Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The agents of human African trypanosomiasis (HAT, sleeping sickness) are flagellated protozoan parasites that belong to the genus Trypanosoma, subgenus Trypanozoon . A general description of the members of this genus and specific characteristics of the subgenus are presented in the introduction to Chapter 276 . Three trypanosome subspecies, Trypanosoma brucei brucei, T. brucei rhodesiense, and T. brucei gambiense, are considered here. They are indistinguishable morphologically, and as a group they are often referred to as the T. brucei complex. T. b. brucei is a parasite of wild and domestic animals that is not infectious to humans. In contrast, T. b. rhodesiense, which is primarily a parasite of wild game, can infect humans, and this difference in host specificity forms the primary basis of the distinction between the two subspecies. T. b. gambiense primarily infects humans, and infections of wild and domestic animals are of limited importance.
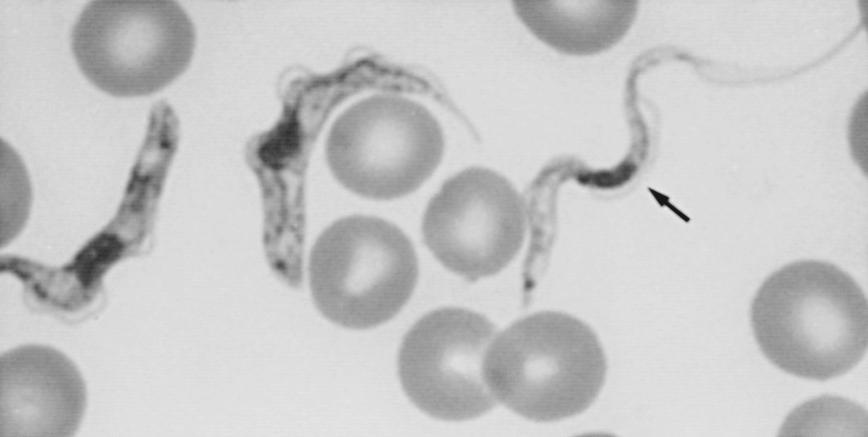
The members of the T. brucei complex are transmitted by various species of tsetse flies that belong to the genus Glossina. These bloodsucking insects are found only in Africa, where their range covers millions of square kilometers of rain forest and savanna. The parasites undergo a developmental cycle in the insect vectors. Tsetse flies of both sexes become infected with trypanosomes when they ingest blood from infected mammalian hosts that contains trypomastigotes, the form of the parasite that circulates in the bloodstream. There are two forms of circulating trypomastigotes: long, slender organisms that are capable of dividing and short, stumpy forms thought to be nondividing parasites that are infective for the insect vectors ( Fig. 277.1 ). Once in the midgut of the tsetse flies, stumpy trypomastigotes transform into relatively long, slender procyclic trypomastigotes. After many cycles of multiplication the procyclic forms migrate to the salivary glands, where they differentiate into epimastigotes and continue to multiply. A final transformation occurs as the epimastigotes become nondividing metacyclic trypomastigotes. Transmission takes place when these infective forms are inoculated during a subsequent blood meal. The cycle is completed when the injected metacyclic forms become bloodstream trypomastigotes and begin to multiply in the blood or other extracellular spaces. The capacity of African trypanosomes to multiply in the bloodstream of their mammalian hosts, where they are continually exposed to humoral defenses, constitutes a fundamental difference between the agents of sleeping sickness and Trypanosoma cruzi, the cause of Chagas disease in the Americas. The African trypanosomes are able to evade immune destruction indefinitely because they undergo antigenic variation, a process in which they periodically change the antigenic structure of the coat of glycoproteins that covers the surface of the parasite. The molecular mechanisms that control this complex process have been studied intensively. When epimastigotes transform into metacyclic trypomastigotes in the salivary glands of the tsetse fly, each parasite synthesizes a surface coat made up of one of about a dozen types of antigenic glycoproteins, called variant antigen types (VATs). Presumably, this occurs as a preadaptation to the relatively hostile environment of the mammalian host into which the metacyclics must be inoculated if they are to survive. After injection into a mammalian host, the parasites express metacyclic VATs for approximately 5 days, after which they switch to the expression of bloodstream VATs. Over time, the host sequentially mounts specific humoral responses directed against the predominantly expressed VATs. The population of parasites survives because an intrinsic rate of VAT switching provides an apparently endless supply of parasites that have surface glycoprotein coats to which the host has not been exposed previously.
Virtually all transmission of African trypanosomes to both wild and domestic animals, as well as to humans, takes place in the cyclic fashion just described. There is no evidence that these parasites can be transmitted by insects other than tsetse flies, and mechanical transmission by vectors is not important, although it may occur occasionally. Congenital transmission can occur, but in humans it is extremely rare, as is transmission by blood transfusion. A small number of laboratory accidents resulting in infection with African trypanosomes have been reported.
The pathogenesis of African sleeping sickness is complex, and many aspects of the process are poorly understood. The first sign of infection with African trypanosomes can be the acute inflammatory lesion (trypanosomal chancre) that appears a week or so after the bite of an infected tsetse fly and resolves spontaneously over several weeks. Interstitial multiplication of the trypanosomes takes place within the chancre, and there is an intense mononuclear cell reaction to the parasites, as well as edema and local tissue destruction.
After this initial local response the infection evolves over weeks and months into a systemic hemolymphatic illness as the parasites disseminate widely through the lymphatic system and the bloodstream. Systemic African trypanosomiasis without central nervous system (CNS) involvement is generally referred to as stage 1 disease. The parasites first travel from the site of inoculation to regional lymph nodes, where they proliferate and cause an inflammatory response. They then move through the lymphatics into the bloodstream, where multiplication continues. Egress of trypanosomes from vessels into interstitial spaces, where multiplication also takes place, is thought to be facilitated by increased vascular permeability.
In stage 1 trypanosomiasis there is widespread lymphadenopathy and histiocytic proliferation, which may be followed by fibrosis. Morular cells (Mott cells) are also often present in tissue. These cells are plasmacytes with vacuolated cytoplasm and pyknotic nuclei that are thought to play a role in the production of immunoglobulin M (IgM). The spleen may be enlarged, with generalized cellular proliferation, congestion, and focal necrosis. As the disease evolves, an endarteritis with perivascular infiltration of both parasites and lymphocytes may develop in lymph nodes and the spleen.
The heart is frequently involved in this stage of the disease, especially with T. b. rhodesiense infections. A pancarditis may develop involving all layers of the heart, including the mural and valvular endocardia. The conduction system may also be affected, and involvement of the autonomic innervation of the heart has also been reported. At the cellular level, pathologic changes include intense mononuclear infiltration consisting of lymphocytes, plasmacytes, and morular cells. As the infection progresses, myocytolysis and fibrosis may develop.
A number of hematologic manifestations accompany the development of stage 1 disease. Normocytic anemia is a regular feature in this phase of the illness and is usually accompanied by a brisk reticulocytosis. Several factors are thought to contribute to the anemia, and immune-mediated hemolysis may be important. Platelet counts are often reduced, especially in infections with T. b. rhodesiense, and disseminated intravascular coagulation before and during therapy has also been described. A moderate degree of leukocytosis is usually present, especially in the early months of the infection, and this is accompanied by polyclonal B-cell activation. High titers of immunoglobulins are a striking and constant feature of the illness. They consist primarily of polyclonal IgM that, for the most part, is not directed against specific parasite antigens. A number of other factors, including heterophile antibodies, rheumatoid factor, and anti-DNA antibodies, are often detectable. In addition, high levels of circulating antigen-antibody complexes are uniformly present, and these may play a role in the anemia, tissue damage, and increased vascular permeability that facilitate the dissemination of the parasites. Erythrocyte sedimentation rates are elevated, and hypocomplementemia has also been noted.
Stage 2 African trypanosomiasis involves invasion of the CNS. Parasites reach the brain and meninges via the bloodstream and cause meningoencephalitis or meningomyelitis, or both. In the brain they are found mainly in the frontal lobes, pons, and medulla, but other areas may be parasitized as well. Edema and hemorrhages may be evident on gross examination of affected areas at autopsy. Trypanosomes are present in perivascular areas, and nests of organisms can be found without apparent relation to blood vessels. The presence of parasites in the CNS is associated with infiltration of mononuclear cells that are predominantly lymphocytes, plasmacytes, and morular cells. The presence of parasites in the CNS is heralded by abnormal findings in the cerebrospinal fluid (CSF). The CSF may be under increased pressure, and the total protein concentration is elevated, with mononuclear cells predominating in addition to small numbers of morular cells and eosinophils. Trypanosomes are frequently present in the CSF as well. A model of T. brucei infection in rats has been developed that differs from a standard view of disease and highlights the prominent role of penetration and residence of parasites in the pia mater, an immune-privileged site. According to this model, the production of prostaglandin D 2 may influence the development of sleeping sickness, and brain parenchymal disease proceeds from this chronic infection. The authors suggest that a better understanding of the physiology of disease might influence assumptions about the pharmacokinetic characteristics of drugs in development.
HAT, which is limited to sub-Saharan Africa, was a much greater problem in the past than it is at present. Hundreds of thousands of people died in major epidemics around the beginning of the 20th century and between 1920 and 1948. Between World War II and independence, the colonial powers invested heavily in controlling HAT and succeeded to the point where the disease was almost eliminated. In the decades after independence, however, in the context of continuing poverty and civil strife in many areas, control programs were neglected and HAT underwent a resurgence that reached a peak in the late 1990s. Angola, Uganda, South Sudan, and the Democratic Republic of Congo were particularly affected, and even today 80% of reported cases occur in the latter. Since then, efforts of the World Health Organization (WHO), governments of the endemic countries, and nongovernmental organizations have resulted in effective control in many affected areas, so much so that the annual number of reported cases decreased to 9878 in 2009 and to 2184 by 2016, which is roughly equivalent to the low point reached in the early 1960s. Although underreporting is a persistent problem, there is no doubt, to the credit of the many organizations involved in these efforts, that the level of control reached to date is impressive. In 2012 a panel of experts convened by WHO to review the then-current situation and developed a vision for the elimination of HAT. The current view at WHO is that efforts are on track for achieving, by 2020, the elimination of HAT as a public health problem, which is defined as fewer than 1000 reported cases per year.
West African (gambiense) trypanosomiasis and East African (rhodesiense) trypanosomiasis are epidemiologically distinct diseases. The general geographic distributions of these two illnesses are presented in Fig. 276.1 in Chapter 276 , and the remaining foci where transmission is known to occur are found in the indicated areas. Distinguishing epidemiologic and clinical features of the two diseases are presented in Table 277.1 .
| WEST AFRICAN (GAMBIENSE) | EAST AFRICAN (RHODESIENSE) | |
|---|---|---|
| Organism | Trypanosoma brucei gambiense | Trypanosoma brucei rhodesiense |
| Vectors | Tsetse flies ( palpalis group) | Tsetse flies ( morsitans group) |
| Primary reservoir | Humans | Antelope and cattle |
| Human illness | Chronic (late CNS disease) | Acute (early CNS disease) |
| Duration of illness | Months to years | <9 mo |
| Lymphadenopathy | Prominent | Minimal |
| Parasitemia | Low | High |
| Epidemiology | Rural populations | Tourists in game parks; workers in wild areas; rural populations |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here