Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
When patients present with chest pain, the clinician needs to be alert and thorough in trying to determine its cause. The patient’s demographic characteristics together with a careful history should provide the initial information for understanding the likely etiologies. The addition of bedside evaluation by means of physical examination, chest radiography, and electrocardiography (ECG) should further narrow the differential diagnosis. However, more advanced diagnostic tools are frequently needed. Depending on the specific clinical scenario, the choices could range from cardiac biomarkers (e.g., troponin, and creatine kinase-MB, B-type natriuretic peptide, D-dimer) to a variety of advanced cardiac imaging tests such as cardiac computed tomography (CT), magnetic resonance imaging (MRI), stress test, and transthoracic or transesophageal echocardiograms. Although determining the likelihood of coronary artery disease as the reason for chest pain, it is of paramount importance (both for chronic and acute chest pain syndromes) for clinicians not to overlook other significant differential diagnoses ( Table 42.1 ). Importantly, point-of-care cardiac ultrasound (POCUS) is becoming a tool available to newer, nontraditional users such as emergency department (ED) physicians and intensivists for a focused evaluation that will address specific clinical questions according to individual patient’s needs. The role of echocardiography in this process, including POCUS, is discussed in this section with an emphasis on the differential diagnosis of acute chest pain syndromes. The use of echocardiography and stress echocardiography in stable chronic syndromes is discussed in other chapters.
| Acute CP | Cardiac | ACS Pericarditis Myocarditis Takotsubo cardiomyopathy |
WMA with coronary distribution Pericardial effusion WMA with: noncoronary distribution Apical ballooning or other noncoronary WMA |
| Noncardiac | Pulmonary embolism Aortic dissection and acute aortic syndromes Pneumothorax Pleuritic syndromes Musculoskeletal Gastroesophageal |
RV strain, McConnell sign, thrombus in transit Aortic aneurysm, flap, AI, pericardial effusion Loss of pleural sliding and B lines Pleural fluid None None |
|
| Chronic CP | Cardiac | Stable CAD Pericarditis Valvular diseases Cardiac tumors |
WMA with coronary distribution Pericardial effusion Aortic stenosis, MV prolapse LA myxoma |
| Noncardiac | Gastroesophageal Musculoskeletal |
None None |
Patients with acute chest pain represent a large percentage of the ED visits in the United States and worldwide and therefore incur a large burden to the health care system. Because of its safety and easy availability, echocardiography is a very useful tool in addressing the differential diagnosis for these patients, particularly in detecting potentially life-threatening conditions. Careful evaluation of left ventricular (LV) regional and global wall motion has the highest yield in detecting acute coronary syndromes (ACSs). However, evaluation of other structures such as the right ventricle (RV), aorta, pericardium, lungs, or pleura can detect other pathologies responsible for the clinical presentation. The use of a focused POCUS in acute chest pain evaluation has been extensively embraced in recent years and addressed in a joint document form the American Society of Echocardiography (ASE) and the American College of Emergency Physicians.
Evaluation of the LV function, regional wall motion, and thickening as well as its morphology can be of critical significance in detecting ACSs and cardiomyopathies.
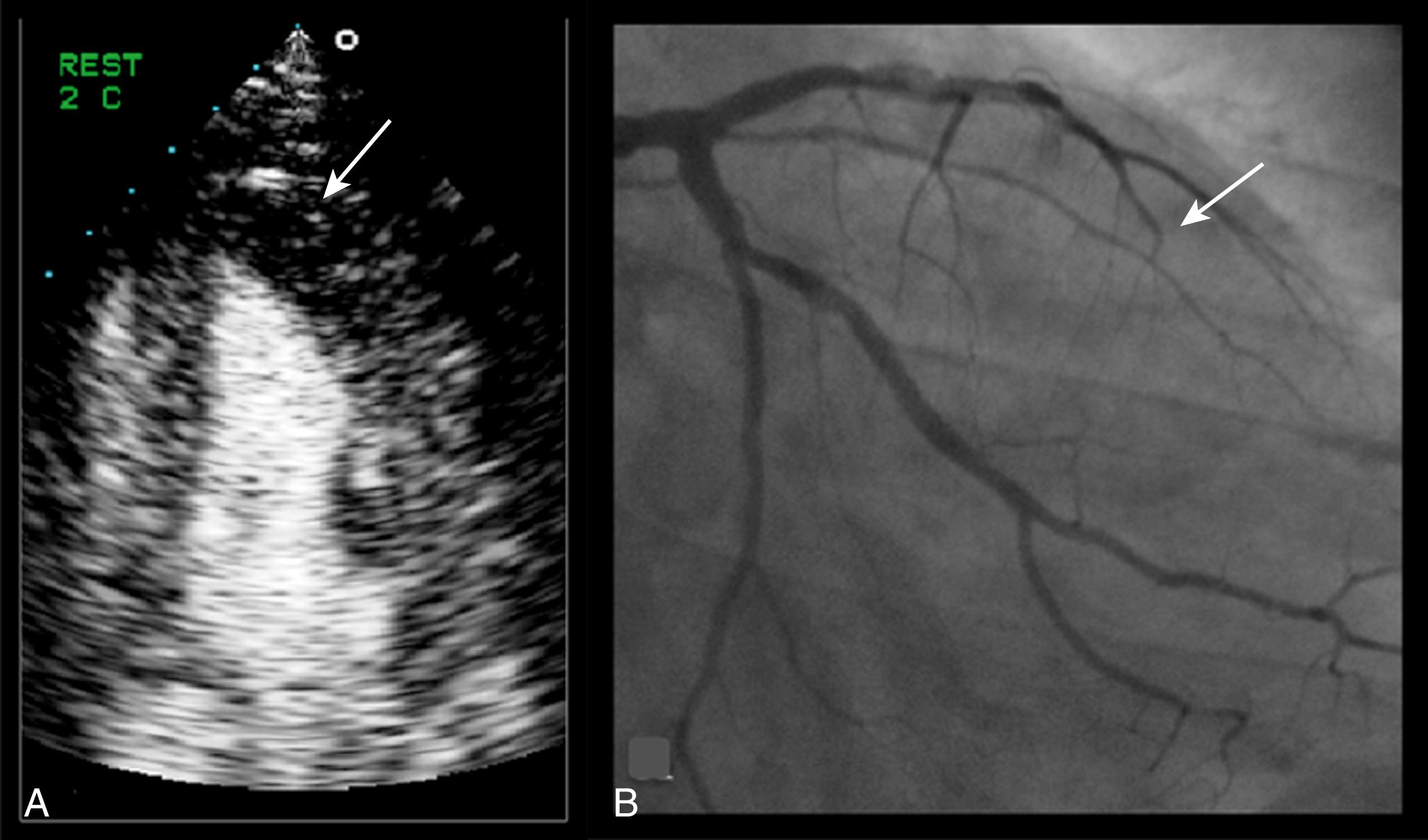
As an acute coronary event occurs, coronary flow through the vessel is impaired, resulting in myocardial ischemia. The coronary arteries are not properly visualized by echocardiography; therefore, the focus is in imaging the myocardium. Classic findings in ACSs include regional wall motion abnormalities (WMAs; hypo- or akinesis) with impaired thickening of the affected regional myocardium. More recently, the use of ultrasound-enhancing agents (echo contrast) for myocardial perfusion imaging has also allowed the detection of ischemic myocardium in resting echocardiograms. Because coronary artery disease affects the myocardium in a regional manner, the distribution of such abnormalities respects the coronary territories. It should be noted, however, that coronary distribution varies on an individual basis and should only be used as a guide.
Although musculoskeletal pain is the most frequent cause of chest pain upon presentation to the ED, detecting ACSs is of critical importance because adequate anti-ischemic therapies (including revascularization) must be implemented in a timely manner. The presence of ST-segment elevation on an ECG should trigger immediate catheterization and percutaneous coronary intervention; therefore, an echocardiogram should not delay this intervention and must be postponed until the procedure is finished. However, in cases of suspected ACS without ST elevation, an echocardiogram in the ED could be of enormous value in detecting myocardial infarction (MI) and predicting cardiac events. Although cardiac biomarkers, particularly troponin and myoglobin, are extremely sensitive in detecting MI, the results of these tests may remain negative for a few hours after chest pain onset. Echocardiographic findings (regional WMA or thickening abnormality) of myocardial ischemia, on the other hand, are detected in almost 90% of patients scanned during or immediately after chest pain. A combined approach using troponin and echocardiogram has high accuracy in detecting ACS without ST elevation, with sensitivity and specificity greater than 90%. ,
Patients with chest pain and left bundle branch block represent a particular challenge in that the abnormal ECG could be masking ST elevation. Although historically this has been an indication for emergent catheterization, the concept has been challenged, and the use of biomarkers and bedside echocardiogram is being advocated to identify acute infarction: evidence of a hypokinetic or akinetic segmental WMA (lack of normal myocardial thickening in addition to myocardial excursion) in the anterior wall in the absence of evidence of a prior infarction (wall thinning, chamber dilatation) should trigger an emergent catheterization. ,
The utility of contrast echocardiography in the ED to evaluate for myocardial perfusion defects has been validated in several studies and reviewed in the recent ASE guidelines. , In the setting of ischemia, typical findings are poor contrast uptake in the subendocardial myocardium ( Fig. 42.1 ). The addition of myocardial contrast echocardiography to regional function increased the diagnostic and prognostic value of patients with chest pain and no ST elevation in the ED and proved to be a cost-effective intervention by facilitating early discharge of those with normal perfusion. Despite their promising potential, contrast agents for myocardial perfusion imaging have not yet been approved by the US Food and Drug Administration.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here