Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute decompensated heart failure (ADHF) is a clinical syndrome of worsening signs or symptoms of heart failure (HF) requiring hospitalization or other unscheduled medical care. For many years, ADHF was viewed as simply an exacerbation of chronic HF as a result of volume overload, with few implications beyond a short-term need to intensify diuretic therapy (a similar paradigm to exacerbations of chronic asthma). Recent decades have seen an explosion of research into the epidemiology, pathophysiology, outcomes, and treatment of ADHF. Although some controversy persists, multiple lines of evidence now support the concept that ADHF is a unique clinical syndrome with its own epidemiology and underlying mechanisms and that there is a need for specific therapies. This viewpoint suggests that ADHF is not just a worsening of chronic HF any more than an acute myocardial infarction (MI) is just a worsening of chronic angina.
Outcome data from a variety of studies now support the concept that hospitalization for ADHF can often signal a dramatic change in the natural history of the HF syndrome. Rates of rehospitalization or death are as high as 50% within 6 months of the initial ADHF event, which is a much higher event rate than is seen with acute MI.
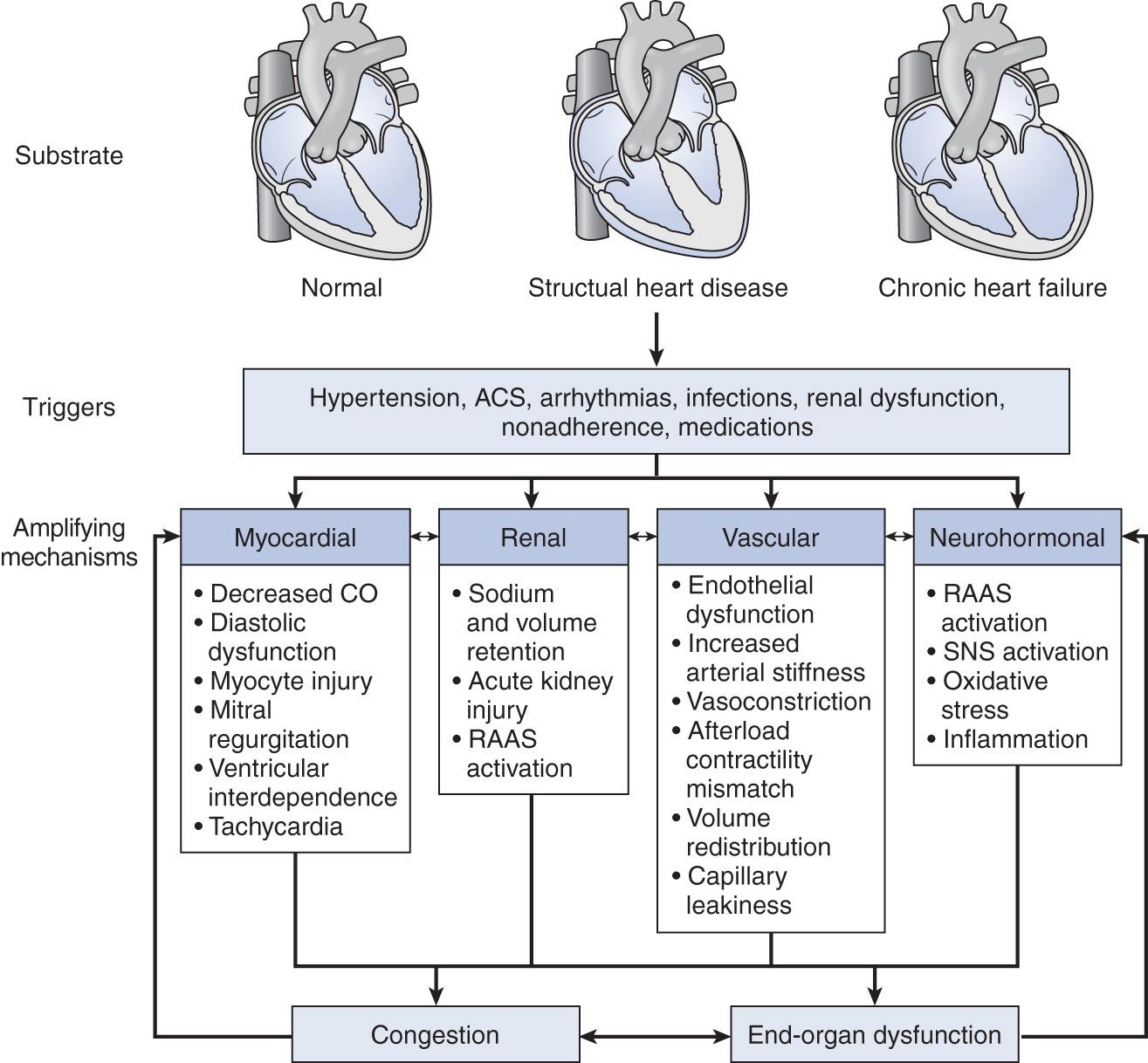
A schematic representation of the pathophysiology of acute HF is given in Fig. 26.1 .
There is great interest in developing a framework for understanding ADHF that would assist in stratifying patients, guiding therapy, and developing new treatments, similar to the basic framework developed for acute coronary syndromes (i.e., ST-segment elevation myocardial infarction [STEMI], non–ST-segment elevation myocardial infarction [NSTEMI], and unstable angina). Although this area is rapidly evolving, a few general clinical phenotypes of ADHF have emerged.
Hypertensive acute heart failure: Data from large registries such as the Acute Decompensated Heart Failure National Registry (ADHERE) and Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) have shown that a substantial portion of ADHF patients is hypertensive on initial presentation to the emergency department. Such patients often have relatively little volume overload (see discussion of volume redistribution later) and preserved or only mildly reduced ventricular function and are more likely to be older and female. Symptoms often develop quickly (minutes to hours), and many such patients have little or no history of chronic HF. Hypertensive urgency or emergency with acute pulmonary edema represents an extreme form of this phenotype.
Decompensated heart failure: This describes patients with a background of significant chronic HF who develop symptoms of volume overload and congestion over a period of days to weeks. These patients typically have significant left ventricular dysfunction and chronic HF at baseline. Although specific triggers are poorly understood, episodes are often triggered by noncompliance with diet or medical therapy.
Cardiogenic shock/advanced heart failure: Although patients with advanced forms of HF are often seen in tertiary care centers, they are relatively uncommon in the broader population (probably fewer than 10% of ADHF hospitalizations). These patients may present with so-called low-output symptoms that may make diagnosis challenging, including confusion, fatigue, abdominal pain, or anorexia. Hypotension (systolic blood pressure [SBP] less than 90 mm Hg) and significant end-organ dysfunction (especially renal dysfunction) are common features. Many of these patients have concomitant evidence of significant right ventricular dysfunction, with ascites or generalized anasarca.
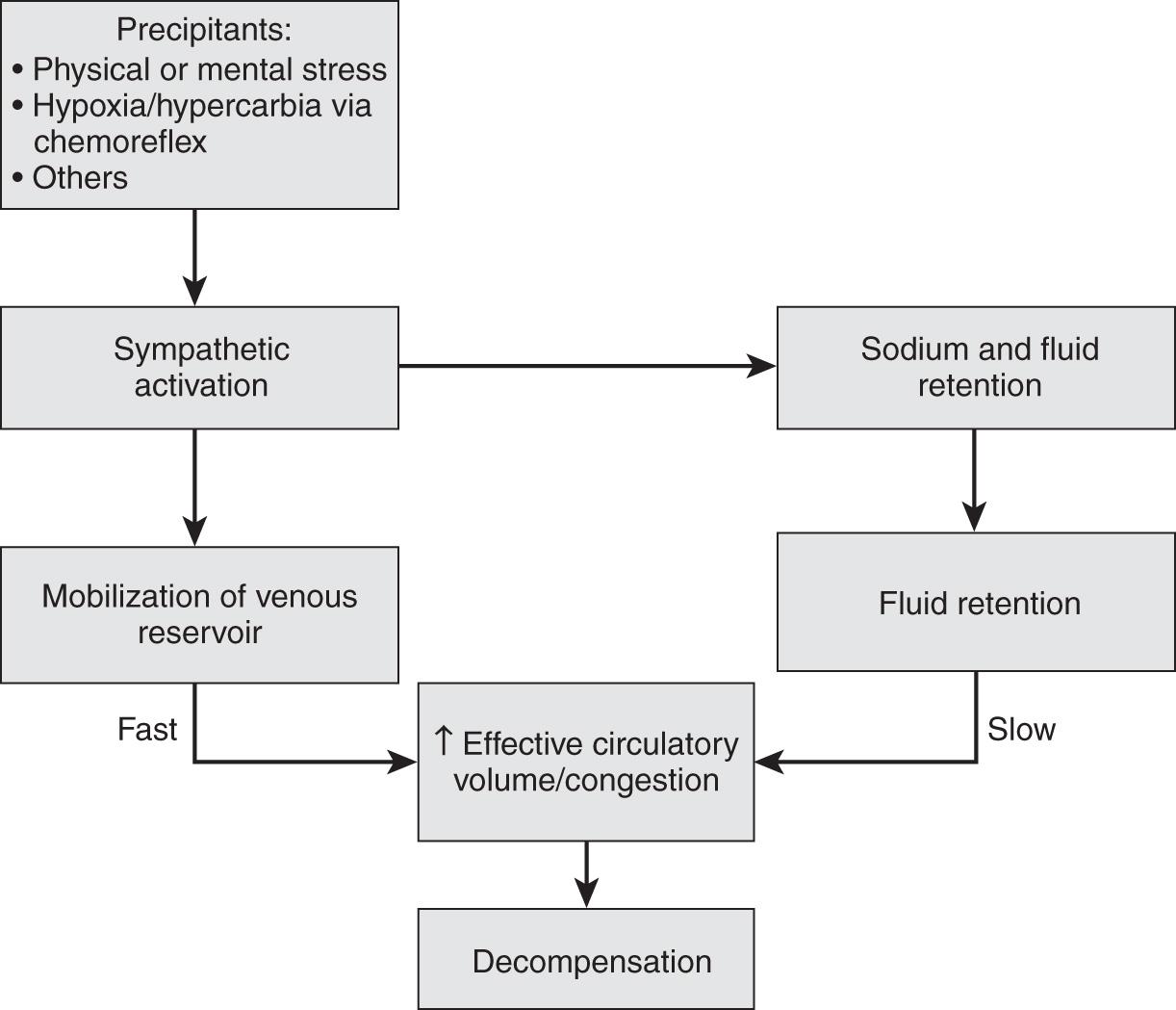
The classic teaching of HF pathophysiology emphasizes the mechanism of poor forward flow (i.e., low cardiac output), resulting in neurohumoral upregulation and poor end-organ function. There is increasing recognition of the central role of systemic congestion as both the consequence and a driver of HF progression. Registry data demonstrate that only about 50% of patients presenting with ADHF gain greater than 2 pounds in weight prior to admission. The transition from chronic HF to ADHF is associated with a progressive increase in cardiac filling pressures. Right-sided cardiac filling pressures begin to increase within 5 days preceding an admission for ADHF, often preceding measurable weight gain or the onset of symptoms. This suggests an internal volume redistribution as a component of ADHF. The largest storage compartment for intravascular volume and likely source of internal volume redistribution is the splanchnic vascular bed. Chronic HF results in splanchnic vascular congestion due to poor cardiac function and a poor vascular capacity due to an increased sympathetic tone, reducing the buffering ability of the abdominal compartment. Since volume redistribution rather than volume gain can be the driver of ADHF, systemic or regional (splanchnic) vasodilation can be a more suitable therapy for this phenotype of ADHF ( Fig. 26.2 ).
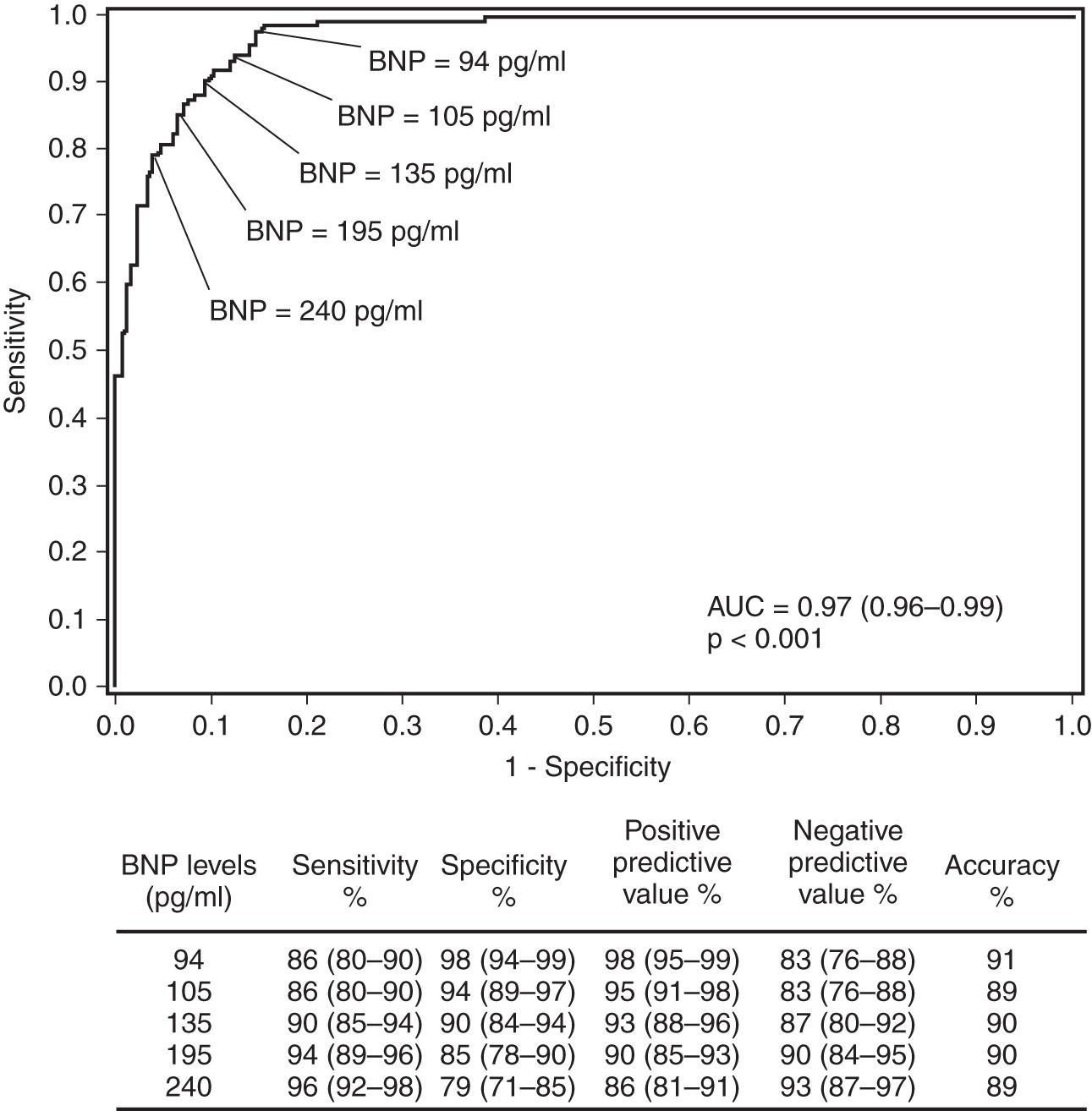
Although the clinical symptoms (dyspnea, paroxysmal nocturnal dyspnea [PND], orthopnea, fatigue) and signs (elevated jugular venous pressure, pulmonary rales, edema) of ADHF are well known, the diagnosis can often be challenging in patients presenting to acute care settings. This is especially true in the elderly and patients with significant comorbid conditions such as chronic obstructive pulmonary disease (COPD). The development of natriuretic peptides as a diagnostic tool has been a major advance in ADHF diagnosis. The clinically available natriuretic peptides for ADHF diagnosis include B-type natriuretic peptide (BNP) and its biologically inert amino-terminal fragment, N-terminal pro-B-type natriuretic peptide (NT-proBNP). Despite some subtle differences between these two biomarkers, they provide similar diagnostic information when used in patients presenting to the emergency department with unexplained dyspnea, although the range of values is significantly different (in general, NT-proBNP levels are approximately 5–10 times greater than BNP levels in the same patient). The landmark Breathing Not Properly Study measured BNP levels in 1586 patients presenting to the emergency department with unexplained dyspnea. In this study, treating physicians were blinded to BNP values, and a panel of cardiologists adjudicated whether hospitalizations were due to ADHF or other causes (based on all clinical data other than the BNP values). As shown in Fig. 26.3 , a cutoff of 100 pg/mL of BNP had a positive predictive value of 79% and a negative predictive value of 89% for the diagnosis of ADHF. The area under the receiver operating curve (ROC) was 0.91, suggesting a very high degree of accuracy for establishing the diagnosis of ADHF. Subsequent studies have demonstrated similar findings for NT-proBNP, although optimal diagnostic cutoffs are different (450 pg/mL for patients younger than 50 years and 900 pg/mL for patients older than 50 years). The use of natriuretic peptide has now become standard of care in the diagnosis of patients with dyspnea presenting to acute care settings and has a class I indication (“should be done”) in clinical practice guidelines. A potentially important new development in the interpretation of natriuretic peptides is the approval of valsartan/sacubitril (Entresto) for chronic HF. This medication increases BNP levels (presumably due to inhibition of neprilysin, which catalyzes the degradation of BNP) but decreases NT-proBNP levels (reflecting an improved hemodynamic state).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here