Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Mass casualties due to combat operations, or natural or manmade disasters, have the capacity to overwhelm multiple levels of care and evacuation capabilities of any system. Military and civilian institutions need a mass casualty response plan in order to facilitate the transition from the routine care of patients to an exponential increase in the required personnel, supplies, and equipment in order to meet the demand.
Effective mass casualty response is established on the principle of triage ; “triage” comes from the French verb “trier,” meaning to sort, separate, shift, or select. Triage is then the system of sorting patients into different categories based on their injuries/illnesses, severity, and prognosis in order to prioritize their treatment with the available resources. Do “the greatest good for the greatest number” has been the proverbial dictum of an ideal triage scenario. The reality is that medical triage is a dynamic and complicated process that includes on-site rescue, evacuation, receiving hospital preparedness, and decontamination (if required). All stages of the continuum of care from the initial event to discharge of the patient require some level of triage by different personnel. Proper medical triage is dependent on many variables not controlled by a single individual but by an experienced team that will approach the casualties taking in consideration real time (ideally) information of the expected numbers of injured and resources and personnel available to handle them. Normative practice of care to include triage during mass casualty events is a mistake made from those that ignore the exponential needs of the patients preventing a logical allocation of resources.
Triage fails in one of two fundamental ways: overtriage and undertriage.
“Undertriage” is defined as the failure of the system to identify severely injured patients who could benefit from rapid evacuation and emergency surgery. Undertriage means poor sensitivity of the system.
“Overtriage,” on the other hand, is the inefficient use of staff and resources on noncritical patients who received immediate care but could have safely waited. Overtriage denotes poor specificity of the system.
Undertriage of less than 5% and overtriage of 35% to 50% is deemed acceptable according to the American College of Surgeons, Committee of Trauma. Other investigators of trauma triage rules agree that an overtriage of 50% to 60% is necessary to reach an undertriage rate of around 10%. Later in the chapter I will discuss how many of the triage algorithms like the four-tiered START (Simple Triage and Rapid Treatment) triage method lead to substantial overtriage of disaster casualties. The thought process may be sustainable if we are talking about 100 to 200 casualties where overtriage may generate 10 to 20 “false reds” casualties. On the other hand, if we are talking about a large-scale disaster with 1000 to 2000 casualties, we are now dealing with 100 to 200 false red in addition to the expected 200 to 400 “true red,” a number that would clearly overwhelm even large urban area hospitals. It is important that those doing the triage adjust their criteria depending on the expected number of casualties to reduce the rate of acceptable overtriage patients even if it means an increase of undertriage casualties. In designing a response to an earthquake with many thousand casualties, it has been suggested that the casualties with a likelihood of survival of less than 50% may need to be initially “black tagged” (expectant). Ideally, triage criteria will be calibrated/standardized using a severity score like the Revised Trauma Score (RTS), which we will discuss in the next segment. The RTS will help balance the resources available with the scope of casualties. Realistically, however, it does not make sense to expect to know exactly the number of casualties in a disaster in order to adjust the triage method, but it is important to prepare different triage plans for different scales of mass casualties and disasters.
The very first documented instance of prioritizing patients by prognosis dates back to the 17th century bc. The Edwin Smith papyrus recovered from a tomb in Thebes, Egypt, is the oldest known surviving trauma text in history. Ancient Egyptian triage medicine focuses their care in the likelihood of surviving an injury as the main outcome of interest.
Baron Dominique Jean Larrey introduced the current understanding of the concept of Triage, in the late 18th to early 19th century. Baron Dominique Jean Larrey was Napoleon’s Army surgeon who would treat the wounded in the battlefield according to the gravity of their injuries, regardless of nationality or rank. He described in his memoirs “that it is necessary to always begin treating the most dangerously injured soldier.” In 1846, John Wilson, a British naval physician, recommended that casualties with minor or fatal injuries be deferred in order to prioritize the treatment of the severely injured. All the same concepts are relevant today as well as the challenges to identify the patients that are not in either category during combat operations or a mass casualty incident.

French doctors who separated the wounded into three categories further refined triage during World War I:
Soldiers that were expected to live, regardless of the care provided at the aid stations
Soldiers expected to die, regardless of the care provided at the aid station
Soldiers for whom immediate care would make a difference in survival
Military triage evolved from World War II, Korea, and Vietnam producing significant reduction in the elapse time of the injury to definitive care to less than 2 hours, improving outcomes. Further advances in medical transportation, including the use of helicopters during the Korean War, demonstrated that proper triage and rapid evacuation to a facility capable of caring for the injured patient saves lives.

In the late 1970s to early 1980s there was an interest to develop a civilian prehospital trauma triage system for individual casualty since there were early indications that patients treated at trauma centers had better outcomes. Field triage decision rules were developed with data from trauma registries to assist in the sorting of trauma patients to the proper level of care in order to prevent overburdening trauma centers. Formal triage scoring systems were developed to assist emergency medical service (EMS) in that decision. The trauma scoring system is designed to take the subjective out of triage on the field.
Civilian and military triage systems in the 1990s continued to share trauma-scoring systems like the Champion’s Revised Trauma score. Civilian and military classifications for mass casualty incident (MCI) use color-coding and comparable levels of acuity. Trauma Sieve and START, which are similar triage decisions, have been use by EMS and the military.
The complexity of decision making in triage varies significantly, often depending on the level of training and experience of the triage officer on the field and at the hospitals. During combat operations tactical combat casualty care divides field triage and care into three phases: care under fire, tactical field care, and tactical casualty evacuation. Care under fire is the care given by a medic or warfighter at the scene of the injury while still under effective hostile fire. In this scenario the focus is on returning fire, controlling hemorrhage by pressure dressings or tourniquets for extremity bleeding. Rapid and lifesaving interventions on the field include a patent airway, resolution or temporizing measure of an open or tension pneumothorax, splinting of extremities, and administration of medications. Casualty evacuation requires on-scene triage personnel to prioritize their evacuation to a higher level of care. The responsibility is enormous to the medic on the field, so a triage scoring system is utilized to assist in the decision-making process and avoid over- or undertriage of the casualties.
Triage scoring offers a sophisticated and flexible approach to triage. The triage scoring system in the military evolved from patient physiologic measures to include Glasgow Coma Scale (GCS), systolic blood pressure (SBP), respiratory rate (RR), and pulse rate or character (HR). The RTS is calculated by adding GCS, RR, HR, and SBP and is a good predictor of mortality risk and the need for massive blood transfusion in combat as analyzed using the data of the U.S. Joint Theater Trauma Registry. The military further modified the RTS due to the difficulty of an accurate SBP on the field with what is called Field Triage Score. The Field Triage Score relies on measurements of the motor component of the GCS and the presence of the radial pulse as a surrogate for an SBP of at least 100 mm Hg. These numbers are then indexed on a scoring system from 0 to 2. The Field Triage Score has been validated retrospectively using the U.S. Joint Theater Trauma Registry as a better predictor than the RTS of mortality rate and length of stay of the combat injured.
The use of a “scoring system” in the civilian and military mass casualties can assist the triage personnel in sorting casualties’ seriousness using more objective criteria for evacuation from the field. The two best-known scoring systems are Champion’s Trauma Score and RTS. The original Trauma Score used capillary refill and respiratory expansion, making those observations very unreliable during a mass casualty or disaster event. The RTS uses GCS, SBP, and RR and can yield a score between 0 to 12. An RTS of 12 predicts mortality of less than 1% (when giving routine care) and a RTS of 5 predicts a 50% mortality. Other notable scores are the Contact Research and Manufacturing Services and the Triage Index, which have also shown suboptimal test characteristics. I will be discussing those scoring systems in more detail in the upcoming sections. The real advantage of a scoring system is that no particular physiologic state preordains a specific triage category; rather a score for “black” and “red” and “yellow” can be established in real time, based on perceived balance of casualties and medical resources.
Pediatric casualties require a special triage criterion due to physiologic differences in the cardiovascular, neurologic, and respiratory systems. These differences are the main reason there is a dedicated pediatric trauma score and pediatric triage tape.
A far simpler alternative to the triage scoring is a triage algorithm, such as the START system. This system, for example, assigns red based on a rigid set of criteria (if airway is compromised; if minute RR is over 30; if capillary refill is over 2 seconds; or if simple commands cannot be followed). Triage Sieve (later discuss in more detail) is another example of an inflexible assignation algorithm; it includes an upper and lower limit for red RR, as well as a fixed upper limit of HR (unlike START, it does not use capillary refill). The advantage of such a rigid system is the simplicity to teach and learn to be used in an MCI with dozens or hundreds of casualties. The disadvantage is the inflexibility that can over or undertriage casualties.
In 2011 the Centers for Disease Control and Prevention sponsored a project to review existing triage systems and develop a national standard for mass casualty triage. The conclusion was that there is insufficient evidence to compare the existing systems or to identify a superior system. Combining the best of all systems, the project developed an algorithmic system, called SALT triage (Sort, Assess, Lifesaving Interventions, Treatment and/or Transport). The system uses the ability to ambulate or follow commands to globally sort patients and prioritize assessment, and it emphasizes the rapid performance of simple, potentially lifesaving intervention such as hemorrhage control and chest decompression. Ultimately the patients are assigned to one of five categories and transported or treated accordingly: immediate, expectant, delayed, minimal, or dead. While SALT was designed in consideration of the best available evidence, it, like other triage systems, is largely consensus based and requires further research to determine if it is effective.
There are special triage considerations that do not fit into standard categories or pose a risk to other casualties, medical personnel, or the facility itself. We are all familiar with the wounded contaminated in a biological and/or a chemical battlefield environment and those with retained unexploded ordinance. In 2020 the worldwide pandemic by a novel coronavirus overwhelmed medical systems around the globe. The COVID-19 pandemic increased the demand of critical care surge capabilities, prompting implementation of triage protocols to determine ventilator allocation.

The novel coronavirus pandemic affected the way casualties were triaged and treated not only in combat zones but also in civilian institutions. Lacking national guidance, many hospitals around the world were forced to institute independent and autonomous triage protocols following ethical principles and clinical criteria. However, the most controversial type of triage during the pandemic was the nonclinical criteria adopted by many countries based on an age cutoff value for unilaterally withholding Advance Life Support. There are reports of using “social utility” criteria, prioritizing health care professionals using first come, first served policies to provide care or access to ventilators.
Throughout the chapter we will revisit many of these topics as well as analyze the most common triage methods used worldwide, the usefulness of a triage scoring system, and how we can prepare our institution for the next mass casualty event.
One of the most significant contributions to survivability in modern warfare has been the proximity of resuscitative and surgical units to combat operations. Casualties are rapidly evacuated along a continuum of care within a theater of combat operations, a region of the globe, and eventually to the continental United States. The U.S. Military Trauma System of the 21st century depends on the proper triage, treatment, and evacuation of casualties to a higher level of care when required.
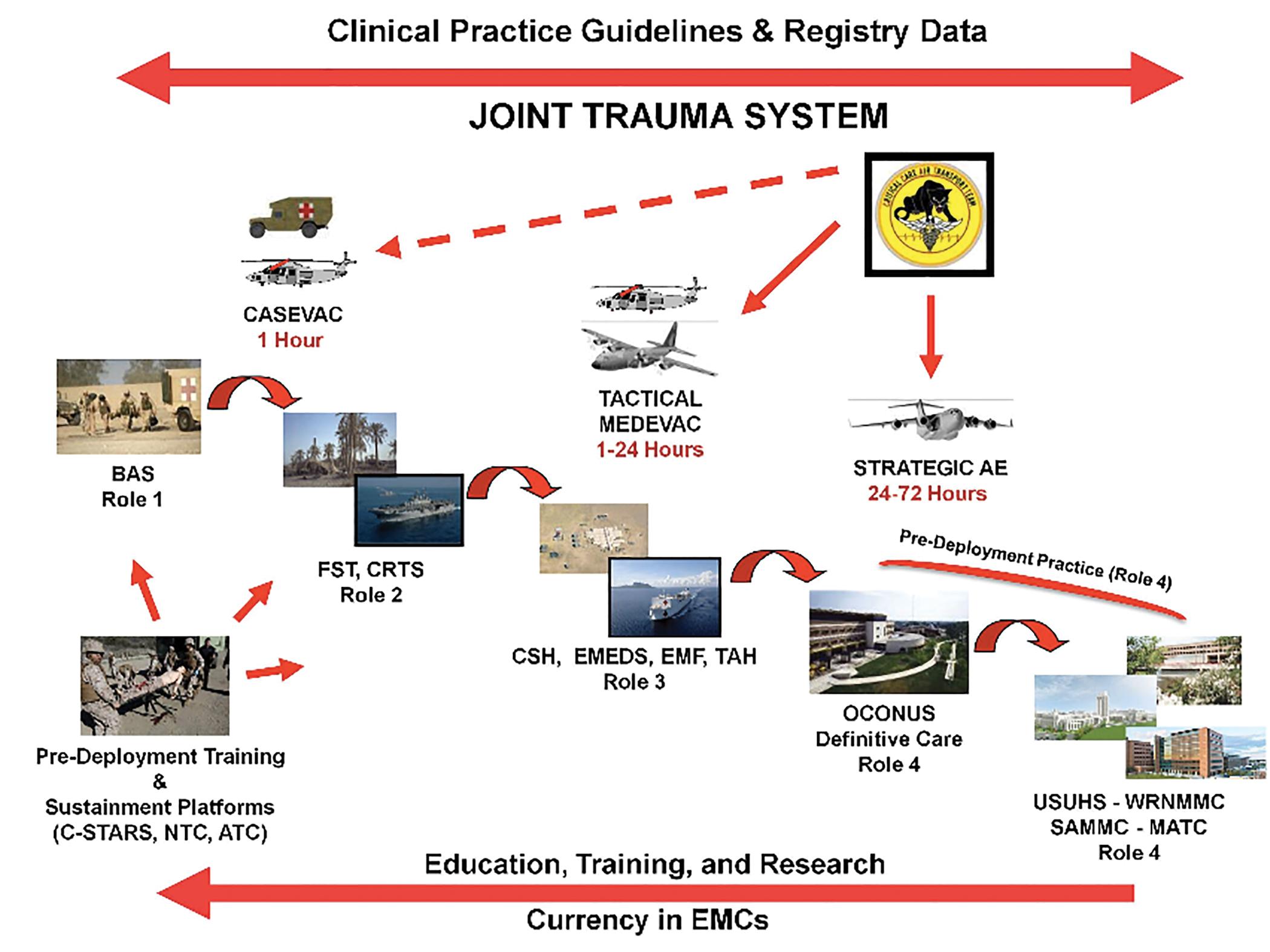
The asymmetric nature of modern warfare increases the likelihood of disruption of supply chains and the potential for direct physical injuries to far forward medical personnel. This operational reality makes military triage a particular difficult challenge to the medical unit expected to care for complex casualties in austere environments.
The unique aspects of military triage can provide valuable lessons to the increasingly complex civilian mass casualties and disaster. Let’s briefly discuss the similarities and relevance to our mutual goal of saving lives.

An overarching concept in the execution of military triage is “Medical Rules of Engagement” (MEDROE). MEDROE provides the guide for the range of care for populations at risk in a theater of operation based on mission, immediate tactical situation, and available resources. A well-crafted MEDROE provides the unit medical commander and staff with real-time decision tools to care for the projected casualties and patients in a theater of operations. The projections will factor in civilian populations, noncombatants, contractors, and injured enemy combatants requiring special security arrangements. The unpredictable number of casualties and the limited facility holding capacity of the levels 1, 2, and even 3 (usually 12 patients) gives us a glance of the importance of proper triage and the need for rapid evacuation of the casualties through the military continuum of care. The civilian disaster planners should be able to reproduce contingency plans to decompress facilities that are overwhelmed by overtriaged individuals during a disaster. Even when a hospital has no apparent shortage of holding capacity during normal operations, the reality is that during a disaster or a mass casualty, those beds are of no use if you do not have the resources to staff them appropriately. In recent years we have seen many examples of opposite poles of this assessment, like the Boston bombing where multiple EMS teams were already standing by and quickly moved the injured patients to different hospitals. The advantage in that particular example is that the routes from the site of the explosion to the different hospitals had been blocked beforehand by the security and medical planners of the Boston Marathon. In contrast we have the Las Vegas shooting and the 911 Pentagon attacks where many ambulances were blocked by the traffic and the chaos of the disaster. One aspect not seen during medical care in a combat zone is the fact that many of the casualties are brought to the hospital in private vehicles bypassing triage or initial care. The majority of those patients are walking wounded and do not require emergency care. It is important for the civilian hospitals to immediately set up a triage station preferably outside of the hospital to prioritize the patients that need medical interventions to survive.
Since there is a high probability of mass casualty events in war, the medical units are constantly training with the goal of incorporating different variables during the simulation scenarios that sometimes involves the entire base and different medical echelons. The average training evolution is 2 hours long, three times a week. That kind of commitment is one of the reasons of the success in triage, treatment, and evacuation of mass casualty victims in the military. Our motto “train as you fight” is one of the reasons we currently have 98% survival rate amongst combat casualties.
The extent of injury associated to weapons of war has no comparison to any injury pattern seen in the civilian community with the exception of incidents involving accidental or terror-related explosions. Rapid triage and treatment sometimes at the scene by well-trained forces has been a crucial element in the current 98% survival rate. Simple interventions like tourniquets, needle chest decompression, and airway-related lifesaving maneuvers provide the casualty on the field the time to reach a forward deployed surgical unit. EMS teams all over the world have adopted many of the proven concepts including triage criteria used by the military medics/corpsman.
As mentioned before, the MEDROE dictates the day-to-day guide for the range of care available for the population at risk in the theater of operation. Those triage decisions are based on unit mission and tactical situation and are adjusted as the situation on the ground and resources change. The civilian community should adopt at each institution, county, city, and state a framework with those principles. Desktop exercises should incorporate different scenarios requiring diverse triage priorities during a mass casualty or disaster.
In the ideal world rapid transfer of mass casualties from the scene to a facility should be in what we call the “platinum 10 minutes.” We need to look beyond the golden hour in the current conflicts if we want to improve survival. For the civilian community the proper distribution of fire department and EMS services should strive to meet the same concept. The proximity of the mobile forward resuscitative and surgical units to the front lines are constantly trying to reduce the times from injury to care. Embedded medics, corpsman, and the casualty itself are the bridge that facilitates the proper triage and transfer of the injured in combat.
One of the elements that revolutionized the care of the injured near the front line has been the incorporation of surgical capabilities near the front line capable of performing “damage control surgery” as a bridge to more definitive care at a higher level in the continuum of care. The success of the forward surgical units has been multifactorial, from air superiority allowing rapid evacuation of the casualties to surgical triage and care at the proper echelon. One of the most efficient ways to triage casualties during combat operations has been to designate the surgeon on duty as the triage officer at Level 2 or the chief of trauma at Level 3. The surgical triage performed by the surgeon on duty is equivalent to the function of the triage officer during a civilian mass casualty or disaster response.
Depending on the setting the triage officer can be on the field but most likely he or she will be at the hospital. Like the surgeon during combat operations, the designated triage officer needs a deep understanding of emergency medical treatments, what outcomes are likely for various casualties, and the resources and manpower available at their particular institution. One of the recommendations from experts in the field is that the triage officers (you should train at least two) should be the most experienced clinician available. In many institutions around the world the surgeon in charge takes the role. Designation of the triage officers should be done as part of your mass casualty or disaster response drills. During a mass casualty or disaster response it is expected that a triage officer will evaluate 10 patients every 20 minutes. The person chosen should be respected in the institution for his experience, judgment, and leadership skills under what could be incredibly challenging circumstances.
Patients are sorted into one of four categories: immediate, delayed, minimal, and expectant.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here