Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
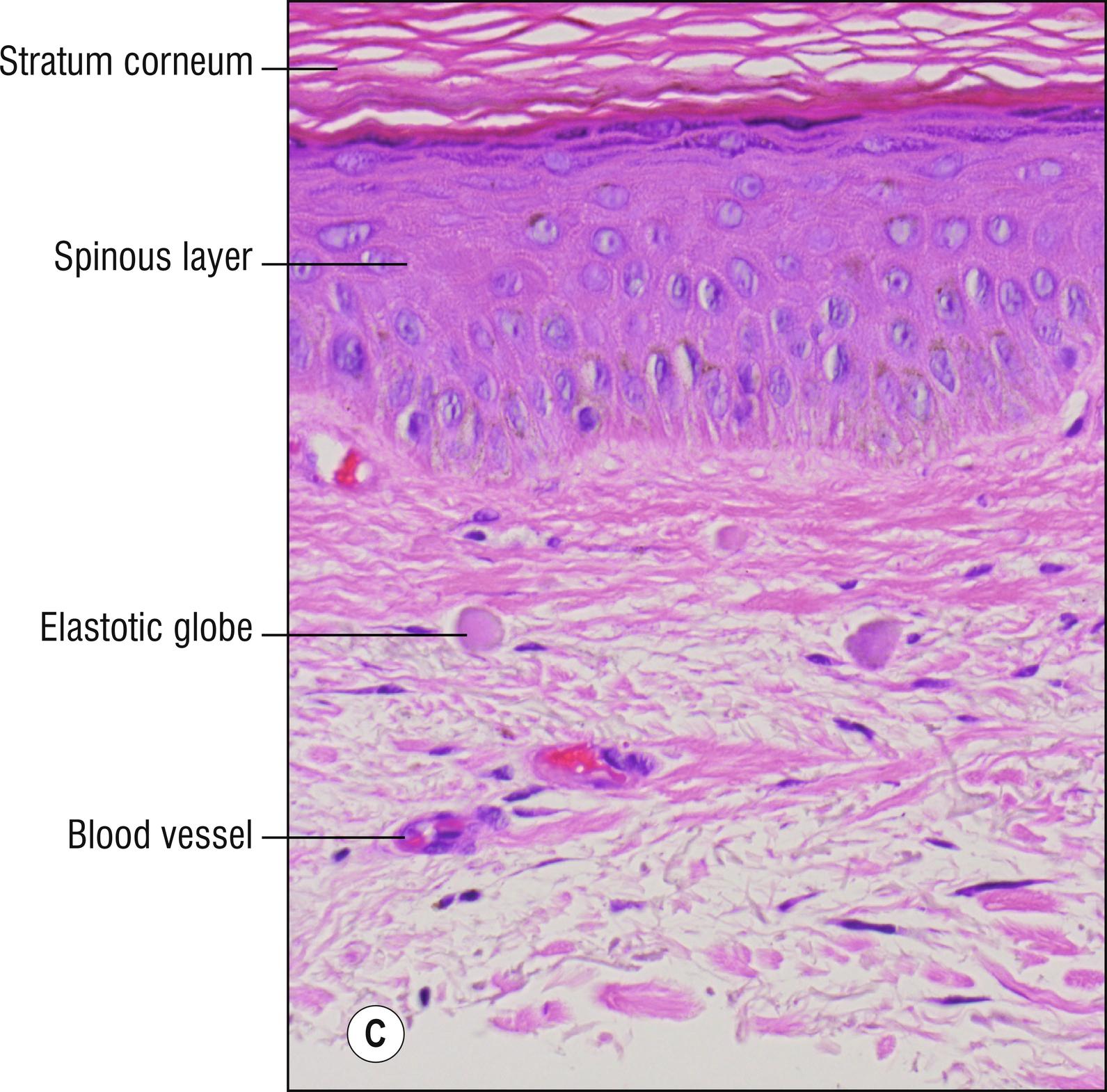
(see Fig. 9.1A,B )
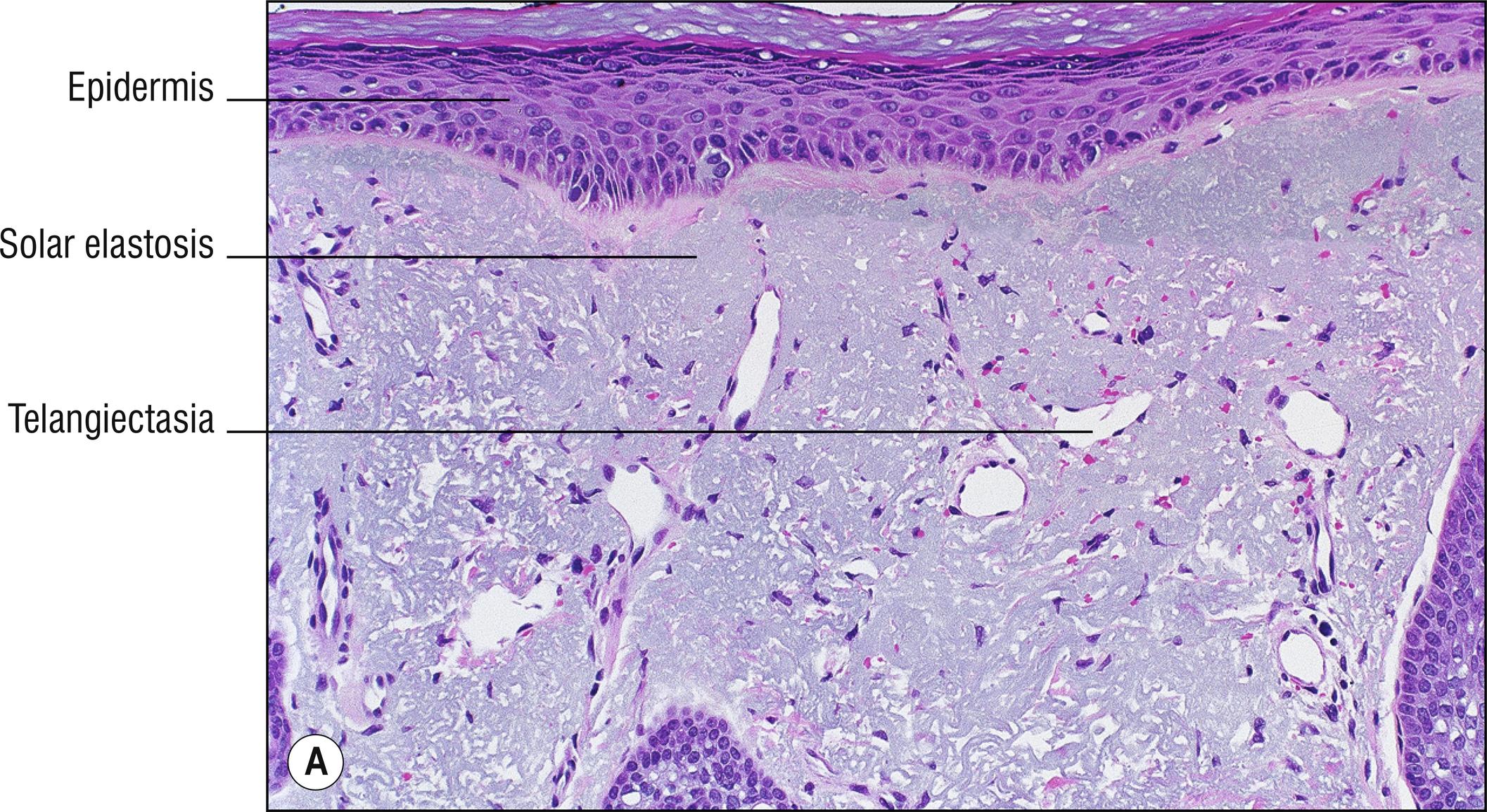
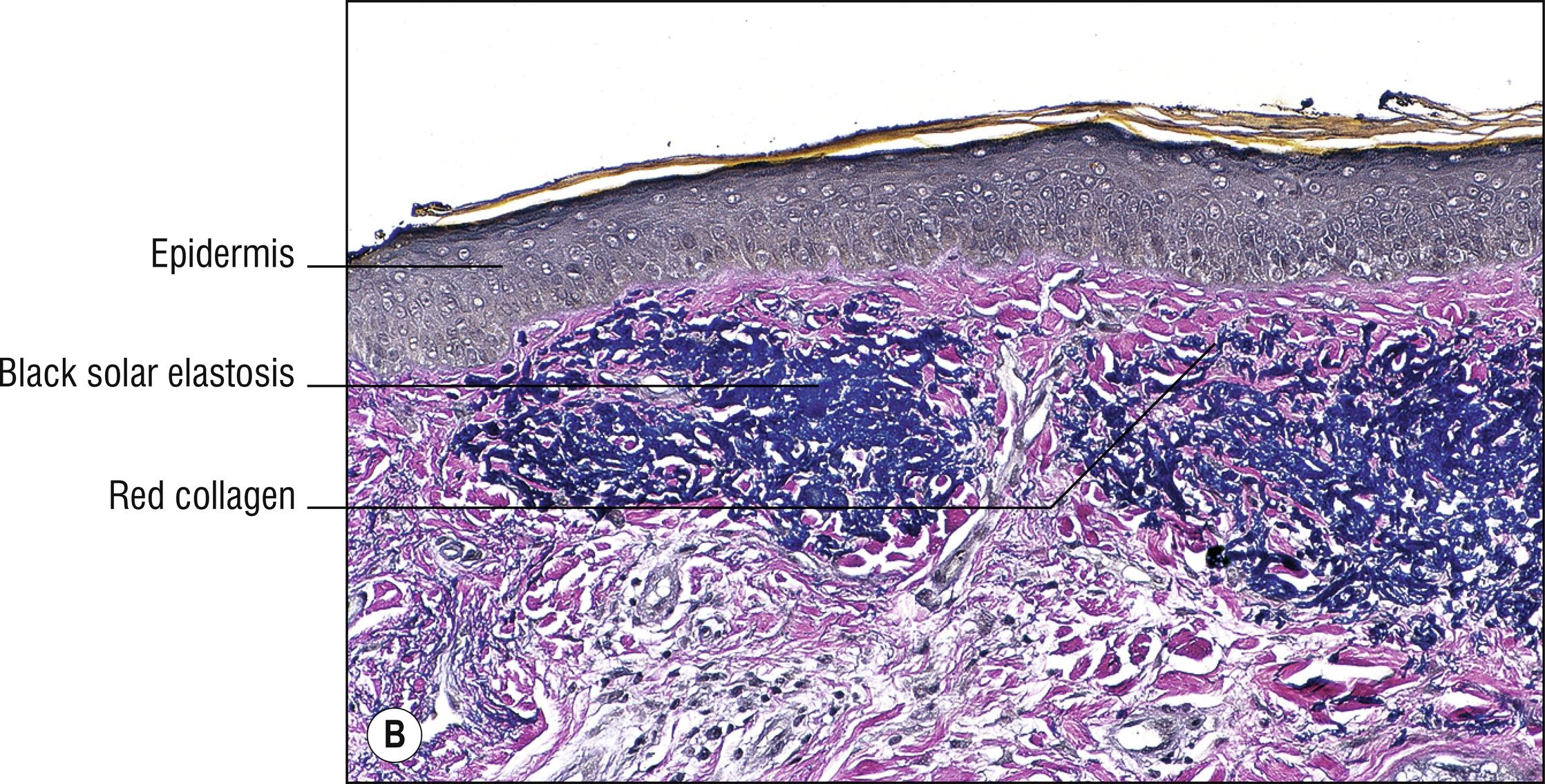
Very common parched or wrinkled skin due to sun damage (dermatoheliosis) with degeneration of connective tissue (increased abnormal elastic tissue and less collagen).
Amorphous, fibrous, or globular basophilic material in the dermis
Elastic fibers (1.31) become bluish–gray and stain positively with elastic tissue stains ( Chapter 30 )
Nodular colloid degeneration: papule or nodule of histologically clumped areas of solar elastosis, often resembling amyloid (8.4). Rarely found in non-sun-damaged areas.
Elastotic globes: small (less than 40 microns), round basophilic to eosinophilic blobs of elastotic material in the dermis ( Fig. 9.1C ).
Weathering nodules of the ears, elastotic nodules of the ears: firm papules on the ears, degenerated cartilage or elastic tissue, fibrosis, not painful like chondrodermatitis (17.9).
Favre–Racouchot syndrome: solar elastosis, cysts (19.1) and comedones (1.24), especially on the malar area.
Collagenous and elastotic plaques of the hands: linear plaques (1.73) along the sides of the hands, with degenerated elastic tissue, resembling acrokeratoelastoidosis (2.15, which is familial, has an earlier age of onset, and involves both hands and feet).
Other diseases with blue deposits (1.15), especially mucin (1.83): mucin is more stringy, smudged, or granular, while even in smudged areas of solar elastosis, individual bluish elastic fibers can be identified.
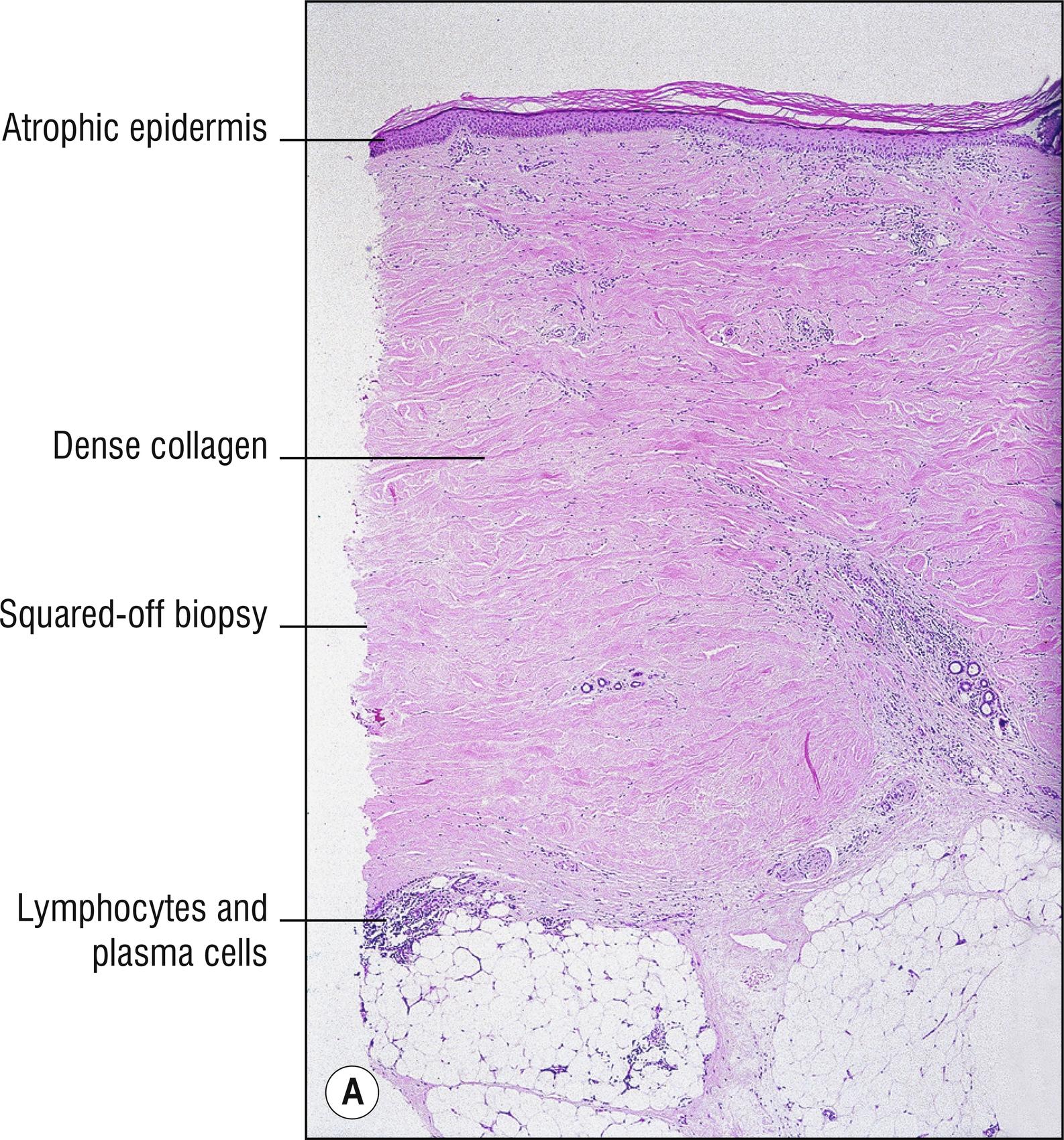
(see Fig. 9.2A,B )
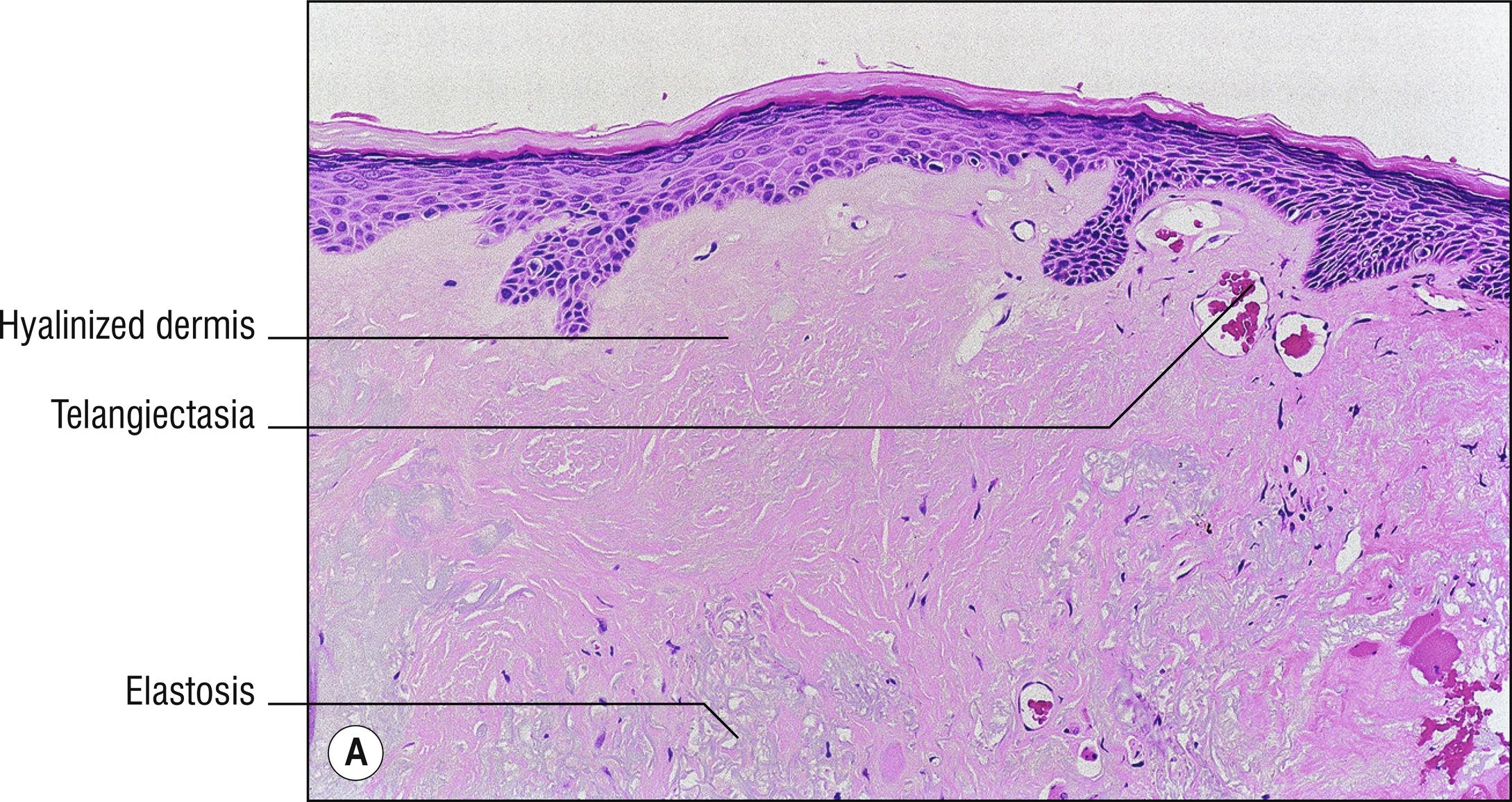
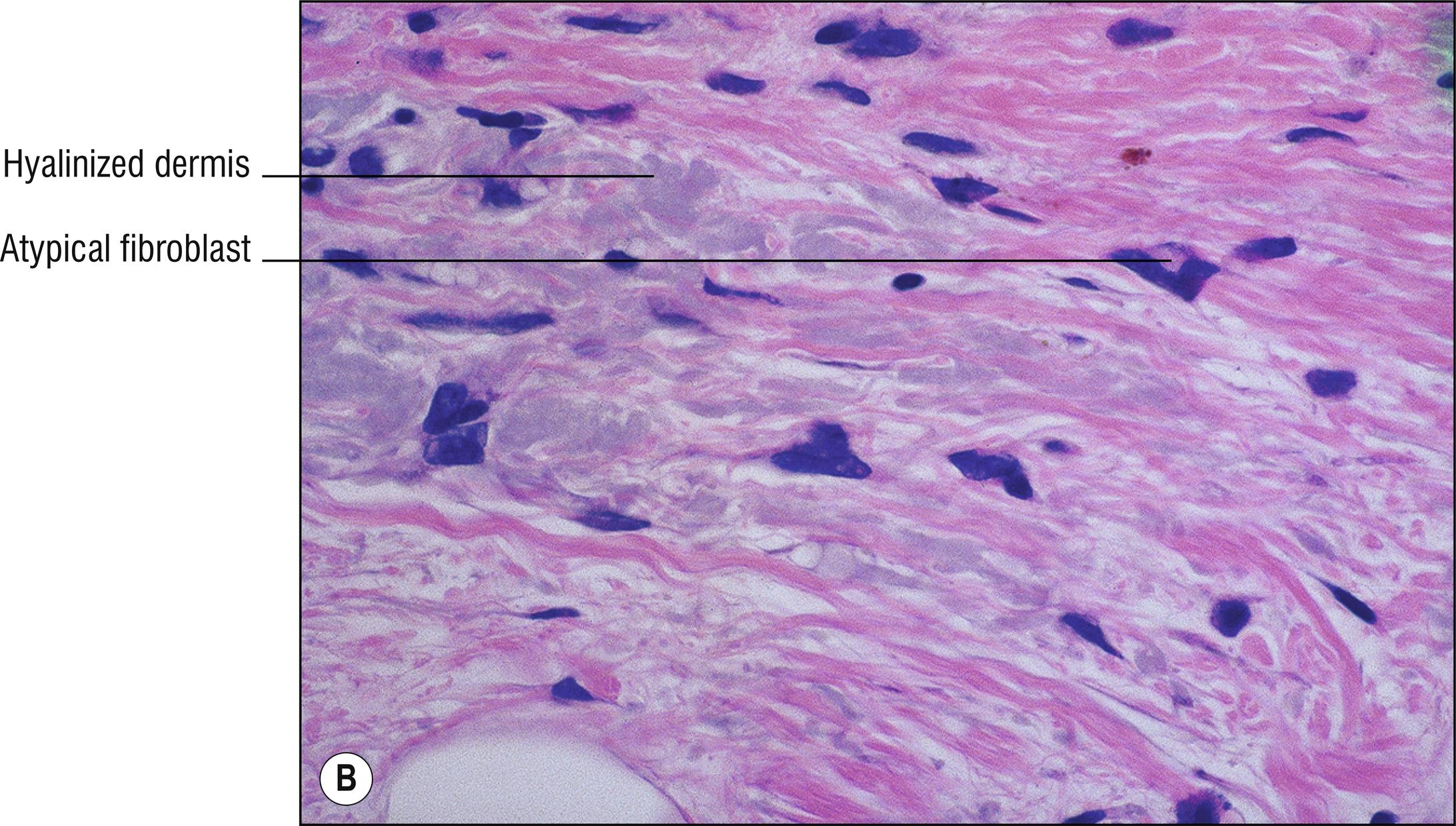
Acute radiodermatitis presents as red patches (1.121), sometimes with desquamation or blistering. Chronic radiodermatitis presents as atrophic (1.9) indurated plaques, often whitish (1.150) or yellowish (1.151), with telangiectasia (1.136), sometimes with hyperkeratosis (1.61), sometimes squamous cell carcinoma or sarcoma can develop years after exposure.
Pale (1.99), vacuolated (1.144), or necrotic keratinocytes (1.86)
Subepidermal blister (1.147) or ulceration (1.142) sometimes
Superficial dermal edema (1.30)
Endothelial proliferation, vascular dilation, thrombi (1.137)
Degeneration of dermal connective tissue
Epidermal hyperplasia (1.61) or atrophy (1.9), sometimes ulceration (1.142)
Keratinocytes pale (1.99), atypical, or necrotic (1.86)
Telangiectatic blood vessels, sometimes surrounded by hyperplastic rete ridges
Thrombi sometimes (1.137)
Decreased adnexal structures
Degenerated dermis (mainly hyalinized , sometimes basophilic)
Sometimes atypical, bizarre fibroblasts
Eosinophilic polymorphic pruritic eruption associated with radiotherapy (EPPER): papular, sometime vesicular, eruption that extends beyond area of radiotherapy, with spongiosis, superficial and deep lymphocytes, and eosinophils.
Other diseases with hyalinization (1.35) or dermal sclerosis (1.125), especially lichen sclerosus (9.5) and scleroderma (9.3).
Solar elastosis (9.1) and actinic keratosis (18.8): dermis more basophilic and degeneration not as deep.
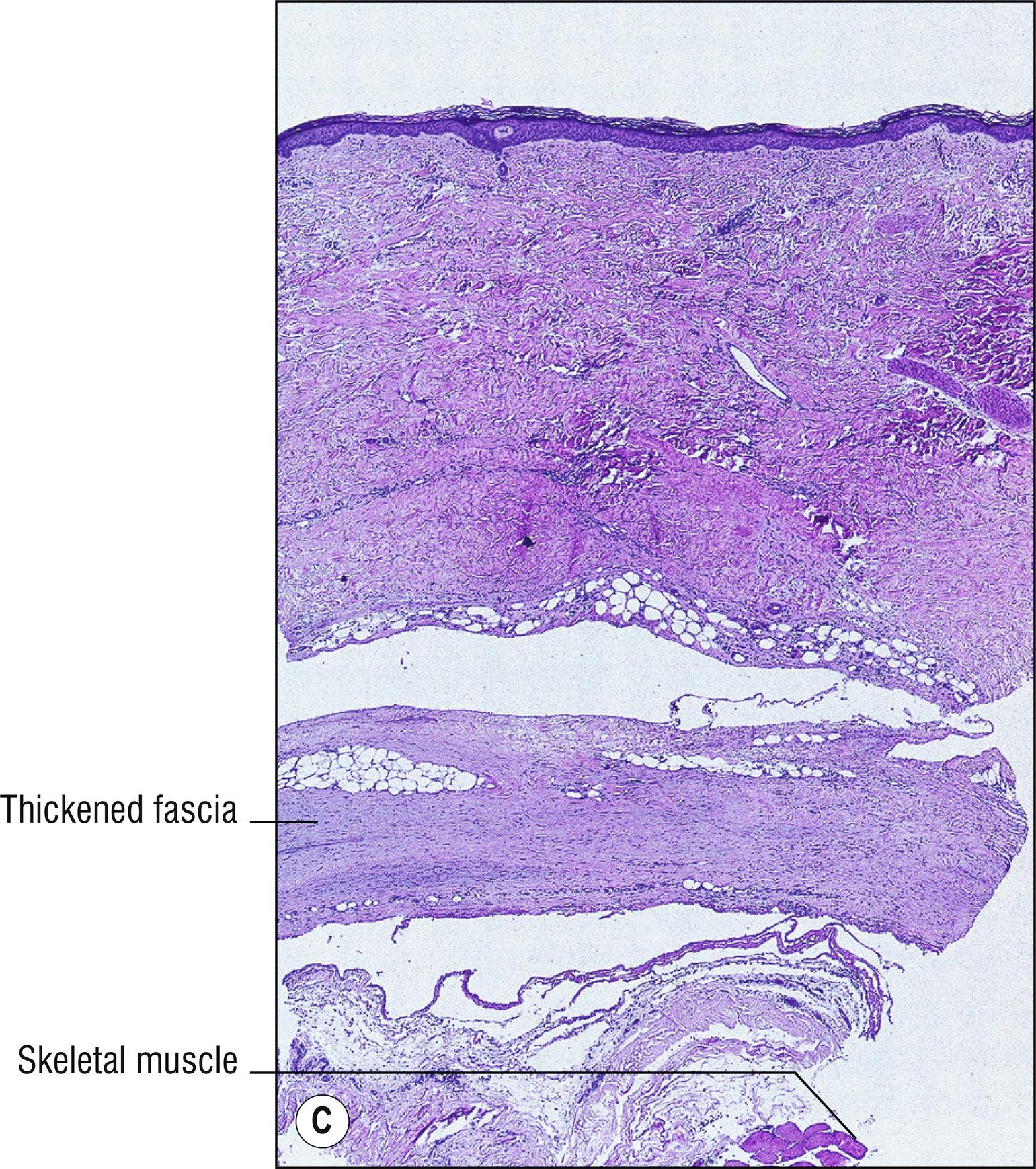
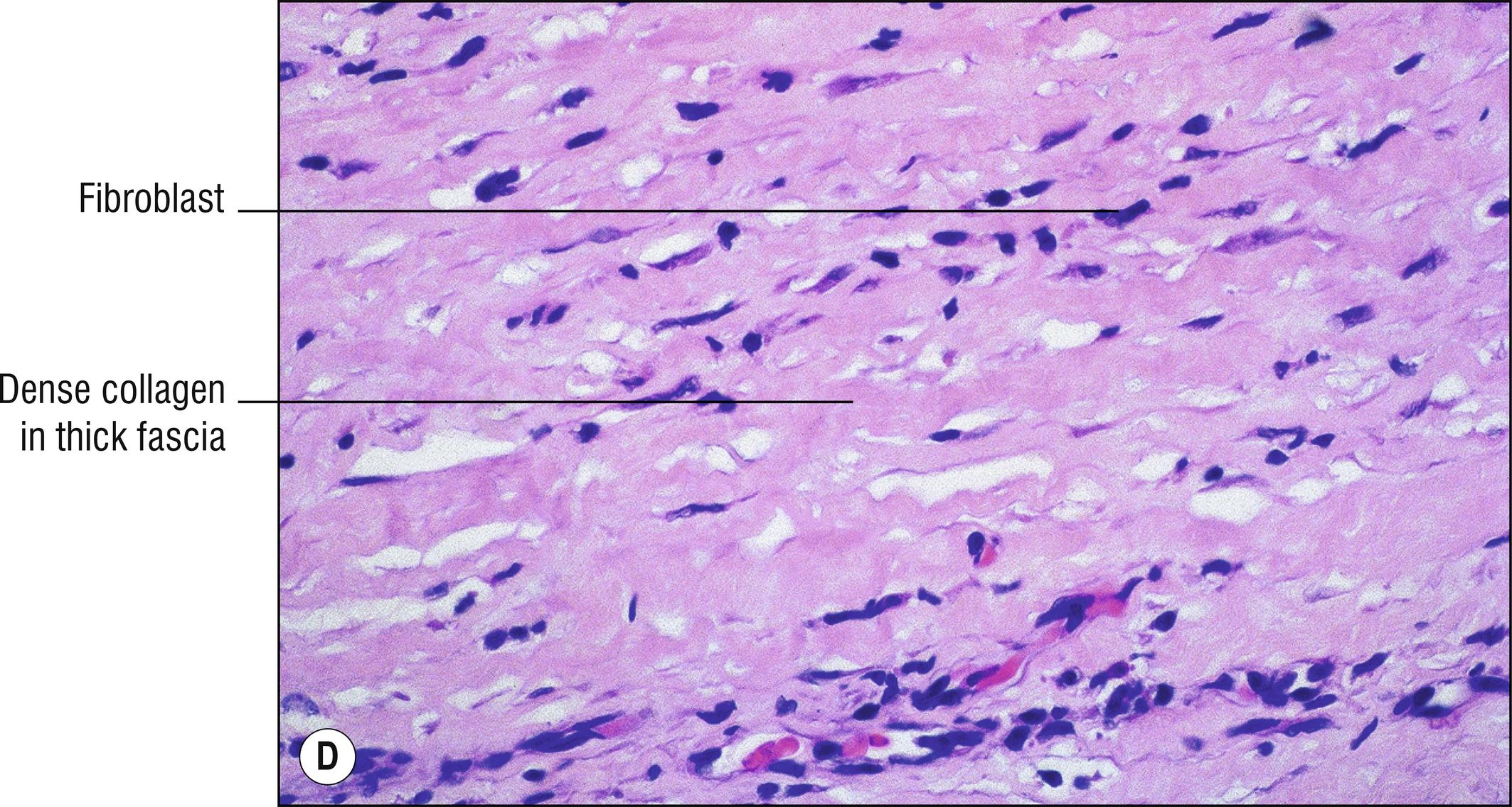
(see Fig. 9.3A–D )
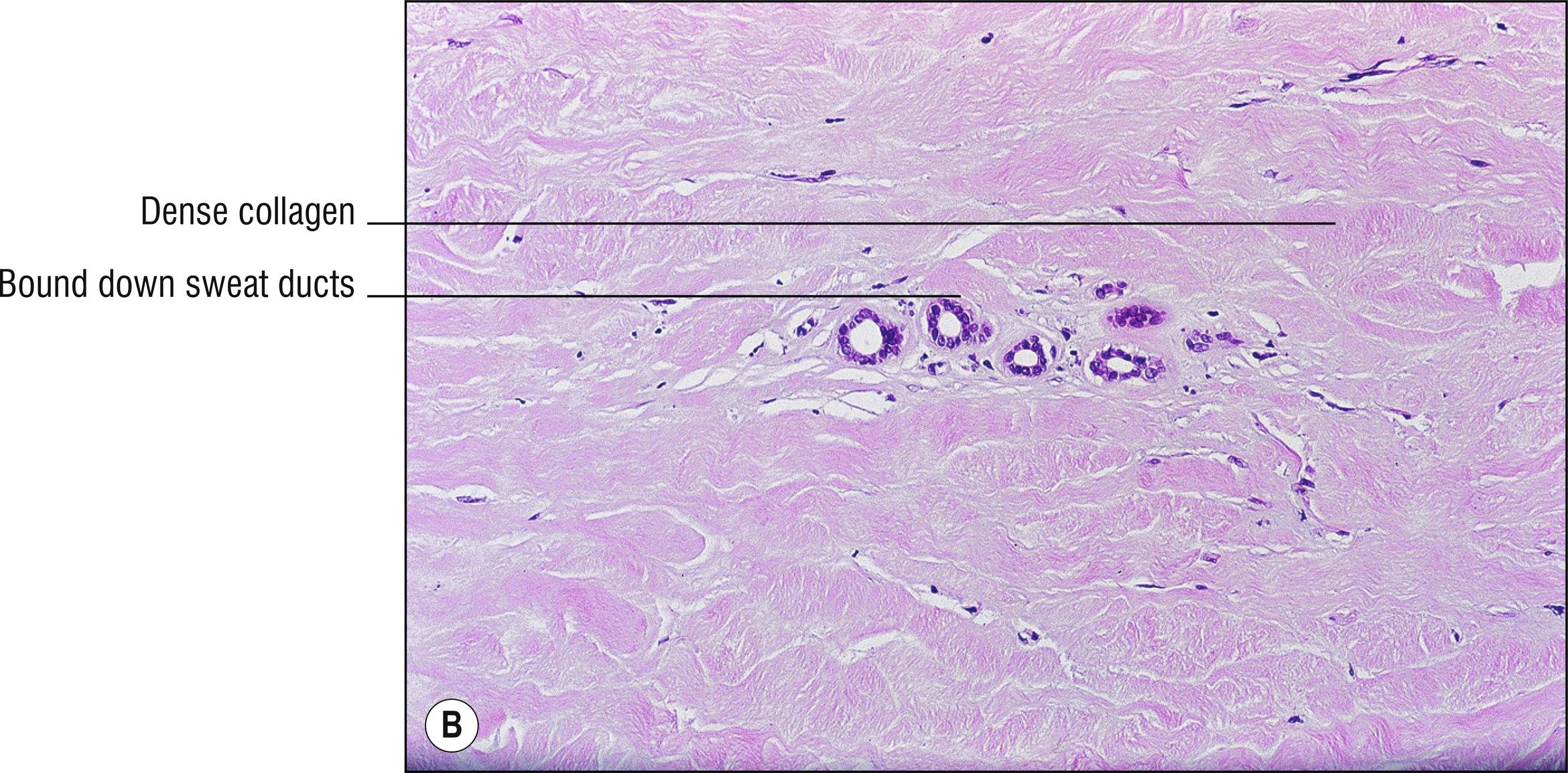
Somewhat common chronic systemic disease with indurated skin , especially of trunk, extremities, perioral face, and fingers (sclerodactyly; 1.56), often with hypopigmentation (1.150) or hyperpigmentation (1.18), often with “salt and pepper” appearance, associated with Raynaud’s phenomenon, hypertension, gastrointestinal disease (especially esophageal dysmotility; 1.49), pulmonary fibrosis, and kidney disease (1.66), sometimes with overlapping features with other rheumatologic diseases. A minority of patients have Scl-70 antibody . ANA with a speckled or characteristic antinucleolar pattern may be present.
Epidermis normal or atrophic (1.9)
Hyalinized dermis and subcutaneous fat, more prominent in late lesions
Sparse perivascular lymphocytes, sometimes plasma cells (1.111), in dermis or subcutaneous fat, more prominent in early lesions and in morphea than in systemic scleroderma
Decreased adnexal structures ; eccrine glands are entrapped by collagen and higher up in the dermis than usual because of increased collagen in subcutaneous fat
Morphea: localized sclerotic plaques of the skin, especially on the trunk (1.141), controversial relationship to tick bites and Borrelia (12.14), often with a violaceous halo (1.148) in active new inflammatory lesions, sometimes whitish, with overlapping histologic features of lichen sclerosus (9.5), no systemic disease . Perineural inflammation is found in 58% of cases of morphea, but is also found in 33% of controls.
Systemic scleroderma (progressive systemic sclerosis, PSS): described above.
Eosinophilic fasciitis (Shulmańs syndrome): acute onset after vigorous exercise , hyalinized, thickened fascia more than dermal sclerosis, more on the extremities , associated with peripheral eosinophilia (1.34) more than eosinophils in the fascia (therefore some prefer to call it fasciitis with eosinophilia), polyclonal gammopathy, occasional aplastic anemia, response to prednisone.
Linear scleroderma: linear form of morphea, without systemic disease, linear plaques (1.73) on the extremities , or on the forehead (1.44) or scalp appearing like a slash of a saber (en coup de sabre), sometimes with underlying bony disease (1.16).
CREST syndrome: calcinosis (1.19), Raynaud’s phenomenon, esophageal abnormalities, sclerodactyly and telangiectasias (1.136), with anticentromere antibody, better prognosis with regard to kidney disease than other forms of systemic scleroderma.
Stiff skin syndrome (congenital scleroderma): is a rare autosomal dominant condition with rock-hard induration of skin, related to mutations in the FBN1 gene and increased fibrillin-1 in the skin (unlike the deficiency of fibrillin-1 found in Marfańs syndrome). Onset in infancy especially involving buttocks, thighs, or shoulders, gradually spreading to entire body, with flexion contractures. Overlying skin may have hypertrichosis or hyperpigmentation. Biopsy demonstrates sclerotic collagen in the deep dermis or fascia, or loss of fat, without inflammation. Stiff person syndrome (Moersch-Woltmann syndrome) is different; it is really a neurologic condition with muscle rigidity.
Other sclerosing or fibrosing conditions (1.125), hyalinized conditions (1.35), especially scleredema (8.12), chronic graft-versus-host disease (17.3), chronic jack-hammer use, polyvinyl chloride exposure, sclerodermoid porphyria cutanea tarda (8.1), scleromyxedema (8.8), congenital stiff skin syndrome, nephrogenic fibrosing dermopathy (8.20), normal thick skin in areas such as the back, and lichen sclerosus (9.5).
Rare prominently depressed large atrophic “ cliff-drop ” plaque , usually on the lower back , often with prominent blood vessels seen within it.
Hyalinized dermis (1.35), often subtle, requiring fusiform excision of adjacent normal skin for comparison to appreciate the dermal atrophy in the involved skin (1.8)
Perivascular lymphocytes (1.109) in early lesions
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here