Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Causes of primary neonatal corneal opacification include congenital hereditary endothelial dystrophy (CHED), posterior polymorphous corneal dystrophy, congenital hereditary stromal dystrophy (CHED), and corneal dermoid. Secondary causes include trauma (e.g., forceps), infection, metabolic disorders, and congenital glaucoma. Corneal opacification requires further workup to diagnose the underlying cause and to help plan any surgical intervention.
Primary megalocornea is defined as a horizontal corneal diameter of >12 mm at birth or >13 mm by 2 years of age in the absence of elevated eye pressure. Congenital glaucoma must be ruled out; isolated cases do not usually require intervention. Microcornea is defined as a clear cornea of normal thickness with a horizontal corneal diameter of <9 mm in newborns and <10 mm after 2 years of age. It is commonly associated with other ocular and/or systemic findings.
Developmental anomalies of the iris include diffuse underdevelopment (congenital aniridia, including its association with Wilms tumor), focal developmental defects (coloboma), failed involution of the central iris (prepupillary membrane), iris cysts (and their association with thoracic aortic aneurysm), bilateral hypopigmentation (e.g., albinism), asymmetric pigmentation (heterochromia, e.g., Waardenburg syndrome, congenital Horner syndrome), iris atrophy (e.g., Axenfeld-Rieger anomaly), and displaced pupil (corectopia) with or without lens displacement (ectopia lentis), both of which can occur in isolation or in association with systemic causes such as neonatal Marfan syndrome.
Primary congenital corneal opacifications include congenital hereditary endothelial dystrophy (CHED), posterior polymorphous corneal dystrophy, congenital hereditary stromal dystrophy (CHSD), and corneal dermoids.
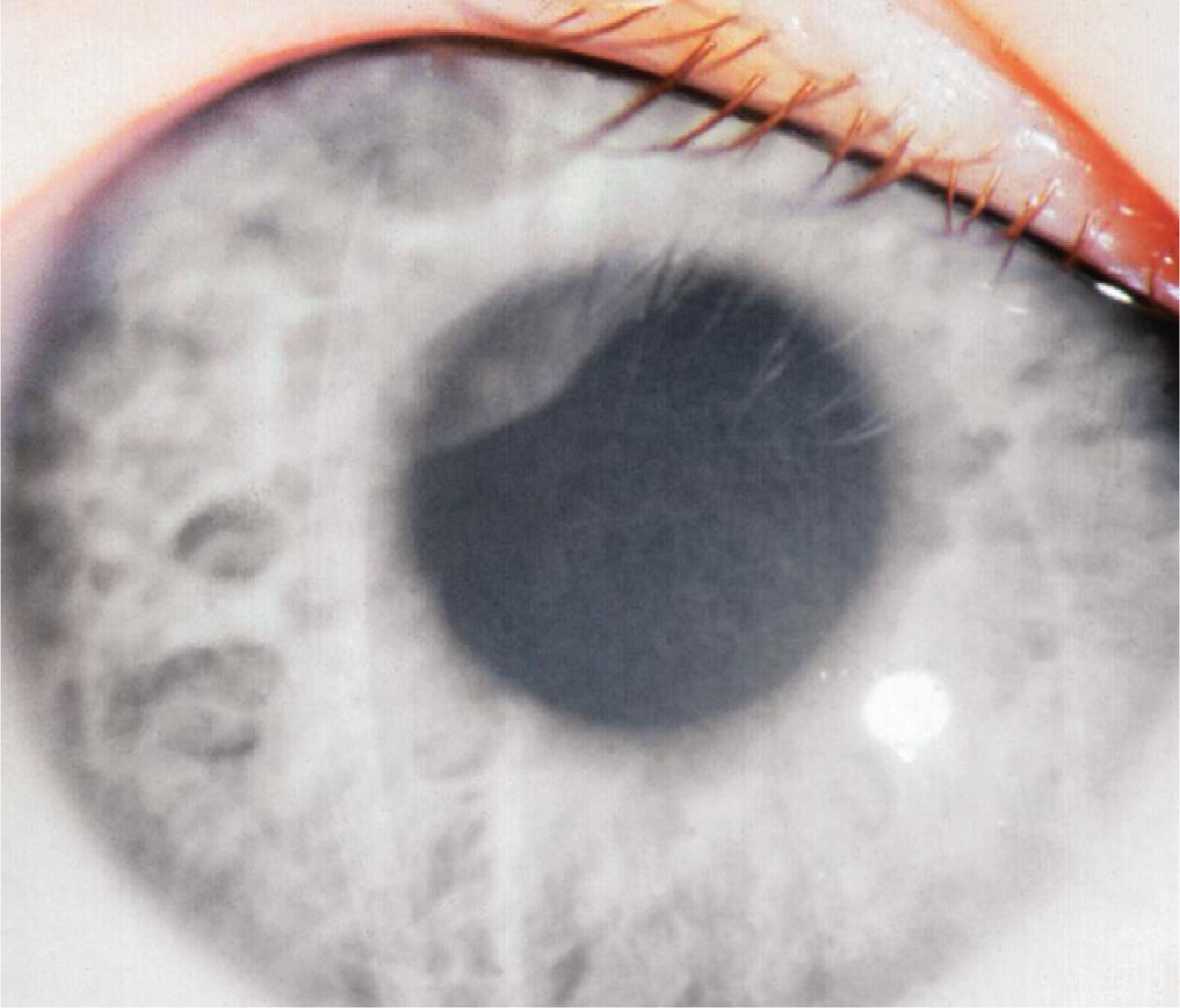
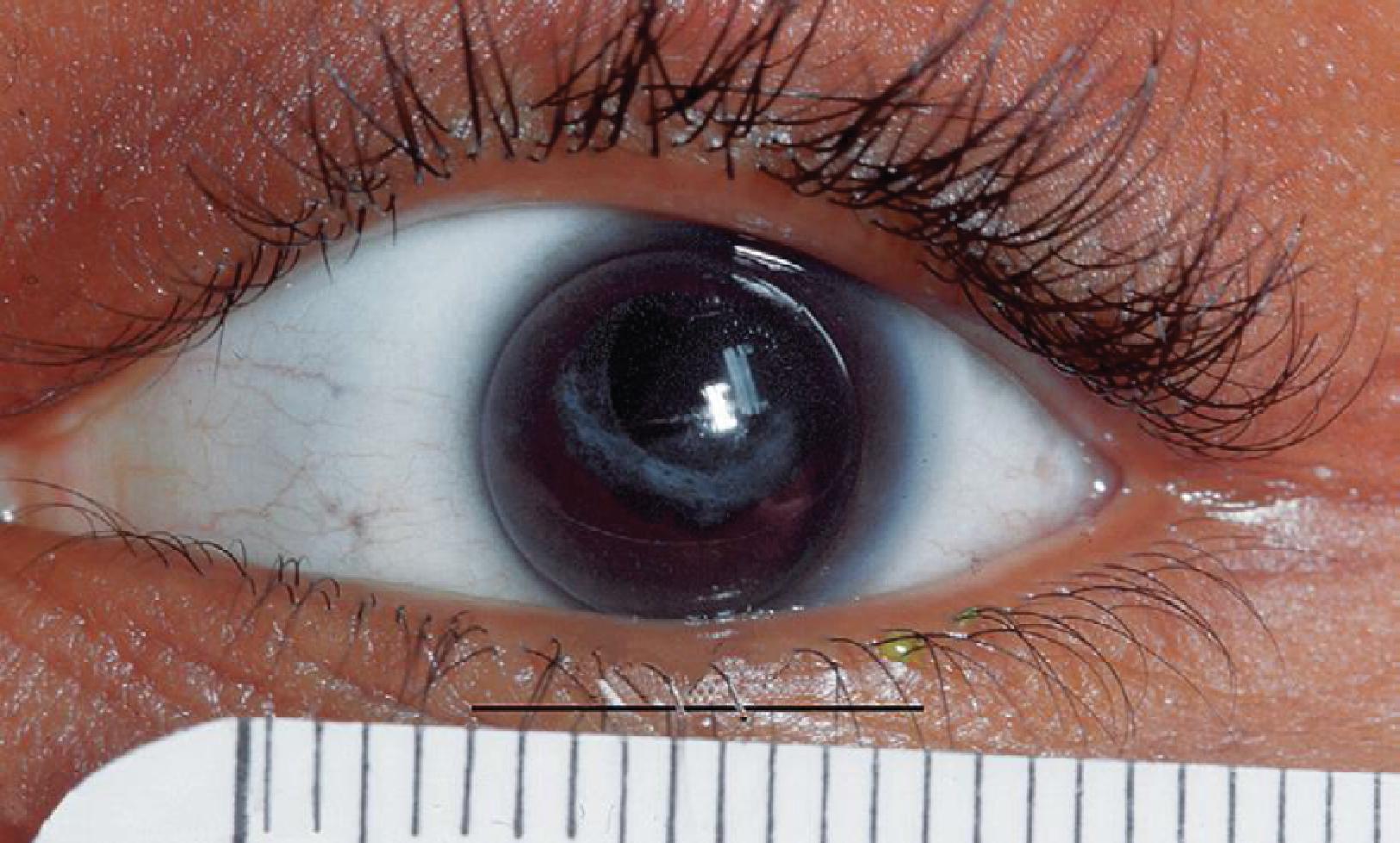
CHED manifests as bilateral, often symmetric, diffuse corneal cloudiness from edema ( Fig. 64.1 ). CHED1 (which is now known as CHED) usually presents with clear corneas at birth that tend to become progressively cloudier during the neonatal period, along with new-onset light sensitivity but no nystagmus. By contrast, CHED2 (which is now considered a neonatal variant of posterior polymorphous corneal dystrophy) usually presents with corneal cloudiness from birth that is nonprogressive and with nystagmus (due to lack of visual input from birth) but no light sensitivity. CHED may also be seen as part of Harboyan syndrome, which presents with CCO and sensorineural deafness.
CHSD presents with limbus-to-limbus corneal clouding and flake-like opacities in the corneal stroma but no corneal vascularization. Corneal dermoids are choristomas (normal cells in an abnormal location) and present as creamy nodular opacities that are classically located at the periphery of the cornea, where they can cause significant visual impairment from astigmatism. Sometimes they can obstruct the visual axis directly or cause ocular surface dryness and thinning (dellen) from tear film disruption.
Peters’ anomaly ( Fig. 64.2 ) and “sclerocornea” ( Fig. 64.3 ) have historically been used to describe certain types of CCO, although these terms are now discouraged due to their nonspecific nature. Because many prior reports utilize such terms, it is still important to note that Peters’ anomaly traditionally refers to abnormal adhesions between the cornea and iris (and is one form of anterior segment dysgenesis [ASD]). This impairs the ability of the inner layer of the cornea (endothelium) to successfully pump fluid out of the cornea in areas of adhesion, the process it uses to maintain clarity. As a result, Peters’ anomaly typically presents with cloudiness in part of the cornea from birth, which often slowly improves over a matter of months to years. Some cases also involve the lens and have congenital cataract. Peters’ plus syndrome includes additional systemic features such as short disproportionate stature, developmental delay, dysmorphic facial features, and cardiac, genitourinary, and central nervous system malformations.
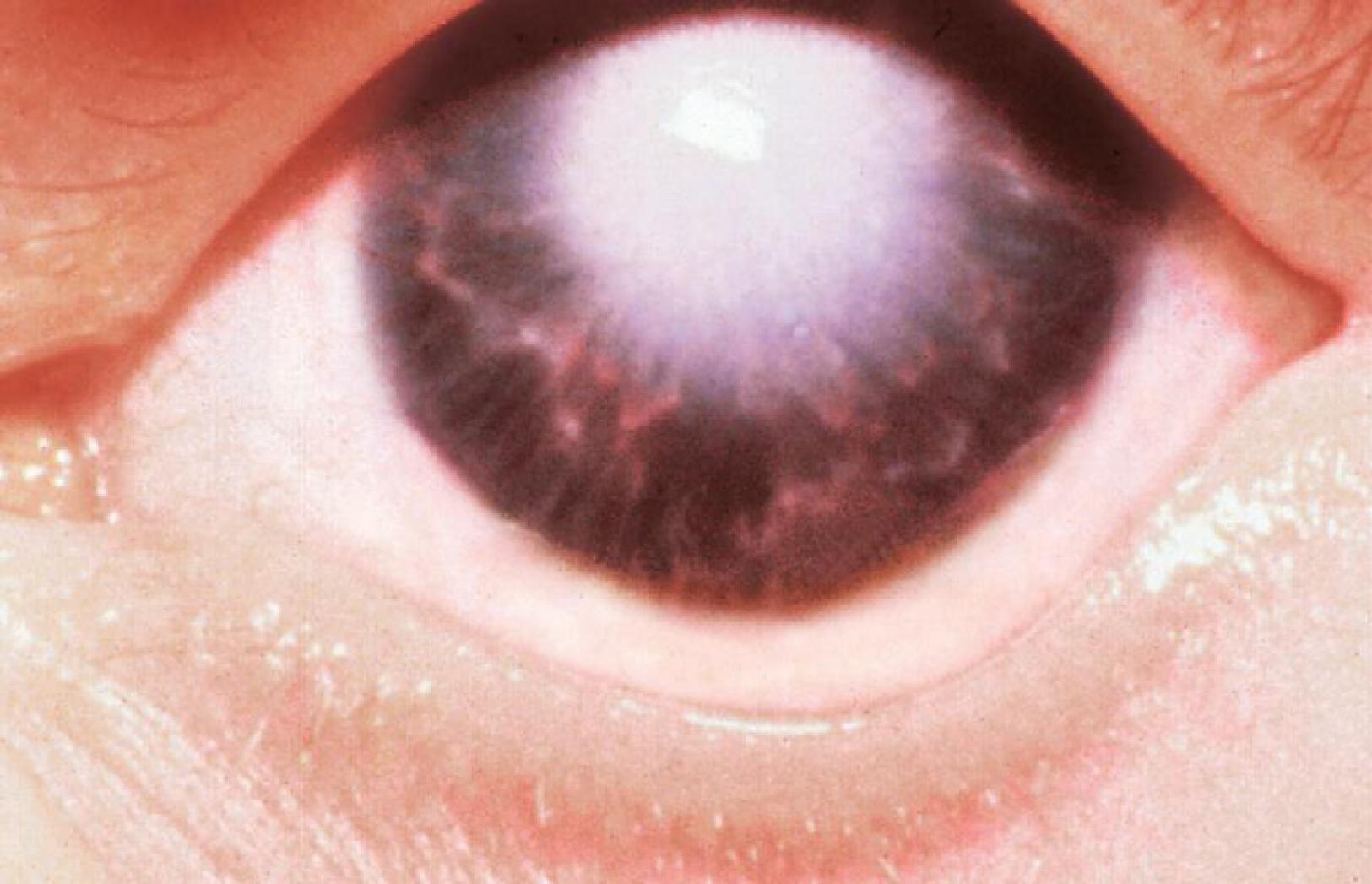

Sclerocornea describes a nonprogressive, noninflammatory ingrowth of opaque sclera extending into the peripheral cornea, causing an indistinct border between the two tissues. It can occur in isolation or along with other ASD syndromes such as Peters’ anomaly. It can be complete, where the whole cornea is opaque and flattened, or it can spare the central cornea and only affect the peripheral part.
Mucolipidosis IV is the only true metabolic cause of neonatal CCO. This rare metabolic storage disease is inherited in an autosomal recessive pattern and is associated with progressive psychomotor retardation.
Acquired corneal opacification that presents early in life includes trauma from accidental or nonaccidental causes. Forceps injury should be kept in mind because this is a well-recognized etiology of postnatal corneal opacification. It is almost always unilateral and is associated with fine streaks (breaks) in the inner cornea, which are only visible with magnification. Viral or bacterial infection may both present with corneal clouding in the neonatal period , but are often accompanied by other findings such as eyelid swelling, corneal ulcer, and/or muco-purulent discharge. Corneal clouding also occurs as part of primary congenital glaucoma (discussed in the glaucoma chapter).
CCO has a prevalence of 3 in 100,000 newborns, or 6 in 100,000 when congenital glaucoma is included. Many of the primary forms are inherited. CHED can be passed on in an autosomal dominant (CHED1) or autosomal recessive (CHED2) manner. , Primary dysfunction of the corneal endothelium increases permeability, causing hydration by aqueous humor and hence clouding. Harboyan syndrome is due to mutations in SLC4A11 . CHSD is caused by disruption of collagen organization due to mutations in DCN (which encodes decorin). , Peters’ anomaly can occur sporadically, but dominant and recessive forms have been reported. It can be caused by mutations in PAX6 , PITX2 , FOXC1 , CYP1B1 , MAF , or MYOC and is associated with trisomy 13. Peters’ plus syndrome is recessively inherited and can be caused by mutations in B3GALTL. , Causes of sclerocornea show significant overlap with other forms of ASD and include mutations in FOXE3 , RAX , SOX2 , PITX3 , PAX6, and PXDN. Mucolipidosis type IV is caused by mutations in MCOLN1 ; mucolipin-1 dysfunction impairs lipid and protein transport, causing their accumulation in lysosomes. Viral infection early in the neonatal period is often caused by herpes simplex. When accompanied by purulent discharge, Neisseria gonorrhea should be considered due to the high rate of progression and risk of perforation.
Diagnosing the cause of neonatal CCO based on clinical appearance alone is hard, because different entities present similarly. High eye pressure helps distinguish primary congenital glaucoma from other causes. Corneal thickness measurement by pachymetry helps distinguish CHED (increased due to edema) from CHSD (normal thickness). Imaging using ultrasound biomicroscopy (UBM) and anterior segment optical coherence tomography (AS-OCT) helps identify cornea-iris or cornea-lens adhesions suggestive of Peters’ anomaly and also aids in preoperative planning. Genetic testing can help identify underlying genetic etiologies. Corneal lesions suspicious for infectious causes must be scraped and sent for microbiologic testing.
Primary corneal diseases without significant ASD can undergo full thickness corneal transplant (penetrating keratoplasty [PKP]) and have fair outcomes, albeit not as good as adults. For disorders that only affect specific layers of the cornea (e.g., CHSD), selectively transplanting that layer (i.e., deep anterior lamellar keratoplasty [DALK]) may be an option. Corneal dermoids can be managed by PKP or DALK, depending on their size. , Corneal transplants are avoided in patients with active infection, but once the infection and associated inflammation have resolved, the residual scar can be replaced with a PKP or DALK. , Conjunctival transplantation may help corneal clouding due to mucolipidosis IV.
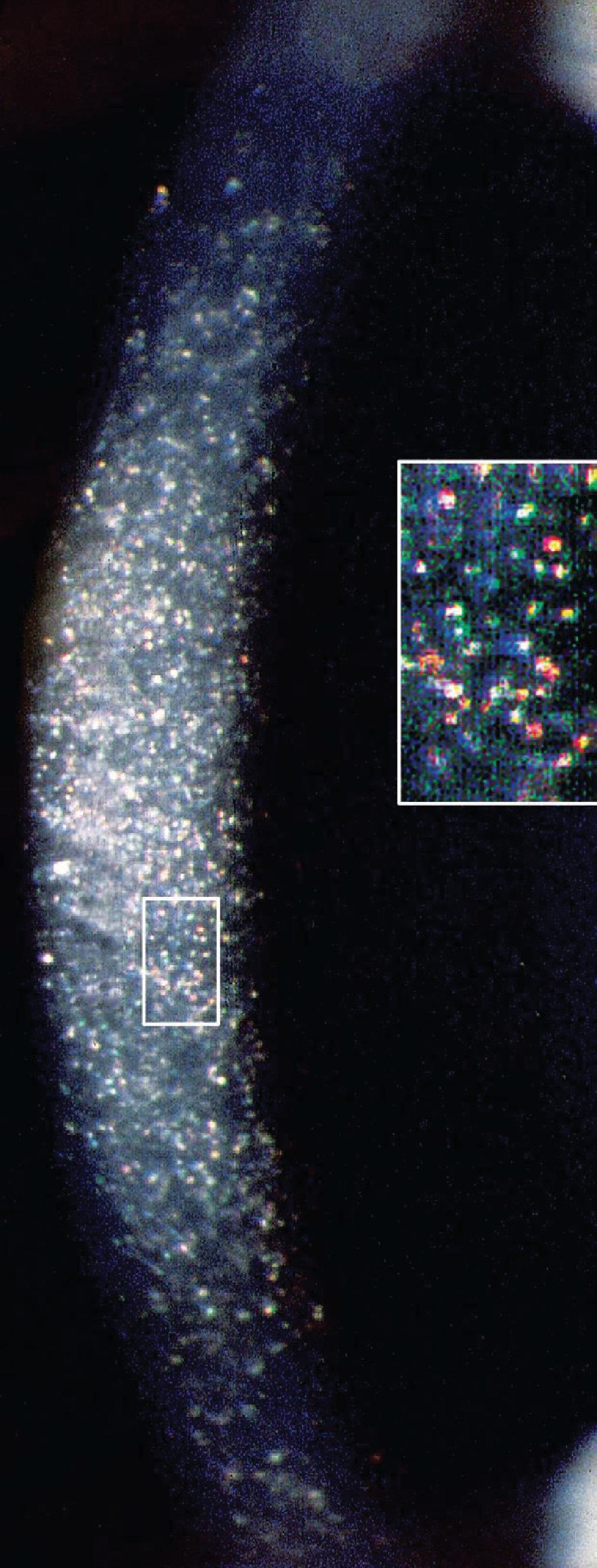
Examples of disorders with corneal crystal deposits include cystinosis and tyrosinemia type 2. Crystals appear as bifringent stromal opacities that may be visually significant. Patients can have light sensitivity due to light scattering by the crystals or redness and irritation from an uneven corneal surface. Fifty percent of infants with cystinosis present with light sensitivity. Tyrosinemia type 2 can also present with corneal epithelial defects that resemble herpes simplex dendrites (pseudodendrites).
Cystinosis occurs in 1 in 100,000 newborns. There is no gender or racial predilection. It is the most common cause of pediatric renal Fanconi syndrome and accounts for 5% of pediatric renal failure cases. It is divided into three types, including nephropathic, intermediate, and nonnephropathic (ocular) forms ( Fig. 64.4 ). The nephropathic form is the most common and severe form and develops in infancy; it presents with light sensitivity and renal failure. The nonnephropathic form only affects the cornea.
Tyrosinemia type 2 results from elevated blood tyrosine levels, and affects the eyes, skin, and intellectual development. Symptoms include eye pain, redness, excess tearing, and light sensitivity as well as painful skin lesions on the palms and soles (palmoplantar hyperkeratosis). Fifty percent of patients have intellectual disability.
Cystinosis is inherited in an autosomal recessive manner. All forms are caused by mutations in CTNS , which encodes lysosomal membrane protein cystinosin. Impaired cystinosin function results in lysosomal cysteine accumulation due to impaired export; the accumulated crystals damage affected tissues.
Tyrosinemia type 2 is inherited in an autosomal recessive manner. It is caused by mutations in the gene tyrosine aminotransferase (TAT) ; this results in impaired function of the enzyme tyrosine aminotransferase, one of the enzymes required for tyrosine breakdown. Impaired tyrosine aminotransferase function causes accumulation of tyrosine crystals in affected tissues.
White blood cell cysteine levels of 3 to 20 nmol half-cysteine/mg protein is diagnostic of cystinosis. Molecular testing for mutations in the gene Cystinosin, Lysosomal Cystine Transporter (CTNS) can be performed. AS-OCT shows hyperreflective and iridescent deposits involving the corneal epithelium and corneal stroma but typically sparing the inner corneal layers. , Tyrosinosis is confirmed by high urinary elimination of tyrosine and tyrosine derivatives and high serum tyrosine levels up to 52 mg/100 mL.
In cases where corneal deposition is nonprogressive, complaints of light sensitivity may decrease over time, so observation is reasonable. Oral cysteamine treatment depletes systemic cysteine levels and is used to improve renal function; of note, it does not help with corneal crystal deposits or eye symptoms due to the cornea being avascular. Cysteamine eye drops do help decrease corneal crystal density and associated symptoms, although to date, existing eye drop preparations require up to hourly instillation and are hence challenging for patient treatment adherence. Crystals found only in the corneal epithelium can sometimes be managed by removal of the outer corneal layers (superficial keratectomy).
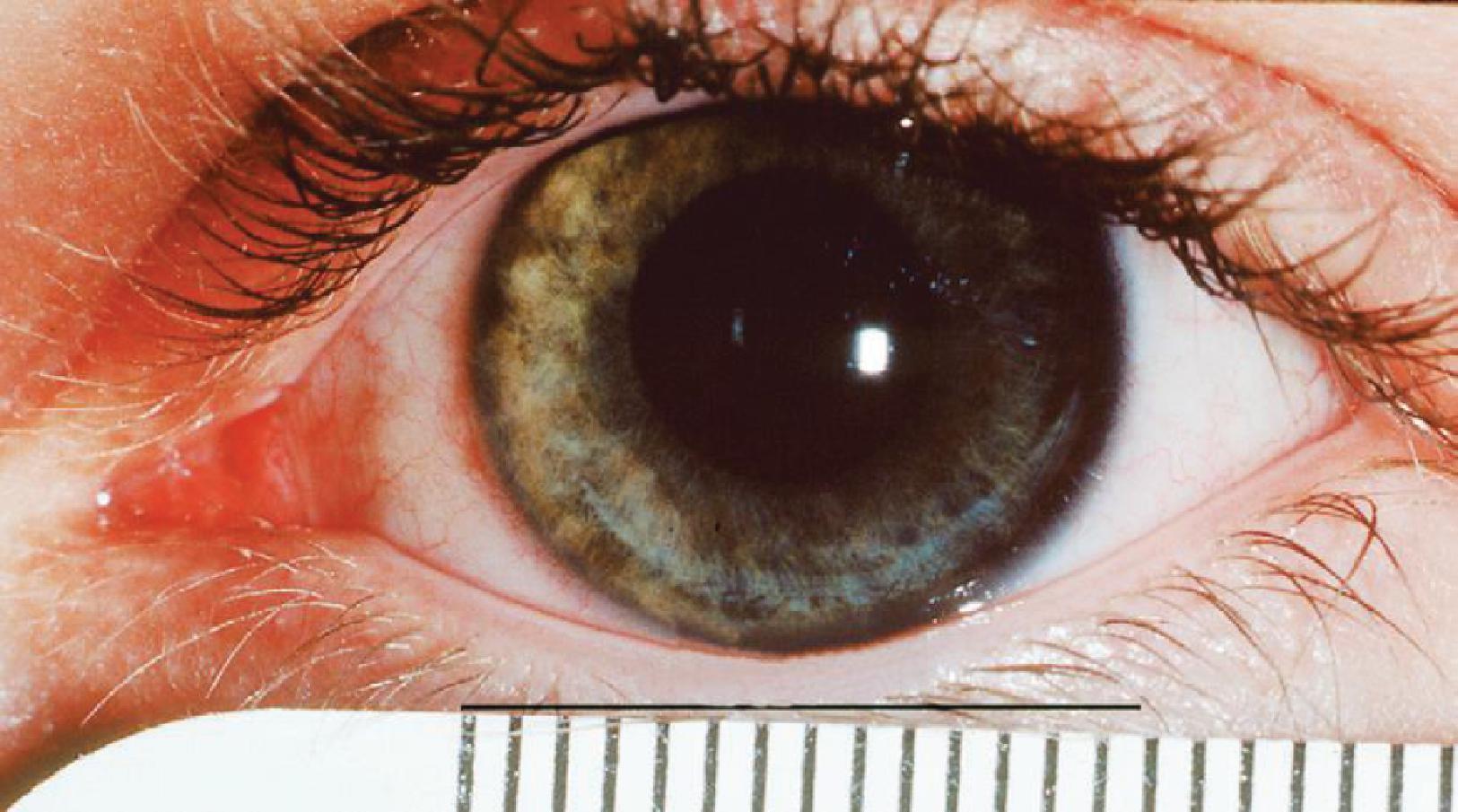
Megalocornea is defined as a corneal diameter >12 mm at birth or >13 mm after 2 years of age in the absence of elevated eye pressure ( Fig. 64.5 ). It is usually bilateral and may be isolated or associated with other ocular or systemic disorders.
Isolated megalocornea is most commonly inherited in an X-linked recessive pattern (90%) and thus occurs mostly in males. It can be inherited in an autosomal recessive manner or very rarely in an autosomal dominant fashion. It is associated with several gene mutations including CHRDL1 (X-linked megalocornea), LTBP2 , SH2PXD2B , NOTCH2 , PIK3R1 , ZNF469 , and chromosome 16 duplication.
Clinical measurement of horizontal corneal diameter is diagnostic. It is important to rule out congenital glaucoma by measuring eye pressure, axial globe length, and refraction and assessing the ocular structures, especially corneal clarity and optic nerve cupping (all of which are affected in glaucoma but not megalocornea).
Intervention is not needed for isolated megalocornea, because it is nonprogressive. Dryness due to exposure can be treated with artificial tears. Treatment of associated ocular or systemic issues are determined by a multidisciplinary team.
Microcornea is defined as a clear cornea of normal thickness with a diameter <9 mm at birth or <10 mm after 2 years of age ( Fig. 64.6 ). It is most commonly associated with other ocular findings such as cataract, coloboma, iris maldevelopment, retinal underdevelopment or outpouching, nystagmus, and/or ptosis. Various systemic findings such as skeletal, cardiac, genitourinary, and neurologic defects have been reported in association with microcornea.
Isolated microcornea is very rare. It is thought to represent an arrest of corneal growth after differentiation is complete in the fifth month age of gestation. Genetic association is poorly defined, , but mutations in PAX6 , CRYBB1 , ZNF408 , and WDR37 have been reported. It has been associated with an FBN1 mutation in one case of severe neonatal Marfan syndrome and bilateral ectopia lentis. In utero exposure to cytomegalovirus has also been implicated.
Clinical measurement of horizontal corneal diameter is diagnostic. Because it rarely occurs in isolation, further investigation to uncover associated ocular or systemic features is warranted. Eye pressure, portable slit-lamp biomicroscopy, and dilated fundus exam should be performed in the first few weeks of life. Further imaging, such as AS-OCT or UBM, may be advisable depending on clinical findings.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here