Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acromioclavicular joint injuries are among the most common shoulder injuries. Classification and indication for surgical or nonsurgical treatment are based on clinical and radiologic findings. Recent surgical techniques allow for anatomic reconstruction of the unstable joint.
Classification is based on both clinical and radiologic examination findings.
High-grade injuries—typically types IV, V, and VI, with greater than 100% displacement in either a posterior or inferior direction—are typically treated surgically.
The Conoid and Trapezoid are important but the acromioclavicular capsule functions similar to the glenohumeral joint
Surgical techniques should aim toward anatomic reconstruction of the acromioclavicular and coracoclavicular ligaments.
Surgical techniques should also aim to reduce posterior rotation at the AC joint properly.
Include the sternoclavicular joint in the operative field to allow wide exposure.
Bump is placed under the scapula to elevate the body away from the bed for better access to the posterior clavicle
Perform a glenohumeral arthroscopy to evaluate for possible associated glenohumeral lesions.
Instead of repositioning the head, the clavicle can be displaced anteriorly with a towel clip to allow access for conoid tunnel drilling.
The skin incision is over the coracoid process, more medial than usual (not over the acromioclavicular joint).
The medial skin incision allows for direct visualization of the coracoclavicular ligament and coracoid process.
Tag the deltoid and trapezial fascia for good repair. The deltoid has two attachments on the clavicle. One is superior and one is inferior. Both are important.
If sutures are passed laterally to medially, make sure the medial coracoid base is exposed and position a Darrach retractor on the medial base to “catch” the passing device.
The bone tunnels are reamed under power. Do not power-spin the reamer out to avoid tunnel widening.
The bone mineral density in the lateral third of the clavicle progressively increases from lateral to medial. The optimal bone density is located at the anatomic insertion area of the CC ligaments between 20 and 50 mm medially from the lateral end of the clavicle
The conoid ligament is placed approximately 45–50 mm medial from the distal end of the clavicle at the conoid tubercule and the posterior aspect of the clavicle.
The conoid tubercle on the inferior surface of the lateral third of the clavicle can be used as an anatomic landmark for the tunnel placement
The bone tunnel for the trapezoid ligament is centered on the clavicle in an anteroposterior dimension, approximately 15–20 mm lateral to the center of the previous tunnel, but definitely 25–30 mm medial to the AC joint
The graft is cyclically loaded multiple times
The 5.5 × 8 mm polyetheretherketone (PEEK) screws are inserted into a 5.5-mm bone tunnel (line to line).
Insert the screw anterior to the graft to adequately recreate the posteriorly positioned coracoclavicular ligaments.
A postoperative platform brace (Lehrman) is prescribed for 6 weeks.
Nonanatomic tunnel placement resulting from improper patient positioning and surgical exposure
Difficult graft passage because of improper graft preparation
Insufficient repositioning of the joint in chronic cases because of soft tissue or scar tissue interposition
Acromioclavicular (AC) joint separation represents one of the most common shoulder injuries, with AC joint injuries accounting for 12% of all shoulder injuries in the overall population. The most common mechanism of this injury is a fall with a direct force to the lateral aspect of the shoulder and with the arm in an abducted position.
Depending on the magnitude of injury to the AC joint capsule and ligaments as well as to the coracoclavicular (CC) ligaments, these injuries can be classified by increasing severity as type I through type VI (according to Rockwood). , Typically, low-grade injuries such as type I or type II should be treated conservatively. Thus, current conservative management strategies show favorable outcomes, less complications and higher return to activity rates with a nonoperative treatment algorithm. , When facing high-grade injuries (types IV-VI), literature recommends surgery. , , No overall consensus exists on treatment for type III dislocations according to Rockwood’s classification, as clinical studies failed to show significant benefit for surgical interventions. Thus, a trend toward initial nonoperative treatment is presently favored in most cases, even though functional impairment due to scapular dyskinesia or chronic pain remains concerning following conservative treatment. Some of these conservatively treated patients will have persistent pain and an inability to return to their sport or job. Subsequent surgical stabilization, albeit delayed, has still allowed return to sport or work in such cases. However, consideration of other factors, such as type of sport, timing of injury relative to athletic season, position in which the athlete competes, or throwing demands, may alter the procedure. Of interest, no differences between operative and conservative treatment have been observed in terms of shoulder strength, pain relief, throwing ability, or development of osteoarthritis (OA). Contrary, better cosmesis and longer sick leave may occur with operative treatment.
The highly variable severity of type III injuries led to a consensus statement published by the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) to further subdivide type III injuries, to more accurately indicate patients who may benefit from surgery : type IIIA injuries are considered stable without overriding of the clavicle on the cross-body adduction view and without significant scapular dysfunction, whereas type IIIB injuries present with horizontal instability and therapy-resistant scapular dysfunction.
In light of the controversy and clear lack of evidence supporting acute surgical management of grade III AC separations, we recommend that all patients be treated initially with 3 to 6 weeks of nonoperative management. Unfortunately, 20% of these patients still present with scapular dysfunction, even after successful completion of conservative treatment. Thus, a patient with a grade III AC separation qualifies for surgical reconstruction after a failed short course of nonoperative management as defined by persistent symptoms.
AC joint repair has a long history. Since 1917, when Cadenet first introduced his technique for AC joint instabilities, over 150 different techniques have been described, whereas a few of these techniques have been abandoned or re-invented secondary to high complication and clinical failure rates. However, none of these has been proven as gold standard. Currently proposed surgical approaches can be separated into three categories: (1) anatomic reconstruction of the conoid and trapezoid ligaments, (2) nonanatomic methods including reconstruction of coracoclavicular (CC) ligaments without or (3) with hardware and nonanatomic open reduction with internal fixation. , Most of the current techniques focus on reconstruction of the CC ligaments in reference to anatomic studies emphasizing the biomechanical importance of the CC ligaments for vertical stability of repairs of the AC joint. From a biomechanical perspective, the importance of the CC ligaments and AC ligaments in controlling superior and horizontal translation of the distal clavicle has been elucidated. In the past decade, a trend towards arthroscopic-assisted techniques has been observed. Among these, anatomic techniques focus on reconstruction of both the conoid and trapezoid ligaments. However, improved horizontal stability may further be facilitated by a reconstruction of the CC ligaments in an early stage after injury with an approach of clavicle and acromion, allowing subsequent healing of the torn AC and CC ligaments. Alternatively, an additional reconstruction of the AC ligaments may be performed, and it is advantageous especially in chronic instabilities with decreased healing potential of the AC ligaments.
We advocate the use of a separate, more robust graft source, semitendinosus tendon rather than the coracoacromial ligament, and an anatomic procedure to achieve optimal postoperative results. The anatomic coracoclavicular reconstruction (ACCR) enables simultaneous reconstruction of the CC ligaments (trapezoid and conoid) and the AC ligaments for optimized restoration of biomechanical function. This technique restores function of both the CC ligaments and the AC ligaments in an anatomic procedure with the use of an allogenic or autologous tendon graft (semitendinosus). , ,
The pain associated with AC joint injury may be difficult to localize because of the complex sensory innervation of the joint. An acute injury as described earlier is an important indicator in the diagnosis. As the AC joint ligaments lose their potential to heal after 3 weeks following injury, the cut-off for acute injuries is less than 3 weeks. , Given an acute injury, it is important to determine the level of perceived pain, its location, and any history of previous shoulder injuries. During examination, the patient should be upright so that the weight of the arm helps exaggerate any deformities. If a patient has more pain than is expected for a simple AC joint injury, then there should be high suspicion for a coracoid fracture or a type IV injury with displacement of the clavicle through the trapezial fascia. An examination for neural, vascular, or additional injuries of the adjoining joints should always be completed. Particularly, intraarticular injuries such as lesions of the long head of the biceps tendon or SLAP lesions (superior labral anterior posterior lesions) have been reported to occur in almost 20% of high-grade AC joint dislocations.
Acute traumatic event versus chronic instability
Current pain, physical limitations, and disability
Failure of at least 3 months of conservative treatment
Age of the patient (physeal fractures)
Prior surgical procedures (distal clavicle resection)
Status post–distal clavicular fracture (not always obvious)
Posterior headache (nuchae)
AC joint examination
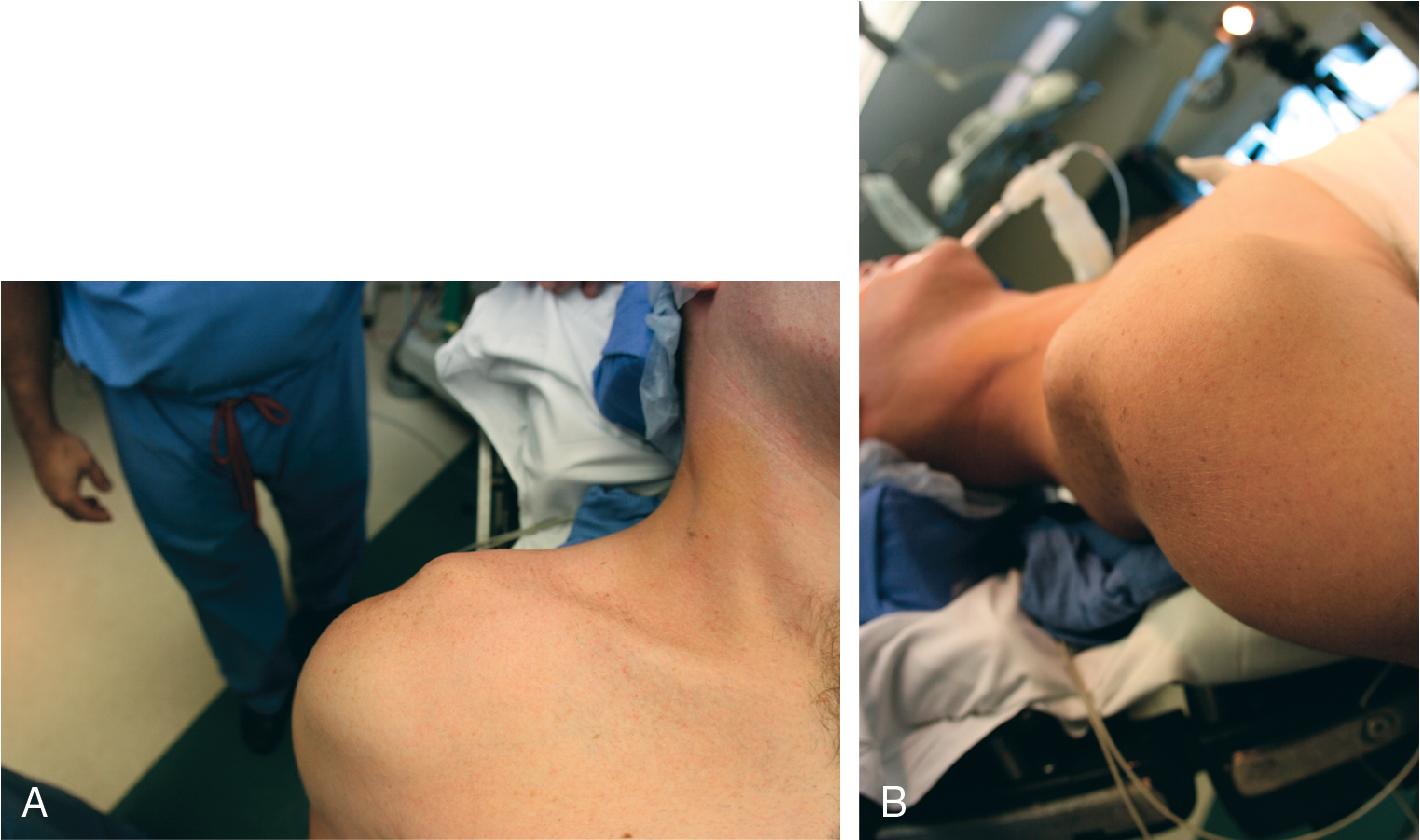
Inspection ( Fig. 38.1 )
Tenderness to palpation
Anterior-posterior translation or mobility
Superior-inferior translation or mobility
Reduction of the distal clavicle with shoulder shrug differentiates type III from type V (distal clavicle buttonhole through deltotrapezial fascia)
Range of motion
Arm positioning limitation
Inability to lift arm
Pain with forward elevation and wing out
Strength testing
Other causes of pain must be ruled out:
Cervical spine disease: trapezial spasm
Thoracic outlet syndrome
Scapular dyskinesis
Hyperlaxity
Coracoid fracture
Intra-articular co-morbidities
Traumatic skin lesions, prior surgeries, incisions
Standard imaging
Bilateral Zanca view: 10- to 15-degree cephalad tilt ( Fig. 38.2 )

(dynamic) Axillary, outlet, and anteroposterior views of the shoulder in the scapular plane
Additional imaging
Cross-arm adduction view: anteroposterior shoulder—measure clavicle override
Magnetic resonance imaging: labral injury masquerading as AC joint pain
Computed tomographic scan: nondisplaced lateral clavicle or acromion fracture or in revision cases
No absolute indications exist.
Type I and II lesions are generally treated conservatively.
Instability after distal clavicle excision.
Treat type III lesions initially with 3 to 6 weeks of nonoperative management. Reconstruction is advocated even for symptomatic type III injuries in laborers, throwers, and overhead athletes.
Operative treatment is generally the accepted method for complete AC joint injuries (types IV, V, and VI).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here