland | DHEAS |
| Periphery | 3 α -diol-G |
Although most causes will result in hirsutism, each of the diagnostic categories can lead to any of the manifestations of androgen excess: acne, hirsutism, or alopecia. One common causative factor of signs of androgen excess is the administration of androgenic medication. In addition to testosterone itself, various anabolic steroids, 19-norprogestogens, and danazol have androgenic effects. Thus a careful history of medication intake is important for all women with hirsutism.
Hirsutism or virilization can also be associated with some forms of abnormal gonadal development. With this cause, individuals have signs of external sexual ambiguity or primary amenorrhea, in addition to findings of androgen excess, and a Y chromosome is often present.
Signs of androgen excess during pregnancy can be caused by increased ovarian testosterone production. This is usually caused by a luteoma of pregnancy or hyperreactio luteinalis . The former is a unilateral or bilateral solid ovarian enlargement; the latter is bilateral cystic ovarian enlargement. After pregnancy is completed, the excessive ovarian androgenic production resolves spontaneously and the androgenic signs regress.
A diagnosis of these three causes of androgen excess can usually easily be made by means of a careful history and physical examination. The remaining causes of androgen excess, together with the origin of hyperandrogenism, are listed in Table 38.3 . Details of each of these causes will be described. “Idiopathic” hirsutism and PCOS are the most common disorders, together making up more than 90% of cases. PCOS is the most common disorder, and because of its overall prevalence and importance among reproductive women, it is covered in detail in a separate chapter.
| Source | Diagnosis |
| Nonspecific | Exogenous, iatrogenic |
| Abnormal gonadal or sexual development | |
| Pregnancy | Androgen excess in pregnancy, luteoma or hyperreactio luteinalis |
| Periphery | Idiopathic hirsutism |
| Ovary | Polycystic ovary syndrome † |
| Functional or idiopathic hyperandrogenism ‡ | |
| Stromal hyperthecosis | |
| Ovarian tumors | |
| Adrenal gland | Adrenal tumors |
| Cushing syndrome | |
| Adult-onset congenital adrenal hyperplasia |
* Idiopathic hirsutism and polycystic ovary syndrome do not present with virilization.
† The hyperandrogenism in PCOS can also be of adrenal origin, at least in part.
‡ Functional hyperandrogenism may well be a type of PCOS, but without clearly defined polycystic ovaries on ultrasound, and can also have an adrenal source of hyperandrogenism.
Idiopathic hirsutism is diagnosed when there are signs of hirsutism and regular menstrual cycles in conjunction with normal circulating levels of androgens (both testosterone and DHEAS). Because this type of disorder is often present in certain families and ethnicities, it has also been called familial , or constitutional , hirsutism . Because neither ovarian nor adrenal androgen production is increased, the cause of the androgen excess has been called idiopathic hirsutism . Several studies have been done, where it has been documented that some women so diagnosed have subtle increases in androgen production and metabolism; however, the more important way to characterize this disorder, where androgens are normal or very slightly increased, is that there is an enhancement of androgen action in the PSU (i.e., an increased androgen sensitivity), which also has a familial predisposition. We have found that approximately 80% of these women have increased levels of 3 α -diol-G, indirectly indicating that the cause of hirsutism is largely the result of increased 5 α -reductase activity ( ). Also, we have directly measured the percentage conversion of testosterone to DHT in genital skin as an assessment of the 5 α -reductase activity (5 α -RA level) in the skin of women with idiopathic hirsutism. The amount of 5 α -RA was increased in hirsute women compared with normal women and correlated well with the degree of hirsutism and levels of serum 3 α -diol-G ( ). Thus idiopathic hirsutism is likely a disorder of the peripheral compartment and is possibly genetically determined, although it is also possible that early exposure to androgens can program increased 5 α -RA. Antiandrogens that block peripheral testosterone action or interfere with 5 α -RA are effective therapeutic agents for this disorder .
PCOS is the most common disorder diagnosed in women presenting with symptoms and signs of androgen excess. A survey taken in 2012 suggested that it accounts for 71% of women presenting with hirsutism ( ).
PCOS was originally described in 1935 by Stein and Leventhal as a syndrome consisting of amenorrhea, hirsutism, and obesity in association with enlarged polycystic ovaries ( ). The classic definition of PCOS includes women who are anovulatory and have irregular periods as well as hyperandrogenism, as determined by signs such as hirsutism or elevated blood levels of androgens, testosterone, or DHEAS. The diagnosis should only be made in the absence of other known disorders, including enzymatic disorders (e.g., 21-hydroxylase deficiency), Cushing syndrome, or tumors ( ).
As will be discussed in Chapter 39 , PCOS is also diagnosed in women with normal menstrual cycles, who are presumably ovulating, and in its widest spectrum of diagnostic categories is the most common reproductive disorder, occurring in 5% to 20% of all women of reproductive age.
For the purposes of understanding the interaction of androgen excess and PCOS, it should be appreciated that the most important feature of PCOS is that it is a hyperandrogenic disorder ( ). Although the majority of women will have an ovarian source of hyperandrogenism (i.e., an elevation in testosterone), adrenal hyperandrogenism (elevations in DHEAS) may be found in up to 50% of women ( ). In some women with PCOS and signs of hyperandrogenism (acne, hirsutism, or alopecia), blood levels of androgens may be “normal.” This most likely relates to the lack of sensitivity of current assays.
Because there are important aspects of PCOS that are prevalent (metabolic disease, fertility concerns, cancer risk, etc.) and because this disorder is extremely common in women of reproductive age, even though it may not be accurately diagnosed, a separate chapter ( Chapter 39 ) is devoted to this discussion.
Although most women with PCOS have elevated levels of circulating androgens, the presence or absence of hirsutism depends on whether those androgens are converted peripherally by 5 α -reductase to the more potent androgen, DHT, as reflected by increased circulating levels of 3 α -diol-G. Nonhirsute women with PCOS have elevated circulatory levels of testosterone, unbound testosterone, or DHEAS, but not 3 α -diol-G ( ).
This category is included because it may be found in other reviews in the literature and is more commonly diagnosed by European clinicians; it is considered to occur in up to 15% of women presenting with hirsutism ( ). It is diagnosed when androgens are elevated (either ovarian or adrenal) and menstrual cycles are regular and ovulatory. There is also no evidence on ultrasound for polycystic ovaries, making this an “idiopathic” state; however, it is our view that this category is really a variant of PCOS, in which women may be ovulatory, otherwise known as PCOS, phenotype C. Because ovarian morphologic type in women with PCOS is variable, this category may essentially be merged with PCOS.
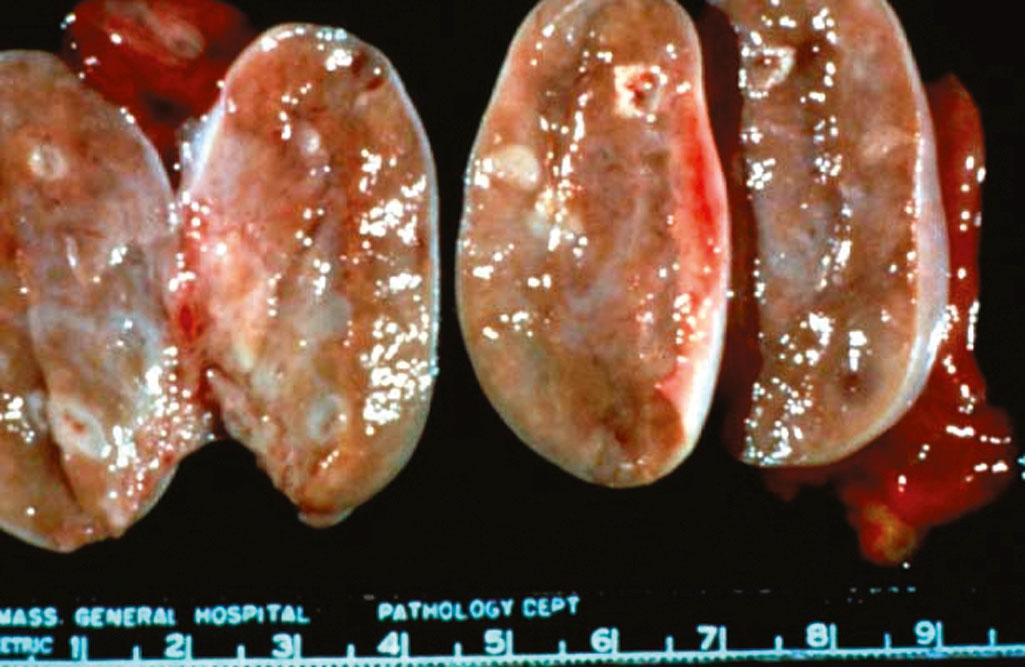
Stromal hyperthecosis is an uncommon benign ovarian disorder in which the ovaries are typically bilaterally enlarged to approximately 5 to 7 cm in diameter. Histologically, there are nests of luteinized theca cells within the stroma ( Fig. 38.8 ). The capsules of these ovaries are thick, similar to those found in PCOS, but, unlike in PCOS, subcapsular cysts are uncommon. The theca cells produce large amounts of testosterone, as determined by retrograde ovarian vein catheterization. The ultrasound picture of stromal hyperthecosis may be variable ( ). Like PCOS, this disorder has a gradual onset and is initially associated with anovulation or amenorrhea and hirsutism; however , unlike PCOS, with increasing age the ovaries secrete steadily increasing amounts of testosterone. Thus when women with this disorder reach the fourth decade of life, the severity of the hirsutism increases and signs of virilization , such as temporal balding, clitoral enlargement, deepening of the voice, and decreased breast size, appear and gradually increase in severity. By this time, serum testosterone levels are often in the range of 2 ng/mL, similar to levels found in ovarian and adrenal testosterone-producing tumors; however, with tumors, the symptoms of virilization appear and progress much more rapidly. Stromal hyperthecosis has also been found to be a cause of androgen excess in postmenopausal women. Here the ovaries are enlarged but not as large as in premenopausal women with the disorder; and testosterone levels are not as high.
Tumors are rare, occurring less than 1% of the time in women presenting with hyperandrogenism, but they represent the most important reason for evaluating women with androgen excess.
It is possible for almost every type of ovarian neoplasm to have stromal cells that secrete excessive amounts of testosterone and cause signs of androgen excess. Thus on rare occasions, excess testosterone produced by benign and malignant cystadenomas, Brenner tumors, and Krukenberg tumors have caused hirsutism, virilization, or both. Certain germ cell tumors contain many testosterone-producing cells. The testosterone produced by two of these neoplasms, Sertoli-Leydig cell tumors and hilus cell tumors, almost always cause virilization. In addition, lipoid cell (adrenal rest) tumors can produce increased amounts of testosterone, DHEAS, or both. Rarely, granulosa/theca cell tumors can also produce testosterone in addition to increased levels of estradiol.
Androgen-producing ovarian tumors usually produce rapidly progressive signs of virilization. Sertoli-Leydig cell tumors usually develop during the reproductive years (second to fourth decades) and, by the time they produce detectable signs of androgen excess, the tumor is almost always (>85% of the time) palpable during bimanual examination. These tumors are uncommon. Less than 1% of solid ovarian neoplasms are Sertoli-Leydig cell tumors. Hilus cell tumors usually occur after menopause. They are usually small and not palpable during bimanual examination; however, the history of rapid development of signs of virilization and the presence of markedly elevated levels of testosterone (more than 2.5 times the upper limits of the normal range), with normal levels of DHEAS, usually facilitate the diagnosis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here