Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Overview: Injuries and disorders of the foot can impose considerable dysfunction in an athlete. Although most foot problems will improve with appropriate care, a clear understanding of normal anatomy and physical examination findings is vital to recognize injuries and abnormal processes to prevent worsening and long-term damage.
Bones: Normal bony architecture includes 28 bones (7 tarsals, 5 metatarsals, 14 phalanges, and 2 hallux sesamoids) ( Fig. 60.1A ).
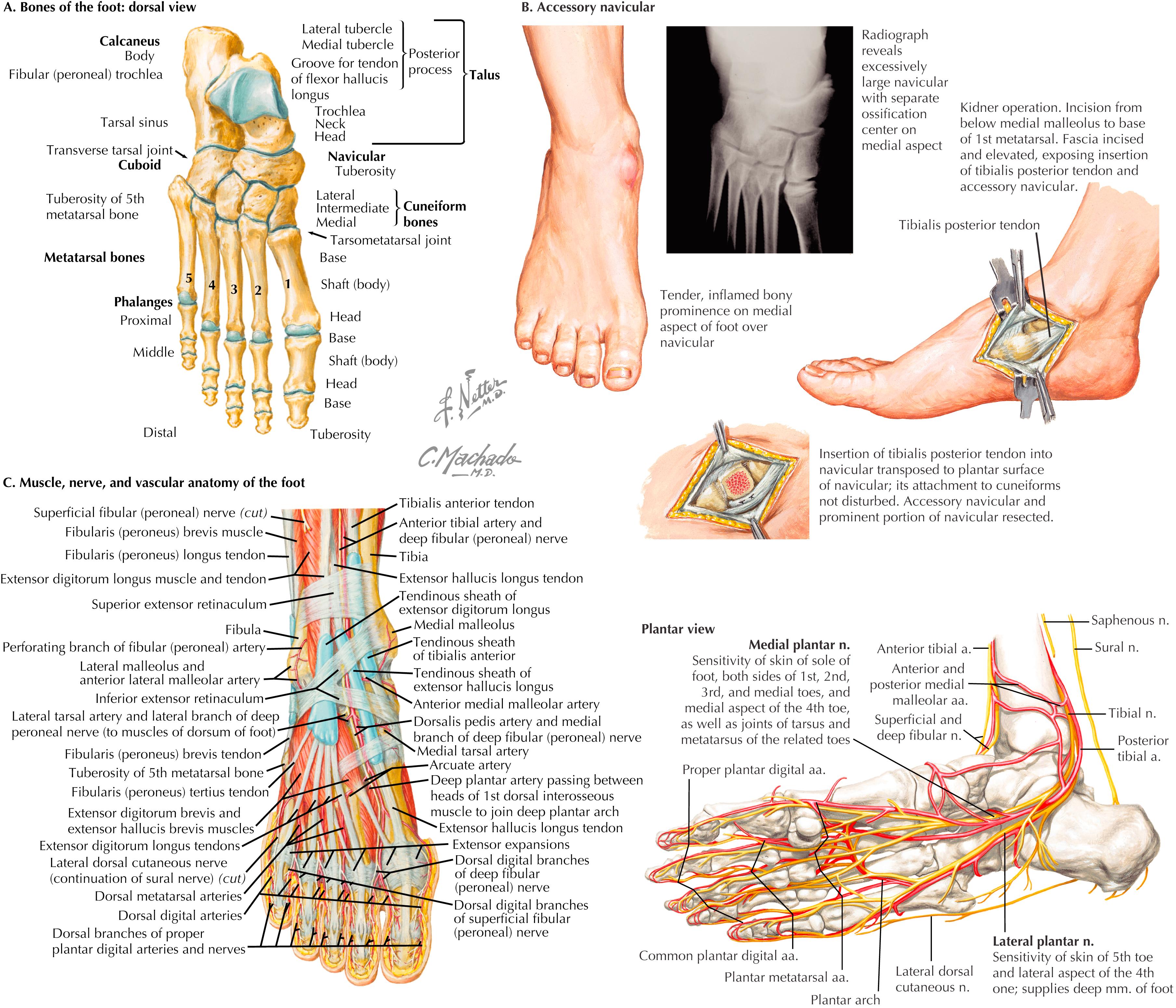
Accessory bones: Common accessory bones that can create symptoms in athletes are the accessory navicular (see Fig. 60.1B ), os trigonum, os peroneum, and os vesiculanum.
Muscular anatomy: Most lower leg extrinsic muscles have tendinous attachments on the foot. Foot intrinsic muscles are important for normal function (see Fig. 60.1C ).
Neurovascular structures: Three primary arteries/veins provide blood supply and five primary nerves provide innervation to the foot (see Fig. 60.1C ).
Overview: Most foot injuries in athletes are caused by acute or repetitive trauma. Several intrinsic and extrinsic factors can increase the risk of injury.
Intrinsic factors: Foot posture, hindfoot alignment, joint laxity and stiffness, nutrition, fitness level, training regimen, biochemical deficiencies, age, and body mass index
Extrinsic factors: Coaching, technique, environmental factors, footwear and equipment, and safety hazards
Running and jumping sports: Increased risk of bone stress injuries, tendinopathies, and fasciopathies
Impact/collision sports: Increased risk of acute fractures, tendon ruptures, ligament tears, and joint injuries
Overview: An athlete’s recollection of injury onset, mechanism, and location is an important part of the diagnostic process.
Mechanism: Acute, chronic, or acute on chronic; position of the foot during injury; was a pop felt or heard?
Severity: Was the athlete able to ambulate on his or her own after the injury? Was there an obvious deformity, swelling, or discoloration?
Location: Ask the athlete to indicate “with one finger” the location of the injury, pain, or symptoms.
Previous injury: Has the athlete experienced a similar injury in the past? Tendinopathies can flare up or rupture, or bone stress injury can lead to fracture.
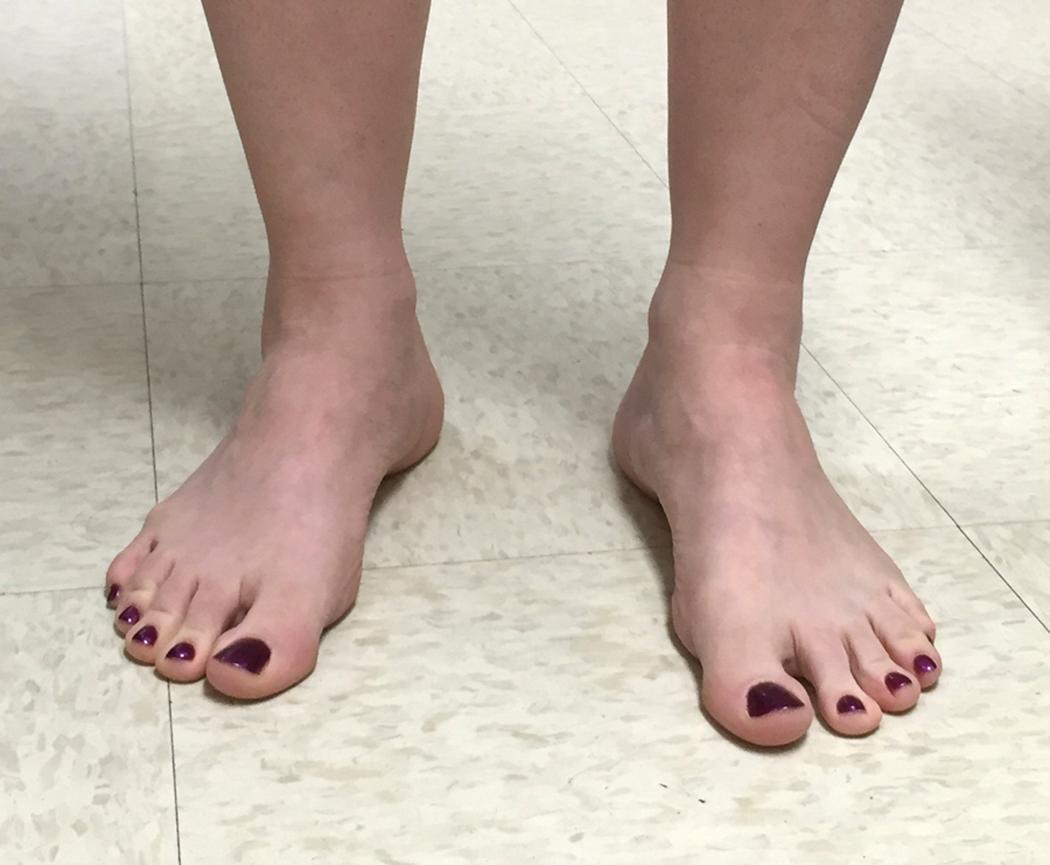
Alignment of the lower extremities: View the patient from the front and back. Check for limb length inequality, pelvic tilt, genu varum, genu valgum, flexion, extension, and rotational abnormalities of both lower extremities.
Foot alignment and mechanics: Evaluate the medial longitudinal arch for pes planus, pes planovalgus, pes cavus, forefoot abduction, and forefoot varus ( Fig. 60.2A ). Check single- and double-leg heel rise to confirm that the heels invert and arches increase. Evaluate the forefoot for hallux valgus (or varus) and pronation; toe crossover, cock-up, hammering, or clawing of lesser toes (see Fig. 60.2B ); and metatarsus adductus.
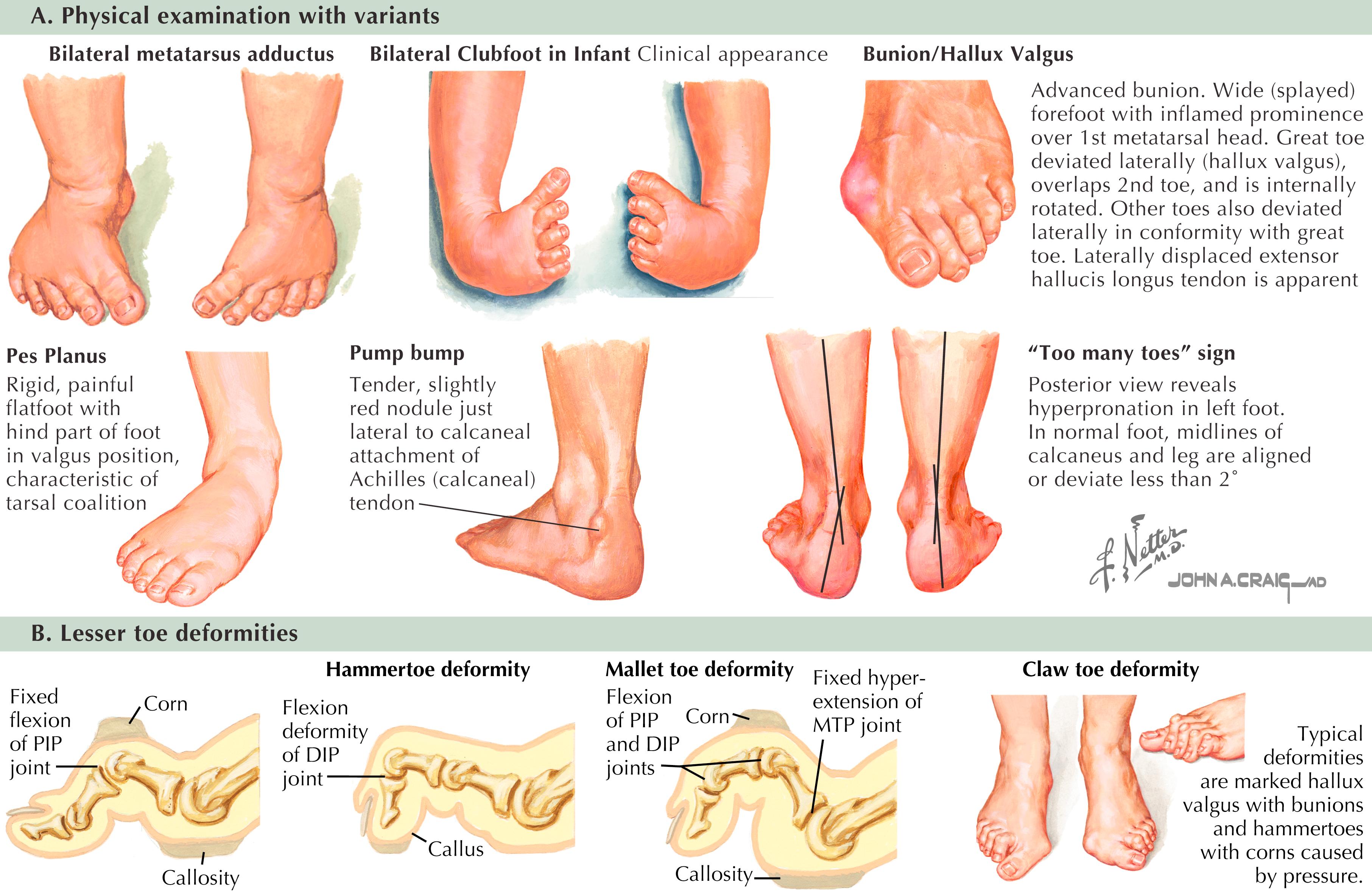
Inspect ambulation: Assess all phases of gait for asymmetric movement on either side of the body, degree of toeing in or out, inversion of the heel, and supination of the foot. Observe the medial longitudinal arch during the stance phase. Assess for antalgic, neuropathic (e.g., steppage), and myopathic (e.g., Trendelenburg) gait and symmetric strength during push-off.
Visible abnormalities: Note varicosities, erythema, ecchymosis, edema, and muscle wasting.
Vascular: Palpate posterior tibial and dorsalis pedis pulses. Assess capillary refill time. Absence of hair distally may indicate peripheral vascular disease.
Skin: Note the location of callus formation, scars, wounds, blisters, ulcerations, and discoloration. Visualize toenails and nail beds.
Range of motion: Check active and passive ankle, subtalar, and transverse tarsal and first metatarsophalangeal joint (MTPJ) motion; compare them with the uninjured side. Notable crepitus during range-of-motion examination can indicate degenerative changes, fracture, or tissue thickening.
Strength testing: Test muscle groups against resistance—dorsiflexion, plantarflexion, inversion, and eversion; compare with the contralateral side.
Bones: Fifth metatarsal base, peroneal tubercle, first tarsometatarsal joint, navicular tuberosity, head of talus, sustentaculum tali, lateral malleolus, medial malleolus, and metatarsal heads (see Fig. 60.1A )
Ligament attachments: Calcaneofibular ligament, anterior talofibular ligament, superficial deltoid ligament, spring ligament, and plantar fascia (see Fig. 60.1C )
Tendons: Posterior tibialis, flexor hallucis longus (FHL), anterior tibialis, peroneal brevis and longus, extensor hallucis longus, and Achilles (see Fig. 60.1C )
Bursae: Calcaneal, retrocalcaneal
Thompson test: Patient prone with affected leg extended; squeeze calf muscles to indirectly plantarflex the foot; failure of the foot to plantarflex (a positive test)
Abduction stress test: Manual abduction of the forefoot while stabilizing the hindfoot; assess for pain clinically and widening of Lisfranc joint on radiographs
Calcaneal compression text: Squeeze the posterior heel simultaneously from medial and lateral sides. Pain is a positive test and suggests stress fracture.
Too many toes sign: View the patient from behind; three or more toes visible lateral to the heel suggests forefoot abduction, often seen with posterior tibial tendon or spring ligament dysfunction (see Fig. 60.2A )
Peek-a-boo heel sign: Viewed from the front, indicates hindfoot varus alignment ( Fig. 60.3 )
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here