Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acetabular impaction grafting allows restoration of bone stock and normal hip biomechanics.
Acetabular impaction grafting is particularly successful as a technique for the reconstruction of cavitary defects.
It is a technically exacting procedure; attention to surgical detail is required for successful results.
The creation of a stable, contained acetabular defect is essential to its success.
Secure fixation of mesh using appropriately placed screws is critical for its use in segmental acetabular defects.
It requires vigorous, forceful impaction with specially designed instruments to achieve a stable base for cup cementation.
The histologic incorporation of impacted morselized cancellous allograft has been proven and is superior to that of bulk allograft.
The treatment of large peripheral segmental defects may be optimized with alternative techniques to impaction grafting.
Loss of acetabular bone stock is a major challenge in revision hip surgery. The facility to restore bone stock and thereby re-create normal hip joint biomechanics is an attractive solution. This can be achieved with impaction grafting of the acetabulum, which is an established technique and should be an essential tool in the armamentarium of the modern revision hip surgeon when other simpler techniques are not adequate.
Use of large amounts of cement in isolation for the reconstruction of loose acetabular components has been well described, with Sotelo-Garza and Charnley concluding that there was no difference in the outcome of primary cemented hip replacement in protrusio acetabuli whether or not bone graft was used. However, the results of this technique in the revision setting are generally poor, with Amstutz et al. reporting 83% radiographic loosening at only 2 years postoperatively. The review by Callaghan et al. of 146 cemented revisions revealed a 34% rate of radiologic loosening or mechanical failure at 3.6 years. Similar results from the Mayo Clinic review of 166 revisions with cement at a mean of 4.5 years revealed probable or possible acetabular loosening in 37.7% of hips and complete radiolucent lines in 70.9% of cases. Following removal of loose acetabular components, the acetabular interface is often found to be sclerotic, particularly following removal of a cemented socket. In these circumstances, it is not possible to gain adequate osteointegration of the cement at revision, and early loosening is common. Therefore, the reconstruction of acetabular defects solely with cement has largely been abandoned. However, impaction bone grafting re-creates an ideal surface for cement integration and has the ability to incorporate, thus restoring bone stock in the longer term and re-creating normal anatomy.
The use of bone graft has its origins in the early days of modern surgery. In 1859, Ollier was credited with describing the first clinical experiment of bone grafting when he attempted to transplant the radius from a rabbit into a tibial nonunion. Subsequent work by Macewen and Ponset on the use of allograft from amputated limbs led to increased interest in the subject. However, the clinical use of bone grafting was hampered by the limited availability of autograft and the inability to store allograft properly. It was the development of bone banks and of methods of freezing allograft at the Hospital for Special Surgery in New York in the late 1940s that secured the future of bone grafting in reconstructive orthopedic surgery. In the 1970s, the first reports on the use of bone graft to treat acetabular deficiencies began to appear. In 1975, Hastings and Parker suggested the use of medial bone graft with a Vitallium mesh, in combination with a cemented acetabular component, for the treatment of primary acetabular protrusio. Further reports by Heywood, McCollum, and Harris confirmed the success of bone graft in acetabular reconstruction.
The development of cementless techniques for implant fixation has offered an alternative method of acetabular reconstruction. Good results have been reported, both with and without bone graft. Most acetabular revisions are performed using these types of implants, particularly in cases in which a defect is segmental and cannot be contained using reinforcement mesh. In our opinion, the successful use of bone graft in large defects and its incorporation relies on adequate loading of the impacted graft, which can be achieved reliably only with a cemented socket. The use of an uncemented acetabular component relies on contact with host bone; loading will occur preferentially at these points of contact. The use of cemented components allows circumferential use of bone graft, in which the cement is in contact with impacted graft over 100% of its interface. This allows restoration of bone stock in all areas of the acetabulum—something that is precluded by the necessity for host bone contact with cementless shells.
In the field of revision hip arthroplasty, the modern techniques of impacting morselized graft to re-create anatomy and to restore bone in the femur and acetabulum have been popularized by the surgeons in Nijmegen on the acetabular side and later on the femoral side by the surgeons in Exeter. Essential to the technique is the creation of a contained defect, be it on the acetabular side, as in this chapter, or on the femoral side, as in Chapter 100 . This in itself can be technically challenging and may require the use of metal reinforcement mesh or porous metal wedges. Once the acetabular defect has been contained, morselized autograft or allograft is impacted within the cavity to form a stable base before cementation of a polyethylene acetabular component.
This chapter describes the indications, technique, and limitations of impaction bone grafting, in combination with a cemented acetabular component, in the reconstruction of acetabular defects.
There are three main reasons for the loss of acetabular bone stock in revision hip arthroplasty: (1) aseptic loosening due to osteolysis, (2) bone loss due to infection, and (3) iatrogenic loss during implant removal.
The main indication for revision of the acetabular component is painful socket loosening. There are notable differences in the patterns of bone loss that occur around cemented and uncemented components, specifically in their tendencies to migrate or cause extensive osteolysis.
There is no doubt that the survival of a cemented acetabular component is dependent on the quality of the original operation. Previously well-fixed, cemented acetabular components may loosen because of excessive mechanical loading over time, osteolysis caused by particulate debris, or by infection. Loosening of cemented sockets has been defined as the development of lucent lines of between 1 mm and 2 mm at the bone-cement interface, or as progressive migration. Once a cemented socket becomes radiologically loose, it will start to migrate and it will often, although not always, become symptomatic, alerting the surgeon to the need for revision surgery.
Periprosthetic bone loss around uncemented components is often classed as silent. Gross suggests that an uncemented shell with at least 50% coverage requires no additional support. A well-supported socket that loses bony support because of osteolysis may need only 50% bony adherence, possibly even less, to remain well fixed and therefore asymptomatic, despite significant loss of bone stock around the component. Regular long-term follow-up of these patients is essential to avoid late presentation with catastrophic bone loss. Hartofilakidis et al. conducted a comparison review of cemented and uncemented acetabular shells and concluded that the lysis around cemented sockets was linear. However, the lysis around uncemented shells was more aggressive and expansile. The advent of highly cross-linked polyethylene has improved the results of uncemented acetabular components and massive osteolysis seems to be much less prevalent with its use. Registry data shows that implants inserted with highly cross-linked polyethylene have a clear advantage in survival over those with regular polyethylene, particularly with the increasing use of larger-diameter femoral heads.
Acetabular impaction grafting is also indicated in primary procedures for conditions in which there is loss of host bone, such as protrusio acetabuli, acetabular dysplasia, and trauma.
The only absolute contraindications to impaction grafting are the following:
Inability to contain a segmental defect, medial or peripheral, as defined by D'Antonio et al.
The presence of active infection, unless it has been adequately controlled with a thorough debridement, as in careful one-stage or two-stage exchange arthroplasty for periprosthetic joint infection
Although large defects can be successfully contained, it is the stability and durability of that containment that are essential to the success of impaction grafting. It can be impossible to contain significant defects of the anterior and posterior columns with enough stability to allow effective impaction grafting; other techniques for reconstruction should be considered in these circumstances. Similarly, large superolateral defects extending down the anterior and posterior columns are difficult to contain with a mesh; cementless implants may be required in these cases.
Acetabular impaction grafting should not be undertaken in the presence of active infection, but this does not preclude its use in the revision of patients with periprosthetic joint infection. The technique can be safely employed at the second stage of a two-stage approach to the treatment of infection. Because of the bone loss that often occurs as a result of infection, its ability to restore bone stock makes it a uniquely useful technique. Its safe use in single-stage revision for infection has also been described. Rudelli et al. reported a 6.2% recurrence of infection at 8.6 years in 32 patients who underwent one-stage revision of infected, loose total hip replacements. Of these patients, 25 underwent impaction grafting of both the femur and the acetabulum; half required the use of mesh to contain the graft. These results are similar to those reported using a two-stage procedure. A one-stage exchange arthroplasty may be viewed as two stages in one operation, whereby the infection is controlled with an initial implant removal, debridement, and irrigation. The reimplantation is done after appropriate re-draping and exchange of all instruments to ones that were not used at the time of the debridement.
A major part of planning any surgery is predicting which pieces of equipment are likely to be required. With particular reference to impaction grafting of the acetabulum, the following items should be available in the operating room:
Fresh-frozen femoral heads: two to three for an average defect
Concave femoral head reamers
Rongeurs for creating bone chips. Alternatively, a bone mill capable of producing large bone chips may be used but with potential drawbacks (see later discussion).
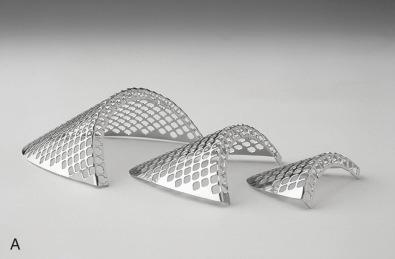
Selection of rim and medial meshes ( Fig. 94.1 ).
3.5-mm small fragment screw set
Specialized acetabular impactors in a selection of sizes ( Fig. 94.2 )

A lateral position is preferred, ensuring that the pelvis is adequately secured with appropriately placed padded positioners. It is important to align the anterior superior iliac spines in the vertical plane to ensure that the position of the pelvis is known and well controlled throughout the procedures, as anatomic landmarks for ensuring correct anteversion and abduction of the implanted cup are typically missing. This, in combination with an assessment of the transverse acetabular ligament if still present or visible, helps with orientation of the new acetabular component.
Perioperative antibiotics should be administered. Multiple tissue samples may be sent for culture at the surgeon's discretion and, where infection is suspected, frozen section may be requested as well. The frozen femoral heads are removed from the freezer and are allowed to defrost in sterile, warmed saline while the exposure continues.
An extensile posterior approach generally gives excellent exposure of the acetabulum and the posterior wall and column, should plating be necessary. The proximal femur is mobilized; sufficient soft tissue is released, and thickened scar tissue is removed to allow safe dislocation of the hip. The short rotators and posterior capsule are retained for later closure to enhance posterior stability postoperatively. The sciatic nerve needs to be identified, protected, and possibly mobilized if work on the posterior wall or ischium is required, as in the case of posterior column plating.
Retention of the femoral component can limit visualization and hamper acetabular reconstruction, but the authors’ strategy regarding the femoral component depends on its method and state of fixation. Clearly, a loose femoral component should be revised using the surgeon's preferred technique for the femoral conditions that exist at the time of revision. However, well-fixed stems do not necessarily require full revision, be they cemented or cementless; revision of a well-fixed stem or cement mantle may cause unnecessary damage to the femur. For a soundly fixed cemented stem and cement mantle, it is relatively easy to bur away cement over the shoulder of the prosthesis and tap the femoral component from its intact cement mantle. After acetabular reconstruction is complete, a new femoral component can be recemented into the old mantle—the cement-in-cement technique. If a cementless femoral component is to be retained and the anterior acetabular wall is intact, then a pocket can be made in the anterosuperior tissues to accommodate the femoral head or trunnion. However, it is often difficult to create a space large enough for the proximal femur, and it is important to avoid imparting excessive force on the anterior wall during exposure of the socket. An alternative approach for well-fixed uncemented stems is use of the trochanteric slide, through which the abductors are safely separated from the femur, thereby allowing circumferential exposure of the acetabulum. Alternatively, if it is necessary to remove a well-fixed uncemented femoral component, an extended trochanteric osteotomy can be used, which also gives excellent exposure of the whole acetabulum.
Whichever approach is used, retractors are placed anteriorly and posteroinferiorly, with care taken to protect the thin walls of the acetabulum and the sciatic nerve. It is important to identify the transverse ligament, if still present, which helps with orientation of the acetabular component and acts as a guide to the level of socket placement. If it is present, the transverse ligament is retained because, apart from its role as a guide to socket placement, it also helps constrain the bone graft during the impaction process. If the transverse ligament is absent, the teardrop is identified as a guide to the inferior margin of the acetabulum.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here