Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
|
|
|
|
Cerebrospinal fluid (CSF) leak from an incidental dural tear is not uncommon in cervical spine surgery. Various studies have reported an overall prevalence ranging from 0.5% to 3%. However, for cervical spine operations in patients with ossification of the posterior longitudinal ligament (OPLL), the incidence is much higher, ranging from 4.3% to 32%. Hannallah and associates reported that the presence of OPLL was the greatest risk factor for the development of a CSF leak after anterior decompression surgical procedures, and patients with OPLL were 13.7 times more likely to have a CSF leak than were patients without this condition.
Dural tears can occur in certain procedures during cervical spine dissection and decompression. The use of an electrocautery device during a posterior exposure, a pituitary rongeur during anterior diskectomy, a Kerrison rongeur during resection of the posterior longitudinal ligament and posterior foraminotomy, and elevation of the lamina during laminoplasty may all inadvertently tear the dura. As previously mentioned, anterior decompression with resection of the OPLL has been associated with the highest risk of producing a dural tear.
The development of meningitis, spinocutaneous fistula, or pseudomeningocele has been associated with CSF leaks in the cervical spine. In addition, patients with inadequately treated dural tears can present with delayed wound healing, postural headaches, vertigo, posterior neck pain, nausea, diplopia, photophobia, tinnitus, and blurred vision. These symptoms are caused by a persistent CSF leak from the subarachnoid space. The subsequent decrease in CSF pressure leads to a loss of buoyancy and caudal displacement of the intracranial contents.
Because of the potential complications that may stem from an unresolved CSF leak, the surgeon must have a strategy to manage CSF leaks both intraoperatively and postoperatively. Repair should involve appropriate measures to promote healing of the dural tear. Cammisa and co-workers reported that when CSF leaks were recognized and treated appropriately, patients experienced no complications such as persistent recurrent headaches, meningitis, pseudomeningocele, cutaneous fistula, or neurologic deficit after an average follow-up of 22.4 months. Various techniques have been described to manage dural tears and CSF leaks. These include the following: primary closure with microsurgical suturing or microdural stapling; augmentation with collagen matrix, fat and fascia graft, and other biologic grafts such as equine or bovine pericardium; reinforcement with the use of fibrin glue or chemical sealants; and insertion of lumbar and wound drains.
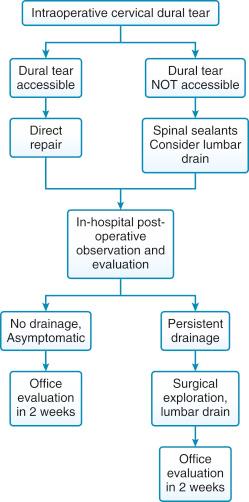
Management begins intraoperatively with proper identification of the dural tear ( Fig. 53-1 ). Ideally, all accessible dural tears are repaired primarily. If a violation of the dura is recognized during the surgical procedure and is amenable to direct repair, then primary closure with microsurgical suture is attempted. Primary repair techniques aim to provide a watertight seal of the dural tear. However, in some cases, the lack of dural elasticity or gapping resulting from resection of adherent or ossified dura precludes watertight closure with sutures. In these instances, primary repair with a microsuturing technique may fail because of the resultant pinhole-sized tears from suture needles that allow CSF to leak through the dura. The potential risk of using primary suture closure for small incidental dural tears is conversion of a low-pressure defect to high-pressure pinholes from suture needles. For this reason, intraoperative adjuncts such as collagen matrix (Duragen, Integra LifeSciences Corporation, Plainsboro, N.J.), autogenous fascia, and equine or bovine pericardium can be used to decrease the pressure gradient across the dural tear ( Fig. 53-2 ). Cain and colleagues studied the biology of dural tear repair in a canine model. These investigators found that fibroblastic bridging of the dural defect starts on the sixth day, and by the tenth day the defect is healed.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here