Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Flat plate is a historical term that refers to a past method of radiography when radiographs were recorded on flat plates of glass coated with an emulsion sensitive to x-rays. This examination also has been termed a plain abdominal radiograph, plain film of the abdomen, abdominal plain film, and KUB. KUB refers to the kidney, ureters, and bladder; this term is not preferred because the ureters are not visible on the plain radiograph, and other organs are visible. The term plain film of the abdomen is not accurate if the image is recorded either on a phosphor plate or directly by electronic means, stored electronically, and displayed on a monitor or plasma screen. No “film” is involved. The preferred terms are plain radiograph of the abdomen or plain abdominal radiograph .
Structures are visible on a plain radiograph as a result of differential attenuation of the x-ray beam by air, fat, soft tissue, calcium, and various metals. The edge of an organ composed of soft tissue is visible only where it interfaces with fat of the retroperitoneum or mesenteries, gas within the lumen of the adjacent bowel, or gas within the intraperitoneal or retroperitoneal spaces ( Figure 23-1 ). Interfaces are best shown when the x-ray beam is tangential to the interface. Calcium density is detected in bones or abnormal calcifications, such as gallstones or kidney stones, or within vessel lumens or vascular walls.

The inferior edge of the liver may be visible. The soft tissue of the spleen may be outlined by air in the stomach and gas in the splenic flexure of the colon. The kidneys and lateral border of the psoas muscles are outlined by retroperitoneal fat. A moderately distended urinary bladder may be outlined by pelvic fat. Portions of the uterus may also be outlined by pelvic fat.
The stomach is defined by its rugal folds. Air and fluid in a nondistended stomach is a normal finding. The duodenal bulb may be shown by air. Small bowel is identified by its thin, transverse folds (valvulae conniventes). The large bowel is defined by its haustral sacculations ( Figure 23-2 ). A small amount of gas may be present in nondistended small bowel. Gas may outline the nondependent portions of the large bowel, in particular, the transverse colon. Although the lung bases and posterior costophrenic angles are usually underexposed during chest radiography, they are well shown on plain abdominal radiographs.
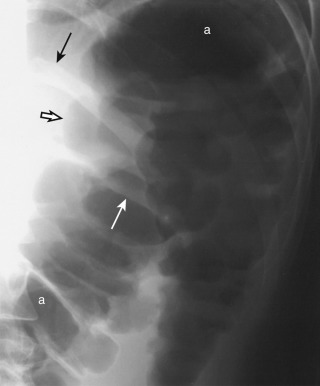
The standard plain abdominal radiograph is obtained with the patient in a recumbent position, lying on his or her back, and is termed a supine radiograph (see Figure 23-1, A ). The x-ray tube is anterior (superior) to the patient, and the radiographic image capture device is posterior (inferior) to the patient. The x-ray beam travels from anterior to the patient to be captured posterior to the patient. By convention, this is termed an anteroposterior radiograph .
The term decubitus means lying down. Without qualification, the term decubitus radiograph is meaningless. A “decub” is obtained with the patient lying with his or her left or right side down. A right lateral decubitus radiograph is an image obtained with the patient lying with his or her right side down, the x-ray tube oriented in a horizontal position on one side of the patient, and the image capture device (usually a “cassette”) oriented perpendicular (upright) to the tube on the other side of the patient. To prevent any confusion, the best terms are right-side-down decubitus and left-side-down decubitus views, referring to the position of the patient.
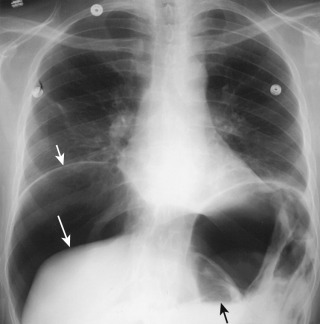
Images obtained with the patient in an erect position (chest or abdominal image) or images obtained with the patient in a lateral decubitus position are used to show air-fluid levels in the gastrointestinal (GI) tract or free intraperitoneal gas ( Figure 23-3 ). These views are important in patients with suspected perforation or bowel obstruction. An erect view is used in patients who can stand; lateral decubitus views are performed in patients who are unable to stand.
Acute or subacute abdominal pain.
Suspected calculus in any viscus.
Suspected bowel obstruction or adynamic ileus.
Suspected perforation of a viscus.
Abdominal trauma.
Abdominal distention.
Determination of presence and location of a tube, catheter, intravascular device, or potential radiopaque foreign body.
A plain abdominal radiograph is a low-cost procedure that is easy to perform with inexpensive radiographic equipment. A radiograph requires little cooperation from the patient. The radiation dose is small. A CT scan is a high-cost procedure that also requires little cooperation from the patient. CT equipment is expensive and delivers a higher radiation dose to the patient. Given the rapid speed of new CT scanners, the time that a patient is lying on the scanner tabletop is nearly equal for a plain radiograph of the abdomen and a CT scan. A plain abdominal radiograph requires no patient preparation. There is about a 1-hour preparation time for a CT scan that uses intravenous (IV) and oral contrast agents.
CT has far greater contrast resolution than a plain abdominal radiograph and is far superior in showing abnormal calcifications or fluid/gas patterns in the viscera or peritoneal space. CT is tremendously superior for assessment of the solid organs. A plain radiograph has better spatial resolution than CT, in particular, the overview scout image of a CT scan (variously termed scanogram or topogram ). A plain abdominal radiograph provides an overall “big picture” for bowel obstruction superior to a CT scan. This advantage is greatly surpassed, however, by the ability of CT to demonstrate individual bowel loops, fluid-filled bowel loops, bowel wall thickness, and intravenous contrast enhancement patterns.
Plain abdominal radiographs are helpful when patients require serial studies, such as patients undergoing decompression for small bowel obstruction or follow-up for resolution of postoperative adynamic ileus. Plain radiographs are also helpful in determining positions of various tubes placed in the abdomen. If there is any question, however, that a tube tip is not within its expected location, a contrast study is performed.
Plain radiographs may be valuable in patients in the intensive care unit (ICU) who are too seriously ill to move. The physicians have to balance the risk of patient transport from the ICU to the CT scanner to obtain greater information obtained by a CT scan with the mediocre diagnostic capability but high safety level of a plain abdominal radiograph obtained with portable radiographic equipment. In situations that require extreme speed, a CT scan without the use of either oral or intravenous contrast material still provides much more information than a plain abdominal radiograph.
Gas in the stomach is initially similar in composition to atmospheric air swallowed by the patient. When various digestive processes occur, the gas in the small or large bowel no longer has the same composition as atmospheric air. Carbon dioxide is generated when acid secreted by the stomach combines with bicarbonate secreted by the pancreas. Oxygen and carbon dioxide are resorbed in the small bowel. Nitrogen is not absorbed. Colonic gas is also composed of gases such as methane and hydrogen sulfide, produced by bacterial fermentation.
Gas in the peritoneal cavity ascends to a nondependent position under the anterior abdominal wall with the patient in a supine position and underneath the diaphragm with the patient in an erect position. Intraperitoneal gas is also trapped in various crevices of the organs and mesenteries. A patient should generally be positioned in an erect or lateral decubitus position for about 5 minutes before a radiograph is obtained to look for “free intraperitoneal gas.”
Free intraperitoneal gas is best shown on an erect chest x-ray centered over the diaphragm (see Figure 23-3 ); 1 mL of gas may be detected under the curve of a hemidiaphragm. A left-side-down lateral decubitus view to show gas above or under the liver edge is the second best choice.
In some patients, an erect chest, erect abdominal, or lateral decubitus radiograph is impossible, and an image can be obtained only with the patient in a supine position. A supine abdominal radiograph shows free intraperitoneal gas in about 60% of patients with free intraperitoneal gas.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here