Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sodium disorders are relatively common in hospitalized patients and elderly people.
The brain is most at risk from acute hyponatraemia because the osmotically expanded intracellular volume may induce increased intracranial pressure (hyponatraemic encephalopathy).
Treatment of hyponatraemia needs to be carefully individualized because of the risk of osmotic myelinolysis.
Hypernatraemia has a high in-hospital mortality rate, which often reflects severe associated medical conditions.
Although usually benign, hypokalaemia may cause cardiac arrhythmias and rhabdomyolysis. Oral replacement is usually sufficient, except where there is severe myopathy or cardiac arrhythmias.
Electrocardiogram changes in the presence of hyperkalaemia require urgent potassium-lowering measures and myocardial protection with calcium.
Management of severe hypercalcaemia includes enhancement of renal excretion of calcium, inhibition of osteoclast activity and treatment of the underlying condition.
Acute symptomatic hypocalcaemia should be treated with intravenous calcium.
Hypomagnesaemia is difficult to diagnose because its symptoms are non-specific and the serum level often does not reflect the true magnesium status of the patient. It usually exists as a ‘deficiency triad’ with hypokalaemia and hypocalcaemia.
Hypermagnesaemia is often iatrogenic, particularly in elderly patients or patients with renal impairment and/or chronic bowel conditions receiving magnesium therapy.
Hyponatraemia, defined as serum sodium concentration of less than 130 mmol/L, is a common condition. The prevalence is estimated at 2.5% in hospitalized patients, two-thirds of whom develop the condition while in hospital.
Hyponatraemia is almost always associated with extracellular hypotonicity, with an excess of total body water relative to sodium (hypotonic hyponatraemia). The exceptions are:
Normotonic hyponatraemia (pseudohyponatraemia): an artefactually low, and rarely seen, sodium measurement seen in hyperlipidaemia and hyperproteinaemia.
Hypertonic hyponatraemia: a dilutional lowering of the measured serum sodium concentration in the presence of osmotically active substances, such as glucose, mannitol, glycerol and sorbitol. In the presence of hyperglycaemia, the true serum sodium can be estimated by adjusting the measured serum sodium upwards by 1 mmol/L for each 3 mmol/L rise in glucose above normal.
Hyponatraemia causes cellular swelling as water moves down an osmotic gradient into the intracellular fluid. Most of the symptomatology of hyponatraemia is produced in the central nervous system (CNS) by the swelling of brain cells within the rigid calvarium, causing raised intracranial pressure (hyponatraemic encephalopathy). As intracranial pressure rises, adaptive responses come into play, returning brain volume towards normal and restoring cellular function.
For this reason, chronic hyponatraemia is generally better tolerated than acute hyponatraemia. Patients can become encephalopathic when hyponatraemia develops rapidly and the adaptive responses have not had time to develop or fail.
Hyponatraemic encephalopathy carries a high mortality (50%) if left untreated.
Hypotonic hyponatraemia may be classified according to the volume status of the patient (hypovolaemic, euvolaemic or hypervolaemic).
These patients have deficits in both total body sodium and total body water, but the sodium deficit exceeds the water deficit. Causes are listed in Box 12.2.1 . Determination of the urinary sodium concentration can differentiate renal or extra renal losses. Extrarenal losses are usually associated with low urinary sodium concentrations (<20 mmol/L) and hyperosmolar urine. The exception is with severe vomiting and metabolic alkalosis, where bicarbonaturia obligates renal sodium loss and urinary sodium is high (>20 mmol/L), despite volume depletion. However, urinary chloride, a better indicator of extracellular fluid (ECF) volume, is low.
Diuretics
Mineralocorticoid deficiency—Addison disease
Salt-losing nephropathy
Ketonuria
Osmotic diuresis—glucose, mannitol, urea
Bicarbonaturia with metabolic alkalosis
Vomiting—self-induced, gastroenteritis, pyloric obstruction
Diarrhoea
Excessive sweating
Blood loss
Third-space fluid loss—burns, pancreatitis, trauma
Total body water is increased with only minimal change in total body sodium. Volume expansion is mild and usually not clinically detectable. Causes are listed in Box 12.2.2 .
Psychogenic polydipsia
Iatrogenic water intoxication
Absorption of hypotonic irrigation fluids during TURP
Inappropriate intravenous fluid administration
Postoperative hyponatraemia (elevated ADH levels)
Non-osmotic ADH secretion
Glucocorticoid deficiency
Severe hypothyroidism
Thiazide diuretics
Drugs (ADH analogues, potentiation of ADH release, unknown mechanisms)
Psychoactive agents: phenothiazines, SSRIs, TCAs, MAOIs, ‘ecstasy’
Oxytocin
Anticancer agents: cyclophosphamide, vincristine, vinblastine
NSAIDs
Carbamazepine
Chlorpropamide
SIADH
ADH, Antidiuretic hormone; MAOI, monoamine oxidase inhibitor; NSAIDs , non-steroidal anti-inflammatory drugs; SIADH , syndrome of inappropriate antidiuretic hormone; SIAOH, syndrome of inappropriate antidiuretic hormone secretion; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; TURP, transurethral resection of prostate.
Total body water is increased in excess of total body sodium. Causes include congestive cardiac failure, hepatic cirrhosis with ascites, nephrotic syndrome and chronic renal failure.
In addition to the features of the underlying medical condition and alteration in extracellular volume, clinical manifestations of hyponatraemia per se usually develop when serum sodium is less than 130 mmol/L. The severity of symptoms depends partly on the absolute serum sodium concentration and partly on its rate of fall. At sodium concentrations from 125 to 130 mmol/L, the symptoms are principally gastrointestinal, whereas at concentrations below 125 mmol/L, the symptoms are predominantly neuropsychiatric. The principal signs and symptoms of hyponatraemia are listed in Box 12.2.3 .
Anorexia
Nausea
Vomiting
Lethargy
Muscle cramps
Muscle weakness
Headache
Confusion/agitation
Altered conscious state
Seizures
Coma
Population groups particularly prone to acute hyponatraemic encephalopathy have been identified ( Box 12.2.4 ).
Postoperative
Menstruating females
Elderly women on thiazide diuretics
Prepubescent children
Psychiatric polydipsic patients
Hypoxaemic patients
AIDS patients
Patients taking ‘Ecstasy’ (MDMA)
Endurance athletes
Premenopausal women appear at risk because oestrogen and progesterone are thought to inhibit the brain Na-K-ATPase and increase circulating levels of antidiuretic hormone (ADH).
Psychogenic polydipsia occurs primarily in patients with schizophrenia or bipolar disorder. These patients develop hyponatraemia with a far lower fluid intake than is usually necessary (over 20 L of water/day in a 60 kg man, in the absence of elevated levels of ADH) and it may arise through a combination of factors: antipsychotics, increased thirst perception, enhanced renal response to ADH and a mild defect in osmoregulation.
Exercise-associated hyponatraemia occurs in endurance athletes and mainly relates to the consumption of excessive fluid.
Hyponatraemia in AIDS is common and associated with a high mortality. It may be secondary to syndrome of inappropriate ADH (SIADH), adrenal insufficiency or volume deficiency with hypotonic fluid replacement.
‘Ecstasy’ (MDMA) been associated with acute hyponatraemia due to a combination of increased secretion of ADH and drinking large quantities of water in an attempt to prevent dehydration.
This is a diagnosis of exclusion and is characterized by inappropriately concentrated urine in the setting of hypotonicity. It accounts for approximately 50% of all cases of hyponatraemia. These patients have elevated serum ADH levels without an obvious volume or osmotic stimulus. The diagnostic criteria for SIADH secretion are shown in Box 12.2.5 and conditions associated with the syndrome are listed in Box 12.2.6 .
Hypotonic hyponatraemia
Urine osmolality >100 mmol/kg (i.e. inappropriately concentrated)
Urine sodium >20 mmol/mL while on a normal salt and water intake
Absence of extracellular volume depletion
Normal thyroid and adrenal function
Normal cardiac, hepatic and renal function
No diuretic use
Neoplasms (ectopic ADH production)
Bronchogenic carcinoma
Pancreatic carcinoma
Lymphoma
Mesothelioma
Thymoma
Carcinoma of the bladder
Pulmonary disease
Pneumonia
Tuberculosis
Aspergillosis
Cystic fibrosis
Chronic obstructive airways disease
Positive-pressure ventilation
CNS disease
Encephalitis
Acute psychosis
Head trauma
Brain abscess
Meningitis
Hydrocephalus
Brain tumour
Delirium tremens
Guillain–Barré syndrome
Stroke
Subdural or subarachnoid bleed
HIV infection
Pneumocystis carinii pneumonia
ADH, Antidiuretic hormone; CNS , central nervous system.
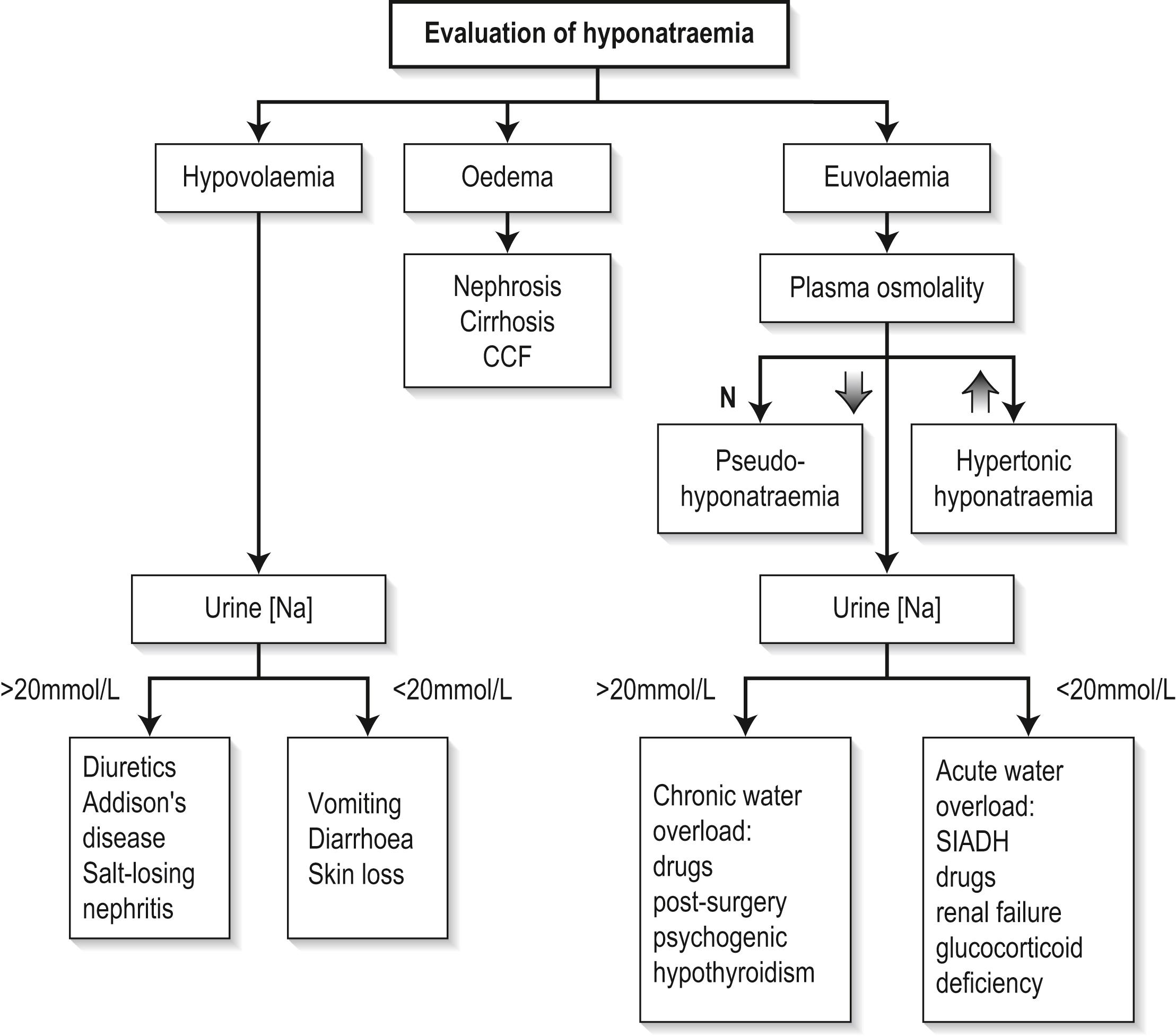
Measurement of serum and urine sodium concentrations and osmolalities, in addition to clinical assessment of volume status, are essential for the assessment of hyponatraemia ( Fig. 12.2.1 ).
There is ongoing controversy over the treatment of hyponatraemia because of the risk of osmotic demyelination, which is discussed below.
Treatment of the underlying cause is obviously essential; it should be carefully individualized and depends on the presence of symptoms, the duration of the hyponatraemia and the absolute value of sodium. Ideally, correction of the serum sodium should be of a sufficient pace and magnitude to reverse the manifestations of hypotonicity but not be so rapid and large as to pose a risk of the development of osmotic demyelination.
Acute symptomatic hyponatraemia is a medical emergency requiring prompt and aggressive treatment, aiming to achieve a serum sodium level of at least 125 mEq/L. An immediate increase in serum sodium concentration by 8 mEq/L over 4 to 6 hours is recommended. This can be achieved by infusing hypertonic saline (3% NaCl) at a rate of 1 to 2 mL/kg/h, which should raise the serum sodium by 1 to 2 mmol/L/h. Where neurological symptoms are severe, hypertonic saline can be infused at 4 to 6 mL/kg/h. Serum sodium concentrations should be monitored closely. Other measures to reduce intracranial pressure, such as intubation and intermittent positive pressure ventilation, may also be required.
Chronic hyponatraemia presents the greatest dilemma. Care must be taken with correction of sodium as these patients are at the greatest risk of developing osmotic demyelination, yet the presence of encephalopathy mandates urgent treatment. In these patients, hypertonic saline can be infused so that a correction rate of no more than 1 to 1.5 mmol/L/h is maintained. Therapy with hypertonic saline should be discontinued when (1) the patient becomes asymptomatic, (2) the serum sodium has risen by 20 mmol/L, or (3) the serum sodium reaches 120 to 125 mmol/L. Thereafter, slower correction with water restriction should follow. The serum sodium should never be acutely elevated to hypernatraemic or normonatraemic levels and should not be elevated by more than 25 mmol/L during the first 48 hours of therapy.
In this situation, saline infusion is usually not required and patients can be managed by treating the underlying disorder, discontinuing diuretic therapy or restricting fluids. Fluid restriction is inexpensive and effective but is often limited by patient non-compliance. Other treatment options include pharmacological inhibition of ADH with demeclocycline, which is limited by its neuro- and nephrotoxic side effects, or increasing solute with the use of furosemide or urea.
This is an iatrogenic disorder which develops progressively over 3 to 5 days following the correction of hyponatraemia. It classically produces symmetrical lesions centred on the midline of the pons and was originally described as ‘central pontine myelinolysis’. However, about 10% of cases involve extrapontine lesions. It is reported as occurring in 25% of severely hyponatraemic patients following correction of serum sodium. Clinically, the disorder is initially manifested by dysarthria, mutism, lethargy and affective changes, which may be mistaken for psychiatric illness. Classically, pseudobulbar palsy and spastic quadriparesis are observed. Recovery is usually gradual and incomplete, although both fatalities and complete recovery are reported. Demyelination in the central pons and extrapontine sites can be demonstrated on magnetic resonance imaging (MRI) scan or at autopsy.
It appears that the risk of developing osmotic myelinolysis is associated with severity and chronicity of hyponatraemia. It rarely occurs if the serum sodium is >120 mmol/L or where hyponatraemia has been present for <48 hours. Alcoholics, malnourished patients, hypokalaemic patients, burn victims and elderly patients on thiazides seem to be most at risk of developing osmotic demyelination
Both the rate and the magnitude of sodium correction appear important in the development of osmotic myelinolysis. To date, although there is no agreed rate of correction regarded as completely safe, most authorities suggest that the serum sodium concentration should not rise by more than 10 to 14 mmol/L during any 24-hour period.
Hypernatraemia (Na >150 mEq/L) is much less common than hyponatraemia.
It is important to recognize hypernatraemia because it is usually associated with severe underlying medical illness. It is a condition of hospitalized patients, the elderly and dependent people. The incidence of hypernatraemia in hospitalized patients ranges from 0.3% to 1%, with from 60% to 80% of these developing hypernatraemia after admission. In-hospital mortality is high (40% to 55%).
Hypernatraemia is a relative deficiency of total body water compared to total body sodium, thus rendering the body fluids hypertonic. The normal compensatory response includes stimulated thirst—the most important response—and renal water conservation through ADH secretion. In the absence of ADH, water intake can match urinary losses because of increased thirst, but where the thirst mechanism is absent or defective, patients become hypernatraemic even in the presence of maximal ADH stimulation. Therefore hypernatraemia is usually seen where water intake is inadequate, that is, in patients too young, too old or too sick to drink, with no access to water or with a defective thirst mechanism.
Extracellular hypertonicity causes a shift of water from the intracellular space until there is osmotic equilibrium. The resultant cellular contraction may explain some of the clinical features of hypernatraemia. The brain is especially at risk from shrinkage because of its vascular attachments to the calvarium. Haemorrhage may occur if these vascular attachments tear.
As with hyponatraemia, the rate and magnitude of the rise in sodium determine the severity of the symptoms, which is a reflection of the brain’s capacity to adapt to the deranged osmotic conditions.
The clinical causes of hypernatraemia are listed in Box 12.2.7 . Population groups at particular risk of developing hypernatraemia are listed in Box 12.2.8 .
Osmoreceptor damage/destruction
Exogenous: trauma
Endogenous: vasculitis, carcinoma, granuloma
Idiopathic: psychogenic, head injury
Drugs
Poor intake
Confusion
Coma
Depression
Dysphagia
Odynophagia
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here