Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Depression, anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder are treatable with medications or psychotherapy.
A history of manic or hypomanic symptoms increases the risk for a “switch” into mania with antidepressant treatment.
Close follow-up, in 1 to 2 weeks, is recommended to monitor for increases in suicidal thoughts with antidepressants, especially in adolescents and young adults.
Active suicidal thoughts and plans are a psychiatric emergency.
Eating disorders are life-threatening conditions that are often unrecognized.
Girls or women presenting with amenorrhea, menstrual dysfunction, low bone density, sexual dysfunction, infertility, anxiety, depression, or hyperemesis gravidarum should be screened for eating disorders.
Women with anxiety disorders (especially panic disorder and posttraumatic stress disorder) are at increased risk for suicide and should be asked about suicidal thoughts or plans.
Anxiety disorders respond well to reassurance, education, and treatment with psychotherapy and medications (especially SSRI antidepressants).
Many substance use disorders, such as alcoholism, have a more rapidly progressive course in women than in men (“telescoping”).
More than seven drinks per week is considered heavy drinking for a woman.
Motivational interviewing is a highly effective, brief intervention that increases engagement in substance abuse treatment and other behavior change.
In cases of misuse of potentially habit-forming medications, a formal treatment agreement may be necessary.
Understanding attachment styles can help providers to work effectively with “difficult” patients.
Nonpharmacologic treatments for hypoactive sexual desire disorder include lifestyle changes for reducing stress and fatigue, recognizing and treating depression, increasing quality time with the partner, improving body image, and bringing novelty into the sexual repertoire.
Environmental, staff, medical record, and physician-related measures can aid in engaging lesbian, bisexual, and transgender individuals in care and in ensuring high-quality health care.
Lesbian, bisexual, and transgender individuals have an elevated rate of mental health problems, substance use disorders, and suicide attempts, especially during adolescence.
Intimate partner violence crosses all ethnic, racial, educational, age, and socioeconomic lines and has a large burden of social, physical, mental, and public health implications.
The physician has a responsibility to screen and acknowledge intimate partner violence and abuse, identify community resources for immediate referrals, assess safety, assist with reporting if necessary or desired, document appropriately using medicolegal tools, and provide ongoing clinical care.
Gynecologists are often called on to provide or refer women for counseling related to grief; losses such as miscarriage, perinatal loss, and infertility; and end-of-life issues.
Women suffering losses as a result of miscarriage, perinatal loss, unplanned pregnancy, or infertility benefit from support, counseling, and screening for depression and posttraumatic stress disorder.
Complicated grief and grief accompanied by symptoms of depression benefit from antidepressant medication treatment in addition to psychotherapy.
Women with terminal illness benefit from an engaged, genuine relationship with physicians and other health care providers, treatment of depression and anxiety states, psychological interventions and psychotherapy, and early integration of palliative care into treatment.
Gynecologists follow women across the life cycle, from puberty through old age. The gynecologist may be a woman’s primary health care provider for much of this time. The gynecologist is thus in an important position to help a woman navigate normal developmental stages and challenges, to share in critical life events and to provide or obtain counseling for a woman as she works her way through emotional adjustments and problems.
Normal development includes challenges such as building an identity and self-esteem; dealing with sexuality and sexual development; forming meaningful relationships; pregnancy and motherhood; life roles and transitions; and losses, grief, and aging. In addition to these normal developmental transitions and challenges, a woman may have to deal with trauma related to difficult early childhood experiences, abuse, rape, or intimate partner violence. Psychiatric disorders such as depression, anxiety, posttraumatic stress disorder, and eating disorders are common in women, and conditions such as alcohol and drug use disorders often have a different presentation and course in women compared with men.
This chapter reviews common psychiatric disorders occurring in gynecologic patients, sexual function and disorders, and behavioral and psychosocial issues and traumas that may arise during a woman’s lifetime, and it offers suggestions as to how the physician can aid the patient.
Major depression is common in women, with a lifetime prevalence of 20% to 25%. Although boys and girls are equally likely to experience depression, major depression is about twice as common in women as in men, starting in adolescence. Worldwide, depression is one of the leading causes of functional impairment and disability. The diagnosis of major depression refers to persistent sadness or lack of interest or pleasure in usual activities, lasting for at least 2 weeks. It is accompanied by symptoms such as changes in eating habits, trouble sleeping, lack of energy and motivation, poor memory or concentration, and feelings of guilt, worthlessness, hopelessness, and despair. In severe cases, depression may lead to suicidal thoughts and actions. The diagnostic criteria for major depression are listed in Box 9.1 . The Patient Health Questionnaire (PHQ-9) ( Table 9.1 ) is a useful screening tool for major depression, can be filled out quickly by the woman in the waiting room or in the office before a visit, and helps in identifying depression, monitoring effects of treatment, and educating the woman about her own characteristic symptoms of depression. Scores of 5, 10, 15, and 20 are cutoff scores indicating mild, moderate, moderately severe, and severe depression, respectively.
Five or more of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad or empty) or observation made by others (e.g., appears tearful)
Markedly diminished interest or pleasure in all, or almost all, activities
Significant weight loss (when not dieting) or weight gain, or decrease or increase in appetite
Insomnia or hypersomnia
Psychomotor agitation or retardation observable by others
Fatigue or loss of energy
Feelings of worthlessness or excessive or inappropriate guilt
Diminished ability to think or concentrate, or indecisiveness
Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation, or a suicide attempt or specific suicide plan
Symptoms cause clinically significant distress or impairment.
| Over the past 2 weeks, how often have you been bothered by any of the following problems? | ||||
| Not at All | Several Days | More than Half the Days | Nearly Every Day | |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
|
0 | 1 | 2 | 3 |
| Total Score | ___ | + ___ | + ___ | + ___ |
| If you checked off any problems, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people? | ||||
| ___ Not difficult at all ___ Somewhat difficult ___ Very difficult ___ Extremely difficult | ||||
The cause of major depression is unclear. It may occur without a clear stress or precipitant, especially in women with a strong family history of depression who are genetically predisposed. A family history of depression, a prior depressive episode, and older age are all risk factors for depression. Rates of depression are higher in women who are socioeconomically disadvantaged. In addition, stressors such as loss of relationships and loved ones, divorce, role transitions, interpersonal conflicts, interpersonal violence, medical illness, or feelings of being trapped in a stressful situation without a way to escape or cope can precipitate depression. Depressive symptoms in a particular person may be uniquely determined by individual factors, such as family relationships while growing up and past experiences that are highly meaningful and evoke negative feelings and memories triggered by current situations or events.
The increased rate of depression in women starting at menarche has also been thought to result from hormonal factors. There are clear increases in risk for depressive symptoms premenstrually, with some women only experiencing mood symptoms at this time and others noting a worsening of underlying depression in the week or two before menses (for a discussion of premenstrual dysphoric disorder, see Chapter 35 ). The postpartum period is a high-risk time for depression and is the highest risk time in a woman’s life for psychiatric hospitalization. There is also an increase in depressive symptoms at the time of menopause and the menopausal transition.
The differential diagnosis of major depression includes adjustment disorder, persistent depressive disorder (dysthymia), depression related to drugs and alcohol or secondary to a medical condition, and bipolar disorder. Adjustment disorder is a stress-related, short-term emotional or behavioral response to a stressful life circumstance. Depressive symptoms begin within 3 months of the onset of the stressor and resolve within 6 months once the stressful circumstance ends. The symptoms do not meet criteria for major depression. The physician can help a woman with an adjustment disorder by helping her to problem solve and cope with the situation she is in or by referring her for short-term therapy or counseling.
Persistent depressive disorder (previously called dysthymic disorder ) is a chronic, low-grade depression, with symptoms present more than half the time for at least 2 years and no more than 2 months without depressive symptoms during that time. The best treatment is antidepressant medication and psychotherapy, but this condition is often harder to treat than major depression because of its chronicity. Depressive symptoms can also be caused by alcohol or drug use or by medical conditions, such as hypothyroidism, vitamin B 12 deficiency, anemia, or cancer (most classically pancreatic cancer). Women presenting with depression should be screened for medical disorders and asked about use of alcohol and drugs.
Probably the greatest dilemma in deciding to prescribe antidepressants is the concern that if the woman has bipolar disorder, antidepressants can cause a “switch” into a manic episode. Manic episodes are characterized by feelings of euphoria or irritability and increased energy or goal-directed activity, with symptoms such as decreased need for sleep, increased activity or agitation, talkativeness, racing thoughts, grandiose and unrealistic plans, and impulsive and risky behavior. If a woman has been hospitalized for mania or has had such symptoms for a week or more in the past, the diagnosis may be clear. However, people often do not recall their manic symptoms or have little insight into them, or they may have had briefer periods of a few days (hypomania) that still predispose them to mania with antidepressants. Screening questionnaires such as the Mood Disorder Questionnaire (MDQ) or clinician-administered Composite International Diagnostic Interview (CIDI) (STABLE Resource Toolkit; , pp. 14-20) can be helpful in assessing the likelihood of a bipolar disorder. Difficulty determining whether or not a woman has bipolar disorder is an indication for psychiatric consultation because bipolar depression usually requires treatment with a mood stabilizer or atypical antipsychotic medication instead of, or combined with, an antidepressant.
Treatment of major depression can include antidepressant medication, psychotherapy, or both. Because both antidepressant medication and psychotherapy are effective, the initial choice of treatment can be made according to the woman’s preference, although for more severe depression medication is indicated. Commonly prescribed antidepressant medications and dosages are listed in Table 9.2 . A 2009 meta-analysis by Cipriani and colleagues suggested that the best combination of efficacy and tolerability is found with sertraline or escitalopram ( ). Because of their more benign side effect profiles, it is reasonable to start a selective serotonin reuptake inhibitor (SSRI) as the first antidepressant in most cases. SSRI side effects include gastrointestinal symptoms (nausea, diarrhea, vomiting), which are minimized by taking the medication with a meal. Other common side effects include initial dizziness and headaches and sexual dysfunction, most commonly delayed orgasm or anorgasmia. Doses of the SSRI citalopram exceeding 40 mg daily are not recommended because of the risk of QT prolongation. SSRIs may also cause uncomfortable withdrawal symptoms if discontinued suddenly. Withdrawal symptoms can include gastrointestinal symptoms, headache, dizziness, and “electric shock” sensations. Fluoxetine, an SSRI with a long half-life, is not generally associated with withdrawal symptoms and women discontinuing other SSRIs can be switched to fluoxetine to minimize withdrawal. Fluoxetine also has the strongest evidence base for medication treatment of major depression in children and adolescents.
| Antidepressant | Dose Range (mg/day) | Comments |
|---|---|---|
| S erotonin R euptake I nhibitors (SSRI s ) | ||
| Citalopram | 20-40 | FDA warning of QT prolongation at doses >40 mg/day |
| Escitalopram | 10-20 | S-enantiomer of citalopram |
| Fluoxetine | 20-80 | Long half-life; unlikely to cause withdrawal symptoms with discontinuation or missed doses; best evidence base for use in children and adolescents |
| Paroxetine | 20-50 (25-62.5 controlled release) | High rate of withdrawal symptoms |
| Sertraline | 50-200 | |
| S erotonin and N orepinephrine R euptake I nhibitors (SNRI s ) | ||
| Duloxetine | 60-120 | May also be effective for neuropathic pain, urinary incontinence |
| Venlafaxine | 75-225 | Risk of elevated blood pressure |
| O ther | ||
| Bupropion | 300-450 | Elevated risk of seizures, especially at doses >450 mg/day; contraindicated in patients with bulimia; may be effective for comorbid attention deficit disorder; activating; does not cause sexual dysfunction or weight gain; effective for smoking cessation |
| Mirtazapine | 15-45 | Sedating; causes weight gain |
| Trazodone | 25-100 (for insomnia) | Sedating; used as adjunctive treatment for insomnia |
Serotonin and norepinephrine reuptake inhibitors (SNRIs) include venlafaxine and duloxetine. Venlafaxine is associated with a dose-related risk for gradual onset of hypertension, and blood pressure should be monitored carefully on this medication. SNRI side effects include gastrointestinal side effects, headaches, dizziness, anorgasmia, activation, and anxiety. Bupropion appears to exert its therapeutic effect by enhancing effects of dopamine and norepinephrine. It increases energy and can cause insomnia, increased anxiety, headaches, and gastrointestinal side effects. Bupropion also lowers the seizure threshold, especially at doses greater than 450 mg daily, and should not be used in women with a history of a seizure disorder or bulimia. Mirtazapine is an alpha 2 -adrenergic, 5-HT2, and 5-HT3 receptor antagonist, which also has antihistaminic effects. Its common side effects include sedation and weight gain. Trazodone is a highly sedating serotonergic antidepressant that is used primarily at low doses (25 to 100 mg at bedtime) for insomnia. Tricyclic and monoamine oxidase (MAO) inhibitor antidepressants are infrequently prescribed because of side effects, in addition to dietary restrictions and the risk of hypertensive crisis with MAO inhibitors. It is important to warn women that antidepressant medication can take up to 4 to 6 weeks to work and to schedule a follow-up visit within that time to monitor treatment adherence, side effects, and therapeutic response. The Food and Drug Administration (FDA) has required black box warnings regarding increases in suicidal ideation and behavior with antidepressants in children, adolescents, and young adults . The mechanism for this is unclear but may be in part an increase in energy and motivation before improvement in mood. Women should be warned of this potential phenomenon and instructed to stop the medication and call the provider if this occurs. Overall, antidepressants reduce depression and risk for suicide, but this potentially serious side effect is another indication for close follow-up early in treatment. In particular, patients younger than 25 years should be seen 1 to 2 weeks after beginning antidepressant medication.
Effective psychotherapies for depression include cognitive behavioral therapy (CBT) and interpersonal therapy (IPT). CBT addresses the negative thinking that is characteristic of depression, such as the belief that things are bad now, have always been bad, and will always be bad, or thoughts of worthlessness and guilt. In addition, behavioral activation, or scheduling activities that provide a sense of accomplishment, mastery, or pleasure, is helpful in depression, and exercise has been shown to decrease depressive symptoms. IPT addresses life changes and interpersonal challenges that contribute to depression. These include grief, conflicts in interpersonal relationships including marital or intimate partner conflicts, and transitions in roles within work or the family. These therapies are usually weekly for an hour for 3 to 4 months. In cases of clear-cut couples issues, couples therapy may be indicated, especially after the woman has recovered from depression sufficiently to participate in such therapy. Other nonmedication treatments for depression include morning light for seasonal or winter depression and electroconvulsive treatment (ECT) or repetitive transcranial magnetic stimulation (rTMS) for depression that does not respond to medication and psychotherapy.
Both medication and psychotherapy are significantly more effective than placebo for treatment of major depression, with response rates varying between about 50% and 70%, depending on the patient population. Combined treatment with both psychotherapy and medication is more effective and is indicated for more severe depression.
The goal of treatment for depression is complete remission, or resolution of all depressive symptoms, because even mild residual symptoms increase the risk of relapse. Several measures can increase rates of remission ( ). First, close follow-up, with visits every 1 to 2 weeks at first and then every 2 to 4 weeks, will enhance adherence and response rates. One third of people prescribed an antidepressant discontinue the medication within 30 days. There is considerable stigma associated with taking psychotropic medication or having a psychiatric diagnosis, so addressing the woman’s concerns that depression is a weakness or a character flaw can be helpful. Frequent visits also allow early identification of side effects that decrease adherence. Patient education about the lag in response to antidepressants and the need to take the medication every day for at least 6 to 12 months after symptomatic improvement is important. Tracking symptoms with a scale such as the PHQ-9 is helpful in monitoring progress and identifying residual symptoms. If there is little response in 2 to 4 weeks, a dose increase should be considered. A partial response at 8 weeks should prompt reassessment of the diagnosis; an attempt to ensure that the patient is taking the maximal tolerated dose of the antidepressant; and consideration of switching medications, adding an augmentation agent such as lithium, an atypical antipsychotic, or triiodothyronine (T3), or referral to a psychiatrist. Women who have had three or more episodes of major depression should be continued on maintenance antidepressant treatment.
Suicide is a feared and tragic outcome of depression and other mental health conditions. In the United States there were 47,173 suicide deaths in 2017; 6.1 per 100,000 women and 22.4 per 100,000 men died by suicide, and suicide was the 10th leading cause of death. Rates of suicide are highest among people aged 45 to 64 years compared with other age groups and in whites, and Native Americans compared with other ethnic groups. There are about 30 suicide attempts per every suicide death. Risk factors for suicide include depression or other mental health disorders; substance use disorders; a prior suicide attempt; a family history of psychiatric or substance use disorders; family violence, including physical or sexual abuse; access to means such as firearms in the house; and exposure to suicidal behavior by people such as family members, peers, or celebrities. All depressed women should be asked about suicidal thoughts. This should include asking about whether the woman feels hopeless or has had thoughts that life is not worth living or thoughts of ending her life, followed by more specific questions about whether she has made suicide plans and how far she has gone to carry these out. The Columbia Suicide Severity Rating Scale ( ; scale available at http://cssrs.columbia.edu/wp-content/uploads/C-SSRS-Screener-with-Triage-Points-for-Primary-Care-2018-1.docx ) provides a useful structured approach to asking about suicidal thoughts, with a screening form and triage recommendations tailored for primary care settings. Active suicidal thoughts and plans are a psychiatric emergency. The woman should not be left alone. The physician or staff should call 9-1-1 to have her taken to the nearest emergency room. Even in less acute cases, it is important to develop a safety plan with the patient, identifying family members, supportive people, and resources (e.g., crisis lines) she can call on, making a plan to remove firearms and other means of suicide from the home (means restriction), having someone else supervise the woman’s medication, and seeking psychiatric or other mental health consultation as soon as possible.
Anorexia nervosa, bulimia nervosa, and binge eating disorder are the major eating disorders and have a lifetime prevalence of 0.6%, 1%, and 3%, respectively (for a review of eating disorders, see ). Eating disorders primarily affect younger people and have their peak onset between the ages of 10 and 19. These disorders are more common in women than in men. Many young women with eating disorders are secretive about their disorder, do not view it as a problem, and do not seek treatment for it. Gynecologists may see such girls or women for related problems, such as amenorrhea, menstrual dysfunction, low bone density, sexual dysfunction, infertility, anxiety, depression, hyperemesis gravidarum, or other pregnancy complications. Because the woman may not volunteer information about disordered eating, it is important to have a high index of suspicion for eating disorders. A simple five-question self-rating scale, the SCOFF questionnaire ( Box 9.2 ), is highly sensitive and specific in detecting eating disorders in primary care settings and thus is a useful screening tool. The Diagnostic and Statistical Manual, Fifth Edition (DSM-5), diagnostic criteria for anorexia nervosa, bulimia nervosa, and binge eating disorder are listed in Box 9.3 . Of note, the DSM-5 diagnosis of anorexia nervosa is also specified by current severity, with a body mass index (BMI) of 17 kg/m 2 being mild, 16 to 16.99 kg/m 2 moderate, 15 to 15.99 kg/m 2 severe, and less than 15 kg/m 2 extreme.
|
____ Yes | ____ No |
|
____ Yes | ____ No |
|
____ Yes | ____ No |
|
____ Yes | ____ No |
|
____ Yes | ____ No |
| Two or more “yes” answers indicate that the patient may have an eating disorder. | ||
Restriction of energy intake relative to requirements, leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health. Significantly low weight is defined as a weight that is less than minimally normal or, for children and adolescents, less than that minimally expected.
Intense fear of gaining weight or becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight.
Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight.
Coding note: The ICD-9-CM code for anorexia nervosa is 307.1, which is assigned regardless of the subtype. The ICD-10-CM code depends on the subtype.
Specify whether:
(F50.01) Restricting type: During the last 3 months, the individual has not engaged in recurrent episodes of binge eating or purging behavior (i.e., self-induced vomiting or the misuse of laxatives, diuretics, or enemas). This subtype describes presentations in which weight loss is accomplished primarily through dieting, fasting, and/or excessive exercise.
(F50.02) Binge-eating/purging type: During the last 3 months, the individual has engaged in recurrent episodes of binge eating or purging behavior (i.e., self-induced vomiting or the misuse of laxatives, diuretics, or enemas).
Specify if:
In partial remission: After full criteria for anorexia nervosa were previously met, Criterion A (low body weight) has not been met for a sustained period, but either Criterion B (intense fear of gaining weight or becoming fat or behavior that interferes with weight gain) or Criterion C (disturbances in self-perception of weight and shape) is still met.
In full remission: After full criteria for anorexia nervosa were previously met, none of the criteria have been met for a sustained period of time.
Specify current severity:
The minimum level of severity is based, for adults, on current body mass index (BMI) or, for children and adolescents, on BMI percentile. The ranges are derived from World Health Organization categories for thinness in adults; for children and adolescents, corresponding BMI percentiles should be used. The level of severity may be increased to reflect clinical symptoms, the degree of functional disability, and the need for supervision.
Mild: BMI ≥ 17 kg/m 2
Moderate: BMI 16 to 16.99 kg/m 2
Severe: BMI 15 to 15.99 kg/m 2
Extreme: BMI < 15 kg/m 2
Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
Eating, in a discrete period of time (e.g., within any 2-hour period), an amount of food that is definitely larger than most individuals would eat in a similar period of time under similar circumstances.
A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
Recurrent, inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise.
The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months.
Self-evaluation is unduly influenced by body shape and weight.
The disturbance does not occur exclusively during episodes of anorexia nervosa.
Specify if:
In partial remission: After full criteria for bulimia nervosa were previously met, some, but not all, of the criteria have been met for a sustained period of time.
In full remission: After full criteria for bulimia nervosa were previously met, none of the criteria have been met for a sustained period of time.
Specify current severity:
The minimum level of severity is based on the frequency of inappropriate compensatory behaviors. The level of severity may be increased to reflect other symptoms and the degree of functional disability.
Mild: An average of 1 to 3 episodes of inappropriate compensatory behaviors per week.
Moderate: An average of 4 to 7 episodes of inappropriate compensatory behaviors per week.
Severe: An average of 8 to 13 episodes of inappropriate compensatory behaviors per week.
Extreme: An average of 14 or more episodes of inappropriate compensatory behaviors per week.
Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
Eating, in a discrete period of time (e.g., within any 2-hour period), an amount of food that is definitely larger than what most people would eat in a similar period of time under similar circumstances.
A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
The binge-eating episodes are associated with three (or more) of the following:
Eating much more rapidly than normal.
Eating until feeling uncomfortably full.
Eating large amounts of food when not feeling physically hungry.
Eating alone because of feeling embarrassed by how much one is eating.
Feeling disgusted with oneself, depressed, or very guilty afterward.
Marked distress regarding binge eating is present.
Binge eating occurs, on average, at least once a week for 3 months.
The binge eating is not associated with the recurrent use of inappropriate compensatory behavior as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa.
Specify if:
In partial remission: After full criteria for binge-eating disorder were previously met, binge eating occurs at an average frequency of less than one episode per week for a sustained period of time.
In full remission: After full criteria for binge-eating disorder were previously met, none of the criteria have been met for a sustained period of time.
Specify current severity:
The minimum level of severity is based on the frequency of episodes of binge eating. The level of severity may be increased to reflect other symptoms and the degree of functional disability.
Mild: 1 to 3 binge-eating episodes per week.
Moderate: 4 to 7 binge-eating episodes per week.
Severe: 8 to 13 binge-eating episodes per week.
Extreme: 14 or more binge-eating episodes per week.
Anorexia nervosa is characterized by a disturbed body image and fears of becoming fat or gaining weight, even though the person’s body weight is less than expected. Weight loss is achieved by restricting food intake, overexercising, self-induced vomiting, or use of laxatives, emetics, and diuretics. Anorexia is most common in white teenage girls in industrialized Western societies. Societal pressures and standards of attractiveness for women, which emphasize thinness, have long been considered to increase the risk for anorexia nervosa, and a preoccupation with dieting is common in girls at menarche. Increasing evidence indicates, however, that there is clearly a significant genetic contribution to anorexia nervosa and other eating disorders, with heritability estimates of 50% to 80%. Other risk factors include a history of childhood sexual abuse and psychological traits of low self-esteem, perfectionism, and obsessive thinking.
Medical signs and symptoms associated with anorexia nervosa include bradycardia, hypotension, hypothermia, leukopenia, hair loss, skin changes, and constipation. Vomiting or laxative use may cause hypokalemia. Endocrine changes include low estrogen and testosterone levels, amenorrhea, decreased libido, hypercortisolemia, and low bone density. Prolonged QT interval is a serious sequela of anorexia nervosa and has been associated with sudden death. The mortality rate of anorexia nervosa from all causes is 5% to 6% per decade of illness.
Psychiatric symptoms associated with anorexia nervosa include depression, anxiety, social difficulties, sleep disturbance, agitation, poor emotion regulation, rigidity, obsessional thinking, and compulsive behaviors. Interestingly, these symptoms occur in individuals without anorexia nervosa during starvation and resolve with weight gain and so are most likely caused, or at least exacerbated, by the illness.
Anorexia nervosa is difficult to treat (for a review, see ). Women do not usually seek help themselves but instead are brought to treatment by concerned family members. They fear gaining weight, do not see their illness as a problem, are often nonadherent with treatment, feel isolated and do not engage with treatment providers, and may have multiple relapses. About one third recover completely, but this may take a number of years. Early recognition and treatment improve outcome. Family members often become frustrated with the woman’s multiple relapses, lack of insight, and apparent lack of cooperation with treatment and may need support themselves in dealing with her illness.
The best treatment for anorexia nervosa involves referral to a multidisciplinary team, with medical, nutritional, psychological, and psychiatric expertise in this area. The focus is on gradual refeeding to achieve weight gain and on outpatient treatment, with hospitalization only for acute, dangerous medical or psychiatric complications. In adolescents, family therapy focused on eating disorder behavior and weight gain or, in nonintact families, adolescent-centered individual psychotherapy is most effective ( ). In adults, several different types of specialized psychotherapy show promise, including cognitive behavioral, psychodynamic, and supportive therapies adapted specifically for treatment of anorexia. In one randomized controlled trial (RCT), focal psychodynamic therapy seemed to help recovery most at 12 months, whereas enhanced CBT was more effective with speed of weight gain and improvement in eating disorder thinking ( ). Few studies address relapse prevention, although a structured aftercare program after inpatient treatment reduces risk of relapse. There is no clear evidence supporting treatment of anorexia with psychotropic medications. Antidepressants do not promote weight gain or reduce eating disorder symptoms during acute treatment, and their efficacy for relapse prevention is unclear. The atypical antipsychotic olanzapine has been tried with the goal of addressing weight gain and distorted thinking about weight and body shape. A 16-week randomized placebo-controlled trial of 152 outpatients with anorexia nervosa (75 treated with olanzapine and 77 with placebo) showed greater weight gain with olanzapine but no significant differences in psychological symptoms such as obsessional thinking ( ). In this study, olanzapine was prescribed at 2.5 mg daily for 2 weeks, 5 mg daily for 2 weeks, then 10 mg daily, as tolerated.
Bulimia nervosa is characterized by binge eating, combined with inappropriate compensatory mechanisms to avoid weight gain, such as self-induced vomiting, misuse of laxatives or diuretics, or fasting or excessive exercise. Binge eating and compensatory behaviors occur an average of once a week for 3 months (see Box 9.3 for full diagnostic criteria). Bulimia, like anorexia, is most common in young women, has a significant genetic component, may follow teasing or criticism about the woman’s weight or shape, and is thought to involve disturbances in hunger-satiety pathways, the drive system and rewarding characteristics of food, or self-regulation. Comorbidity with mood and anxiety disorders, addictions, and suicidal thoughts and behaviors is common. All-cause mortality rates, including suicide rates, are elevated, with a mortality rate of 3.9% over 8 to 25 years of follow-up.
Women with bulimia nervosa and purging may develop hypokalemia, hyponatremia, hypochloremia, a metabolic alkalosis as a result of vomiting, or a metabolic acidosis with laxative abuse. Recurrent self-induced vomiting can result in loss of dental enamel, parotid gland enlargement, or calluses and scars on the dorsal aspect of the hand. Rare but serious complications include esophageal tears, gastric rupture, rectal prolapse, and cardiac arrhythmias.
There is strong evidence for the efficacy of CBT for bulimia nervosa, although complete remission of binging and purging occurs in only 30% to 40%. Other therapies for which there is some evidence of efficacy are IPT, dialectical behavior therapy (DBT) focusing on emotion regulation, and family therapy in adolescents. Antidepressants are superior to placebo in treatment of bulimia, with the agent of choice being fluoxetine 60 mg daily. Of note, the antidepressant bupropion is contraindicated in women with a history of bulimia because of an elevated risk of seizures, presumably because of electrolyte abnormalities. The outcome of bulimia is full recovery in 45%, significant improvement in 27%, and a chronic, protracted course in about 23%.
In binge eating disorder, the woman binge eats (as in bulimia nervosa) an average of once a week for at least 3 months, but she does not engage in compensatory behaviors such as purging, fasting, or excessive exercise. As a result, she may also develop obesity but does not develop the medical complications associated with purging or low weight. Treatment for binge eating disorder includes nutritional consultation, diet, physical activity, education, and specific psychotherapies. There is strong evidence for the efficacy of CBT in binge eating disorder and other psychotherapies, such as DBT and IPT, are also effective. Medication treatments include antidepressants such as SSRIs. Weight loss agents, topiramate, and stimulants may also be effective.
Although obesity is not uniquely a gynecologic condition, obesity and overweight affect a substantial proportion of patients for whom gynecologists provide care. The prevalence of obesity continues to increase in the United States. The World Health Organization (WHO) definitions for BMI are shown in Table 9.3 . Table 9.4 outlines classification by BMI. In 2016, 39.8% of U.S. adults were obese and 71.6% were overweight or obese. The prevalence of obesity is higher in adults aged 40 to 59, minority women, and low-income women and varies by geographic region. Non-Hispanic Black and Hispanic women have slightly higher prevalence of obesity than non-Hispanic white women, whereas non-Hispanic Asian women have the lowest prevalence. The WHO describes obesity as a global epidemic, contributing substantially to chronic disease and disability.
| BMI (kg/m 2 ) | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Height (inches) | Body Weight (lb) | ||||||||||||||||||
| 58 | 91 | 96 | 100 | 105 | 110 | 115 | 119 | 124 | 129 | 134 | 138 | 143 | 148 | 153 | 158 | 162 | 167 | ||
| 59 | 94 | 99 | 104 | 109 | 114 | 119 | 124 | 128 | 133 | 138 | 143 | 148 | 153 | 158 | 163 | 168 | 173 | ||
| 60 | 97 | 102 | 107 | 112 | 118 | 123 | 128 | 133 | 138 | 143 | 148 | 153 | 158 | 163 | 168 | 174 | 179 | ||
| 61 | 100 | 106 | 111 | 116 | 122 | 127 | 132 | 137 | 143 | 148 | 153 | 158 | 164 | 169 | 174 | 180 | 185 | ||
| 62 | 104 | 109 | 115 | 120 | 126 | 131 | 136 | 142 | 147 | 153 | 158 | 164 | 169 | 175 | 180 | 186 | 191 | ||
| 63 | 107 | 113 | 118 | 124 | 130 | 135 | 141 | 146 | 152 | 158 | 163 | 169 | 175 | 180 | 186 | 191 | 197 | ||
| 64 | 110 | 116 | 122 | 128 | 134 | 140 | 145 | 151 | 157 | 163 | 169 | 174 | 180 | 186 | 192 | 197 | 204 | ||
| 65 | 114 | 120 | 126 | 132 | 138 | 144 | 150 | 156 | 162 | 168 | 174 | 180 | 186 | 192 | 198 | 204 | 210 | ||
| 66 | 118 | 124 | 130 | 136 | 142 | 148 | 155 | 161 | 167 | 173 | 179 | 186 | 192 | 198 | 204 | 210 | 216 | ||
| 67 | 121 | 127 | 134 | 140 | 146 | 153 | 159 | 166 | 172 | 178 | 185 | 191 | 198 | 204 | 211 | 217 | 223 | ||
| 68 | 125 | 131 | 138 | 144 | 151 | 158 | 164 | 171 | 177 | 184 | 190 | 197 | 203 | 210 | 216 | 223 | 230 | ||
| 69 | 128 | 135 | 142 | 149 | 155 | 162 | 169 | 176 | 182 | 189 | 196 | 203 | 209 | 216 | 223 | 230 | 236 | ||
| 70 | 132 | 139 | 146 | 153 | 160 | 167 | 174 | 181 | 188 | 195 | 202 | 209 | 216 | 222 | 229 | 236 | 243 | ||
| 71 | 136 | 143 | 150 | 157 | 165 | 172 | 179 | 186 | 193 | 200 | 208 | 215 | 222 | 229 | 236 | 243 | 250 | ||
| 72 | 140 | 147 | 154 | 162 | 169 | 177 | 184 | 191 | 199 | 206 | 213 | 221 | 228 | 235 | 242 | 250 | 258 | ||
| 73 | 144 | 151 | 159 | 166 | 174 | 182 | 189 | 197 | 204 | 212 | 219 | 227 | 235 | 242 | 250 | 257 | 265 | ||
| 74 | 148 | 155 | 163 | 171 | 179 | 186 | 194 | 202 | 210 | 218 | 225 | 233 | 241 | 249 | 256 | 264 | 272 | ||
| 75 | 152 | 160 | 168 | 176 | 184 | 192 | 200 | 208 | 216 | 224 | 232 | 240 | 248 | 256 | 264 | 272 | 279 | ||
| 76 | 156 | 164 | 172 | 180 | 189 | 197 | 205 | 213 | 221 | 230 | 238 | 246 | 254 | 263 | 271 | 279 | 287 | ||
| BMI (kg/m 2 ) | 36 | 37 | 38 | 39 | 40 | 41 | 42 | 43 | 44 | 45 | 46 | 47 | 48 | 49 | 50 | 51 | 52 | 53 | 54 |
| 58 | 172 | 177 | 181 | 186 | 191 | 196 | 201 | 205 | 210 | 215 | 220 | 224 | 229 | 234 | 239 | 244 | 248 | 253 | 258 |
| 59 | 178 | 183 | 188 | 193 | 198 | 203 | 208 | 212 | 217 | 222 | 227 | 232 | 237 | 242 | 247 | 252 | 257 | 262 | 267 |
| 60 | 184 | 189 | 194 | 199 | 204 | 209 | 215 | 220 | 225 | 230 | 235 | 240 | 245 | 250 | 255 | 261 | 266 | 271 | 276 |
| 61 | 190 | 195 | 201 | 206 | 211 | 217 | 222 | 227 | 232 | 238 | 243 | 248 | 254 | 259 | 264 | 269 | 275 | 280 | 285 |
| 62 | 196 | 202 | 207 | 213 | 218 | 224 | 229 | 235 | 240 | 246 | 251 | 256 | 262 | 267 | 273 | 278 | 284 | 289 | 295 |
| 63 | 203 | 208 | 214 | 220 | 225 | 231 | 237 | 242 | 248 | 254 | 259 | 265 | 270 | 278 | 282 | 287 | 293 | 299 | 304 |
| 64 | 209 | 215 | 221 | 227 | 232 | 238 | 244 | 250 | 256 | 262 | 267 | 273 | 279 | 285 | 291 | 296 | 302 | 308 | 314 |
| 65 | 216 | 222 | 228 | 234 | 240 | 246 | 252 | 258 | 264 | 270 | 276 | 282 | 288 | 294 | 300 | 306 | 312 | 318 | 324 |
| 66 | 223 | 229 | 235 | 241 | 247 | 253 | 260 | 266 | 272 | 278 | 284 | 291 | 297 | 303 | 309 | 315 | 322 | 328 | 334 |
| 67 | 230 | 236 | 242 | 249 | 255 | 261 | 268 | 274 | 280 | 287 | 293 | 299 | 306 | 312 | 319 | 325 | 331 | 338 | 344 |
| 68 | 236 | 243 | 249 | 256 | 262 | 269 | 276 | 282 | 289 | 295 | 302 | 308 | 315 | 322 | 328 | 335 | 341 | 348 | 354 |
| 69 | 243 | 250 | 257 | 263 | 270 | 277 | 284 | 291 | 297 | 304 | 311 | 318 | 324 | 331 | 338 | 345 | 351 | 358 | 365 |
| 70 | 250 | 257 | 264 | 271 | 278 | 285 | 292 | 299 | 306 | 313 | 320 | 327 | 334 | 341 | 348 | 355 | 362 | 369 | 376 |
| 71 | 257 | 265 | 272 | 279 | 286 | 293 | 301 | 308 | 315 | 322 | 329 | 338 | 343 | 351 | 358 | 365 | 372 | 379 | 386 |
| 72 | 265 | 272 | 279 | 287 | 294 | 302 | 309 | 316 | 324 | 331 | 338 | 346 | 353 | 361 | 368 | 375 | 383 | 390 | 397 |
| 73 | 272 | 280 | 288 | 295 | 302 | 310 | 318 | 325 | 333 | 340 | 348 | 355 | 363 | 371 | 378 | 386 | 393 | 401 | 408 |
| 74 | 280 | 287 | 293 | 303 | 311 | 319 | 326 | 334 | 342 | 350 | 358 | 365 | 373 | 381 | 389 | 396 | 404 | 412 | 420 |
| 75 | 287 | 295 | 303 | 311 | 319 | 327 | 335 | 343 | 351 | 359 | 367 | 375 | 383 | 391 | 399 | 407 | 415 | 423 | 431 |
| 76 | 295 | 304 | 312 | 320 | 328 | 336 | 344 | 353 | 361 | 369 | 377 | 385 | 394 | 402 | 410 | 418 | 426 | 435 | 443 |
| Weight | BMI * |
|---|---|
| Normal weight | 18.5-24.9 |
| Overweight | 25.0-29.9 |
| Obesity | >30 |
| Class I | 30.0-34.9 |
| Class II | 35.0-39.9 |
| Class III | >40 |
Waist circumference is another parameter by which to measure obesity and when combined with BMI can be a predictor of obesity-related morbidity. Increased central adiposity is associated with increased risk of morbidity and mortality. The waist circumference can be measured at the level of the anterior superior iliac spine, at the end of expiration. For women with a BMI of 25 to 34.9 kg/m 2 (overweight or class I obesity), a waist circumference of more than 35 inches (88 cm) is associated with heart disease and diabetes mellitus. Risks are increased even more for those with BMI of 35 kg/m 2 or greater (class II or III obesity).
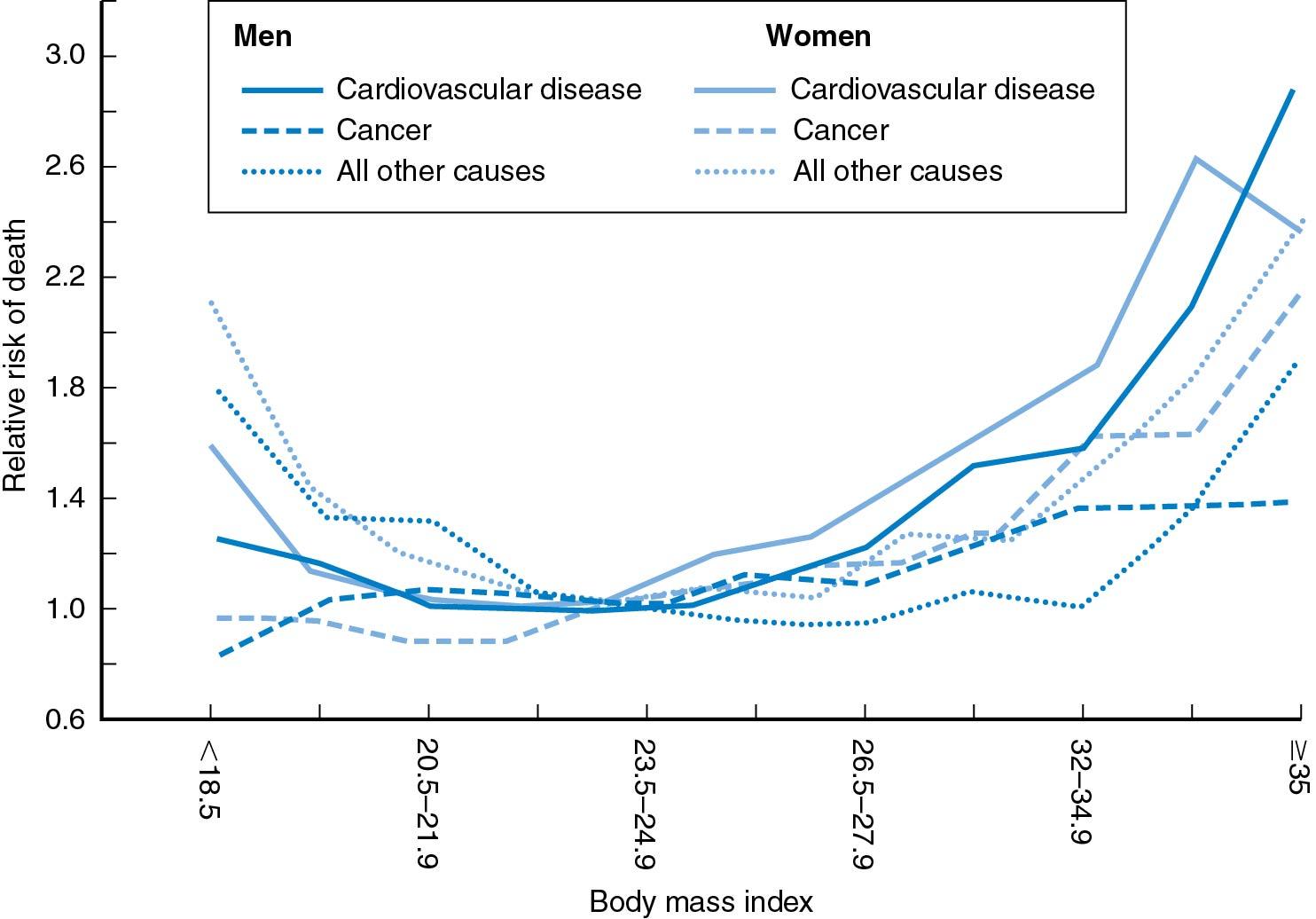
There is a strong relationship between mortality and increased BMI greater than 25 kg/m 2 (and less than 20 kg/m 2 ) ( Fig. 9.1 ). Even in healthy people who have never smoked, at age 50 years there is still an elevated risk of death for persons whose BMIs are between 25 and 30 kg/m 2 ( ). The risk of death increases 20% to 40% in the overweight group and by two to three times among obese persons. Severe obesity is a health hazard that carries a 12-fold increase in mortality.
Obesity often coexists with medical conditions such as hypertension, diabetes mellitus, dyslipidemias, arthritis, and obstructive sleep apnea (OSA). Obesity has been linked to increased operative morbidity and mortality, as well as obstetric and gynecologic conditions, including miscarriage, infertility, endometrial hyperplasia, and some types of cancer. High BMI has also been associated with increased vasomotor symptoms in menopause. One meta-analysis of increased BMI and cancer risk found a strong association between a five-point BMI increase and risk of endometrial cancer (relative risk [RR] 1.59, P < .0001), gallbladder cancer (RR 1.59, P = .04), esophageal adenocarcinoma (RR 1.51, P < .0001), and renal cancer (RR 1.34, P < .0001). A weaker positive association was found with postmenopausal breast, pancreatic, thyroid, and colon cancer plus leukemia, multiple myeloma, and non-Hodgkin lymphoma. The mechanisms of cancer’s association with obesity may be linked to hormone systems like insulin, insulin-like growth factor, sex steroids, adipokines, and other substances.
For overweight individuals or those with class I obesity, diet, exercise, and behavior modification are appropriate interventions. Those with class II or III obesity may benefit from medically supervised diet, exercise, and behavior modification or surgical management. A systematic review of 12 trials found that intensive behavioral counseling, diet (reducing intake by ≥500 kcal/day), and exercise (≥150 minutes of walking/week) lead to clinically meaningful weight loss of 0.3 kg to 6.6 kg over 6 months ( ). Because sustained adherence to diet and exercise modifications can be difficult, surgical intervention (bariatric surgery) is likely to be the most effective approach for those with very high BMI.
Organizations focused on weight management, such as Weight Watchers, may be successful for motivated individuals. Interventions that patients can manage themselves include tracking calorie intake, using smartphone apps for weight loss, avoiding food binges or eating at night, and practicing stress reduction or mindfulness-based training. A meta-analysis of 48 randomized trials of named diet programs reported that the largest weight loss was associated with low-carbohydrate diets and low-fat diets ( ), although differences in weight loss among these programs were minimal. It is more important to find a healthy diet that a person can adhere to long term. Because fat represents 9 Cal/g and protein and carbohydrate represent 4 Cal/g, a change in eating habits can allow an individual to eat more food while reducing unnecessary calories. Adherence to the U.S. Department of Agriculture (USDA) ChooseMyPlate dietary recommendations ( https://www.choosemyplate.gov/ ), which emphasize fruits, vegetables, and grains over meat and dairy, is one way to make healthy diet changes that may facilitate weight loss. The use of portion-controlled servings has also been demonstrated to be effective for weight loss because people in general tend to underestimate how much they eat. Many diet programs prescribe or sell low-fat foods in an attempt to achieve a diet containing about 20% to 30% fat, though individuals may be able to achieve the same results through careful diet planning. Educating patients to change eating habits is important not only for losing weight but also for maintaining weight loss, which is more difficult. Setting a realistic goal of 5% loss of body weight over 6 months is helpful.
Many individuals attempting weight loss have turned to fad diets such as juicing, detoxification, intermittent fasting, and paleo diets. Juicing and detoxification rely primarily on significant caloric restriction and are not sustainable ( ). Intermittent fasting and paleo diets are associated with short-term weight loss and may be more sustainable, but long-term data are lacking and long-term adherence may be problematic or impractical. Many of these diets may also be associated with adverse effects.
Exercise is a useful, and often necessary, addition to diet regimens. Several studies have demonstrated that although similar weight loss can be obtained by both diet alone and diet plus exercise programs, the latter will allow for a greater loss of fat stores while maintaining muscle mass. To maintain this advantage, exercise programs must be maintained. Although exercise alone is not a good method for losing weight, it is beneficial for long-term weight management and overall health. One study looked at amount of physical activity and weight gain in women and concluded that physical activity is inversely related to weight gain in women of normal weight but not in women who are overweight ( ). Getting more active might be manageable for some women via their work commute. A U.K. study found that people who commuted to work by active methods (biking or walking) or public transport had significantly lower BMI and percentage of body fat than people who used private transportation ( ). Presumably, using public transportation required more walking each day. Women in the United States may face challenges obtaining similar benefits because the built environment is often not conducive to exercise. Many areas lack accessible public transportation, and many individuals must commute long distances to work. Further, many in the United States live in neighborhoods where they do not feel safe walking or that lack sidewalks and other amenities that facilitate exercise.
Some attention has focused on what types of exercise may be most beneficial for weight loss. For example, several studies have focused on comparisons between moderate intensity training (MIT), such as distance running or cycling, and high-intensity training (HIT), which involves short bursts of high-intensity exercise. HIT seems to be associated with short-term weight loss and cardiovascular benefits but may not be feasible or safe for those with physical limitations or significant comorbidities, which may be concerns for many obese individuals. A systematic review reported small reductions in percentage of body fat with both HIT and MIT but noted that in the short term neither approach resulted in clinically meaningful reductions in body fat.
Pharmacologic therapy should be used as an adjunct to diet, exercise, and lifestyle modifications, rather than a solo approach. FDA-approved formulations are associated with varying degrees of weight loss. Some medications are approved only for short-term (up to 12 weeks) use, whereas others can be used for a longer duration. Although surgical interventions generally result in greater levels of weight loss than do medications, many approved formulations have been associated with low to moderate weight loss in clinical studies. Medications may be a reasonable approach for those with BMI greater than 30 kg/m 2 or those with BMI 26 to 29.9 kg/m 2 and comorbidities. The initial choice of pharmacologic agent may depend on these and other factors.
Examples of pharmacologic weight loss therapy include orlistat, lorcaserin, phentermine-topiramate, and metformin, although there are several others as well.
Orlistat inhibits dietary fat absorption and is considered first-line treatment because of its favorable safety profile. It is approved for up to 4 years of use. Most subjects can expect about 3% loss of initial weight, though side effects of fecal urgency, flatulence, and oily stools may occur.
Lorcaserin is a serotonin 2c receptor agonist, which reduces appetite. It is an alternative for patients who cannot take orlistat. Over 1 year, about 50% of patients lost at least 3% of their body mass. Side effects include headache, dizziness, fatigue, nausea, and constipation.
Phentermine-topiramate is an acceptable option for postmenopausal women who do not have hypertension or cardiac disease. Up to 70% of individuals taking this medication will lose weight ( ). Warnings include metabolic acidosis, increased heart rate, anxiety, insomnia, and increased creatinine levels. Both lorcaserin and phentermine-topiramate have warnings about memory, attention, and depression.
Metformin is a reasonable initial therapy for individuals who require glycemic control in addition to weight loss.
| Body Mass Index Category | |||||
|---|---|---|---|---|---|
| Treatment | 25-26.9 kg/m 2 | 27-29.9 kg/m 2 | 30-34.9 kg/m 2 | 35-39.9 kg/m 2 | >40 kg/m 2 |
| Diet, physical activity, and behavior therapy | With comorbidities | With comorbidities | + | + | + |
| Pharmacotherapy | With comorbidities | + | + | + | |
| Surgery | With comorbidities | With comorbidities | With comorbidities | ||
There are other available medications as well; a comprehensive list is beyond the scope of this chapter. Long-term safety and efficacy data are limited for many weight loss medications. A guide to selecting treatment for obesity is given in Fig. 9.5 .
Many bariatric surgery patients are women of reproductive age. Bariatric surgery is a proven intervention for weight loss and is associated with improvements in obesity-related medical comorbidities. Eligible candidates for bariatric surgery include those with a BMI greater than 40 kg/m 2 or a BMI greater than 35 kg/m 2 with an obesity-associated comorbidity. Additional considerations include whether nonsurgical weight loss measures have failed, the woman is motivated and well informed, and there is acceptable surgical risk. The majority of postoperative obesity patients have resolution of or improvement in comorbid conditions such as diabetes, hypertension, dyslipidemia, and OSA ( ).
Types of bariatric surgery include malabsorptive procedures, restrictive procedures, and malabsorptive-restrictive procedures. Of the more common procedures, gastric banding is a restrictive procedure, and gastric bypass is both malabsorptive and restrictive. Surgeries can be performed via laparoscopic or open approaches. The chief benefit of bariatric surgery is weight loss, but improvements in comorbidities often occur. In an evaluation of 29 studies and 7971 patients, gastric bypass had better outcomes than gastric banding for long-term weight loss, type 2 diabetic control and remission, and improvements in hypertension and hyperlipidemia. Gastric bypass and sleeve gastrectomy were associated with weight loss exceeding 50% versus 31% in gastric band studies.
Surgical options can provide long-term weight loss but are not without complications. The 30-day mortality from bariatric surgical procedures ranges from 0.1% to 2%, depending on type of procedure and numerous patient factors. Short-term complications include thrombotic events, anastomotic leak, bleeding, and wound infection (all 2% or less), and long-term complications include thrombotic events, anastomotic or band complications, and nutritional deficiencies, particularly of iron and vitamin B 12 . Reproductive-aged patients are advised to avoid pregnancy for 12 to 24 months after surgery to allow stabilization of rate of weight loss and correct nutritional deficiencies. Contraceptive counseling is an important role for the obstetrician-gynecologist in the postbariatric surgery period.
The percentage of young people who are overweight or obese has more than tripled since 1980. In the United States, 20.6% of adolescents aged 12 to 19 are obese, and the prevalence of obesity among adolescent girls is 21%. Standard adult BMI categories should not be applied to adolescents, whose BMI determination should incorporate growth chart data. For adolescents, overweight is defined as a BMI at or greater than the 85th percentile, obesity a BMI at or greater than the 95th percentile, and severe obesity a BMI greater than or equal to the 99th percentile for age.
Adolescents who are affected by obesity are at risk of developing impaired glucose tolerance, cardiovascular disease, nonalcoholic fatty liver disease, disordered breathing, and orthopedic problems. Consequences of these can continue and worsen into adulthood. Abnormal uterine bleeding and polycystic ovary syndrome (PCOS) are also more common among adolescents who are obese. Overweight and obesity during adolescence are also associated with psychosocial conditions, such as low self-esteem.
Diet, exercise, and behavioral modifications are the mainstay of treatment for children and adolescents who are overweight or obese. To be most successful, these interventions must be adopted by the entire family because children and adolescents are not in full control of their environments. A systematic review concluded that effective lifestyle interventions generally require a commitment of 28 hours or more to be effective. It further concluded that weight loss medications offer small benefit that is of unclear clinical significance. Orlistat is approved for use by adolescents and may result in weight loss, but gastrointestinal side effects may limit its use. Other weight loss medications may require further study before their use in adolescents can be recommended
Bariatric surgery may be appropriate for some obese adolescents who meet adult BMI criteria, and have attained at least Tanner IV stage of development or 95% of adult height based on bone age. For appropriately selected adolescent candidates, bariatric surgery can be an effective intervention to effect significant weight loss.
The Centers for Disease Control and Prevention (CDC) advised a multipronged approach to preventing obesity. Recommendations include: (1) increasing consumption of fruits and vegetables; (2) regular physical activity, including for children; (3) increasing physical activity in overweight people to prevent the complications associated with obesity; and (4) breastfeeding, which is associated with a reduced risk of overweight children. Population-based strategies and policies will likely be needed to have widespread impact.
The American College of Obstetricians and Gynecologists (ACOG) has issued guidance for the ethical care of patients with obesity. Providers should be aware of their own implicit bias toward obese patients. As with other aspects of care, obstetrician-gynecologists should incorporate principles of patient-centered counseling and open communication and focus on offering concrete strategies and goals to optimize overall health for individuals with obesity.
Anxiety disorders are the most common psychiatric disorders in the general population. They usually have their onset in childhood, adolescence, or early adulthood and are more common in women than in men. Anxiety is a normal, adaptive response to danger or threat and is associated with physical symptoms (e.g., increased heart rate, sweating, shaking) and cognitive symptoms (e.g., worry, fear). Increases in anxiety are common with life stressors, including medical appointments, diagnoses, and procedures. In addition, anxiety may result from a number of drugs (e.g., caffeine, cannabis, cocaine, methamphetamine, withdrawal of alcohol or opiates), medications (e.g., theophylline, steroids), or medical conditions (e.g., asthma, arrhythmias, temporal lobe epilepsy). Some people experience primary anxiety disorders, which involve excessive anxiety that interferes with daily functioning without apparent explanation or out of proportion to any stressor. Primary anxiety disorders include panic disorder, generalized anxiety disorder (GAD), social anxiety disorder, and specific phobias (for a review of primary anxiety disorders and their treatment, see ). Obsessive-compulsive disorder (OCD) and posttraumatic stress disorder (PTSD), although categorized separately from anxiety disorders in DSM-5, also involve significant anxiety and fear.
Panic disorder is characterized by sudden, intense attacks of fear. The symptom criteria for a panic attack are shown in Box 9.4 . People with panic disorder have recurrent, unexpected panic attacks, with at least one of the attacks followed by a month or more of persistent concern about having additional attacks or worry about their consequences (e.g., losing control, having a heart attack, going crazy) or a maladaptive change in behavior because of panic attacks (e.g., avoiding certain situations for fear of having an attack). About one third of people in the general population have at least one panic attack during their lives, so that a woman presenting with a single panic attack can be reassured that this is very common. Panic attacks can be precipitated by frightening situations or heightened stress, in which case they are called situational panic attacks. People with only situational panic attacks are not diagnosed with panic disorder. Panic attacks without apparent precipitant are called spontaneous.
Note: Symptoms are presented for the purpose of identifying a panic attack; however, panic attack is not a mental disorder and cannot be coded. Panic attacks can occur in the context of any anxiety disorder as well as other mental disorders (e.g., depressive disorders, posttraumatic stress disorder, substance use disorders) and some medical conditions (e.g., cardiac, respiratory, vestibular, gastrointestinal). When the presence of a panic attack is identified, it should be noted with a specifier (e.g., “posttraumatic stress disorder with panic attacks”). For panic disorder, the presence of panic attack is contained within the criteria for the disorder and panic attack is not used with a specifier.
An abrupt surge of intense fear or discomfort that reaches a peak within minutes, and during which time four (or more) of the following symptoms occur:
Note: The abrupt surge can occur from a calm state or an anxious state.
Palpitations, pounding heart, or accelerated heart rate
Sweating
Trembling or shaking
Sensations of shortness of breath or smothering
Feeling of choking
Chest pain or discomfort
Nausea or abdominal distress
Feeling dizzy, unsteady, lightheaded, or faint
Chills or heat sensations
Paresthesias (numbness or tingling sensations)
Derealization (feelings of unreality) or depersonalization (being detached from oneself)
Fear of losing control or “going crazy”
Fear of dying
Note: Culture-specific symptoms (e.g., tinnitus, neck soreness, headache, uncontrollable screaming or crying) may be seen. Such symptoms should not count as one of the four required symptoms.
Panic disorder occurs in 1% to 2% of the population and is about twice as common in women than in men. Risk factors include a family history of panic disorder and significant life stress in the year before the development of symptoms. The disorder has a genetic component, with a heritability of about 30%. Complications include depression in about two thirds of people, and one third are depressed at the time of clinical presentation. Especially because panic attacks are unpredictable, they often lead to anticipatory anxiety (anxiety about having the next panic attack) and phobic avoidance, or avoidance of situations in which the person has had or would fear having a panic attack. These situations commonly include crowds, being in lines or in the middle of an audience, driving (especially in tunnels, over bridges, or in freeways), or other situations in which the woman would feel trapped, unable to get out, or publicly embarrassed. With time, the fear and avoidance surrounding panic attacks often become significantly more distressing and disabling than the attacks themselves and may lead to agoraphobia, or avoidance of multiple situations and activities. Panic disorder, like other anxiety disorders, is also associated with an increased rate of alcohol use as a form of self-medication. Finally, panic and other anxiety disorders are associated with an increased risk for suicide attempts. Thus even though a woman presents with anxiety and does not endorse depression, she should be asked about hopeless or suicidal thoughts.
The treatment of panic disorder includes reassurance, education, general measures, medication, and psychotherapy. Fortunately, treatment response rates are high, so it is possible to be optimistic that the woman has a highly treatable condition. She may fear that she is dying, has a life-threatening or serious medical illness, or that she is “going crazy,” and she can be reassured that, although panic attacks are terrifying, none of these fears is true. Presenting a model of panic attacks as being the body’s natural, healthy “alarm system” that is malfunctioning and being triggered for no reason is often helpful. As general measures, the woman should be counseled to avoid exacerbating factors, such as caffeine, alcohol, stimulants, or other illicit drugs, and to examine possible modifiable sources of increased life stress.
Panic disorder responds well to both medication and psychotherapy. In more severe cases or with significant comorbid phobic avoidance, a combination of both treatments is preferable. However, because both are effective, the approach to treatment can be determined by the woman’s preference. The first-line medication treatment for panic disorder is SSRIs. There are two important differences in prescribing these medications for panic disorder versus for depression. First, people with panic disorder are often very sensitive to medication side effects. Because panic attacks involve feeling out of control of physical sensations and one’s own body, side effects can initially increase anxiety and panic. Thus although ultimately doses need to be similar to antidepressant doses, it is wise to start treatment at a low dose (e.g., a daily dose of 12.5 mg sertraline, 5 mg citalopram), increasing the dose rapidly after a few days if the woman has no side effects. Second, whereas antidepressants take 4 to 6 weeks or less to relieve depression, they can take up to 12 weeks to have their full effect on panic and anxiety, with some effect expected by 6 weeks. It is important to educate the woman about this delayed and gradual onset of action. Many women present in distress and ask about something that will act more rapidly. In cases of severe disability resulting from panic attacks (e.g., inability to function, work, or go to school), it is reasonable to prescribe a benzodiazepine along with an SSRI, with the expectation that the SSRI will be the long-term treatment and the benzodiazepine will be tapered after at most 12 weeks. A benzodiazepine such as clonazepam, which has a longer half-life, requires only twice a day dosing and maintains more constant blood levels, is preferable to shorter-acting agents such as alprazolam. For women with a history of substance use disorders or who need to avoid the potential slowed reflexes, psychomotor impairment, and cognitive slowing associated with benzodiazepines, other alternative adjuncts to reduce anxiety and panic quickly could include hydroxyzine or gabapentin. Buspirone has not been proven effective for panic disorder. In those who do not tolerate SSRIs, most other antidepressants (e.g., venlafaxine, mirtazapine) are also effective for the long-term treatment of panic disorder, with the exception of bupropion, which can increase anxiety symptoms.
Psychotherapy is a highly effective treatment for panic disorder. The best established therapy treatment is CBT, which focuses on addressing the catastrophic thoughts associated with panic attacks (e.g., “I’m dying,” “I’m going to crash my car and kill myself and other people”), learning coping and anxiety reduction strategies (e.g., relaxation, paced breathing to combat hyperventilation), and a gradual approach to feared situations to decrease disability. CBT for panic disorder is a weekly therapy for about 12 to 16 weeks, has significant improvement rates equal to or better than the 70% response rate with medication, yields long-term benefits after therapy is over, and increases the patient’s sense of mastery and control, which is valuable in a disorder that makes people feel out of control. CBT can also help patients tolerate medication side effects and benzodiazepine withdrawal symptoms.
Overall, of the varied symptoms of panic disorder, panic attacks are the easiest to treat and quickest to resolve with both medication and therapy. Phobic avoidance and anticipatory anxiety usually linger for a longer time because of the unpredictability of panic attacks. People with panic disorder in most cases have a relapsing and remitting condition that requires long-term medication treatment (at least a year and often longer) and may recur in periods of increased stress.
In contrast with the sudden attacks of fear in panic disorder, GAD is characterized by excessive anxiety and worry about a number of life situations (e.g., work, school, family members) occurring more days than not for at least 6 months. The patient experiences her worries as excessive and difficult to control and as causing significant distress or trouble functioning. In addition, she has three or more of the following symptoms associated with her anxiety and worry: restlessness, insomnia, muscle tension, fatigue, trouble concentrating, or irritability. GAD usually begins early in life, is about twice as common in women than in men, has a genetic component, and has a lifetime prevalence of 5%. This is often a chronic disorder, with other lifetime psychiatric diagnoses (depression, other anxiety disorders, substance use disorders) superimposed in up to 90% of people. The restlessness and trouble concentrating associated with GAD and anxiety in general may lead to a misdiagnosis of attention deficit disorder.
The treatment of GAD often depends on the need to treat comorbid psychiatric conditions, which may have actually led the woman to seek medical help. GAD itself responds to general measures such as avoiding caffeine, alcohol, and illicit drugs; medication; and psychotherapy. Antidepressants are effective for GAD, and the first-line long-term medication treatment is an SSRI. Buspirone 30 to 60 mg daily is effective for GAD and has few side effects. Hydroxyzine and beta-blockers have been shown to be effective, as have benzodiazepines. However, given the chronic, often lifelong course of GAD, benzodiazepines are not recommended. Psychotherapy for GAD focuses on addressing and coping with worry (“What if” thoughts).
Social anxiety disorder (or social phobia) refers to anxiety in and avoidance of social situations, where the patient is or feels as though she is the center of attention and fears humiliation, embarrassment, or being judged negatively by other people (for diagnostic criteria, see Box 9.5 ). Symptoms of social anxiety disorder can include full-blown panic attacks, but these are provoked by social situations and are not spontaneous. In many cases, social anxiety disorder is restricted to specific situations, most often public speaking or other public performances. Some people have a more pervasive form of this disorder, in which fears and avoidance relate not just to public performance but to most social situations and interactions, such as meeting new people, parties, initiating and maintaining conversations, dating, group projects, speaking with authority figures, or asserting oneself.
Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. Examples include social interactions (e.g., having a conversation, meeting unfamiliar people), being observed (e.g., eating or drinking), and performing in front of others (e.g., giving a speech).
Note : In children, the anxiety must occur in peer settings and not just during interactions with adults.
The individual fears that he or she will act in a way or show anxiety symptoms that will be negatively evaluated (i.e., will be humiliating or embarrassing; will lead to rejection or offend others).
The social situations almost always provoke fear or anxiety.
Note: In children, the fear or anxiety may be expressed by crying, tantrums, freezing, clinging, shrinking, or failing to speak in social situations.
The social situations are avoided or endured with intense fear or anxiety.
The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context.
The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more.
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
The fear, anxiety, or avoidance is not attributable to the physiologic effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
The fear, anxiety, or avoidance is not better explained by the symptoms of another mental disorder, such as panic disorder, body dysmorphic disorder, or autism spectrum disorder.
J. If another medical condition (e.g., Parkinson’s disease, obesity, disfigurement from burns or injury) is present, the fear, anxiety, or avoidance is clearly unrelated or is excessive.
Specify if:
Performance only: If the fear is restricted to speaking or performing in public.
Social anxiety disorder has lifetime and 12-month prevalences of 13% and 8%, respectively. Age of onset is usually early in life (mean 13 years), and women are more commonly affected than men. In Asian cultures, social anxiety often focuses on fears of giving offense to other people—for example, through making inappropriate eye contact, body odor, flatulence, or blushing. There is evidence for a genetic or familial risk for this condition. Women with social anxiety disorder may have associated poor self-esteem, difficulty asserting themselves, depression, or problematic alcohol use. Social anxiety disorder may be difficult to differentiate from shyness, although by definition social anxiety disorder involves marked distress or impairment in functioning.
Treatment of social anxiety disorder also includes medication and psychotherapy ( ). SSRIs are the first-line medication treatment and, as in other anxiety disorders, may take 8 to 12 weeks to have their full therapeutic effect. The SNRI venlafaxine is also effective. MAO inhibitors, though effective, bring with them dietary restrictions and risk of hypertensive crisis. Beta-blockers are helpful for performance anxiety but not for more generalized social anxiety disorder. Benzodiazepines are effective but should be used with caution because of the chronicity of this disorder, its comorbidity with alcohol use disorder, and risks of tolerance, dependence, withdrawal, sedation, psychomotor slowing, and cognitive effects with benzodiazepines. There is some evidence for efficacy of gabapentin or pregabalin. Women with social anxiety restricted to public speaking may benefit from practicing public speaking in a safe setting. CBT for social anxiety disorder is very effective. CBT includes individual treatment focusing on distorted thoughts about social situations (e.g., thoughts that the patient will make a fool of herself, has embarrassed herself, and that this will have catastrophic consequences) and on problem solving around and role-playing feared situations. Surprisingly, group CBT is also effective for social anxiety disorder. CBT and SSRIs yield response rates of 50% to 65% compared with a placebo response rate of 32%. Other psychotherapies, including mindfulness-based stress reduction, IPT, and psychodynamic therapy, appear promising but require further study.
Specific phobias occur in up to 20% of the general population and include fears of specific animals (e.g., snakes, spiders), phenomena (e.g., lightning), or situations (e.g., heights, flying in airplanes, driving, medical or dental procedures). People usually come to medical attention for specific phobias when these interfere with daily life or with their medical treatment. For example, people may develop specific phobias related to repeated medical events like chemotherapy treatments or to necessary aspects of their daily life, such as driving or traveling by plane. The best treatment for a specific phobia is desensitization, or gradually confronting the feared situation with the aid of an anxiety reducing strategy such as relaxation or imagery. In an acute situation, a benzodiazepine may help the woman to get through the particular event, but this will not reduce her future fear of the same situation.
OCD is characterized by persistent, repetitive thoughts, ideas, or images that the patient finds irrational and intrusive (obsessions), and with repetitive behaviors or rituals (compulsions) designed to decrease the anxiety caused by obsessions. Common obsessions include fears of contamination, dirt, germs, and illness; doubts (e.g., about having locked the door, turned off the oven, run over someone in one’s car); needing to have things in order; and sexual or religious images or preoccupations. Compulsions include repetitive and excessive washing, cleaning, checking, putting things in order, or asking for reassurance. These obsessions and compulsions are distressing, time-consuming, or interfere with functioning. The full diagnostic criteria are shown in Box 9.6 . Although most people with OCD realize that their obsessions and compulsions are irrational, some have poor or absent insight and think that their OCD-related beliefs may be true.
Presence of obsessions, compulsions, or both:
Obsessions are defined by (1) or (2):
Recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress.
The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion).
Compulsions are defined by (1) and (2):
Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels driven to perform in response to an obsession or according to rules that must be applied rigidly.
The behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive.
Note: Young children may not be able to articulate the aims of these behaviors or mental acts.
The obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day), or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The obsessive-compulsive symptoms are not attributable to the physiologic effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
The disturbance is not better explained by the symptoms of another mental disorder (e.g., excessive worries, as in generalized anxiety disorder; preoccupation with appearance, as in body dysmorphic disorder; difficulty discarding or parting with possessions, as in hoarding disorder; hair pulling, as in trichotillomania [hair-pulling disorder]; skin picking, as in excoriation [skin-picking] disorder; stereotypies, as in stereotypic movement disorder; ritualized eating behavior, as in eating disorders; preoccupation with substances or gambling, as in substance-related and addictive disorders; preoccupation with having an illness, as in illness anxiety disorder; sexual urges or fantasies, as in paraphilic disorders; impulses, as in disruptive, impulse-control, and conduct disorders; guilty ruminations, as in major depressive disorder; thought insertion or delusional preoccupations, as in schizophrenia spectrum and other psychotic disorders; or repetitive patterns of behavior, as in autism spectrum disorder).
Specify if:
With good or fair insight: The individual recognizes that obsessive-compulsive disorder beliefs are definitely or probably not true or that they may or may not be true.
With poor insight: The individual thinks obsessive-compulsive disorder beliefs are probably true.
With absent insight/delusional beliefs: The individual is completely convinced that obsessive-compulsive disorder beliefs are true.
Specify if:
Tic-related: The individual has a current or past history of a tic disorder.
OCD has a lifetime prevalence of 2% to 3% and is more common in monozygotic than dizygotic twins and in first-degree relatives of affected individuals than in the general population. Rates are similar in men and women. However, men have an earlier peak age of onset than women (6 to 15 years old vs. 20 to 29 years old) and a higher comorbidity with Tourette’s syndrome and tic disorders. In people with OCD, the incidence of Tourette’s is 5% to 7% and of tics is 20% to 30%. Other conditions commonly associated with OCD, in both genders, include major depression, anxiety disorders, hypochondriacal concerns, and excessive use of alcohol and sedatives.
Treatment of OCD includes both medications and psychotherapy ( ). The first-line treatment is serotonergic antidepressants, specifically SSRIs and clomipramine, which is a highly serotonergic tricyclic antidepressant. People with OCD may require higher doses of these medications than do depressed patients and take about 12 weeks for a full response. Response rates tend to be lower than in anxiety disorders and are generally 40% to 60%. It is uncommon for a patient with OCD to have complete resolution of symptoms, and this is usually a chronic, relapsing and remitting disorder requiring ongoing treatment. The specific psychotherapy treatment most helpful in OCD is exposure and response prevention. This treatment involves gradually increasing exposure to the feared situation, without performing the compulsive ritual (e.g., exposure to dirt without the ability to wash one’s hands). Patients who agree to this treatment must tolerate significant anxiety, which, however, subsides with time after each exposure and diminishes over the course of treatment.
PTSD refers to a characteristic set of responses to a traumatic situation that involves exposure to actual or threatened death, serious injury, or sexual violence, either to oneself or experienced by witnessing the trauma occurring to others , learning that the trauma has happened to a close friend or family member, or working in a setting with repeated or extreme trauma exposure. The characteristic responses include symptoms of reexperiencing the event, avoidance of stimuli associated with the event, negative thoughts and mood associated with the trauma, and increased arousal. The full diagnostic criteria and lists of symptoms are given in Box 9.7 . It is common for people to experience symptoms like this in the first month after a major trauma, in which case the diagnosis is acute stress disorder. After a month, when most people would have recovered, persistent symptoms are then diagnosed as PTSD.
Note: The following criteria apply to adults, adolescents, and children older than 6 years.
Exposure to actual or threatened death, serious injury, or sexual violence in one (or more) of the following ways:
Directly experiencing the traumatic event(s)
Witnessing, in person, the event(s) as it occurred to others
Learning that the traumatic event(s) occurred to a close family member or close friend. In cases of actual or threatened death of a family member or friend, the event(s) must have been violent or accidental
Experiencing repeated or extreme exposure to aversive details of the traumatic event(s) (e.g., first responders collecting human remains; police officers repeatedly exposed to details of child abuse).
Note: Criterion A4 does not apply to exposure through electronic media, television, movies, or pictures, unless this exposure is work related.
Presence of one (or more) of the following intrusion symptoms associated with the traumatic event(s), beginning after the traumatic event(s) occurred:
Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).
Note: In children older than 6 years, repetitive play may occur in which themes or aspects of the traumatic event(s) are expressed.
Recurrent distressing dreams in which the content and/or effect of the dream are related to the traumatic event(s).
Note: In children, there may be frightening dreams without recognizable content.
Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. (Such reactions may occur on a continuum, with the most extreme expression being a complete loss of awareness of present surroundings.)
Note: In children, trauma-specific reenactment may occur in play.
Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
Marked physiologic reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event(s).
Persistent avoidance of stimuli associated with the traumatic event(s), beginning after the traumatic event(s) occurred, as evidenced by one or both of the following:
Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
Negative alterations in cognitions and mood associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidence by two (or more) of the following:
Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs).
Persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” “The world is completely dangerous,” “My whole nervous system is permanently ruined”).
Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others.
Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame).
Markedly diminished interest or participation in significant activities.
Feelings of detachment or estrangement from others.
Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings).
Marked alterations in arousal and reactivity associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by two (or more) of the following:
Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects.
Reckless or self-destructive behavior.
Hypervigilance.
Exaggerated startle response.
Problems with concentration.
Sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep).
Duration of the disturbance (Criteria B, C, D, and E) is more than 1 month.
The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The disturbance is not attributable to the physiologic effects of a substance (e.g., medication, alcohol) or another medical condition.
Specify whether:
With dissociative symptoms: The individual’s symptoms meet the criteria for posttraumatic stress disorder, and in addition, in response to the stressor, the individual experiences persistent or recurrent symptoms of either of the following:
Depersonalization: Persistent or recurrent experiences of feeling detached from, and as if one were an outside observer of, one’s mental processes or body (e.g., feeling as though one were in a dream; feeling a sense of unreality of self or body or of time moving slowly).
Derealization: Persistent or recurrent experiences of unreality of surroundings (e.g., the world around the individual is experienced as unreal, dreamlike, distant, or distorted).
Note: To use this subtype, the dissociative symptoms must not be attributable to the physiologic effects of a substance (e.g., blackouts, behavior during alcohol intoxication) or another medical condition (e.g., complex partial seizures).
PTSD has an estimated lifetime prevalence of 8% in adults in the United States. Rates of PTSD vary from one third to more than half of people exposed to specific traumas, such as combat, rape, or captivity. Risk factors for development of PTSD in people exposed to a specific trauma include female sex, younger age, severity and duration of the event, lack of social support, history of prior trauma, and history of preexisting psychiatric disorders. There is also evidence that people with greater autonomic arousal (higher heart rate and blood pressure) after the trauma are at increased risk. Although PTSD would appear to be a quintessentially environmentally determined disorder, the risk of development of PTSD after trauma appears to be heritable. PTSD is associated with depression, panic attacks and anxiety, substance abuse and dependence, suicidal thoughts and attempts, and, in severe cases, psychotic symptoms such as hallucinations or paranoia.
Several types of individual and group psychotherapy are effective in the treatment of PTSD. These therapies include coping with current life problems and triggers, exposure to and reexperiencing of the trauma through a trauma narrative with desensitization (e.g., prolonged exposure, eye movement desensitization, and reprocessing therapies), and examining any distorted thoughts about the trauma, such as guilt that the woman brought this on herself or could have done more to prevent or stop it (cognitive processing therapy). It is important to recognize that many people are retraumatized and their symptoms worsened by retelling the story of the trauma, especially if this is not in the context of a structured, ongoing psychotherapeutic treatment.
Medications are often used to address symptoms of PTSD. For example, SSRIs are effective in reducing depression, anxiety, and emotional numbing. Hypnotics may be helpful for insomnia. Prazosin, an alpha-adrenergic antagonist, may be helpful in reducing trauma-related nightmares and more general PTSD symptoms. Benzodiazepines should be used with caution, given the comorbidity with substance use disorders and reports of increased impulsivity in patients with PTSD given these medications. Acute management immediately after the trauma of a rape is discussed further later in the chapter.
The gynecologist often sees women who are taking psychotropic medications for one of the disorders described earlier or for other less common psychiatric disorders such as bipolar disorder or schizophrenia and may be called on to advise them about options for birth control. There are several psychotropic medications that alter the metabolism and efficacy of oral contraceptives (OCs) or whose metabolism is in turn altered by OCs ( ).
Induction of the hepatic cytochrome P450 3A4 enzyme can increase OC metabolism and cause contraceptive failure. Psychotropic medications that induce 3A4 and that have been associated with spotting, breakthrough bleeding, or unwanted pregnancy include the mood stabilizers carbamazepine (Tegretol) and oxcarbazepine (Trileptal), topiramate (Topamax; at doses >200 mg daily), and the wakefulness-enhancing agent modafinil (Provigil). St. John’s wort, commonly used over the counter as an antidepressant, also induces 3A4 and can cause contraceptive failure. OC activity may be increased or prolonged by 3A4 inhibitors such as the antidepressants fluoxetine (Prozac) and possibly fluvoxamine (Luvox).
OCs are themselves moderate 1A2 and 2C19 inhibitors and mild 2B6 and 3A4 inhibitors. Thus OCs can increase levels and effects of amitriptyline (Elavil), bupropion (Wellbutrin), chlordiazepoxide (Librium), chlorpromazine (Thorazine), clozapine (Clozaril), diazepam (Valium), imipramine (Tofranil), and possibly olanzapine (Zyprexa). Drugs whose clearance is increased with OCs and therefore have lower blood levels include nicotine and the mood stabilizers lamotrigine (Lamictal) and valproic acid (Depakote). Lamotrigine levels have been found to be 84% higher in the week off ethinyl estradiol. Given the risk of Stevens-Johnson syndrome with fluctuating levels of lamotrigine and the likelihood of worsening mood symptoms with variations in blood levels of mood stabilizers such as lamotrigine and valproic acid, it is best to advise women taking these medications to use a continuous OC or another form of birth control.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here