Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
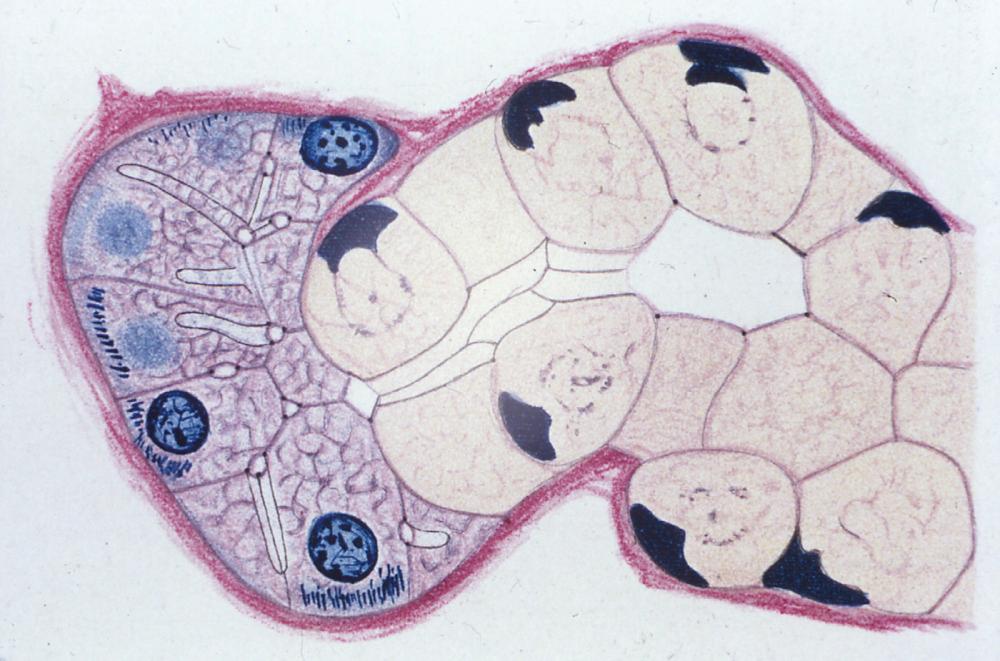
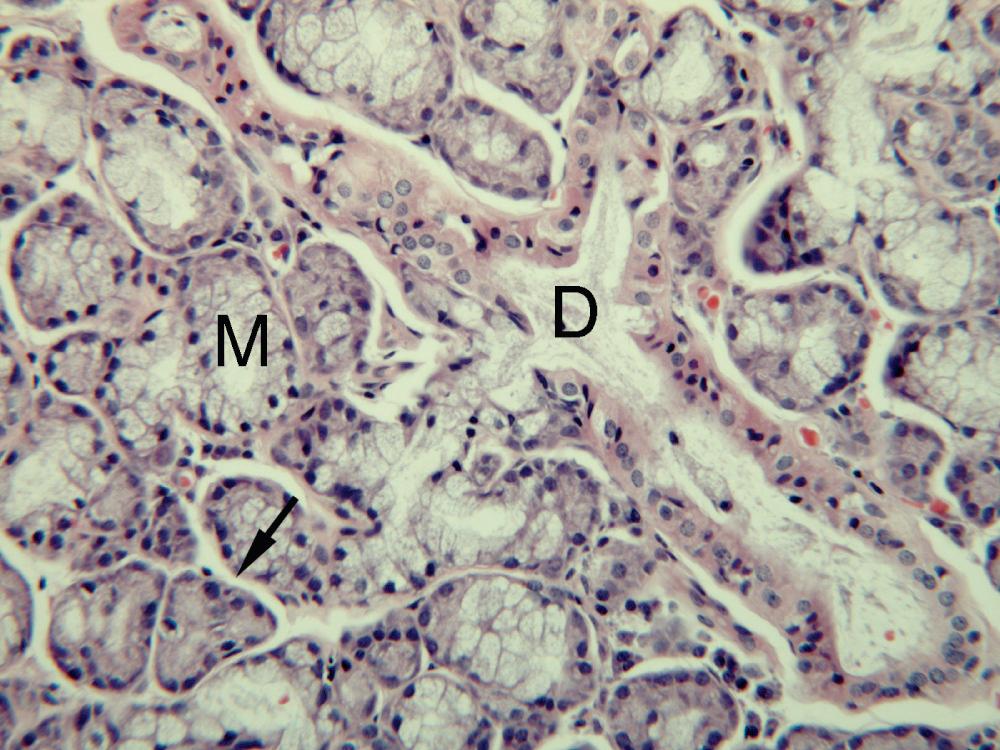
The histology of salivary glands was established by the end of the 19th century, when some intracellular organelles could be demonstrated ( Fig. 5.1 ). Today, the familiar and reproducible routine histologic appearance of the salivary glands is a light microscopic picture prepared from pieces of gland fixed in formaldehyde and embedded in paraffin wax from which sections are cut and stained with hematoxylin and eosin (H&E). However, there have been developments in histochemistry and electronmicroscopy that have revealed important information about both the histology and function of salivary glands. The present chapter is a brief survey but for those interested in more detail, see Berkovitz et al.
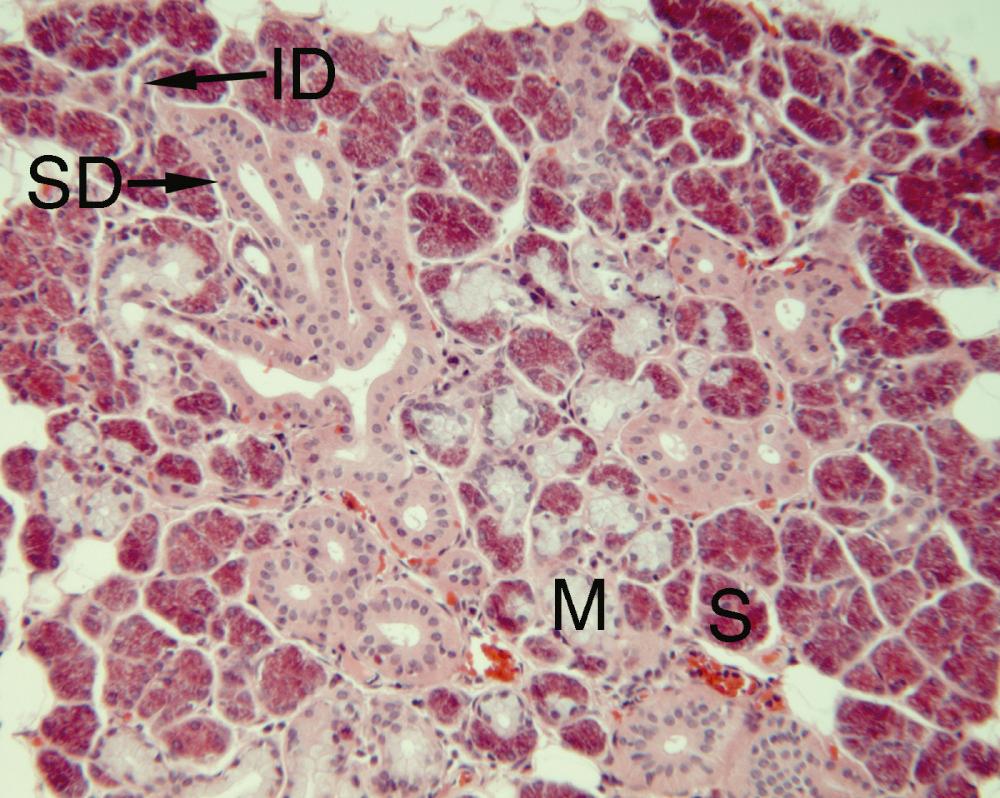
Salivary glands consist of glandular secretory tissue (the parenchyma) and the supporting connective tissue (the stroma). The parenchyma consists of secretory acini, intercalated ducts, striated ducts in parotid and submandibular glands, and collecting ducts, which join to form the main duct at the hilum.
There are two methods of protein secretion in salivary acini. The main, regulated pathway involves the synthesis of protein that is packaged into secretory granules by the Golgi apparatus and stored until a neural stimulus causes it to be secreted from the cell. The other, constitutive pathway involves the synthesis of protein that is packaged by the Golgi apparatus into small vesicles that immediately pass to the luminal or the basal cell membrane to be discharged. There is also transcytosis, whereby substances such as immunoglobulin A (IgA) from the interstitial tissue pass in vesicles from the basal cell membrane to the luminal cell membrane to be discharged.
Over 99% of the saliva is water. Primary saliva is isotonic with plasma and is produced in the acini by the transfer of sodium, chloride, and water across cell membranes and between adjacent cells into the lumen.
Parasympathetic and sympathetic secretomotor nerves supply the parenchymal cells and are responsible for reflex salivary secretion. Parasympathetic stimulation causes formation and secretion of secretory granules and secretion of fluid by the secretory cells, and sympathetic stimulation usually increases the output of preformed components from the secretory cells.
The parotid and submandibular gland only secrete saliva when neurally stimulated. However, the sublingual and mucous minor salivary glands produce a spontaneous, continuous very small secretion of saliva, as well as saliva produced by neural stimulation. The spontaneous secretion is of importance in the maintenance of the health of the oral surfaces and is also a factor in the development of extravasation mucoceles, in which mucus extravasated from these glands accumulates without relation to mealtimes.
The salivary glands show differences in their response to noxious stimuli including obstruction. The parotid is most sensitive, the sublingual and mucous minor glands the most resistant, and the submandibular gland is intermediate.
The salivary glands can be divided into: parotid with serous acini; submandibular gland with serous and mucous acini; and sublingual gland and minor salivary glands with mucous acini, except the posterior lingual glands of von Ebner with serous acini.
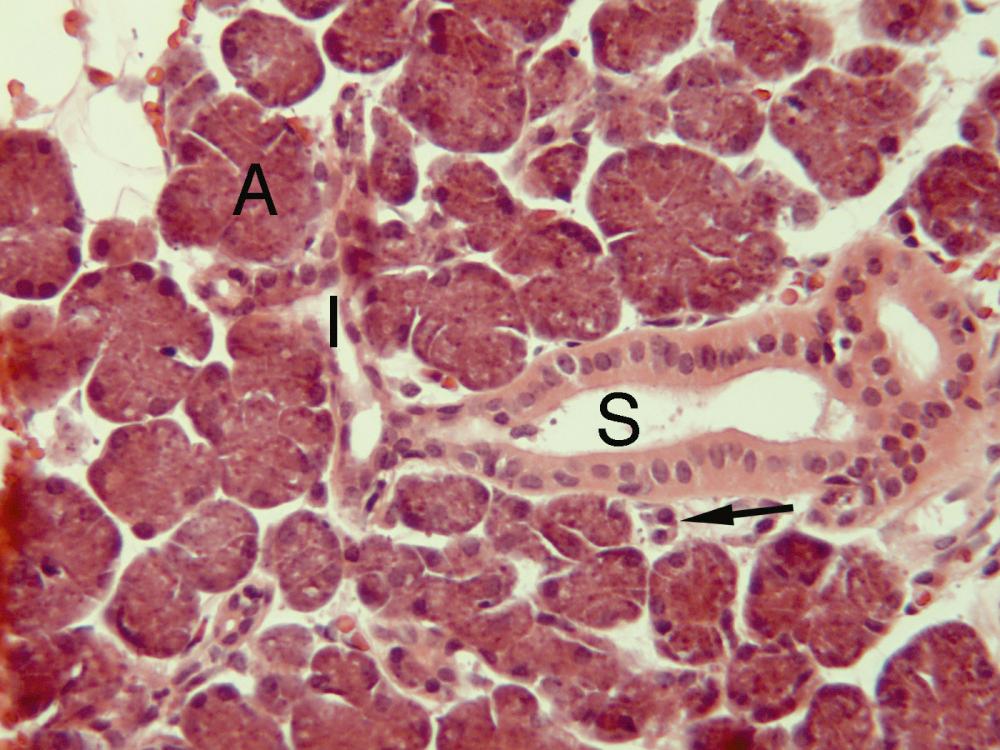
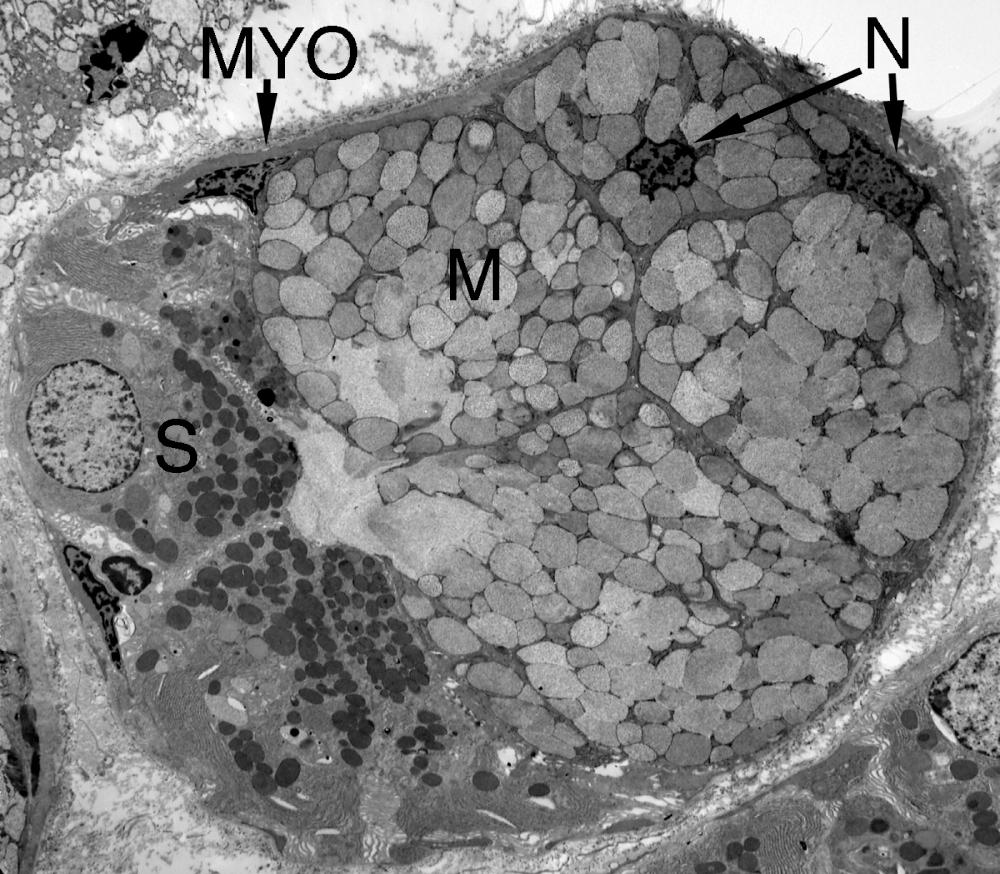
Serous acinar cells ( Figs. 5.1–5.5 ) contain discrete secretory granules, which can be seen more clearly electronmicroscopically (see Figs. 5.4 , 5.5 ). The secretory granules contain protein and glycoprotein. Useful information about the secretory glycoprotein, which can be termed mucin, is given by a mucosubstance histochemical technique, namely staining with Alcian Blue at pH 2.5 followed by the periodic-acid-Schiff procedure (ABPAS). It stains neutral mucin red and acidic mucin purple to royal blue depending on the acidity of the mucin. It shows the mucin of the serous cells of the parotid to be neutral and that of the serous cells of the submandibular gland to be a mixture of neutral and acidic mucins ( Fig. 5.6 ). The serous acinar cells ( Figs. 5.4 , 5.5 ) contain rough endoplasmic reticulum, where protein is produced by the ribosomes and is transported in the cisternae of the rough endoplasmic reticulum to the cis face of the Golgi apparatus. Carbohydrate is added to some of the protein in the Golgi apparatus to produce mucin. Protein and mucin are packaged at the trans face of the Golgi apparatus into condensing vacuoles, which develop into mature secretory granules. Electronmicroscopic histochemistry shows that many serous secretory granules are multipartite with mucin and protein in separate compartments. Mitochondria, which generate energy for metabolic processes, are present.

![Fig. 5.6, Submandibular gland with acidic mucin in mucous cells (M) stained diffusely royal blue. Serous cells (S) and intercalated ductal cells (I) contain a granular mixture of neutral mucin stained red and acidic mucin stained royal blue. (Section stained with Alcian Blue at pH 2.5 followed by periodic-acid-Schiff [ABPAS], ×180) Fig. 5.6, Submandibular gland with acidic mucin in mucous cells (M) stained diffusely royal blue. Serous cells (S) and intercalated ductal cells (I) contain a granular mixture of neutral mucin stained red and acidic mucin stained royal blue. (Section stained with Alcian Blue at pH 2.5 followed by periodic-acid-Schiff [ABPAS], ×180)](https://storage.googleapis.com/dl.dentistrykey.com/clinical/SalivaryGlandHistology/5_3s20B9780323672368000055.jpg)
Mucous acinar cells are seen light microscopically to contain a diffuse mass of secretory material that is weakly stained ( Figs. 5.1, 5.3, 5.7 ). They are seen electronmicroscopically to be packed with secretory granules ( Fig. 5.5 ). The ABPAS technique ( Fig. 5.6 ) shows the mucin to be a diffuse, strongly stained mass that varies from red to purple to royal blue, which indicates a variable mixture of neutral and acidic mucins. Electronmicroscopic histochemistry shows that mucous secretory granules are bipartite with little protein and extensive mucin in separate compartments. Rough endoplasmic reticulum, Golgi apparatus, and mitochondria are difficult to discern, and the nucleus is irregular in outline and usually at the base of the cell.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here