Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The vast majority of nonparasitic cystic lesions of the liver are simple cysts. They are unilocular, do not communicate with the biliary tree, have a serous content, and although the epithelium does divide to account for volume expansion, they are not considered tumors and have no malignant potential. Furthermore, they do not tend to recur after partial resection. These lesions are described in detail in Chapter 73 . Although primary or secondary solid hepatic malignancies may become cystic as a result of tumor necrosis, it is extremely rare for them to be totally cystic. However, this has been described in case reports for embryonic liver sarcoma, malignant fibrous histiocytoma, or metastases from a variety of primaries, most including neuroendocrine tumors or even colorectal primary tumors.
Primarily cystic hepatobiliary neoplasms that constitute another group of cystic tumors are extremely rare. These tumors are of biliary origin and include both benign (with malignant potential) and malignant tumors that have initially been given the names of cystadenoma and cystadenocarcinoma ; however, increasing evidence, in particular from Asian authors, suggests that biliary cystic neoplasia include a wider group of entities that resemble those described in the pancreas as being either mucinous cystic neoplasms (MCNs) or intraductal papillary mucinous neoplasms (IPMNs). , The main difference relates to the presence or absence of an ovarian stroma (OS) and whether a luminal communication exists between the tumor and the bile ducts (see Chapter 89 ).
Given this confusion and based on the evolution of the classification of pancreatic mucinous cysts, the latest World Health Organization (WHO) Classification of Tumours of the Digestive System, published in 2010, proposed that the disease entity previously designated as “biliary cystadenoma/adenocarcinoma” should instead be classified as either MCN when an OS is present or IPMN of the bile duct (IPMN-B) when the tumor communicates with the biliary tree. However, some cystic neoplasms of the liver with mucinous epithelium may lack both OS and bile duct communication or at least a communication is not always demonstrated. The ratio of MCN to IPMN-B seems to vary between geographic areas, being greater than 1 in the West and less than 1 in Asia (see Chapter 89 ).
Detailed characteristics of these tumors are not always described in the literature, and the WHO-2010 classification is not widely applied even today, , casting some confusion on previous descriptions and reports of cystadenoma. Although the same confusion has been observed for cystic tumors of the pancreas, the clinical and pathologic differentiations of these two tumors are accepted worldwide now that a consensus on the definition of pancreatic MCNs has been reached. , A second problem in analyzing the literature is that because of the rarity of the tumor, the number of large series remains very limited, and most references are case reports.
The initial definitions of cystadenoma by Edmondson in 1958 and by Wheeler and Edmondson in 1985 were strict and included three distinctive features: the lesion should be (1) multilocular (composed of multiloculated cysts), (2) lined by a columnar epithelium, and (3) accompanied by a densely cellular ovarian-like stroma (see Chapter 87 ).
This definition was revisited in 1994 by Devaney and colleagues after retrospective analysis of a larger series of 70 patients. Although most fulfilled the criteria set out by Edmondson and Wheeler, that definition was considered too restrictive because the presence of an OS was inconsistently observed. Furthermore, not all cystadenoma-like lesions they saw were multilocular, and the epithelium lining was not exclusively of the columnar type; it was associated in one-third with a cuboidal epithelium. This led the authors to suggest that lesions diagnosed as cystadenoma (or cystadenocarcinoma) should include cystic tumors both with and without OS as well as those having a unilocular gross appearance. More precisely, only 14% of the tumors they observed lacked OS, and only a single patient had a unilocular tumor, which actually was a cystadenocarcinoma.
Although this landmark study showed that cystadenoma-like lesions encompass different entities (those with OS were exclusively observed in women and those without were observed in both sexes, with potentially different courses, which will be discussed later) this revision might have introduced some confusion because a detailed pathologic description of tumors subsequently reported as being cystadenoma (cystadenocarcinoma) has not always been provided, and some occasionally resemble atypical benign cysts or cystic forms of intrahepatic cholangiocarcinoma (ICC), rather than genuine cystadenoma (or cystadenocarcinoma), on the imaging or pathologic pictures illustrating these series and case reports.
It has been suggested that by differentiating biliary cystic tumors based on their stroma and communication between the tumor and the bile duct, two groups of biliary tumors could be identified that are the counterparts of pancreatic cystic neoplasms. The first group, MCN, has OS, typically does not communicate with the bile duct, and is the biliary counterpart of pancreatic mucinous cystadenoma. The second group lacks OS, communicates with the biliary ducts, and is referred to as IPMN-B, similar to the IPMN of the pancreas (IPMN-P; see Chapter 60 ). Although most cases of IPMN-B present as tubular or fusiform dilation of the involved bile duct, some may present as cystic dilations. The latter is known as cyst-forming IPMN-B and resembles cyst-forming branch-duct IPMN-P.
The most classic primary cystic tumors of the liver are hepatobiliary cystadenoma. Being of biliary origin, these tumors may occur anywhere along the biliary tree, including the common hepatic duct, cystic duct, or gallbladder, but the most frequent location, found in 83% to 94% of the patients, is the liver. , , These tumors are well known because of their inherent risk of malignant transformation, common to all adenomatous lesions. The risk of malignant transformation of hepatobiliary MCN of the liver (MCN-L), however, remains somewhat ill-defined.
Cystadenomas are exceedingly rare. No accurate incidence estimates are available, but the two largest series included 52 and 54 patients, , and most studies have involved fewer than 10 patients; in the early 2000s, it was estimated that fewer than 200 patients had been reported. It is frequently quoted that intrahepatic cystadenomas constitute less than 5% of cystic lesions of the liver based on an old report, but this figure is likely overestimated; it has since become obvious that the prevalence of simple cysts of the liver in the adult population is higher than previously thought.
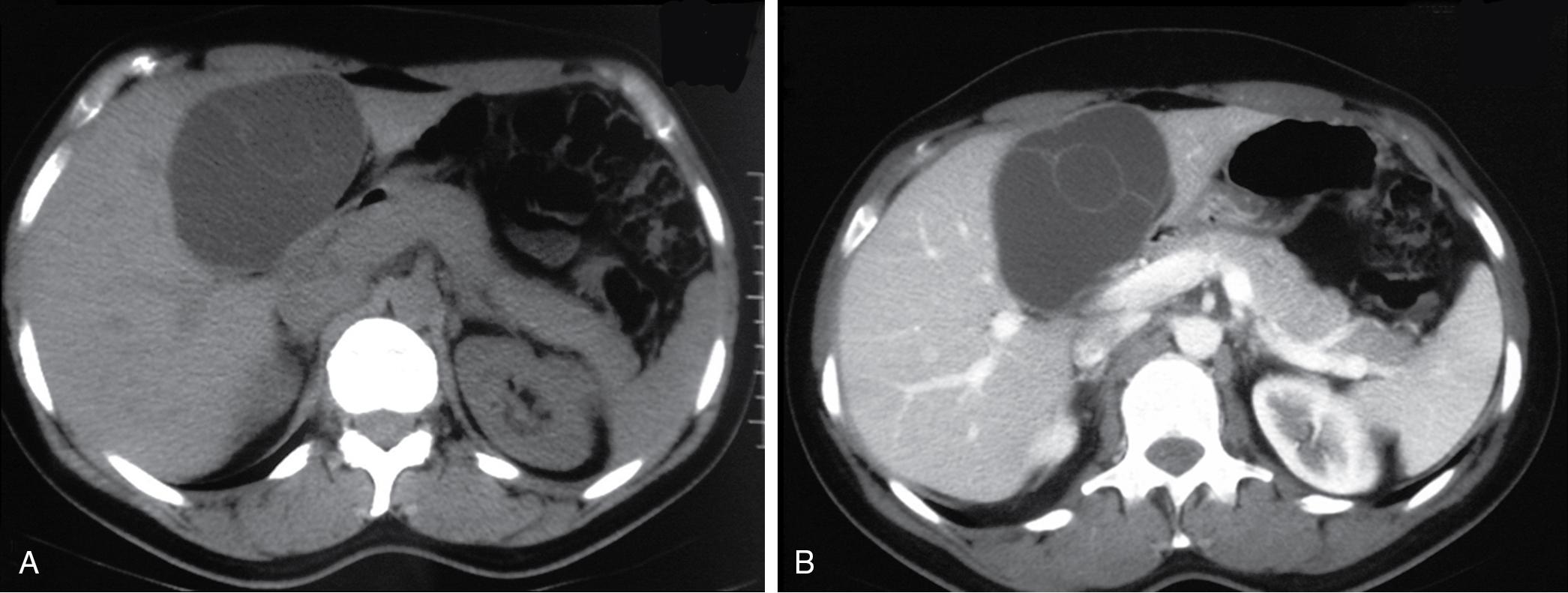
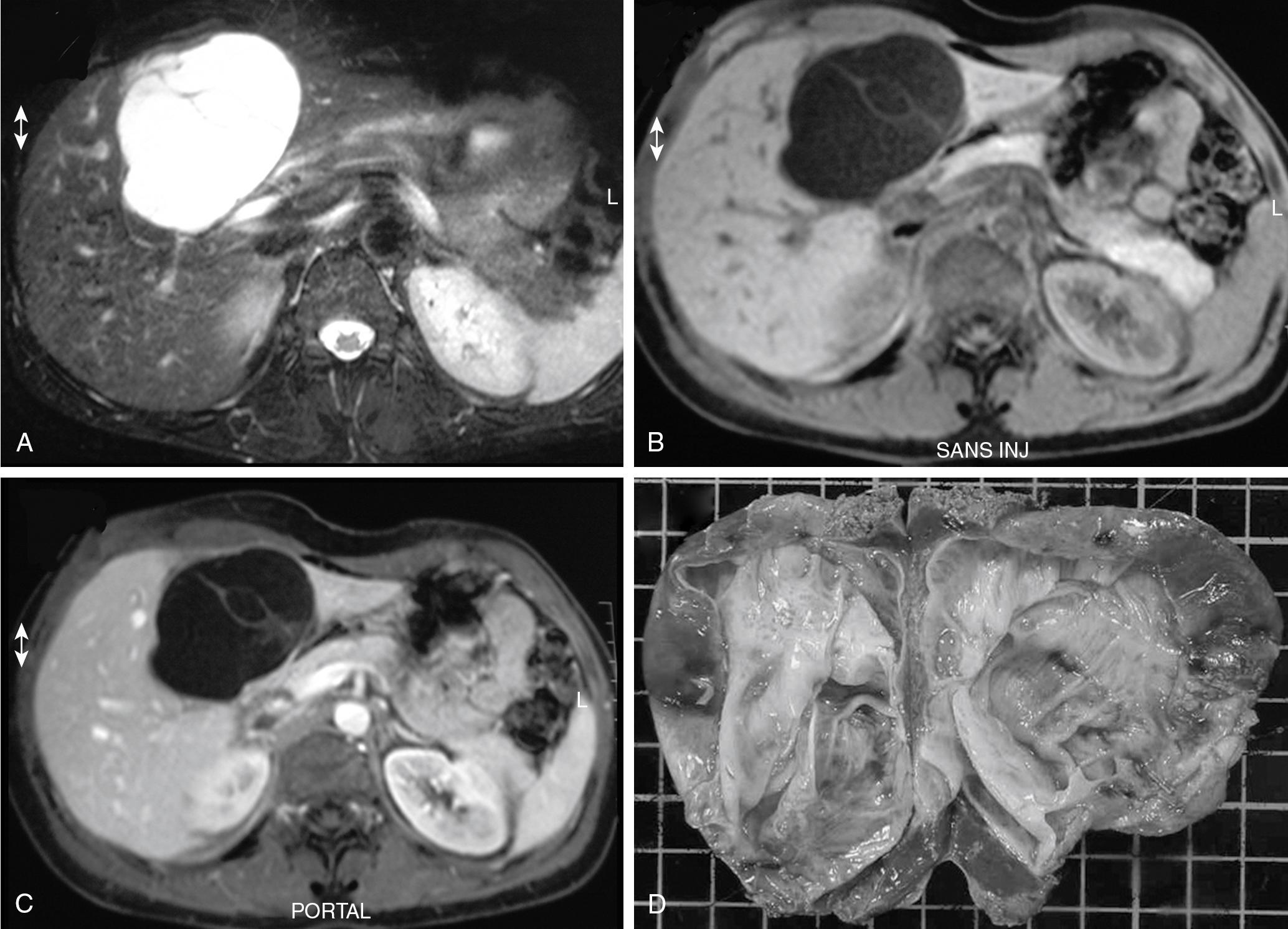
Cystadenomas are almost always solitary, and they may range in size from less than 1 to 40 cm; they are generally large, with a mean diameter of 15 cm, which suggests that they are probably slow growing. Cystadenomas have been reported to develop equally in the right and left liver or to involve both lobes (approximately 33% each) , ; however, a striking feature in our experience, as well as in recent series, is the very high proportion of tumors occurring in the left paramedian section (segment IV) or the left liver. , Pictures of cystadenoma provided in the literature also show tumors in this location almost exclusively; an example is shown in Figure 88B.1 .
Cystadenomas are grossly lobulated and multiloculated and usually contain clear to mucinous fluid. Hemorrhagic fluid may be present, but this is very rare and should raise the suspicion of malignancy. A bilious content is similarly very unusual because lack of communication with the biliary tree is a distinctive feature; however, fistulization of cystadenoma in the biliary tree has been reported, , the same as for pancreatic mucinous cystadenoma, which may explain the bilious content.
The internal lining is generally smooth but may contain microscopic or, more rarely, macroscopic polypoid lesions projecting into the lumen ( Fig. 88B.2 ). This internal lining has three distinct layers: (1) an epithelial layer, (2) a mesenchymal stroma, and (3) an outer layer of collagen connective tissue that separates it from the adjacent parenchyma ( Fig. 88B.3 ).

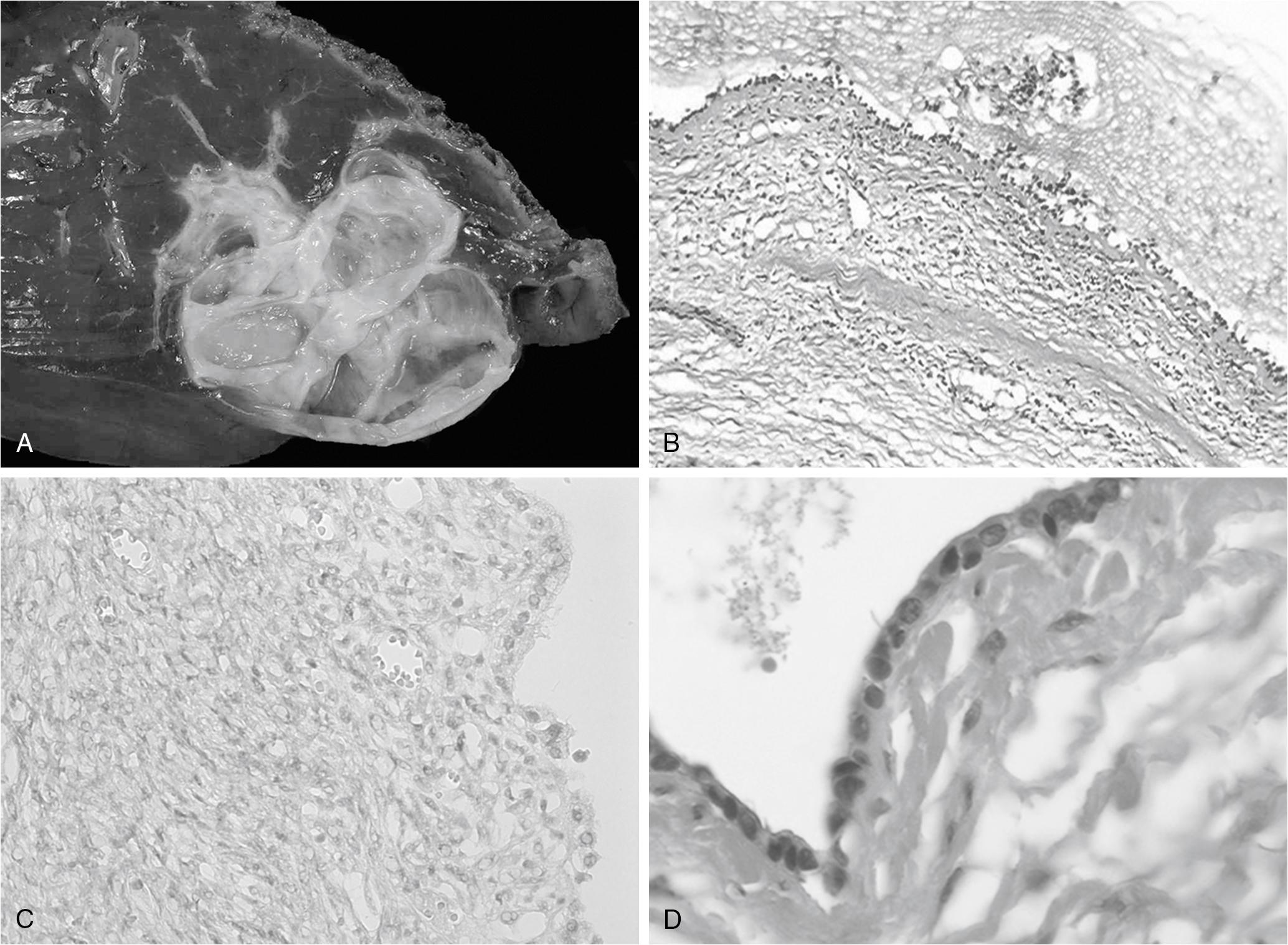
The epithelial lining , as for pancreatic cystadenoma, consists of glandular, nonciliated cells arranged in a single flat row with occasional papillary or polypoid projections, pseudostratifications, and crypt-like invaginations. In two-thirds of the patients, the epithelium is columnar, but in one-third, it consists of a combination of columnar and cuboidal epithelium. The epithelial lining may show denuded areas with chronic inflammation and hemorrhage. The columnar cells contain histologically benign-appearing, basally located nuclei and intracellular mucin. However, mucinous epithelium may be lacking in up to 20% of the cases, which may represent the initial phase of the tumor with the appearance of mucinous epithelium representing the next phase in tumorigenic progression.
The lining epithelium occasionally shows papillary infoldings, and mild epithelial atypia with a slight increase in the size of the basally located nuclei has been reported to be at least focally present in most patients. More severe dysplasia, consisting of a multilayer appearance of hyperchromatic cells with loss of polarity, appears much less frequently. Foci of intestinal metaplasia are also rare, seen in the form of numerous goblet cells. Atypia and metaplasia are suggestive of a high risk of malignant transformation.
Phenotype has been further characterized in a limited number of patients. The epithelium shows strong and diffuse cytoplasmic staining with antibodies against carcinoembryonic antigen (CEA) and cancer antigen (CA) 19-9, whereas CA-125 staining is focal or absent. , It also stains positive for cytokeratin-7 (CK-7), CK-19, CK-8, and CK-18, which supports a biliary origin, and it is negative for inhibin-α, , vimentin, and estrogen or progesterone receptors, and CD56 is only expressed focally.
The stroma consists of a compact arrangement of bland, spindle-shaped cells with round to oval nuclei. This appearance is reminiscent of OS, hence the name given to these tumors. However, it has also been found to resemble the primitive mesenchymal elements associated with the developing biliary system in the fetus. This stroma may be abundant or diffuse in approximately half of the patients but at the other extreme may only be focal in 10% of the patients and mitotic activity is not prominent. It expresses estrogen and progesterone receptors, as does the stroma of pancreatic cystadenoma , ; inhibin-α, a gonadal protein that has a more limited expression in the sex cord–stromal tissue, is also expressed in both hepatic and pancreatic mucinous cystadenoma , and in sex cord–stromal tumors. They are immunoreactive with α–smooth muscle actin, vimentin, but also desmin. There is no immune reaction with CEA, CA19-9, or CA-125. ,
A densely hyalinized pseudocapsule surrounds the tumor and separates it from the adjacent liver tissue, which explains how these tumors can be enucleated.
Despite the similarities between hepatic and pancreatic mucinous cystadenomas, few studies have compared the phenotypes of both lesions. One reported denser and more abundant stroma, more intense estrogen or progesterone receptors, and more inhibin-α in hepatic than in pancreatic cystadenomas, but the significance of this is unclear.
There are no clearly identified risk factors apart from sex because cystadenomas with OS are exclusively observed (or at least in more than 90% as for pancreatic cystadenoma) in women. However, a history of previous oral contraceptive use does not appear to be a distinctive feature. Several hypotheses have been raised based on some pathologic features of the tumor, most notably the presence of an ovarian-like stroma or the occasional presence of eosinophilic or endocrine cells. It is still unclear whether cystadenomas are of congenital origin or are acquired neoplastic lesions.
The resemblance is striking among cystadenomas with OS located in the liver, pancreas, retroperitoneum, and ovary. The particular OS common to these locations contains estrogen and progesterone receptors and inhibin-α. These similarities suggest a common pathway of tumor development, although simultaneous occurrences of hepatic cystadenoma with pancreatic or ovarian cystadenoma are exceedingly rare.
One hypothesis is that during embryonic development, ectopic ovarian cells would have migrated to the liver or pancreas, released hormones and growth factors, and caused endodermally derived epithelium to proliferate and finally to form a tumor. The right and left primordial gonads are indeed located directly under the diaphragm before their descent, at the level of the dorsocranial side of the liver and the tail of the pancreas, respectively. Furthermore, the cells covering the gonads show an activated morphology in contrast to the peritoneal epithelium elsewhere, which suggests that they have the ability to detach from the gonadal surface, cross the peritoneal cleft, and attach to the peritoneal surface of nearby organs. This hypothesis would explain the predominance of cystadenoma in the body or tail of the pancreas, rather than in the head, as well as the apparent predominance of liver cystadenoma in segment IV. Splenogonadal fusion has also been documented, and demonstration of endocrine cells in about 50% of cystadenomas is a distinctive feature compatible with the hypothesis of these tumors developing from peribiliary glands.
The OS resembles the primitive embryonic mesenchyma of embryonic gallbladder and large bile ducts that contribute to the connective tissue surrounding the bile ducts, and it has therefore also been suggested that these tumors could derive from ectopic embryonal tissue destined to form the gallbladder or from ectopic embryonic rests of primitive foregut sequestered within the liver.
Intrahepatic biliary cystadenoma with an OS is exclusively observed in women, with few exceptions. Age at diagnosis is highly variable, between 1 year and 70 years, but it peaks in the fourth or early fifth decade. In most patients, the tumor is discovered during the workup of epigastric or right upper quadrant pain or vague abdominal complaints that include abdominal discomfort or swelling. Palpation of an abdominal mass that moves freely with respiration is also a classic circumstance of diagnosis. Because the tumor may grow to a considerable size, a gradual increase in abdominal girth and/or compression of the stomach or duodenum may also occur; however, because of the slow progression of the neoplasm, the onset of symptoms tends to be insidious and to have evolved for a prolonged period of time before treatment. , This may explain why large tumors are over-represented in most reports of cystadenomas. With the increasingly liberal use of imaging to investigate even the most minor symptoms, cystadenomas are often discovered incidentally, and it is possible that a significant proportion are not identified or are mistaken for simple cysts (see Chapter 73 ).
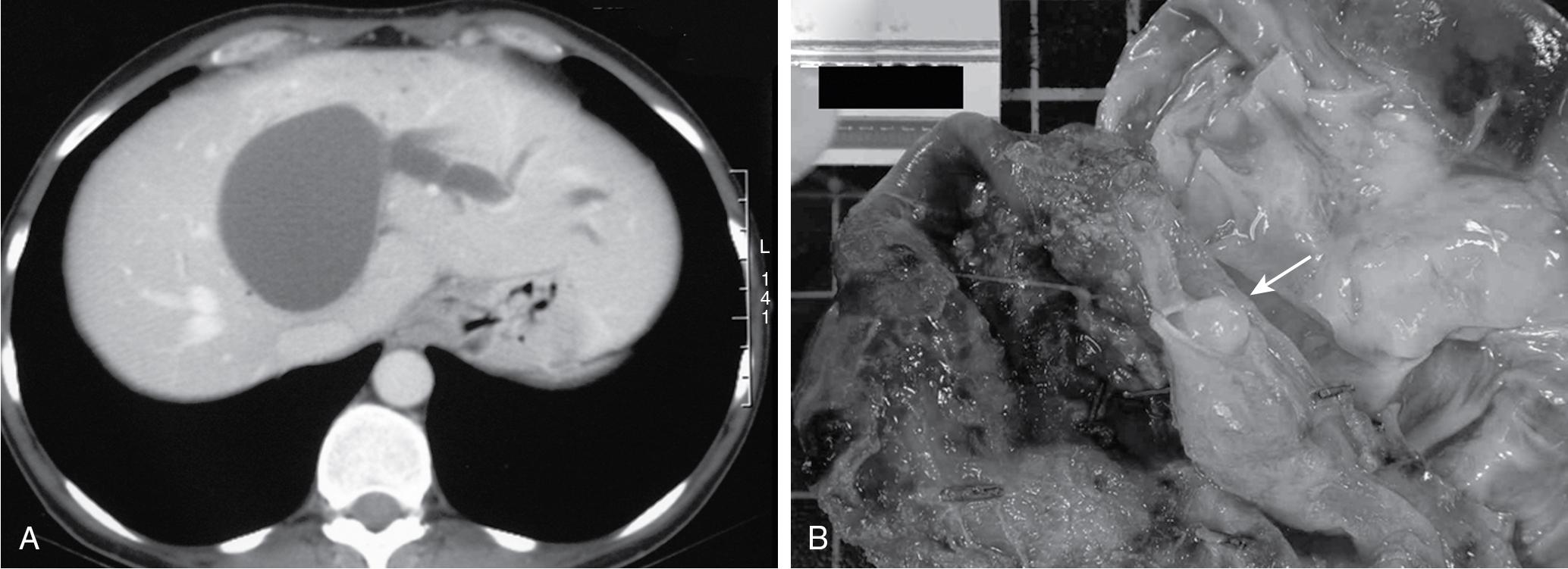
More acute episodes of pain have been reported in up to 35% of the patients, and most of these are related to biliary obstruction. , This is biologically witnessed by concomitant cytolysis or cholestasis. Jaundice or itching may also be present, whereas cholangitis is rare. Typically, such episodes are transient, and any jaundice tends to resolve spontaneously, which is compatible with the migration of mucous material or tumor embolus from the cyst into the bile duct ( Fig. 88B.4 ). Such tumor protrusion in the bile duct lumen has been reported even for small cystadenomas less than 4 cm in diameter. An alternative mechanism of obstruction is simple compression of the biliary confluence by the cystadenoma. Other causes of acute presentation have included tumor rupture, superinfection, bleeding, and caval compression, but these are rare.
Apart from the other cystic tumors addressed in this chapter, most notably cystadenocarcinoma, the main differential diagnosis of cystadenoma is simple cysts that have become atypical on imaging studies as a result of intracystic bleeding or previous sclerotherapy (see Chapter 73 ). The risk of mistaking a cystadenoma for a benign cyst is that this lesion may be treated by simple unroofing, which is an inappropriate treatment associated with a high risk of recurrence (see “Management” later); to mistake a simple or atypical cyst for a cystadenoma is to perform an occasionally risky and unwarranted resection because simple cysts do not require complete resection. Considering the very high incidence of simple cysts, the latter is probably much more common, and it has been shown that a cystadenoma-like lesion is almost as likely to be a simple cyst as to be a cystadenoma. , Clinical history is totally unreliable in the diagnosis of hemorrhagic cysts because intracystic hemorrhage can occur in the absence of any symptoms, and the diagnosis mainly relies on imaging (see Chapter 14 ).
Alternative differential diagnoses include nonsuppurative granulomatous infection of a simple cyst, hepatic abscess (see Chapter 70 ), echinococcal cysts (see Chapter 72 ), mesenchymal hamartoma (see Chapter 88A ), ciliated hepatic foregut cysts (see Chapter 88A ), intrahepatic lymphangioma (see Chapter 88A ), cystic hemangioma (see Chapter 88A ), cystic forms of hepatocellular carcinoma (see Chapter 89 ), ICC (see Chapter 50 ), mucin-producing metastases from thyroid or colon carcinoma, and cystic metastases of the ovary, of melanoma, and of kidney and neuroendocrine tumors. They have also been occasionally confused with pancreatic cysts.
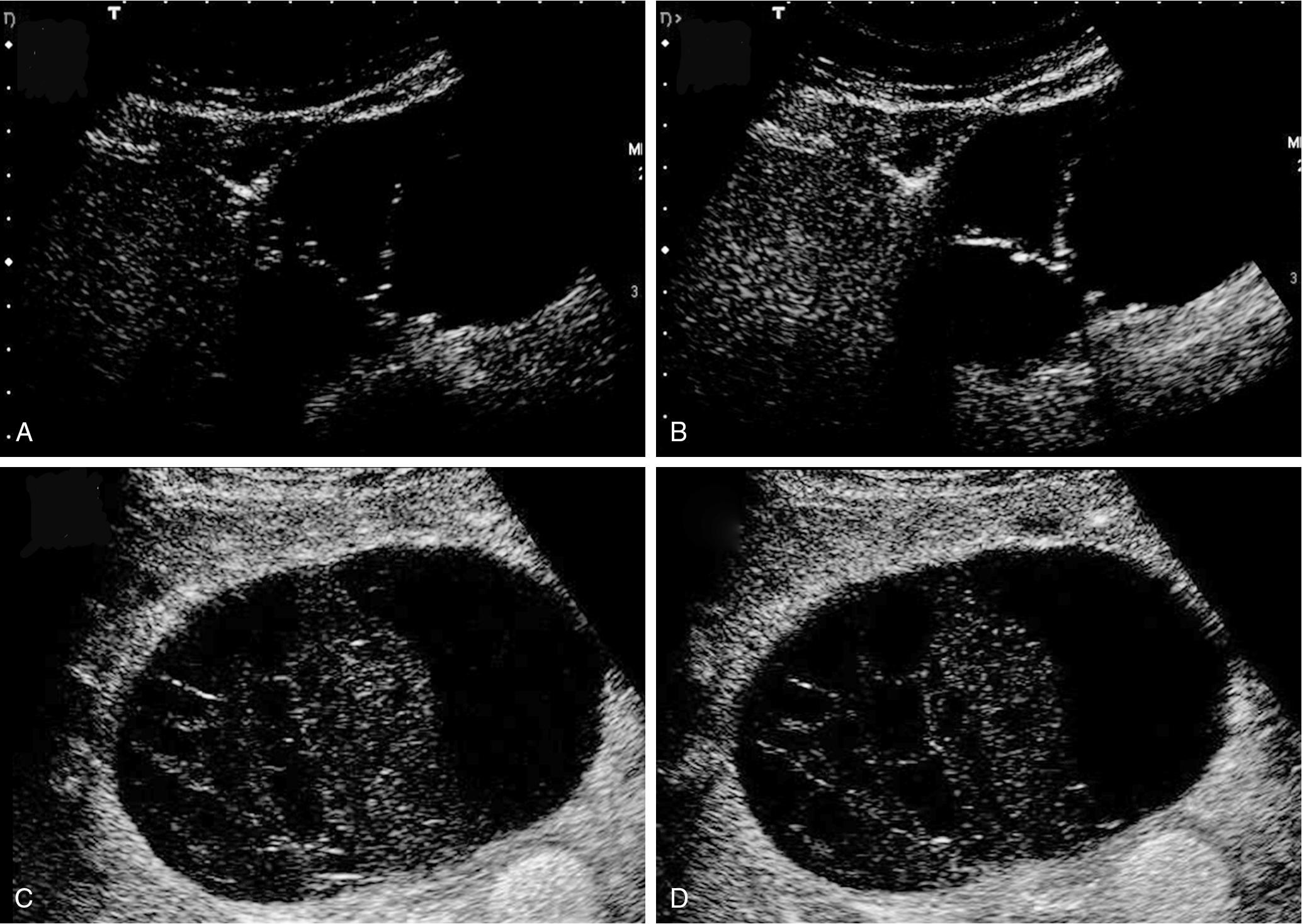
The characteristic ultrasonographic (US) finding for biliary cystadenoma is an anechoic mass with echogenic internal septations ( Fig. 88B.5 ). Papillary projections into the cystic space may also be seen. On computed tomography (CT) scans, the lesions appear as multiloculated hypodense masses with a well-defined wall. The content demonstrates fluid attenuation because of the presence of mucin, blood, or bile. Fine septal calcifications may occasionally be seen, and both the wall and the septations enhance after administration of contrast material (see Fig. 88B.1).
With magnetic resonance imaging (MRI), cystadenoma is typically seen as a fluid-containing multilocular cyst with homogeneous high signal intensity on T2-weighted images and homogeneous low or isosignal intensity on T1-weighted images. These signals may vary depending on the content of the cystic fluid. Mucinous fluid will appear with an isosignal, serous fluid with a hyposignal, and hemorrhagic fluid with a hyperintense signal that can only be seen in the lower part of a fluid-fluid level. Thin internal septal structures separate fluid-filled spaces. These, along with the wall of the lesion, are contrast enhanced ( Fig. 88B.6 ).
Contrast US is a reliable exploration that shows a typical honeycomb enhancement pattern of the cyst wall and septa. An intracystic structure of complicated simple cysts corresponds to clots and is not enhanced. Although the periphery of simple cyst may show enhancement, this corresponds to compressed adjacent liver, and this should be differentiated from enhancement of the cyst wall of cystadenoma (see Fig. 88B.5 ).
As for other cystic lesions, CT scan is less reliable and accurate than US or MRI (see Chapter 14 ). Cystadenoma in particular may wrongly appear unilocular on CT scan, whereas US and MRI , will visualize the internal septa. Two additional features besides multilocularity may help in the differential diagnosis of simple cysts: They are frequently multiple, whereas cystadenomas are single lesions, and although biliary dilation has been considered uncommon, a mild enlargement upstream of the tumor is probably more frequent than previously thought; using higher resolution imaging, enlargement was observed in one- to two-thirds of the patients in a recent series. , Along the same line, an increase in serum alkaline phosphatase levels has recently been shown to be a feature distinctive from simple cysts.
Aspiration cytology is either nonspecific or shows chronic inflammatory exudates with large numbers of neutrophils, lymphocytes, and macrophages. A few groups of nonatypical bland cuboidal-to-columnar epithelial cells, occasionally arranged in papillary clusters, may be seen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here