Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
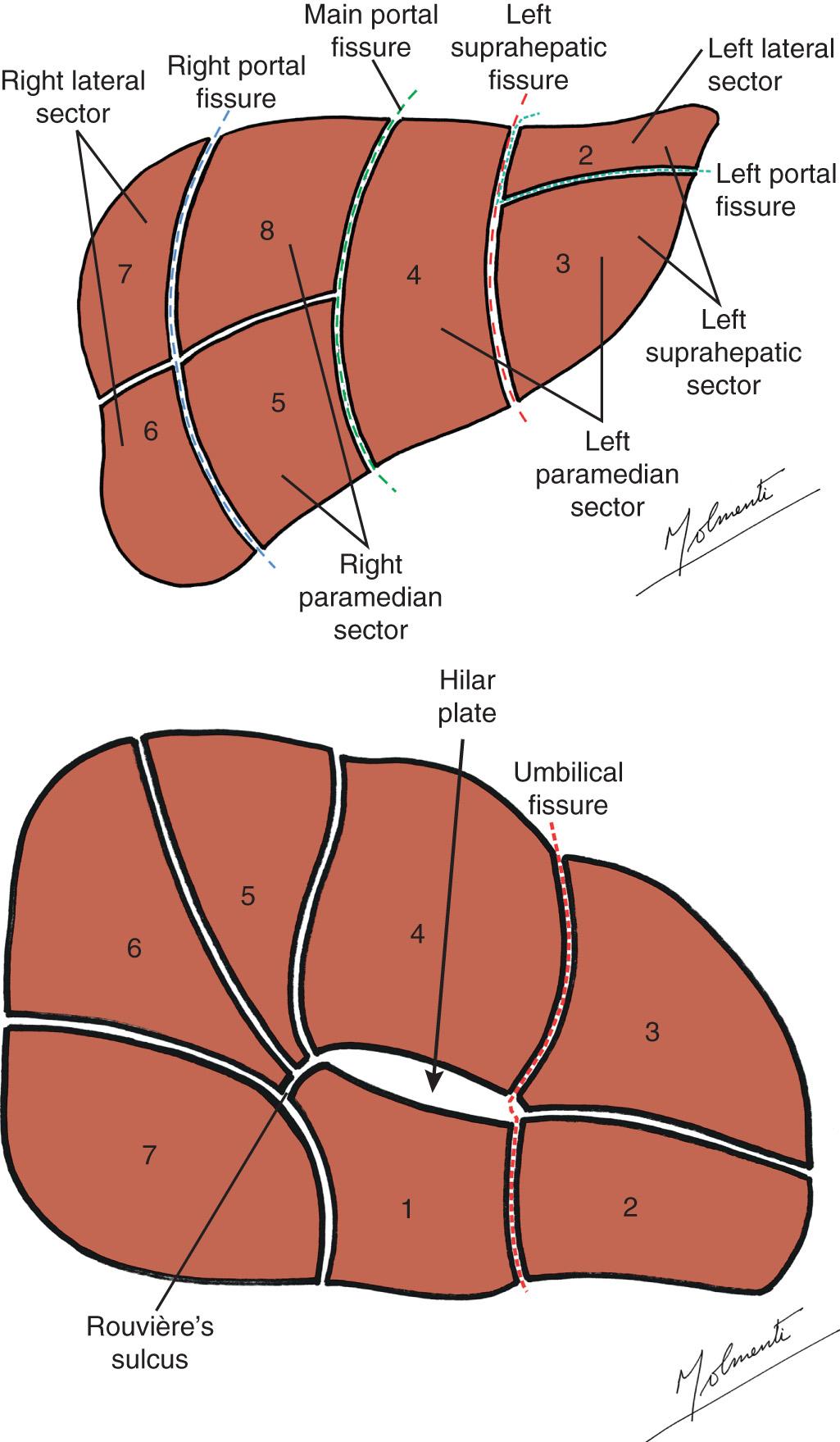
Our understanding of functional surgical hepatic anatomy evolved significantly through technical advances in repair of hepatobiliary injury, liver transplantation, hepatic resection, and radiologically guided intervention. This evolution was essential to the development of live-donor and deceased-donor segmental liver transplantation. Molmenti described this reconception of hepatic anatomy as derived from an anatomic-physiologic inside-out approach, as opposed to the purely topographic outside-in view of the past ( Fig. 118.1 ).
Human anatomy may be classified and is classifiable, but variation is the rule. This chapter reviews basic concepts of hepatic anatomy, with the important caveat that these simple concepts will not always hold true in all circumstances. There are now tools that allow the individual anatomy of the subject to be outlined preoperatively and intraoperatively in cases such as hepatic resection or live liver donation.
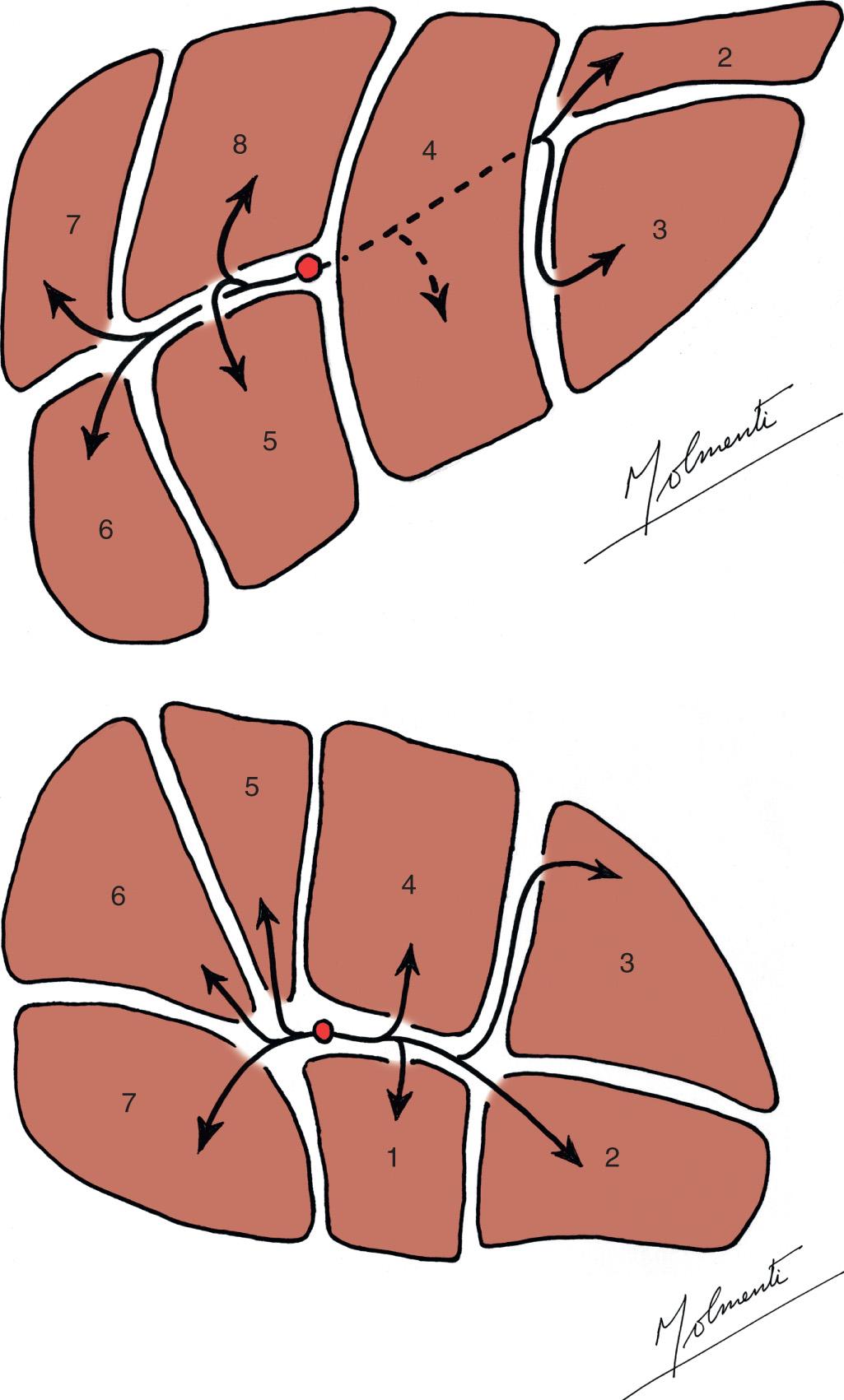
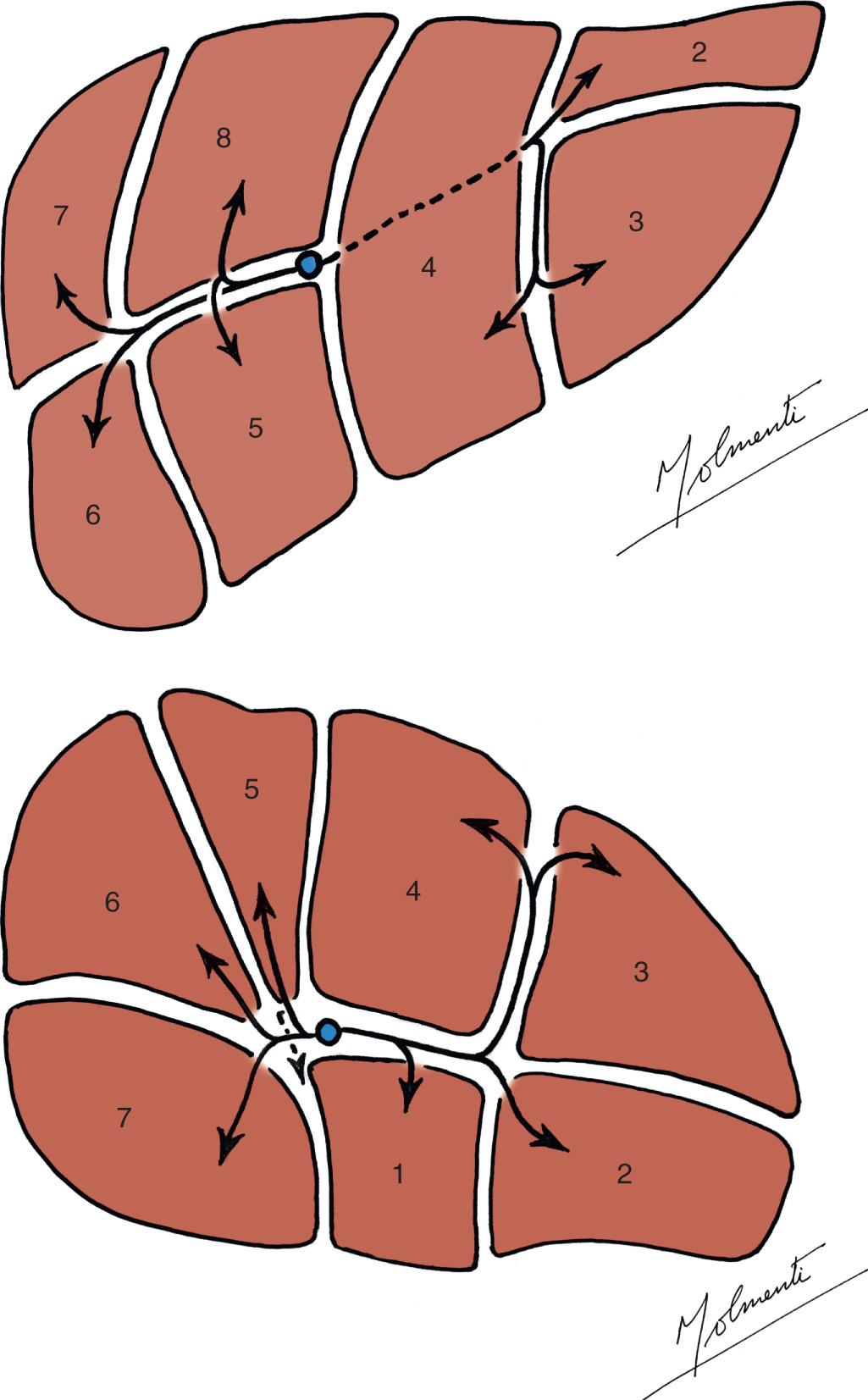
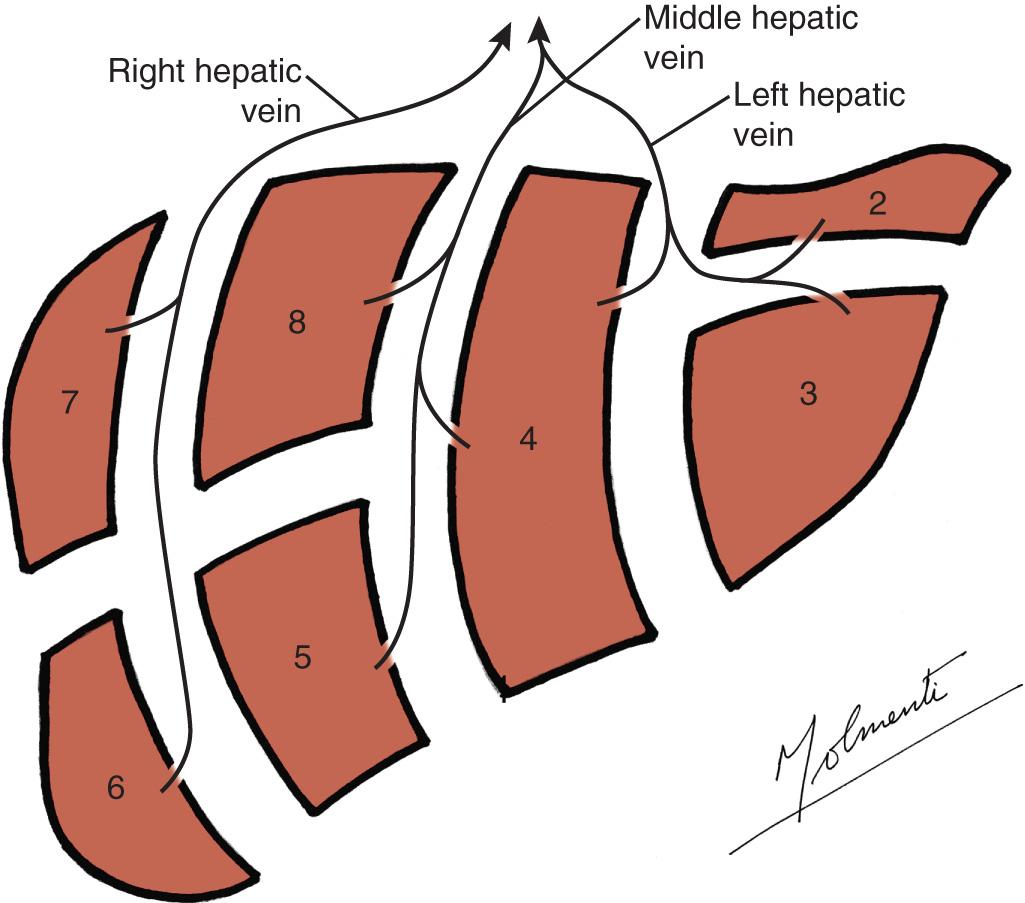
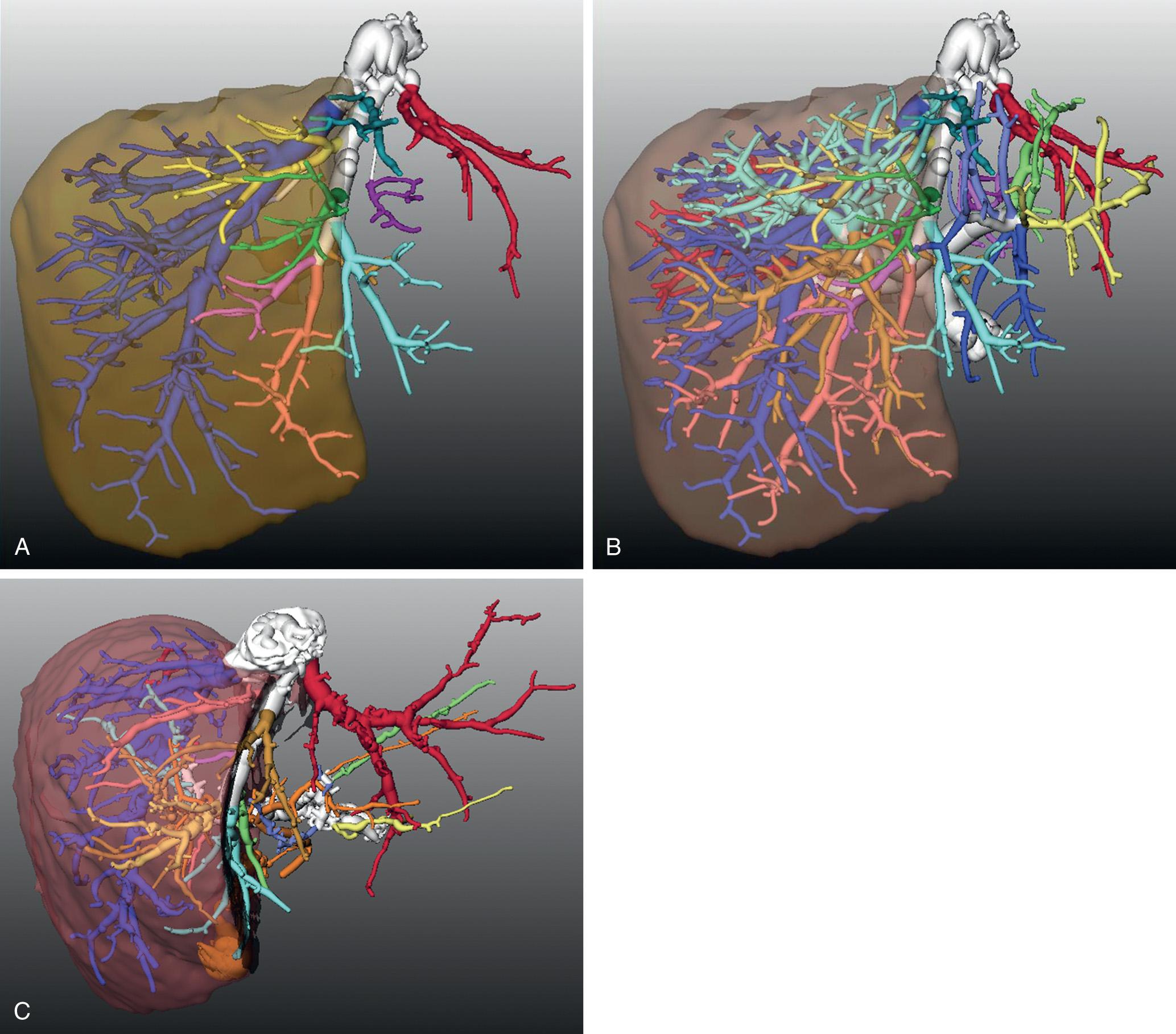
The liver is a single organ that can be functionally regarded as two hemilivers. The parenchyma can be further subdivided into several regions sharing common arterial, portal, and biliary supply and venous drainage. The portal and venous systems define these regions that are named sectors and segments, respectively ( Figs. 118.2–118.5 ). The liver has a rather constant anatomic pattern, the knowledge of which allows for a safe surgical approach. Nevertheless, there are some anatomic irregularities, and in particular instances, exact knowledge of the anatomy specific to the individual patient being examined or operated on is necessary (live donors, left extended or central hepatectomies, caudate lobe masses). In these cases a computed three-dimensional reconstruction of each anatomic detail is possible following an accurate computed tomographic or magnetic resonance imaging contrast scan. Several software packages are currently available that allow for the mapping of the individual anatomy, as well as for the calculation of volumes corresponding to the whole liver, liver sectors, and segments (Hepavision, MeVis-Germany, Hitachi-Japan, Hepavis-Slovenia, Université de Strasbourg-France). The reliability of virtual three-dimensional reconstructions based on standard anatomic landmarks for both surgical planning and graft volume calculations has been demonstrated ( Fig. 118.6 ). For standard liver surgery, the operating surgeon should be familiar with the basic anatomic pattern of the liver and the most frequent variations that have been described.
The liver primordium, also known as diverticulum hepatis or liver bud, arises from endoderm in weeks 3 through 4 of embryologic development and invades the septum transversum, vitelline (omphalomesenteric) veins, and umbilical veins. Its connection to the embryologic duodenum (foregut) will eventually become the bile duct. Embryologically the liver receives blood from both portal and umbilical veins, themselves connected by the left portal vein. Although the primitive portal veins arise from the caudal part of the vitelline veins, the primitive hepatic veins arise from the cranial part of the vitelline veins. In humans and many other mammals the inferior vena cava (IVC), ductus venosus, and umbilical vein are initially surrounded by liver parenchyma and become extrahepatic only in later stages of embryologic development. The arteries develop in conjunction with the bile ducts at a later period than the veins. On the right side, arteries and bile ducts follow the trajectory of the portal venous branches. On the left side, although arterial and biliary branching follows a symmetric pattern similar to that of the right side, the portal vein branches do not. During early stages of development, there are three hepatic arteries: (1) a left hepatic artery arising from the left gastric artery, (2) a middle hepatic artery arising from the celiac trunk, and (3) a right hepatic artery arising from the superior mesenteric artery. Although in most cases the middle artery is the only one that persists, variations in regression and origin of these three early arteries account for the so-called accessory and replaced variants. A complete ductal system is present by the 10th week of intrauterine life. The mesoderm of the septum between liver and abdominal wall develops into the falciform ligament . The surface of the developing liver in contact with the diaphragm is devoid of peritoneum, and the so-called bare area is a reminder of such association. By week 10 of development, the liver is involved in hematopoietic function, an activity that diminishes markedly during gestational months 8 and 9. By week 12 of development, the liver is already producing bile. However, hepatocytes only attain single-cell plate configuration by the age of 5 years. Several events take place at birth. The ductus venosus, which optimized venous return from the placenta to the fetus by connecting the left umbilical and common hepatic vein, closes and becomes the ligamentum venosus . Also at birth, the extrahepatic umbilical vein closes and becomes the ligamentum teres.
True anomalies of the liver are relatively infrequent. Prolongations of liver tissue from either the right (Riedel lobe) or left lobes usually present as incidental abdominal masses. In other instances, hepatic tissue connected by an isthmus to the liver is found in the chest. Small accessory collections of tissue attached to the liver by a pedicle are also occasionally encountered.
Several nomenclatures and topographic divisions have been proposed. According to Couinaud, the right and left hemilivers are supplied by first-order branches. Sectors are supplied by second-order branches. Segments are supplied by third-order branches. Subsegments are supplied by fourth-order or other branches. Segments are numbered in a counterclockwise fashion, from I to VIII. A main portal fissure, a right portal fissure, and a left portal fissure are grossly or conceptually defined because they may not always be anatomically present. Left and right paramedian sectors are adjacent to the main portal fissure. Left and right lateral sectors are located on the outer side of the corresponding paramedian ones (see Figs. 118.2–118.5 ). During our discussion, we follow this nomenclature with some modifications.
Couinaud referred to the vasculobiliary sheaths that envelop the portal elements as “the most important structure of liver anatomy.” They seem to have been described initially by Walaeus in 1640, and thus some have used the terms walaean pedicles or walaean sheaths . Glisson published his description of the liver “tunic” in 1642, and Laennec did so in 1803. The elements of the portal pedicle (hepatic artery, portal vein, bile ducts, nerves, and lymphatics) are surrounded throughout their trajectory to the parenchymal plates by connective tissue. Not so the hepatic veins. The hilar plate is located over the left and right pedicles, and the portal division, on the hilum of the liver. The umbilical plate is found in continuity with the hilar plate and the round ligament, covering the left paramedian pedicle in its upper surface. According to Couinaud and others, dissection of the hilar plate allows for the detachment of the hilar contents. Exposure of the umbilical plate is the gateway to the segmental and sectoral pedicles of the left liver. Because dissection at the level of the plates can lead to complications, an approach to the sheaths is recommended. This strategy has been applied by Lazorthes et al. in the so-called suprahilar approach for anatomic hepatectomies and segmentectomies. Sheaths originate at the right edge of the hilum, at the umbilical plate, and at the posterior margin of the hilar plate. From these sites they will reach the right liver, the left liver, and the caudate area, respectively. In cases of narrow hila or hila of difficult access, consideration should be given to dividing the anterior portion of the main portal fissure. This maneuver does not damage any structures of significance and allows better exposure of the hilar elements.
Couinaud recognized the following three types of approaches to a portal pedicle :
Intrafascial—dissection within the sheath, where the elements are identified
Extrafascial—dissection around the pedicle sheath
Extrafascial and transfissural—dissection of the sheaths at their origin from the hilar and umbilical plates (considered the safest approach, especially for second- and third-order branches)
According to Couinaud and Houssin, the most frequent arterial and biliary configurations, accounting for almost 90% of cases in their series, are the following :
A unique artery and bile duct on right and left (24%)
Two right bile ducts (17%)
Two left arteries (26%)
Two right ducts and two left arteries (22%)
Bile ducts are usually located above the portal branches and arteries below the corresponding veins. The bile ducts derive their blood supply predominantly from arterial branches. However, preliminary results from our observations in live-donor liver transplantation would point to some differences in the classically accepted (see Fig. 118.3 ) anatomic similarities among arteries and bile ducts.
Molmenti et al. noted that “the occurrence of (arterial) variants that differ from the usual pattern is both surprisingly common and unpredictable.” Such findings are especially relevant not only in liver transplantation but in all types of hepatobiliary surgery. When addressing arterial polymorphism and nomenclature, it is essential to keep in mind the embryologic reality that the liver has a tripartite arterial supply during developmental life. Although all these structures may not be patent in adulthood, vestigial remnants such as fibrous bands will always be encountered by the hand and sight of gifted surgeons.
The common hepatic artery originates from the celiac trunk in more than 80% of cases. In 5% of instances, there is a replaced common hepatic artery , most frequently arising from the superior mesenteric artery. In approximately 10% of cases, there is an absent common hepatic artery . In such instances the right and left hepatic arteries originate independently.
The right hepatic artery originates from the proper hepatic artery in more than 80% of cases. In approximately 15% to 20% of cases, there is a replaced right hepatic artery that arises in most instances from the superior mesenteric artery. In slightly more than 5% of individuals, there is an accessory right hepatic artery that may arise from the superior mesenteric artery. The right hepatic artery crosses underneath the common hepatic duct in 65% of cases, anterior to it in approximately 10% of cases, and underneath the common bile duct in approximately 10% of cases.
The left hepatic artery arises from the hepatic artery proper in more than 80% of instances. In approximately 15% to 20% of cases, there is a replaced left hepatic artery that most frequently may arise from the left gastric artery, celiac axis, or replaced common hepatic artery. An accessory left hepatic artery may be seen in up to 35% of individuals. Finding such vessels is of help during surgical interventions. Replaced and accessory left hepatic arteries can usually be detected by palpation of the gastrohepatic ligament. Replaced and accessory right hepatic arteries can be identified by palpating the posterior right portion of the hepatoduodenal ligament, with one finger inserted into the foramen of Winslow. The most frequent left-sided arterial distribution is a common trunk formed by the arteries of segments III and IV, which is joined by the artery of segment II. When the latter enters the former near the left-right bifurcation, the left hepatic artery is short. When the entrance occurs at the bifurcation or at the hepatic artery proper, there is a duplication of the left hepatic artery. The hepatic artery is rarely involved by severe atherosclerotic changes, even in elderly individuals.
The left hepatic duct drains segments II to IV. It is formed by the junction of ducts from segments II and III into a common trunk that is subsequently joined by the duct from segment IV (see Fig. 118.3 ). Duct IV usually joins at the umbilical fissure or somewhat to its right. In most cases the left hepatic duct lies in the most superior location of the left portal pedicle. The most frequent left biliary distribution is a common trunk from segments II and III that is joined by that of segment IV. In cases in which duct IV joins late, it may form the upper edge of the left portal pedicle. In a very small number of cases the ducts from the left paramedian sector (segments III and IV) may themselves form a trunk, which is joined by the duct of the left lateral sector (segment II) and the caudate lobe (segment I), or the duct from segment IV enters the confluence of the other ducts or the common duct itself. Such variations may lead to the finding of a short left hepatic duct (approximately 17% of cases) or a double left hepatic duct (approximately 12% of cases). The left duct has a classic configuration in almost 70% of cases. Biliary drainage may be achieved by performing a bilioenteric anastomosis to the left hepatic duct at the hilum or to ducts III or IV by accessing them at the umbilical fissure (Hepp-Couinaud operation). Variations in anatomic patterns should be kept in mind.
The right hepatic duct is present in slightly more than 50% of cases (see Fig. 118.3 ). It is harder to reach than its left counterpart, is usually short, and may even be missing in cases of an early second-degree bi-trifurcation (or division). It drains segments V to VIII. The duct draining segments VI and VII has a horizontal trajectory. The duct draining segments V and VIII has a vertical course.
The caudate lobe has its own bile drainage.
The confluence of the hepatic ducts is observed in front of the portal bifurcation in 57% of cases, in front of the left portal vein in 37% of cases, and in front of the right portal vein in 6% of cases. Isolated segmental or subsegmental bile ducts, usually arising from segments I, IV, and V, can lead to biliary fistulas after interventions in the hilar region. The confluence of the right and left hepatic ducts is described as following a normal configuration in approximately 70% of cases. Other possible configurations and their approximate incidences include trifurcation with left, paramedian and lateral right ducts (10%), right sectoral duct merging into the common bile duct (20%), and right sectoral duct joining the left duct (5%).
The left portal, left paramedian, left lateral, and right paramedian veins are constant structures within the liver architecture. The absence of the bifurcation of the portal vein can be an extremely dangerous situation. In such cases the portal vein follows a curvilinear trajectory within the liver, arching from right to left, and giving off collateral branches along the way until it reaches the caudate lobe. Ligation of the presumed right portal vein branch leads to complete interruption of portal blood into the liver. The classically accepted portal venous branching is illustrated in Fig. 118.4 .
Couinaud reminded us that “ hilum meant in Latin a tiny black point seen in beans” and that anatomists in antiquity referred to that region as porta hepatis , or gateway of the liver. It contains the bifurcation of the portal elements, with the short right and the long left branches. In approximately 23% of cases the right portal vein is not present but rather is replaced by two sectoral branches. In 47% of cases the right hepatic duct is not present as such.
The location of the main portal fissure, described by Rex, may vary (see Fig. 118.2 ). It is identified by the posterior extremity of the cystic plate and, in cases of normal right portal vein anatomy, tends to be located to the right of the portal vein, less frequently at the site of the bifurcation of the portal vein, or even less frequently to its left. In cases of right portal vein variants the fissure is almost always at the level of the bifurcation or at the left portal vein. Its topographic location on the liver is not outlined by superficial markings in humans and can be traced from the gallbladder fossa to the left anterior surface of the IVC. Furthermore, it has been noted that when the main portal fissure lies on the left, the biliary confluence is located in more than 70% of cases in front of the left portal vein.
The hilar plate (see Fig. 118.2 ) is detached from the liver parenchyma by dissecting in between the left portal pedicle and liver tissue. The left hepatic duct is the structure located in the superior aspect of the portal elements. No major vessels or biliary ducts are encountered in this pathway. Only in the posterior region are there branches to the caudate lobe.
The umbilical fissure and plate (see Fig. 118.2 ) is the site of origin of segmental and sectoral pedicles to the left liver. Its anatomic landmarks are the falciform ligament and the left longitudinal sulcus. The left paramedian pedicle and the umbilical plate can be identified by following the round ligament in continuity with the left portal vein. No walaean pedicles cross the umbilical fissure. This structure divides the left lobe from the rest of the liver and is a landmark point for the evaluation and performance of left lobectomies and trisectorectomies (trisegmentectomies in the classic diction).
The sulcus of Rouvière is an irregular fissure in continuity with the right hilum (see Fig. 118.2 ). It represents the extrahepatic anatomic landmark of the right fissure, usually buried in liver parenchyma. Following this structure leads to the pedicles of segments V and VI and further deeply and posteriorly to the pedicles of segments VII and VIII. The maneuver of isolating these structures is advantageous in the difficult procedures of right sectorectomy (segments VI to VII resection) or left trisectorectomy (trisegmentectomy) (segments I-II-III-IV-V-VIII resection).
The right paramedian portal pedicle is, according to Couinaud, “one of the most constant vessels of the liver.”
The parabiliary venous system of Couinaud is an accessory venous system with collateral branches to the duodenum, pancreas, and stomach, located within the hilar plate. It is associated with liver parenchyma, especially in the caudate and quadrate lobes, as well as with cystic veins. It may act as a collateral pathway in cases of portal hypertension and may serve as a connection between the right and left livers.
The cystic vein(s) usually drain into the right portal vein but may also drain into the right liver, the left liver, and/or enter the parabiliary venous system.
In 20% to 50% of cases, small ducts that are not part of a portal pedicle and do not communicate with the gallbladder are encountered in the cystic fossa. These ducts, described by Luschka, represent part of the “vasa aberrantia.” They are different from the cystohepatic ducts , which are true biliary ducts that traverse from liver tissue to the gallbladder.
There are three main hepatic veins that drain into the IVC (see Fig. 118.5 ): the right hepatic vein (RHV), middle hepatic vein (MHV), and left hepatic vein (LHV). Accessory, inferior, right inferior, right middle, or dorsal hepatic veins also drain directly into the IVC. The MHV and LHV show a relative lack of anatomic diversity, whereas the RHV exhibits multiple variants.
In most cases the RHV is single; rarely, it is double. In more than 50% of cases, it has no tributaries within 1 cm of its entrance into the IVC. In such cases, it is possible to ligate it before parenchymal transections. In the other variants, attempts to ligate it may lead to profuse bleeding and potentially air emboli in cases where injuries occur.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here