Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Fetal malformations can be caused by chromosomal defects detectable by fetal karyotype and chromosomal microarray analysis, by sequence variants (mutations) in single genes or can be multifactorial in origin.
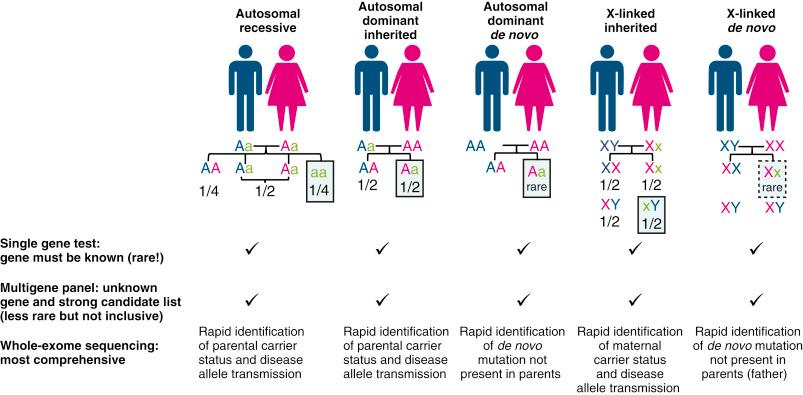
Single-gene disorders can be inherited from parents (autosomal recessive, autosomal dominant or X-linked) with substantial recurrence risk or can be caused by de novo mutations in the fetus with an extremely low recurrence risk.
When a genetic disorder in the family is known, specific single gene testing can be performed using standard sequencing. However, in all other circumstances, single gene testing is limited prenatally because genetic heterogeneity and incomplete description of the prenatal phenotype of many single-gene disorders preclude optimal selection of the putative disease gene to sequence.
Next-generation sequencing, a new method that can assay multiple genes at once, up to the entire genome, has driven development of new genetic tests, such as disease-specific multigene panels, whole-exome sequencing (WES) and whole-genome sequencing.
Multigene panels allow for testing of multiple genes in parallel, which can be useful in prenatal diagnosis if there is a distinct phenotype, such as skeletal dysplasia or specific brain abnormalities.
WES is more comprehensive than multigene panels because it analyses the coding regions of most genes in a single test.
WES has improved genetic diagnosis by 16% to 45% in paediatric and adult populations.
Initial reports indicate that WES also improves detection of a genetic aetiology for prenatally diagnosed fetal structural abnormalities.
Prenatal WES is usually performed as trio sequencing of fetal, maternal and paternal DNA to facilitate more rapid results.
Although prenatal WES is promising, more research is needed to address challenges related to cost and access, clinical utility, indication for the test, interpretation of pathogenicity of variants and issues surrounding reporting of variants of uncertain significance and incidental or secondary findings.
Three percent of all pregnancies are complicated by fetal congenital anomalies identified by prenatal imaging. Standard genetic tests, including karyotype and chromosomal microarray analysis (CMA) performed on fetal samples, typically amniotic fluid (AF) or chorionic villus sampling (CVS), can identify the cause in about 30% of affected pregnancies, but for the remaining 70%, the genetic cause remains unknown, and it is predicted that a significant fraction of these could be explained by single-gene disorders. Until recently, testing for single-gene disorders in the prenatal setting has been difficult and limited to cases with prior knowledge of an increased risk for a specific genetic disorder, for example, if there is a strong family history for an inherited autosomal dominant, autosomal recessive, X-linked condition ( Fig. 25.1 ). This scenario is relatively rare, and in many cases, the affected fetus represents the first de novo presentation of the phenotype in a particular family. In these fetuses, it is difficult to select which gene to test for because the ultrasound findings can be nonspecific or unexpected from known postnatal presentations. In some cases, there is genetic heterogeneity, a scenario in which mutations in several different genes can cause the same phenotype. For others (e.g. lethal fetal anomalies), the causative genes may not yet be known. Finally, some conditions are multifactorial with both genetic and environmental causes. Table 25.1 shows the different possible genetic and nongenetic causes for fetal structural birth defects, their relative frequencies and appropriate testing strategies. It is therefore difficult to choose which gene to test after a normal karyotype or CMA result, supporting the need for multiplex assays that analyse several genes at once, but development of such assays was slowed by the limitations of the older technology of Sanger sequencing. With the development of modern next-generation sequencing (NGS), this has now become reality. In this chapter, we focus first on the use of NGS to find point mutations in multiple genes at once through multigene panel sequencing and next on its application for whole-exome sequencing (WES), a method in which the entire ‘coding’ genome can be searched. The technology of NGS is also the basis for other new tests highlighted elsewhere in this textbook, such as noninvasive cell free DNA screening for cytogenetic conditions (see Chapter 21 ), noninvasive screening and testing for single-gene disorders (see Chapter 22 ) and panethnic expanded carrier screening (see Chapter 26 ).
| Condition | Prevalence (%) | Appropriate Diagnostic Test |
|---|---|---|
| Common trisomies (21, 13, 18) | 0.2 | Karyotype or CMA |
| Chromosomal abnormality other than trisomy | 0.2 | Karyotype or CMA, but CMA does not detect balanced rearrangements |
| Pathogenic copy number variants (deletion or duplication) | 1.2 | CMA |
| Known Mendelian genetic disorders | 0.4 | Specific gene testing when gene is known; if not known, multigene panels or WES (investigational) |
Structural or functional congenital abnormalities
|
3 | Karyotype or CMA to exclude chromosomal abnormalities and pathogenic CNVs followed by WES if normal (investigational) |
| Multifactorial conditions | 0.2–0.1 | Ultrasonography is the primary tool; genetic testing only useful to exclude other causes; some screening possible (e.g. neural tube defects) |
| Teratogen exposure (e.g. warfarin, retinoid) | Rare | History and ultrasound are primary tools; genetic testing may be useful to exclude other causes |
| Disruption (e.g. amniotic band) | Rare | Ultrasonography is the primary tool; genetic testing may be useful to exclude other causes. |
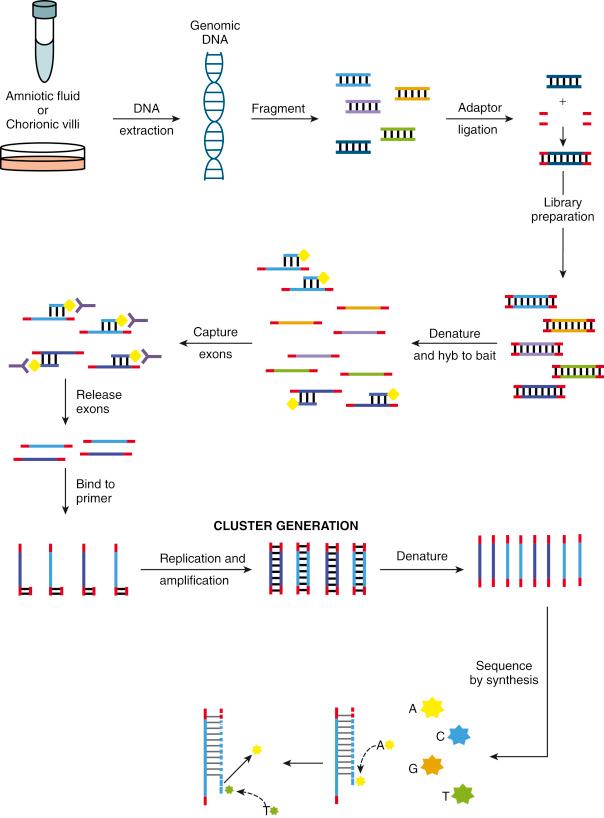
Next-generation sequencing is a relatively new technology based on massively parallel sequencing (MPS). In MPS ( Fig. 25.2 ), the DNA of the sample that is being sequenced (e.g. DNA extracted from AF or a CVS) is first sheared into small fragments and linked to adapters to generate the ‘sequencing library’. Either the entire library of fragments or only a selected subset of fragments of interest is used as templates for the synthesis of millions of short and overlapping DNA fragments. Each nucleotide incorporated into these fragments is labelled with a different coloured fluorescent probe so that the sequence or ‘genetic code’ of each fragment is identifiable. Data from all the obtained sequences are then aligned and compared with the human genome reference sequence. Because NGS is more error prone than traditional Sanger sequencing, each fragment is sequenced multiple times, with the ultimate goal of assuring that all regions of the sequenced DNA are covered by multiple overlapping fragments. This coverage is referred to as the sequencing depth. The standards for coverage when NGS is used for clinical diagnosis are set by the Laboratory Quality Assurance Committee of the American College of Medical Genetics and Genomics (ACMG). For diagnostic WES, a mean coverage of 100-fold for proband-only WES and 70-fold coverage for trio-based tests is recommended, each with 90% to 95% of the sequenced nucleotides covered at least 10-fold. Recent technical advances in NGS allow clinical laboratories to offer shorter turnaround times (TATs) together with better sequencing depth.
Although NGS is a powerful new method, some limitations inherent to the technology affect clinical diagnosis ( Table 25.2 ). Some genes can be incompletely covered because of sequencing depth variation, and it is more difficult to get accurate results from regions with ‘high GC content’ (regions with more guanine and cytosine than adenine and thymidine). Genes that belong to families of highly homologous genes or have a pseudogene are also difficult to sequence. Certain mutation types, including triplet repeat mutations (e.g. the CGG trinucleotide repeat in fragile X syndrome), deletions and duplication that are longer than a few nucleotides, low-level mosaic mutations, balanced and unbalanced translocations or inversions, are more difficult to detect by NGS. Newer approaches to overcome some of these difficulties are under development.
| Well-Detected Mutations | Poorly or Not Detected Mutations |
|---|---|
| In unique genes, exons | In pseudogenes, repeated exons, highly homologous genes and GC-rich sequences |
| Point mutations | Large rearrangements, aneuploidy |
| Small indels | Low-level mosaic mutations |
| Germline mutations | Repeat expansions |
| Only in covered regions (WES) | In uncovered regions (WES) |
| Only in regions that can be sequenced with NGS | In regions with low coverage or sequencing depth |
| In regions with sufficient coverage and depth | Epigenetic mutations |
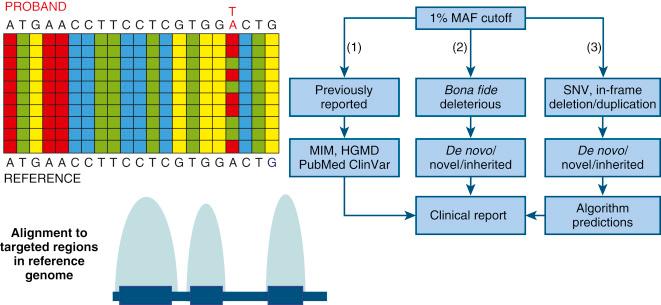
The interpretation of the sequencing data is the most challenging part of diagnostic genome-wide sequencing ( Fig. 25.3 ). Because of individual variation in DNA sequences, thousands of sequence variants are identified with WES and sequence variants obtained from whole-genome sequencing (WGS) amount to millions, most of which are benign polymorphisms that are not disease causing. To sort out and prioritise those that are clinically important, powerful bioinformatics algorithms are used. Identified sequence variants that differ from the reference sequence are compared with information in databases and interpreted for their known or predicted functional impact. They are also classified using tools that predict the effect of the mutation on the function of the protein coded by the gene. Information about whether sequence variants are in known disease genes is also integrated. To ensure consistency in interpretation among diagnostic laboratories, the ACMG has provided standard guidelines for variant classification. Variants are classified as pathogenic, likely pathogenic, of unknown significance, likely benign, or benign and further qualified as in genes related to the clinical presentation or unrelated to the clinical presentation ( Table 25.3 ). Pathogenic or likely pathogenic sequence variants unrelated to the proband’s clinical presentation (phenotype) are referred to as ‘incidental findings’. In some cases, they have well-known clinical consequences, and for a subset, called actionable findings, there is treatment or prevention that can improve outcome. The ACMG has published and updated a guideline for clinical laboratories that suggests that they actively seek and report known pathogenic and expected pathogenic variants in 59 ‘actionable’ genes (e.g. cancer or cardiac disease predisposition genes). These most recent recommendations state that patients should be counselled about this during pretest counselling and can be given the option to opt out of receiving this information. It should be noted that this guideline does not include the application of WES for prenatal diagnosis.
| Classification | Related to Indication for Sequencing | Unrelated to Indication for Sequencing (Incidental Finding) |
|---|---|---|
| Definite pathogenic | Always reported if in known disease gene (prior evidence) Sometimes reported if in plausible gene (no or limited prior evidence) |
Typically reported if secondary finding in 59 ACMG-actionable genes if postnatal Varies for other actionable genes and varies prenatally |
| Likely pathogenic | Typically reported if in known disease gene (prior evidence). Sometimes reported if in plausible gene (no or limited prior evidence) |
Typically reported if secondary finding in 59 ACMG-actionable genes if postnatally Varies for other actionable genes and varies prenatally |
| Variant of uncertain significance | Reporting varies | Typically not reported |
| Likely benign | Typically not reported | Typically not reported |
| Benign | Not reported | Not reported |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here